Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Enfermería: Cuidados Humanizados
versão impressa ISSN 1688-8375versão On-line ISSN 2393-6606
Enfermería (Montevideo) vol.13 no.1 Montevideo 2024 Epub 01-Jun-2024
https://doi.org/10.22235/ech.v13i1.3611
Original Articles
The Role of Nursing in Rapid Response Teams in the Care of Cardiorespiratory Arrest: An Integrative Review
1 Universidade Estadual Paulista “Julio de Mesquita Filho”, Brasil, s.meneguin@unesp.br
2 Universidade Estadual Paulista “Julio de Mesquita Filho”, Brasil
3 Universidade Estadual Paulista “Julio de Mesquita Filho”, Brasil
4 Universidade Estadual Paulista “Julio de Mesquita Filho”, Brasil
Objective:
To identify the role of nursing staff on rapid response teams in cases of cardiorespiratory arrest on different continents.
Methods:
An integrative review of the literature was performed. Searches were conducted in the PubMed, Web of Science, Scopus, Lilacs and CINAHL databases for studies published in Portuguese, English or Spanish between 2010 and 2020 that investigated the role of nursing staff on rapid response teams. The following search terms were used: rapid response team, nursing care, multiprofessional team, cardiac arrest and nursing.
Results:
The sample included six articles, half of which were from North America. The role of nurses on rapid response teams involved two dimensions: direct care for critical patients until the arrival of medical staff and the administrative functions of continuing education activities, the development of clinical protocols, improvement of communication between different sectors and care management.
Conclusions:
Nursing staff on rapid response teams play the role of coordinator of multiple care and management activities for hospitalized patients with signs of clinical deterioration who require immediate intervention.
Keywords: hospital rapid response team; nursing care; patient care team; nurses; nursing
Objetivo:
Identificar en la literatura científica el rol de equipo de enfermería en los equipos de respuesta rápida en la atención del paro cardiorrespiratorio, en las diferentes regiones continentales.
Metodología:
Se realizó una revisión integrativa de la literatura con búsqueda en las bases de datos PubMed, Web of Science, Scopus, Lilacs y CINAHL, utilizando los descriptores: equipo de respuesta rápida, cuidados de enfermería, atención de enfermería, equipo multiprofesional, paro cardíaco y enfermería. Se incluyeron estudios en portugués, inglés y español, publicados entre 2010 y 2020, que describieran el papel de la enfermería en los equipos de respuesta rápida.
Resultados:
La muestra comprendió 6 artículos y abarcó prácticamente la mitad del continente americano, específicamente en América del Norte. El papel de los enfermeros en los equipos de respuesta rápida incluye dos dimensiones: la asistencial, que abarca la atención directa al paciente crítico hasta la llegada del profesional médico, y la administrativa, relacionada con actividades de educación continua, elaboración de protocolos clínicos y comunicación entre sectores, equipos y gestión de la asistencia.
Conclusiones:
El equipo de enfermería, en los equipos de respuesta rápida, desarrolla el papel de coordinador de múltiples actividades asistenciales y de gestión para los pacientes hospitalizados con signos de empeoramiento clínico y que necesitan intervención inmediata.
Palabras clave: equipo hospitalario de respuesta rápida; atención de enfermería; grupo de atención al paciente; enfermeras y enfermeros; enfermería
Objetivo:
Identificar na literatura científica o papel da equipe de enfermagem em equipes de resposta rápida no atendimento à parada cardiorrespiratória em diferentes regiões continentais.
Metodologia:
Foi realizada uma revisão integrativa de literatura, com busca nas bases de dados PubMed, Web of Science, Scopus, Lilacs e CINAHL, utilizando os descritores: equipe de resposta rápida, cuidados de enfermagem, atendimento de enfermagem, equipe multiprofissional, parada cardíaca e enfermagem. Foram incluídos estudos em português, inglês e espanhol, publicados entre 2010 e 2020, que descrevessem o papel da enfermagem em equipes de resposta rápida.
