Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.25 no.42 Montevideo 2023 Epub 01-Dez-2023
https://doi.org/10.22592/ode2023n42e416
Case report
Paracoccidioidomicosis, reflection of a disseminated mycosis: case report
1Institución Universitaria Visión de las Américas, Sede Medellín, Colombia.
2Institución Universitaria Visión de las Américas, Sede Medellín, Colombia. eilien.tovio@uam.edu.co
3Universidad de Antioquia, Colombia
4Universidad de Antioquia, Colombia
Introduction:
Paracoccidioidomycosis is an endemic mycosis in different Latin American countries, including areas of Colombia, with a very varied clinical manifestation since it is considered a disease that can be chronic and systemic.
Objectives:
To expose the importance of the clinical-stomatological examination in the detection of different entities in the stomatognathic system, and the multidisciplinary management of oral and systemic paracoccidioidomycosis.
Clinical case:
male patient in the sixth decade of life, who presented glossalgia and pain in the ocular region. Clinically, it presents a granulomatous-type lesion on the lateral edges of the tongue with evolution of approximately 1 year ago, the result of the biopsy is paracoccidioidomycosis, multidisciplinary management is started with intravenous and oral medications, after 10 months it resolves. Conclusions: a good questioning, analysis of the clinical picture and complementary tests are key to early diagnosis and timely treatment, preserving the patient's life, especially in opportunistic infections such as paracoccidioidomycosis.
Key words: paracoccidioidomycosis; mycosis; Invasive Fungal Infections; Pathological Conditions, Signs and Symptoms; mycobiome (Mesh)
Introducción:
La paracoccidioidomicosis, es una micosis endémica en diferentes países de latinoamérica, incluyendo zonas de Colombia, con manifestación clínica muy variada ya que es considerada una enfermedad que puede ser crónica y sistémica.
Objetivos:
Exponer la importancia del examen clínico-estomatológico en la detección de diferentes entidades en sistema estomatognático, y el manejo multidisciplinario de paracoccidioidomicosis oral y sistémica.
Caso clínico:
paciente masculino en sexta década de vida, el cual presenta glosalgia y dolor de región ocular. Clínicamente presenta lesión de tipo granulomatoso en bordes laterales de lengua con evolución de hace 1 año aproximadamente, el resultado de la biopsia es paracoccidioidomicosis, se inicia manejo multidisciplinario con medicamentos intravenosos y orales, luego de 10 meses presenta resolución de este.
Conclusiones:
un buen interrogatorio, análisis de cuadro clínico y exámenes complementarios, son claves para un diagnóstico temprano y tratamiento oportuno, preservando la vida del paciente, especialmente en infecciones oportunistas como la paracoccidioidomicosis.
Palabras clave: paracoccidioidomicosis; micosis; infecciones fúngicas invasoras, condiciones patológicas, signos y síntomas; micobioma (DeCS)
Introdução:
A paracoccidioidomicose é uma micose endêmica em diferentes países da América Latina, incluindo áreas da Colômbia, com manifestação clínica muito variada por ser considerada uma doença que pode ser crônica e sistêmica.
Objetivos:
Expor a importância do exame clínico-estomatológico na detecção de diferentes entidades do sistema estomatognático e no manejo multidisciplinar da paracoccidioidomicose oral e sistêmica.
Caso clínico:
paciente do sexo masculino na sexta década de vida, que apresentava glossalgia e dor na região ocular. Clinicamente apresenta lesão tipo granulomatosa nas bordas laterais da língua com evolução de aproximadamente 1 ano, resultado da biópsia é paracoccidioidomicose, inicia-se manejo multidisciplinar com medicações endovenosas e orais, após 10 meses resolve.
Conclusões:
um bom questionamento, análise do quadro clínico e exames complementares são fundamentais para o diagnóstico precoce e tratamento oportuno, preservando a vida do paciente, principalmente nas infecções oportunistas como a paracoccidioidomicose.
