Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.25 no.42 Montevideo 2023 Epub 01-Dez-2023
https://doi.org/10.22592/ode2023n42e415
Reporte de caso
Molar incisor hypomineralization in a pediatric patient with distal renal tubular acidosis. Case report. Control and monitoring for 14 years.
1Departamento de Atención integral al niño y el adolescente. Odontopediatría. Facultad de Odontología. Universidad de Carabobo. Venezuela.
2Departamento de Estomatoquirúrgica. Radiología Dentomaxilofacial. Facultad de Odontología. Universidad de Carabobo. Venezuela. mairaquevedo@gmail.com
Introduction:
molar incisor hypomineralization is a systemic developmental defect that affects one or more permanent first molars, is frequently associated with permanent incisors, of multifactorial etiology and with various treatment options.
Objective:
the case of a patient who presents molar incisor hypomineralization in his first permanent molars with a history of having suffered from distal renal tubular acidosis is presented, this entity can cause enamel defects
Case report:
7-year-old male diagnosed with distal tubular acidosis at 4 months of age, at the time of the consultation he had already passed. In his first permanent molars, lesions suggestive of molar incisor hypomineralization were observed. It is evaluated clinically and radiographically. Glass ionomer restorations were performed, reviewed at six-monthly controls, and at 10 years it was decided to place composite resins on the affected molars. Periodic controls are indicated, which he regularly attends for 14 years.
Conclusion:
early identification of molar incisor hypomineralization will allow the application of preventive measures to ensure the permanence of affected teeth in the mouth. It is important to strengthen hygienic practices, especially on affected surfaces, concomitantly with the application of restorative materials.
Key words: Hypomineralization of teeth; Renal Tubular Acidosis; child
Introducción:
la hipomineralización incisivo molar es un defecto sistémico del desarrollo que afecta a uno o más primeros molares permanentes, se asocia con frecuencia a los incisivos permanentes, de etiología multifactorial y con diversas opciones de tratamiento.
Objetivo:
se presenta el caso de un paciente que presenta hipomineralización incisivo molar en sus primeros molares permanentes con antecedentes de haber padecido de acidosis tubular renal distal, dicha entidad puede ocasionar defectos en el esmalte.
Reporte del caso:
masculino de 7 años de edad diagnosticado con acidosis tubular distal a los 4 meses de edad, al momento de la consulta ya superado. En sus primeros molares permanentes se observan lesiones sugestivas de hipomineralización incisivo molar. Se evalúa clínica y radiográficamente. Se le realizan restauraciones con vidrio ionomérico revisadas en controles semestrales y a los 10 años se decide colocar resinas compuestas en los molares afectados. Se indican controles periódicos a los cuales asiste regularmente por 14 años.
Conclusión:
la identificación temprana de la Hipomineralización incisivo molar permitirá la aplicación de medidas preventivas para asegurar la permanencia de los dientes afectados en boca. Es Importante afianzar las prácticas higiénicas especialmente en las superficies afectadas, concomitantemente con la aplicación de materiales restauradores.
Palabras clave: Hipomineralización de los dientes; Acidosis Renal Tubular; niño
Introdução:
a hipomineralização molar incisivo é um defeito sistémico do desenvolvimento que afeta um ou mais primeiros molares permanentes, está frequentemente associada a incisivos permanentes, de etiologia multifatorial e com várias opções de tratamento.
Objetivo:
é apresentado o caso de um paciente que apresenta hipomineralização molar incisivo em seus primeiros molares permanentes com histórico de ter sofrido acidose tubular renal distal, esta entidade pode causar defeitos de esmalte.
Relato de caso:
menino de 7 anos de idade diagnosticado com acidose tubular distal aos 4 meses de idade, à época da consulta já ultrapassado. Em seus primeiros molares permanentes, foram observadas lesões sugestivas de hipomineralização molar incisivo. É avaliado clínica e radiograficamente. Restaurações de ionômero de vidro foram realizadas, revisadas em controles semestrais, e aos 10 anos foi decidido colocar resinas compostas nos molares afetados. São indicados controles periódicos, que frequenta regularmente há 14 anos.
Conclusão:
a identificação precoce da hipomineralização molar incisivo permitirá a aplicação de medidas preventivas para garantir a permanência dos dentes acometidos na boca. É importante reforçar as práticas de higiene, principalmente nas superfícies afetadas, então com a aplicação de materiais restauradores.
Palavras-chave: Hipomineralização de dentes; Acidose Tubular Renal; criança
INTRODUCTION
The formation process of tooth enamel, or amelogenesis, relies on the contribution of many genes 1. Molar incisor hypomineralization (MIH) is a systemic developmental defect that affects one or more first permanent molars and is frequently associated with permanent incisors 2. Clinically, it is characterized by well-defined opacities with variable size and discolorations ranging from white to yellow-brown 3. They are considered enamel qualitative defects. Molecularly, a high number of proteins is observed, such as serum albumin, type I collagen among others, and it is suggested that these proteins inhibit the growth of hydroxyapatite crystals and enzymatic activity during enamel maturation, resulting in a reduced mineral content of the enamel 4,5.