Resultados:
A amostra foi composta por 6 artigos e abrangeu quase metade do continente americano, especificamente a América do Norte. O papel do enfermeiro em equipes de resposta rápida inclui duas dimensões: assistencial, abrangendo o cuidado direto ao paciente crítico até a chegada do profissional médico; e administrativa, relacionada a atividades de educação continuada, elaboração de protocolos clínicos e comunicação entre setores, equipes e gestão assistencial.
Conclusões:
A equipe de enfermagem em equipes de resposta rápida desempenha o papel de coordenadora de múltiplas atividades assistenciais e de gestão para os pacientes hospitalizados com sinais de deterioração clínica e que necessitam de intervenção imediata.
Palavras-chave: equipe hospitalaria de resposta rápida; atendimento de enfermagem; grupo de atendimento ao paciente; enfermeiras e enfermeiros; enfermagem
Introduction
Emergency situations that occur within the hospital setting require rapid, precise, safe action on the part of health care providers. Cardiac arrest is one of the most frequent emergency events in the hospital environment due to the rapid deterioration of the clinical state of patients in intensive care units (ICUs) and hospital wards. The reduction in oxygen saturation (< 80%), bradypnea (< 8 breaths per minute) and hypotension (systolic blood pressure < 80 mmHg) 1,2 constitute warning signs that enable the early identification of cardiac arrest and, consequently, the activation of the rapid response team (RRT).
According to the World Health Organization/Pan American Health Organization, cardiovascular diseases are the main cause of death, accounting for an estimated 17.0 million deaths throughout the world annually. (3 Besides being an important health problem on the global level, intra-hospital cardiac arrest is also one of the main causes of death in developed countries, with around 800 thousand cases annually in Europe and the United States. The incidence reported in the literature ranges from one to six events for each 1,000 hospitalized patients. 4 More than 200 thousand adults suffer cardiac arrest in hospital environments in the United States. 5,6 In Brazil, there are no official data and few studies have described the magnitude of the occurrence of cardiac arrest. However, approximately 200,000 cases per year is estimated, with half occurring within the hospital setting and the other half occurring elsewhere. (7)
Immediate intervention in terms of recognition to initiate cardiopulmonary resuscitation (CPR) is crucial to increasing the chance of survival until the arrival of the RRT. The main purpose is to provide immediate care to hospitalized patients with signs of clinical deterioration and who need immediate intervention. 8 The RRT began in 1991 in Australia 9 and in 2004 in the United States after a campaign promoted by the Institute for Healthcare Improvement with the aim of reducing deaths in the hospital environment through improvements in its structure and a reduction in preventable adverse events.10 After this campaign, the implementation of RRTs was recommended by the majority of agencies capable of carrying out this intervention. (7
In 2015, the American Heart Association updated cardiac arrest guidelines, proposing not only the understanding and execution of the practice of CPR, but also the early recognition of the clinical deterioration of patients in diverse hospital scenarios. 11 Thus, the RRT was introduced as the first link in the chain of survival (denominated “surveillance and prevention”) in cases of cardiac arrest in the hospital setting for the early identification of these events and the reduction in mortality rates. 12,13
In countries of Latin America, the implementation of RRTs has become an important institutional strategy, considering the scarcity of beds in ICUs at public hospitals. 14 Organizations such as the Joint Commission and Institute for Healthcare Improvement have recommended the existence of RRTs at hospitals 12,15) with the aim of providing improvements in the quality of health care as well as reductions in morbidity/mortality rates14,16,17,18 and cases of cardiac arrest outside the ICU. 19
The goal is to avoid the death of patients who exhibit clinical instability identified though the early analysis of vital variables. 14,20 Once activated, the RRT has roughly five minutes to assess the patient and define the main conduct. Delayed activation of the RRT, the frequency of which ranges from 21% to 56% of all calls, (21,22 continues to be a problem and increases morbidity and mortality rates. 21,23
There is no standardization with regards to the composition and functioning of the RRT and this team is often considered a mobile intensive care service due to the complexity of care provided for patients in critical situations. 24 In most cases of cardiac arrest, however, the nurse is the first member of the multidisciplinary team to identify signs of patient deterioration and must have both technical skill and scientific competence for immediate decision-making. 1
Nurses who work on RRTs provide care to critically ill patients in any part of the hospital, maintain the safety and quality of care for patients who are clinically deteriorating during their hospitalization, train teams to recognize clinical deterioration and participate in proactive assessments of patients at risk. (14,20,25) Although the implementation of RRTs in hospitals throughout the world is not recent, the functions performed by nurses as members of the multidisciplinary team are not widely known. 26,27
This lack of knowledge motivated the execution of the present investigation, as the quality of care is linked to the incorporation of good care practices based on scientific principles, clinical reasoning and the best scientific evidence.