Palavras-chave: paracoccidioidomicose; micoses; infecções fúngicas invasivas, condições patológicas, sinais e sintomas; micobioma
INTRODUCTION
Mycotic pathologies are prevalent in dentistry. Therefore, dentists should be trained to recognize them at an early stage, since many of the lesions begin as ulcers, bleeding red spots, or infiltrates in the lips and tongue. Additionally, various effects can be observed in the oropharynx and the oral mucosa in general1.
Paracoccidioidomycosis is considered a multifocal disease that can develop into a systemic one, and it is caused by a fungal etiologic agent called Paracoccidioides spp2. The predominant species is Paracoccidioides brasiliensis, which belongs to the group of dimorphic fungi or yeast-like molds. These species are able to change their morphology and metabolism to adapt to the environment, which gives them a biological advantage and constitutes their primary virulence factor. It provides them with enhanced resistance and efficiency in evading the immune response, thereby facilitating the maintenance of their progeny in the hosts3.
Epidemiologically, both men and women are equally likely to suffer from this mycosis. However, this disease is more prevalent in men between the ages of 30 and 50 years when clinical manifestations are exhibited. For women, it is believed that sexual hormones serve as a barrier to yeast formation so they do not develop chronic cases4.
Paracoccidioidomycosis is classified among endemic mycoses, meaning it is present in specific geographical regions worldwide. It is particularly prevalent in South American countries, including Brazil, Colombia, Venezuela, and Peru. Primarily concentrated in the Amazon region of these countries, its dissemination has increased due to migrations5. This condition contributes to 51% of deaths caused by systemic mycoses. However, in Colombia, its impact varies from 0.5 to 2.2 cases per 100,000 inhabitants in at least nine departments in the Sierra Nevada de Santa Marta and the Andean region, recognized as endemic areas6-7.
This mycosis generally affects lymph nodes, skin, lungs, and oral, nasal, and gastrointestinal mucous membranes. The disease can take many forms and affect various organs, even simultaneously, becoming potentially fatal and severe; this always depends on the host's level of immunocompetence8. Oral clinical manifestations can range from intraoral lesions, such as painful gums and palate ulcers with necrotic and granulomatous bases, to tooth loss or periodontal disease with high prevalence 9. At a systemic level, various clinical manifestations have been observed in different organs, including generalized or localized lymphadenomegaly, weight loss, loss of appetite, and fever. Additionally, it is infrequently associated with appendicitis 10.
Radiographically, pulmonary lesions can be diagnosed showing ground-glass, reticular, and diffuse nodular interstitial opacities, typical of infection by conidia of Paracoccidioides spp11.
Furthermore, histopathological studies typically reveal chronic inflammation characterized by multinucleated giant cells and epithelioid macrophages containing substantial amounts of the fungus. This analysis is conducted using methenamine silver or hematoxylin-eosin stains. These studies also aid in the differential diagnosis of the disease, preventing confusion with syphilis, tuberculosis, or any neoplasia exhibiting similar lesions. To confirm this mycosis, conclusive histological and clinical findings are essential 10.
The treatment of mycosis typically takes an extended period, lasting approximately six to twelve months from the initiation of therapy. The duration depends on the severity of the disease, the organs affected, and whether it is predominantly an acute or chronic condition. Itraconazole is the most commonly prescribed drug for mild or moderate cases, given its lack of adverse effects when used for short periods. Sulfamethoxazole and trimethoprim can also be employed. Amphotericin B is used for severe manifestations. Following the treatment period, the resolution of symptoms and clinical signs, such as mucosal and skin lesions, should be evident, along with the elimination of the causative agent 12.
Given the high prevalence of systemic paracoccidioidomycosis, a multidisciplinary approach is essential. This emphasizes the importance of training healthcare professionals, especially in endemic areas like Latin America, regarding the presence of this type of mycosis and the potential clinical conditions. Additionally, upon suspicion or a presumptive diagnosis, it is crucial to complement it with histopathological analysis of the lesion. This ensures the identification of splitting blastoconidia, resembling a ship's rudder as described by pathologists. This finding serves as a pathognomonic sign of Paracoccidioidomycosis spp10.
This article aims to expose the importance of the clinical-stomatological examination in the detection of different entities in the stomatognathic system, as well as the multidisciplinary management of oral and systemic paracoccidioidomycosis.