It usually affects the first permanent molars and incisors, hence its name. The clinical implications are significant for both patients and the health care team. As for prevalence, Rao et al. indicate that it is variable, depending on the population group. In Brazil, a study carried out in Rio de Janeiro reported a 40.2%, whereas in Germany and Bulgaria it was close to 2.4%. China and the United States have the highest prevalence rates. In general, the estimated rate is 14.2% 6; Lopes et al. argue that this wide range of results is mainly due to the lack of population standardization by clinicians and researchers 2.
Enamel formation takes approximately 1,000 days, two thirds of which is devoted to the maturation stage of amelogenesis; therefore, the first year of life is the most critical period for the appearance of enamel defects in first molars and permanent incisors, since ameloblasts are very sensitive to various environmental disturbances during this period 7.
Regarding MIH pathogenesis, it was suggested that its origin could be related to systemic or environmental disturbances during the maturation stage of amelogenesis in the first molars and incisors (8. Various etiological hypotheses have been presented, such as pre or perinatal problems, postnatal childhood diseases, environmental factors, use of medications (e.g., antibiotics such as amoxicillin and penicillin or corticosteroids and bronchodilators used for the treatment of asthma) and genetic influences7-9. However, in Garot et al.'s systematic review, it is emphasized that the real etiology of MIH has not yet been defined, concluding that it likely has a multifactorial etiology 10-12.
In turn, mineral metabolism alterations in renal tubules could be associated with dental enamel disorders 11,13. One of these pathologies is renal tubular acidosis, which is characterized by abnormalities in the transport mechanism of the distal and/or proximal tubules of the kidneys leading to a decrease in HCO3 reabsorption or H+ excretion, resulting in metabolic acidosis 14. Specifically, distal renal tubular acidosis is a rare disease caused by failure of the normal urine acidification process at the distal and collecting tubular level. Clinical manifestations among these patients are common, although they present some particularities depending on the causal gene 15). These electrolyte imbalances can affect the amelogenesis mechanism and craniofacial development. Enamel hypomaturation has been associated with distal renal tubular acidosis of unknown cause and in severe cases patients may develop amelogenesis imperfecta 16,17.
For the diagnosis of MIH, both the location and the extent of the defect in the enamel can serve as a biological marker 4. The location is related to the period in which the defect occurred and the extension to the time that the damage occurred. Thus, defects in the cusp tip show that the interference in the enamel formation occurred early; if the defect is mild, it indicates that the damage was acute 18. Therefore, the extent of the lesion reflects the degree of exposure to the damage that led to the defect, which can be for a defined or long-term period 18.
Clinically, given the poor quality of the enamel, there may be increased sensitivity of the affected teeth 19, causing children to refuse tooth brushing and dental treatment 5. Since the enamel is soft and porous in texture, the most severely affected teeth may rupture after eruption, which can lead to destruction of the crown 20.
Another important aspect to consider is the difficulty of adhering restorative materials to hypomineralized enamel, which poses a challenge and leads to frequent retreatments, as well as atypical restorations that often result in tooth loss 20.
This case describes the enamel changes observed in the first permanent molars of a 7-year-old patient diagnosed with distal renal tubular acidosis at the age of 4 months. The clinical and radiographic findings, diagnostic conclusions, and treatment decisions made during routine check-ups and the most recent visit, which occurred after 11 years of composite resin restorations, are presented.
Case report
A 7-year-old male patient from Valencia, Carabobo state, Venezuela, attended the pediatric and adolescent care clinic at the Faculty of Dentistry of Carabobo University, accompanied by his mother, who stated that "the child's teeth get fractured and hurt." During anamnesis, the mother explained that the child suffered from distal renal tubular acidosis diagnosed at the age of 4 months, which manifested as urolithiasis. He received treatment from a pediatric nephrologist until he was 22 months old, attending regular check-ups with his treating physician.
In the initial physical examination at the age of 7, he presented brachycephalic facial features, with sagittal symmetry, hair implantation and normal pinnae, lip incompetence with lower lip hypotonia, height in the 25th percentile, weight in the 50th percentile.