Therefore, the aim of the present study was to identify the role of nursing staff on rapid response teams in cases of cardiorespiratory arrest on different continents through an integrative review of the literature.
Method
An integrative review was conducted to summarize evidence (theoretical or empirical) to provide a better understanding of the subject and contribute to evidence-based nursing science. Integrative reviews contribute to the development of theory as well as applicability in the field. 28
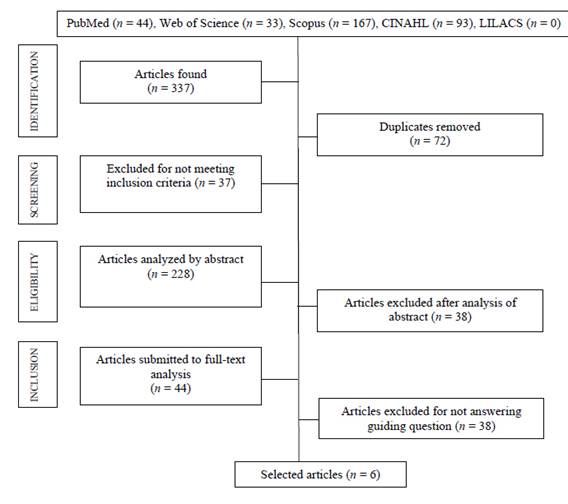
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA statement), involving five steps: identification of the research question; identification of valid studies relevant to the investigation; selection of articles; mapping of data extracted from the articles included; and narrative synthesis of the results.(29) For the present study, the following research question was used: What is the role of nursing staff on rapid response teams in cases of cardiac arrest on different continents?
Online searches were conducted of the US National Library of Medicine (PubMed), Web of Science, Scopus, Literatura Latinoamericana y del Caribe en Ciencias de la Salud (Lilacs (Latin American and Caribbean Health Sciences Literature)) and Current Nursing and Allied Health Literature (CINAHL) databases. The following search terms and Boolean operators (AND and OR) were used to search for relevant articles published in English, Spanish and Portuguese: equipo de respuesta rápida OR equipo hospitalario de respuesta rápida OR hospital rapid response team AND cuidados de enfermería OR atención de enfermería OR nursing care AND equipo multiprofesional OR patient care team OR grupo de atención al paciente AND parada cardíaca OR paro cardíaco OR cardiac arrest AND enfermería OR nursing.
Full articles published between 2010 and 2022 that answered the guiding question were included. This period was selected to provide adequate scope, relevance and methodological consistency. Review articles, books, theses, dissertations and articles with paid access were excluded.