CASE REPORT
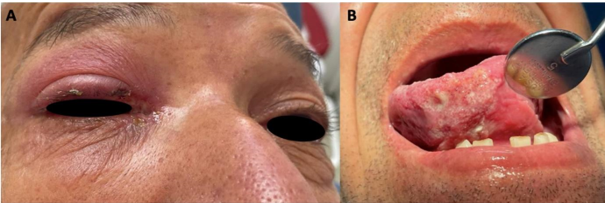
A male patient in his sixth decade of life, a farmer by profession with no significant medical history, sought consultation at the Maxillofacial Surgery Department of the Hospital San Vicente Fundación due to pain in the tongue and right eye (RE). He brought the histopathology results from a biopsy performed on the RE, indicating keratoacanthoma. Clinically, he exhibited upper palpebral ecchymosis, serous crusts on the inner canthus extending to the upper tarsal plate region, 360-degree conjunctival ecchymosis, pupils equal in size and reactive to light, anicteric left eye (LE) sclera, preserved ocular movements, and a fibrous tissue layer with a transparent whitish color extending from the inner canthus of LE to the ipsilateral cornea, associated with pterygium (Fig. 1a).
On stomatognathic examination, a granulomatous lesion, approximately 6 cm in diameter, was observed on the ventral side of the right-sided tongue. The lesion extended to the lateral edges of the ipsilateral tongue and consisted of whitish pseudoplaque areas that detached when scraped. Adjacent to these were erythematous punctate lesions, approximately 1 mm in diameter, with an evolution time of approximately 1 year. The lesion was asymptomatic upon palpation, exhibiting irregular, non-indurated, and well-defined borders. The etiology is currently unknown (Fig. 1b).
Due to the clinical characteristics of the ocular and oral mucosa lesions, a simple and contrast-enhanced Computed Tomography (CT) of the face and paranasal sinuses (PNS) and creatinine measurement were considered. The patient was also scheduled for a tongue biopsy.
An incisional biopsy was performed with a #6 punch at the anterior 1/3 of the right lateral border of the tongue, involving both compromised and healthy tissue, followed by a histopathological study. The results revealed extensive areas of ulceration and granulation tissue. In-depth, countless nodular formations of epithelioid histiocytes accompanied by multinucleated giant cells were identified.
No pathogens were identified in routine staining, so immunohistochemistry studies were conducted. ZN and modified ZN tests were negative for (AFB. Methenamine-silver staining presented abundant fungal structures of variable size and shape. Some displayed membrane reinforcement and central clearing, while others were large, folded, and many took the form of yeast with multiple budding, giving the impression of a ship rudder or a silhouette similar to "Mickey Mouse." The final diagnosis was paracoccidioidomycosis.
The initial CT imaging results of the face and simple and contrasted PNS showed no alterations in morphology. Based on the obtained results, it was decided to initiate treatment with itraconazole tablets at a dosage of 200 mg every 12 hours for 3 months.
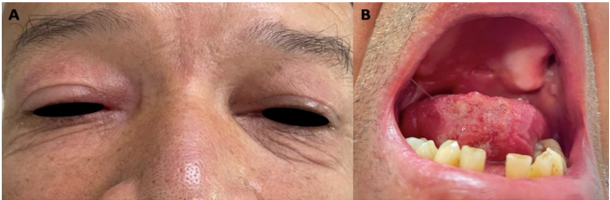
At the two-month follow-up, a significant improvement in the granulomatous lesions at the right eye (RE) and tongue levels was observed, although they persisted (Fig. 2a and b). Additionally, during the physical examination, palpation revealed a mass in the upper abdominal quadrant, accompanied by signs of respiratory distress. Consequently, a complete abdominal ultrasound and chest X-ray were requested, along with a cranial magnetic resonance imaging (MRI) to investigate pruritus in the right eye (RE). For the follow-up of drug management with itraconazole, a liver function evaluation was deemed necessary. This involved requesting Alanine transaminase (ALT), Aspartate transaminase (AST), Direct Bilirubin (BD), Indirect Bilirubin (BI), and Alkaline Phosphatase (AF).