After the searches, all records retrieved were grouped and entered into Microsoft Excel spreadsheets. Duplicates were removed. Two independent reviewers selected titles and abstracts using the following steps: contextualization, inclusion criteria, search strategy, article selection, data extraction and report of the results. (30 The eligibility and inclusion steps were conducted by the main investigator. For such, an instrument was created to extract and analyze the following data from the articles selected: title, author, journal/year/database, continent on which study was conducted and nursing action/intervention. After the selection process, six articles were included to compose the present integrative review, as shown in the PRISMA flowchart. 29
After the data extraction step, information on nursing staff activities was synthesized for categorization, followed by content analysis. 31 F3
As the present study had a methodological focus that did not involve direct contact with human beings, approval from a Human Research Ethics Committee was not required, according to Resolution n.º 510 of the National Board of Health, issued on April 7, 2016, for investigations in human and social sciences. 32
Results
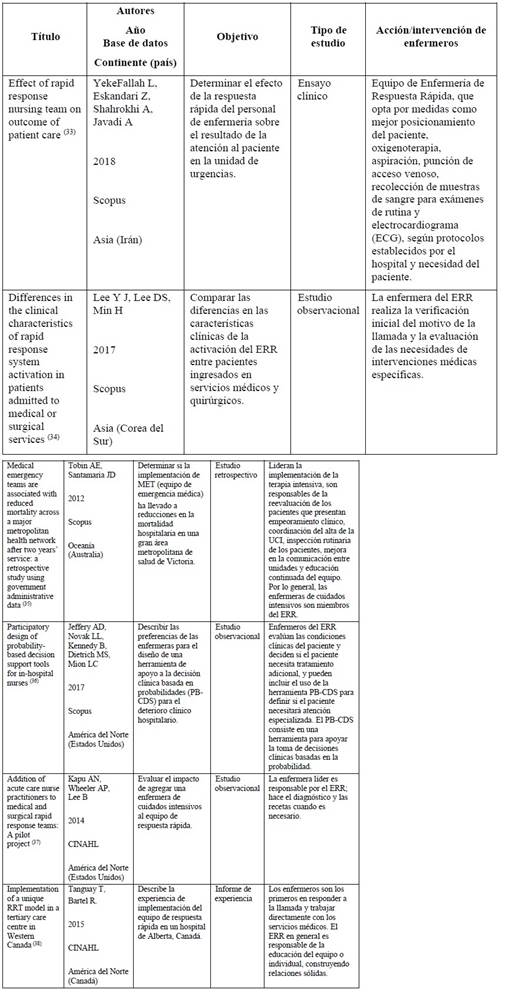
Among the articles selected, half of the studies were conducted in North America: Unites States (33%) and Canada (17%). The other studies were conducted in Asia (Iran (17%) and South Korea (17%)) and Oceania (Australia (17%)). No studies developed in South America or Europe were found. Among the databases searched, 66.6% of the articles selected were found in SCOPUS and 33.3% were found in CINAHL.T2
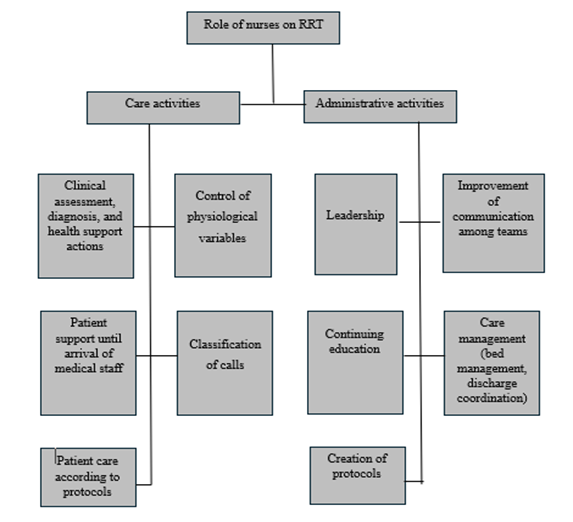
The main categories of nursing staff activities -care and administrative activities- were identified from the analysis of the studies, as shown in Figure 2.
Discussion
Nursing staff are historically known to be responsible for the practice of constant patient surveillance and follow-up and, as such, are the main protagonists in the early detection of cardiac arrest and prompt decision-making to activate the rapid response team (RRT). Such abilities are likely related to perceptions that arise from professional experience. 39
As members of the multidisciplinary team, nurses who participate on an RRT have the capacity to systematize emergency care and ensure the timely transfer of patients to the ICU. 33 In the care dimension, nursing activities involve the immediate care to the patient until and after the arrival of medical staff, based on the clinical assessment and support actions guided by clinical protocols. In the administrative dimension, nurses are involved in care management, the training of staff, the creation of protocols and improved communication between hospital sectors to optimize care.
The authors of the study conducted in South Korea report that, when a problem is not resolved by the ward nurse, the RRT is activated and is responsible for the first assessment of the patient. The RRT decides whether additional assessments and/or specific medical interventions are necessary and notifies the medical staff to ensure appropriate treatment. 34)
According to the research conducted in Australia, hospitals have an emergency medical team (EMT) that offers intensive care services and outreach services that offer health services to the population. Nurses typically manage the ICU and participate in the EMT. Outreach services are led by nurses who have a variety of responsibilities and perform various functions related to the management of discharge from the ICU, the reassessment of patients in a state of physiological deterioration, the improvement of communication between units as well as the offer of education and support to the wards. 35
In the studies carried out in the United States and Canada, nurses have different autonomy on the RRT. In one of the studies in the United States, all RRT nurses make an individual assessment of the patient and determine whether the patient needs a specialized medical intervention, contributing to the development of a technological tool for the assessment clinical deterioration as well as determining the likelihood of cardiac arrest and the need for admission to the ICU. The instrument is known as a probability-based clinical decision support (PB-CDS) tool. 36
In the other study from United States, the nurse in charge of the RRT follows defined protocols, such as fluid replacement and laboratory tests. After assessing the patient, RRTs led by nurses make the clinical diagnosis and determine actions for each case. Nurses record information on their activities to improve the quality of care, since a well-established relationship with the team facilitates the transfer of patients to the ICU and communication among the members of the multidisciplinary team. 37
The study from Canada showed that the RRT is led by an experienced critical care nurse or respiratory therapist, as these professionals are the first to respond to the call and work directly with medical care due to limitations with regards to immediate access to the intensive care physician when a patient becomes unstable. As an unconventional model, the RRT offers continuing education in diagnostic imaging units, all outpatient clinics and services, such as physical therapy and occupational therapy, as well as to nursing staff so that the team understands the role of each member for effective teamwork. 38)
The literature has shown that all these activities are important to reducing the incidence of death and cardiac arrest, but the quality of the scientific evidence is low, as shown in a Brazilian study on RRT activities. 24 The literature highlights five key categories considered essential to RRT effectiveness: institutional culture, team structure, experience, communication and teamwork. 40 However, the success of the work depends on the clear definition of the roles of each member on the team, who must have clinical and crisis management experience. 25
Studies conducted with RRT nurses report that the experience is very positive; in addition to contributing to the reduction in cases of cardiac arrest and intra-hospital complications, these nurses offer emotional support to other health professionals who provide care for critically ill patients (41, 42, 43) thus strengthening interpersonal relationships among the different teams that work within the hospital since the implementation of the RRT.
Limitations of the study
Few articles were found in the literature, demonstrating a gap in knowledge on the subject and limiting the number of findings that support the criteria listed. Moreover, the wide range of study designs makes it difficult to compare the results and few studies had the specific aim of assessing the roles of nursing staff.
Contribution of the study to practice
This study shows the important roles that nurses play in the organization and operationalization of RRTs. These complex, multifaceted roles follow well-established clinical protocols to ensure prompt, effective emergency care that achieves the expected success, demonstrating the importance of nursing staff on RRTs with regards to perfecting strategies and interventions that contribute to improving the quality of care for critically ill patients.
Conclusions
Nurses on rapid response teams play the role of coordinator of multiple care and administrative activities. In the care dimension, nurses provide direct care for critically ill patients until the arrival of medical staff. In the administrative dimension, the roles of nurses include continuing education activities, the development of clinical protocols, improved communication between hospital sectors and care management, such as bed management and discharge coordination.
We found no studies on the subject conducted in South America or Europe, despite the fact that RRTs are found in numerous hospitals. The nursing work process in the different continents where studies were found has similar characteristics with some particularities. Considering the limited production on the subject, further studies on the role of nurses on RRTs should be encouraged in other countries.
This study can also contribute to the development of other investigations, advancing knowledge on the role of nursing staff on rapid response teams, with data that highlight the importance of the actions carried out by these health professionals for hospitalized patients with signs of clinical deterioration requiring immediate intervention.