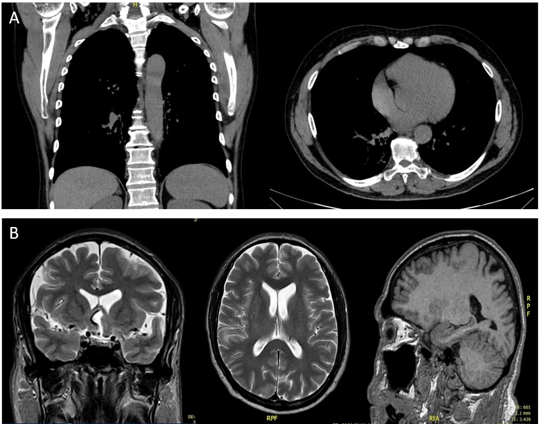
Chest X-ray imaging revealed micronodules (Fig. 3a), and an MRI of the skull showed hypodense areas predominantly in the anterior brain and preseptal cellulitis (Fig. 3b).
Liver transaminases were within normal parameters. With these results, disseminated ocular, periorbital, pulmonary, and lymph node paracoccidioidomycosis was considered. An evaluation by infectious disease specialists and neurosurgeons was requested based on these findings. The treatment plan provided by the infectious disease specialist includes fluconazole tablets of 200 mg every 6 hours, trimethoprim-sulfamethoxazole 160/800 mg every 24 hours, and amphotericin B deoxycholate 50 mg IV every 24 hours, all administered intravenously over a three-week period in the hospital.
On the other hand, neurosurgery recommended drainage in case of no improvement in infectious disease management; however, in the follow-up, such intervention was not necessary as there was marked improvement in CSF cytochemical results.
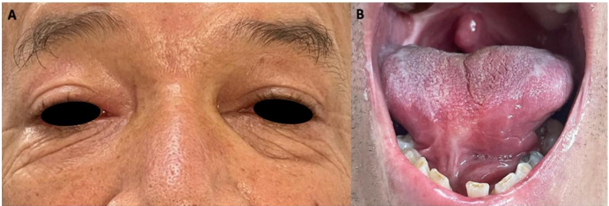
At the 10-month follow-up, there is clear evidence of complete resolution of the lesions in the RE and tongue (Fig. 4a and b). However, scar remnants left by paracoccidioidomycosis on the mucosa are also observable. Despite the treatment yielding satisfactory results, it is advised to continue for 6 additional months, completing a full year of medication as prescribed by the infectious disease specialist.
ETHICAL CONSIDERATIONS
All procedures conducted in the study involving human participants adhered to the ethical standards of the institutional and/or national research committee and to the Declaration of Helsinki 201313. Additionally, written informed consent was obtained from the patient for the publication of their clinical photographs as well as their permission to disclose the case, ensuring the protection of personal data and the patient's image.
DISCUSSION
Mycotic lesions in the oral mucosa are increasingly prevalent, presenting a challenge for healthcare professionals in delivering effective multidisciplinary patient care, as these lesions can spread to different parts of the organism and become systemic mycoses that must be monitored by several specialists depending on each case. The most common systemic mycoses are histoplasmosis and paracoccidioidomycosis, exhibiting a higher prevalence in men than women14.
Although fungal infections can be prevented with good oral, personal, and home hygiene habits, catching paracoccidioidomycosis does not depend on the patient. Such is the case of visiting endemic areas or doing fieldwork, agriculture, gardening, and transporting food with residues of contaminated soil, where the patient is exposed to inhaling conidia that can be found in the air after walking on contaminated soil or in caves, since inhalation is the most frequent form of contagion (6.
Histopathological studies are vital to confirm the fungus's presence upon suspicion. In this case, an incisional biopsy was performed in the anterior third of the right lateral border of the tongue, covering healthy and compromised tissue; the result was abundant fungal structures of variable shape and size, where yeasts with multiple gemmations were observed in the shape of a ship's rudder. Thus, a positive diagnosis of paracoccidioidomycosis could be affirmed12.