REFERENCES
1. Souza BT, Lopes MCBT, Okuno MFP, Batista REA, Góis AFT de, Campanharo CRV. Identification of warning signs for prevention of in-hospital cardiorespiratory arrest. Rev Latino-Am Enfermagem. 2019;27:e3072. doi: 10.1590/1518-8345.2853.3072 [ Links ]
2. Pulze G, da Silva Alves W, de Paiva BC, de Lucena Ferretti-Rebustini RE. Incidência e fatores associados à parada cardiorrespiratória nas primeiras 24 horas de internação em unidades de terapia intensiva. Rev Soc Cardiol Estado de São Paulo. 2019;29(2):192-196. doi: 0.29381/0103-8559/20192902192-6 [ Links ]
3. WHO/PAHO. Technical Advisory Group on Cardiovascular Disease Prevention Through Dietary Salt/Sodium Reduction: Final Report Phase 3 (Internet). 2024 (cited 2024 Mar 18). Available from: Available from: https://iris.paho.org/handle/10665.2/59313 [ Links ]
4. Tran A, Fernando SM, Rochwerg B, Vaillancourt C, Inaba K, Kyeremanteng K, et al. Pre-arrest and intra-arrest prognostic factors associated with survival following traumatic out-of-hospital cardiac arrest. A systematic review and meta-analysis. Resuscitation. 2020;153:119-135. doi: 10.1016/j.resuscitation.2020.05.052. [ Links ]
5. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics. 2019 Update: A Report From the American Heart Association. Circulation (Internet). 2019Mar 5 (cited 2023 Jan 20);139(10), e56-e528. doi: 10.1161/CIR.0000000000000659 [ Links ]
6. Holmberg MJ, Ross CE, Fitzmaurice GM, Chan PS, Duval-Arnould J, Grossestreuer AV, et al. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ: Cardiovascular Quality and Outcomes. 2019;12(7):e005580. doi: 10.1161/CIRCOUTCOMES.119.005580 [ Links ]
7. Futterman LG, Lemberg L. Cardiopulmonary resuscitation review: critical role of chest compressions. Am J Crit Care. 2005;14(1):81-84. doi: 10.4037/ajcc2005.14.1.81 [ Links ]
8. Gonzalez MM, Timerman S, Oliveira RG de, Polastri TF, Dallan LAP, Araújo S, et al. I Guideline for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Brazilian Society of Cardiology: Executive Summary. Arquivos Brasileiros de Cardiologia. 2013;100(2):105-113. doi: 10.5935/abc.20130022. [ Links ]
9. Dias AO, Martins EAP, Haddad M do CL. Instrumento para avaliação da qualidade do Time de Resposta Rápida em um hospital universitário público. Rev Bras Enferm. 2014;67(5):700-707. doi: 10.1590/0034-7167.2014670505 [ Links ]
10. Berwick DM. Overview of the 100,000 Lives Campaign (Internet). IHI’s 16th Annual National Forum on Quality Improvement in Health Care; 2004. Available from: https://www.ihi.org/engage/initiatives/completed/5millionlivescampaign/documents/overview%20of%20the%20100k%20campaign.pdf [ Links ]
11. American Heart Association. Destaques da American Heart Association 2015. Atualização das Diretrizes de RCP e ACE (Internet). 2015 (cited 2024 Mar 19). Available from: http://www.bombeiros.ms.gov.br/wp-content/uploads/2015/10/Atualiza%C3%A7%C3%A3o-das-Diretrizes-de-RCP-e-ACE-2015.pdf [ Links ]
12. Fischer CP, Bilimoria KY, Ghaferi AA. Rapid Response Teams as a Patient Safety Practice for Failure to Rescue. JAMA. 2021;326(2):179. doi: 10.1001/jama.2021.7510 [ Links ]
13. American Heart Association. Destaques das diretrizes de RCP e ACE de 2020 da American Heart Association (Internet). 2020. Available from: https://cpr.heart.org/-/media/cpr-files/cpr-guidelines-files/highlights/hghlghts_2020eccguidelines_portuguese.pdf [ Links ]
14. Churpek MM, Edelson DP. In search of the optimal rapid response system bundle: Optimal Rapid Response System Bundle. J Hosp Med. 2015;10(6):411-411. doi: 10.1002/jhm.2346 [ Links ]
15. Almeida MC, Portela MC, Paiva EP, Guimarães RR, Pereira Neto WC, Cardoso PR, et al. Implementation of a rapid response team in a large nonprofit Brazilian hospital: improving the quality of emergency care through Plan-Do-Study-Act. Revista Brasileira de Terapia Intensiva (Internet). 2019 (cited 2023 Jan 20);31(2). Available from: Available from: http://www.rbti.org.br/artigo/detalhes/0103507X-31-2-14 [ Links ]
16. Teuma Custo R, Trapani J. The impact of rapid response systems on mortality and cardiac arrests. A literature review. Intensive and Critical Care Nursing. 2020;59:102848. doi: 10.1016/j.iccn.2020.102848 [ Links ]
17. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19(1):254. doi: 10.1186/s13054-015-0973-y [ Links ]
18. Dias AO, Feijó IER, Fernandes KBP, Feijó VBER, Andraus RAC. Time de Resposta Rápida: percepção de enfermeiros sobre o atendimento do serviço em um hospital público de ensino. RSD. 2022;11(8):e32211831045. doi: 10.33448/rsd-v11i8.31045 [ Links ]
19. Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of in‐hospital cardiopulmonary arrest and mortality: A systematic review and meta‐analysis. Journal of Hospital Medicine. 2016;11(6):438-445. doi: 10.1002/jhm.2554 [ Links ]
20. Dias ADO, Bernardes A, Chaves LDP, Sonobe HM, Grion CMC, Haddad MDCFL. Critical incidents as perceived by rapid response teams in emergency services. Rev esc enferm USP. 2020;54:e03595. doi: 10.1590/S1980-220X2018027903595 [ Links ]
21. Barwise A, Thongprayoon C, Gajic O, Jensen J, Herasevich V, Pickering BW. Delayed Rapid Response Team Activation Is Associated With Increased Hospital Mortality, Morbidity, and Length of Stay in a Tertiary Care Institution. Critical Care Medicine. 2016;44(1):54-63. doi: 10.1097/CCM.0000000000001346 [ Links ]
22. Boniatti MM, Azzolini N, Viana MV, Ribeiro BSP, Coelho RS, Castilho RK, et al. Delayed Medical Emergency Team Calls and Associated Outcomes. Critical Care Medicine. 2014;42(1):26-30. doi: 10.1097/CCM.0b013e31829e53b9 [ Links ]
23. Tirkkonen J, Ylä-Mattila J, Olkkola KT, Huhtala H, Tenhunen J, Hoppu S. Factors associated with delayed activation of medical emergency team and excess mortality: An Utstein-style analysis. Resuscitation . 2013;84(2):173-8. doi: 10.1016/j.resuscitation.2012.09.021 [ Links ]
24. Rocha HAL, Alcântara AC de C, Rocha SGMO, Toscano CM. Effectiveness of rapid response teams in reducing intrahospital cardiac arrests and deaths: a systematic review and meta-analysis. Revista Brasileira de Terapia Intensiva (Internet). 2018 (cited 2023 Jan 20);30(3). doi: 10.5935/0103-507X.20180049 [ Links ]
25. Jackson SA. Equipos de respuesta rápida: ¿qué novedades hay? Nursing. 2018;35(4):30-37. doi: 10.1016/j.nursi.2018.07.009 [ Links ]
26. Rigotti AR, Brugugnolli ID, Ariosa RH, Coutinho NC. Informe de experiencia: implantación del equipo de respuesta rápida en un hospital público de nivel secundario en el interior de São Paulo. Cuidarte Enfermagem (Internet). 2019;13(2). Available from: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1087619 [ Links ]
27. Rincón-López JV, Larrotta-Castillo D, Estrada-Orozco K, Gaitán-Duarte H. Estructura y función de los equipos de respuesta rápida para la atención de adultos en contextos hospitalarios de alta complejidad: Revisión sistemática de alcance. Rev Colomb Obstet Ginecol. 2021;72(2):171-92. doi: 10.18597/rcog.3671 [ Links ]
28. Guirao Goris SJA. Utilidad y tipos de revisión de literatura. 2015;9(2). doi: 10.4321/S1988-348X2015000200002 [ Links ]
29. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71). doi: 10.1136/bmj.n71. [ Links ]