It is common to encounter oral and pulmonary lesions at the onset of this pathology due to the route of infection. However, it easily spreads to other parts of the body, including the skin, heart, brain, abdominal cavity, and other organs, complicating the treatment and resolution of the infection. Therefore, early detection and intervention are advisable. The quicker the infection is identified and treated, the fewer sequelae will manifest in the patient. Nevertheless, it is crucial to note that this type of mycosis demands careful attention as it involves a polymorphic fungus capable of adapting its shape based on environmental conditions, primarily influenced by food availability and temperature. Consequently, treatments are prolonged, spanning months or even years. Regular follow-ups are also essential to ensure the infection does not recur (15, in line with this case.
The preferred treatment for this mycosis typically involves oral administration of itraconazole at a maximum dose of 200 mg twice a day, known to exhibit a 90% therapeutic effectiveness. However, its success may be compromised in cases of intestinal involvement or mesenteric lymphatic blockage. Alternative treatments include trimethoprim/sulfamethoxazole at 8-10mg/TMP/day, ketoconazole at 5-7 mg/kg/day, and amphotericin B, reserved for severe and critical cases or when a non-enteral route of administration is necessary16. In this particular case, the initial treatment comprised itraconazole tablets at 200 mg every 12 hours, maintained for three months. Following an assessment by the infectious disease specialist, fluconazole tablets at 200 mg every 6 hours, trimethoprim-sulfamethoxazole at 160/800 mg every 24 hours, and intravenous amphotericin B deoxycholate at 50 mg every 24 hours were added for 4 weeks.
CONCLUSION
Paracoccidioidomycosis, although typically found in endemic areas with high humidity, proximity to rivers, and rural areas, can still affect individuals engaged in certain activities like gardening or professional agricultural work. Hence, taking a comprehensive health history and conducting a meticulous analysis of the clinical condition and the required tests is crucial. Early diagnosis is paramount for effective treatment and preserving the patient's life, preventing complications and the spread of the infection. This approach ensures appropriate treatment, managing the disease without leaving irreversible sequelae.
REFERENCES
1. Mutalik VS, Bissonnette C, Kalmar JR, McNamara KK. Unique Oral Presentations of Deep Fungal Infections: A Report of Four Cases. Head Neck Pathol. 2021;15(2):682-690. Doi:https://doi.org/10.1007/s12105-020-01217-0. [ Links ]
2. Drummond-Suinaga T., Gomez G., Blanco-Arandia P. Paracoccidioidomicosis juvenil diseminada y tuberculosis miliar: Reporte de un caso. Rev Panam Enf Inf. 2022; 5(1):e2. Disponible en: https://ojs2.utp.edu.co/index.php/panamericana/article/view/25086/16745. [ Links ]
3 3. Santos LA, Grisolia JC, Burger E, de Araujo Paula FB, Dias ALT, Malaquias LCC. Virulence factors of Paracoccidioides brasiliensis as therapeutic targets: a review. Antonie Van Leeuwenhoek. 2020;113(5):593-604. Doi: https://doi.org/10.1007/s10482-019-01382-5. [ Links ]
4. Ashraf N, Kubat RC, Poplin V, Adenis AA, Denning DW, Wright L, McCotter O, Schwartz IS, Jackson BR, Chiller T, Bahr NC. Re-drawing the Maps for Endemic Mycoses. Mycopathologia. 2020;185(5):843-865. Doi: https://doi.org/10.1007/s11046-020-00431-2. [ Links ]
5. Alvarado P, Teixeira MM, Cavallera E, Paes HC, Guerra G, Santander G, Merino-Alado R. Epidemiology of paracoccidioidomycosis in Venezuela: a retrospective study from 1954 to 2019. Mem Inst Oswaldo Cruz. 2021;8116:e210203. Doi: https://doi.org/10.1590/0074-02760210203. [ Links ]
6. Ramirez S., Ayala-Castillo Ml. Paracoccidioidomicosis con compromiso de sistema nervioso central. Acta Neurol Colomb. 2021;37(1Suppl 1): 106-111. Doi: https://doi.org/10.22379/24224022341. [ Links ]
7. Garropoli, Gastón J; Silva Balbuena, Micaela S; Cabrero, María del Carmen. Paracoccidioidomicosis: Reporte de un caso clínico con repercusión oral. Rev. Soc. Odontol. La Plata, 2022; XXXII(62):7-10. Disponible en: http://www.scielo.edu.uy/scielo.php?pid=S2393-67972019000300043&script=sci_arttext. [ Links ]
8. de Macedo PM, Teixeira MM, Barker BM, Zancopé-Oliveira RM, Almeida-Paes R, Francesconi do Valle AC. Clinical features and genetic background of the sympatric species Paracoccidioides brasiliensis and Paracoccidioides americana. PLoS Negl Trop Dis. 2019;13(4):e0007309. Doi: https://doi.org/10.1371/journal.pntd.0007309. [ Links ]
9. Tomo S, da Silva RL, Miyahara GI, Stefanini AR, Simonato LE. Diagnosis and treatment of primary paracoccidioidomycosis in oral mucosa. Dermatol Ther. 2020;33(3):e13314. Doi: https://doi.org/10.1111/dth.13314. [ Links ]
10. Wagner G, Moertl D, Glechner A, Mayr V, Klerings I, Zachariah C, Van den Nest M, Gartlehner G, Willinger B. Paracoccidioidomycosis Diagnosed in Europe-A Systematic Literature Review. J Fungi (Basel). 2021;7(2):157. Doi: https://doi.org/10.3390/jof7020157. [ Links ]
11. Ribeiro SM, Nunes TF, Cavalcante RS, Paniago AMM, Pereira BAS, Mendes RP. A scoping study of pulmonary paracoccidioidomycosis: severity classification based on radiographic and tomographic evaluation. J Venom Anim Toxins Incl Trop Dis. 2022;28:e20220053. Doi: https://doi.org/10.1590/1678-9199-jvatitd-2022-0053. [ Links ]
12. Berbeo-Velásquez Y., Vélez-López N., Vargas-Suaza, G., Ruiz-Restrepo J. Paracoccidioidomicosis crónica diseminada. Rev Asoc Colomb Dermatol. 2022;30(1):60-63. Doi: https://doi.org/10.29176/2590843X.1731. [ Links ]
13. Barrios OI, Anido EV, Morera PM. Declaración de Helsinki: cambios y exégesis. Revista Cubana de Salud Pública. 2016;42(1):132-142. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=64992. [ Links ]
14. Lemus-Espinoza D, Teresa Maniscalchi MB. Micosis sistémicas en pacientes del estado Anzoátegui, Venezuela, 2009-2018. Revista de la Sociedad Venezolana de Microbiología, 2021;41:27-32. Disponible en: https://www.researchgate.net/profile/Maria-Maniscalchi/publication/362452087_Micosis_sistemicas_en_pacientes_del_estado_Anzoategui_Venezuela_2009-2018/links/62ea8a374532247693780f65/Micosis-sistemicas-en-pacientes-del-estado-Anzoategui-Venezuela-2009-2018.pdf [ Links ]
15. Costa A., Dos Santos V., Leite M., de Farias F. A Brazilian male with typical oral and pulmonary paracoccidioidomycosis. Med J Islam Repub Iran. 2019; 33:145. DOI: 10.34171/mjiri.33.145. [ Links ]
16. Dutra LM, Silva THM, Falqueto A, Peçanha PM, Souza LRM, Gonçalves SS, Velloso TRG. Oral paracoccidioidomycosis in a single-center retrospective analysis from a Brazilian southeastern population. J Infect Public Health. 2018;11(4):530-533. DOI: 10.1016/j.jiph.2017.10.009. [ Links ]
Conflict of Interest Statement The authors have no conflict of interest in the publication of the article.
Authorship contribution note 1.Study concept and design 2.Data acquisition 3.Data analysis 4.Discussion of results 5.Manuscript drafting 6. Approval of the final version of the manuscript ●MC has contributed in 1, 5. ●ET has contributed in 1,4,5,6. ●SU has contributed in 2,3,4,6. ●SJ has contributed in 2,4,6.
Received: May 10, 2023; Accepted: June 28, 2023











 texto em
texto em