30. Mendes KDS, Silveira RCDCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto contexto - enferm. 2008;17(4):758-764. doi: 10.1590/S0104-07072008000400018 [ Links ]
31. Minayo, Maria Cecília de Souza. The challenge of knowledge: qualitative research on health. São Paulo; Hucitec. 2004; p. 269. [ Links ]
32. Ministério da Saúde. Conselho Nacional de Saúde. Resolução no. 510 de 07 de abril de 2016. [ Links ]
33. YekeFallah L, Eskandari Z, Shahrokhi A, Javadi A. Effect of Rapid Response Nursing Team on Outcome of Patient Care. Trauma Mon (Internet). 2018 May 14 (cited 2023 Oct 13);23(4). Available from: Available from: http://traumamon.com/en/articles/14488.html [ Links ]
34. Lee YJ, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Differences in the Clinical Characteristics of Rapid Response System Activation in Patients Admitted to Medical or Surgical Services. J Korean Med Sci. 2017;32(4):688. doi: 10.3346/jkms.2017.32.4.688 [ Links ]
35. Tobin AE, Santamaria JD. Medical emergency teams are associated with reduced mortality across a major metropolitan health network after two years service: a retrospective study using government administrative data. Crit Care . 2012;16(5):R210. [ Links ]
36. Jeffery AD, Novak LL, Kennedy B, Dietrich MS, Mion LC. Participatory design of probability-based decision support tools for in-hospital nurses. Journal of the American Medical Informatics Association. 2017;24(6):1102-10. doi: 10.1093/jamia/ocx060 [ Links ]
37. Kapu AN, Wheeler AP, Lee B. Addition of Acute Care Nurse Practitioners to Medical and Surgical Rapid Response Teams: A Pilot Project. Critical Care Nurse. 2014;34(1):51-60. doi: 10.4037/ccn2014847 [ Links ]
38. Tanguay T, Bartel R. Implementation of a unique RRT model in a tertiary care centre in Western Canada. Can J Crit Care Nurs. 2017;28(1):34-7. [ Links ]
39. Queiroz ÁS de, Nogueira L de S. Nurses’ perception of the quality of the Rapid Response Team. Rev Bras Enferm. 2019;72(suppl 1):228-234. doi: 10.1590/0034-7167-2017-0168 [ Links ]
40. Sørensen EM, Petersen JA. Performance of the efferent limb of a rapid response system: an observational study of medical emergency team calls. Scand J Trauma Resusc Emerg Med. 2015;23(1):69. doi: 10.1186/s13049-015-0153-8 [ Links ]
41. Jackson S, Penprase B, Grobbel C. Factors Influencing Registered Nurses’ Decision to Activate an Adult Rapid Response Team in a Community Hospital. Dimensions of Critical Care Nursing. 2016;35(2):99-107. doi: 10.1097/DCC.0000000000000162 [ Links ]
42. Radeschi G, Urso F, Campagna S, Berchialla P, Borga S, Mina A, et al. Factors affecting attitudes and barriers to a medical emergency team among nurses and medical doctors: A multi-centre survey. Resuscitation . 2015;88:92-98. doi: 10.1016/j.resuscitation.2014.12.027 [ Links ]
43. Stolldorf DP. Original Research: The Benefits of Rapid Response Teams Exploring Perceptions of Nurse Leaders, Team Members, and End Users. American Journal of Nursing. 2016;116(3):38-47. doi: 10.1097/01.NAJ.0000481279.45428.5a [ Links ]
How to cite: Meneguin S, Pollo B, Pollo CF, Segalla AVZ. The Role of Nursing in Rapid Response Teams in the Care of Cardiorespiratory Arrest: An Integrative Review. Enfermería: Cuidados Humanizados. 2024;13(1):e3611. doi: 10.22235/ech.v13i1.3611
Authors’ contribution (CRediT Taxonomy): 1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing. S. M. has contributed in 1, 3, 5, 6, 7, 8, 11, 12, 13, 14; B. P. in 2, 3, 5, 9; C. F. P. in 2, 3, 5, 6, 10, 13, 14; A. V. Z. S. in 11, 13.
Received: July 31, 2023; Accepted: March 22, 2024











 texto em
texto em 
 Curriculum ScienTI
Curriculum ScienTI