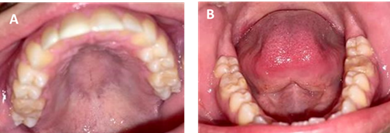
The intraoral clinical examination showed a class III molar relationship, a right posterior crossbite, an edge-to-edge bite, and a permanent supernumerary tooth in the lower incisor region in giroversion (figure 1 ABC). The floor of the mouth, palate, and gums showed no apparent lesions. Dental units (DU) 1.6 and 2.6 exhibited morphological changes with white and yellow-brown opacities in the middle third and on the occlusal surface with diffuse edges, along with post-eruptive fractures in the enamel. Dental units 3.6 and 4.6 had cavity preparations without restorative material on the occlusal-lingual surfaces, which were performed in a private practice around two months ago but became dislodged (figure 2 AB). During thermal tests, the patient displayed sensitivity to cold in DU 1.6, 2.6, 3.6, and 4.6. Dental impressions and a radiographic study were indicated.
There is evidence of mixed dentition in the eruption process, with presence of the permanent teeth germs in their entirety and a supernumerary tooth in the lower incisor area. In the first permanent molars of the maxilla and mandible, enamel density resembling that of dentin is observed (figure 3).
Through clinical and radiographic examination, MIH in the first permanent molars and the presence of a supernumerary in the mandibular incisor region were concluded as a diagnostic impression. The indicated treatment plan is prophylaxis, restoration with ionomeric glass, sealants of pits and fissures in DU 1.6, 2.6, 3.6, 4.6 and topical application of fluoride. Periodic six-monthly check-ups were indicated at the beginning of the treatment to review the restorations for a period of three years. At the age of 10, it was decided to place composite resins. From that date on, visits to the dentist were made annually. Currently, at age 21, the restorations with composite resins that were placed 11 years ago are still in the mouth. They show changes in color and slight wear of the occlusal surface, but the patient does not report any symptoms (figure 4).
DISCUSSION
Alterations in the neonatal period are considered important risk factors for the development of enamel defects in the first permanent molars, mostly affecting the occlusal surfaces of the molars 8. MIH has been related to episodes triggered before, during and/or after birth. Prenatal events include maternal fever, viral infections in the last month of pregnancy and prolonged antibiotic medication; perinatal events include prematurity, low birth weight, among others 9. As for postnatal risk factors that occur mainly during the first year of life, high fevers, respiratory problems, otitis and alterations in calcium-phosphate metabolism can be listed 5. The most critical period for the development of enamel defects in the first permanent molars and incisors is during the first year of life 7. In this patient, MIH could be related to the child's distal tubular acidosis and hypercalciuria, since his renal problem was clinically manifested when he was 4 months old. In the medical history reported by his mother, there were no reports of prolonged antibiotic therapy nor other conditions suffered during pregnancy.
Clinically in MIH, lesions range from demarcated yellowish-white or brownish-yellow opacities to severe hypomineralization with enamel rupture and pronounced sensitivity to thermal changes and may manifest painful symptomatology 3. In more severe cases, posteruptive fractures of this weaker enamel can be observed, due to its greater porosity, which causes a decrease in its mechanical properties, turning it brittle and susceptible to fracture under normal masticatory forces 19. In this case, the lesions were yellowish-brown and the patient manifested sensitivity to cold. Just like the posteruptive fractures referred by the mother in the anamnesis. Regarding prevalence by sex, it is higher in males, a situation consistent with this case, as well as the teeth affected by MIH, which are mostly molars, as observed in the patient whose first four permanent molars were affected.
Differential diagnosis with enamel hypoplasias, fluorosis, and amelogenesis imperfecta has to be made. In amelogenesis, almost all teeth are affected, and there is always a correlated hereditary pattern 16. Hypoplasia occurs when the ameloblast disrupts the secretion of the enamel matrix, resulting in a quantitative defect. As a consequence, the enamel is thin, and the occlusal surfaces of the posterior teeth are relatively soft with low cusps. Their color can vary from very light to grayish white, yellow, or brown 21.
MIH is a quality defect, which is characterized by enamel demarcated opacities (9. Also, the loss of tissue margin structure is rough and irregular. Generally, the lesions are located in the occlusal two-thirds of the crown and decrease in severity from the occlusal to gingival region 21. This pattern of involvement was observed in the patient, as lesions were absent at the gingival margin. Another important aspect is that a higher severity of lesions at the molar level increases the probability of finding some manifestation in the incisors 21. In this patient, lesions were observed affecting all the first permanent molars, but they were not visualized in the erupted lower central incisors. Once the upper incisors erupted, no signs of MIH were observed in the controls.
From a radiographic standpoint, enamel hypomineralization and hypoplasia are difficult to differentiate when enamel fractures have already occurred. Defects during the calcification/maturation stages generally lead to normal enamel volumes with insufficient mineralization (hypomineralization) and, consequently, altered translucency 9. In the case shown in the panoramic X-ray, decreased enamel mineral content is observed as it presents dentin-like radiodensity, due to reduced calcium and phosphate content. Patients with enamel hypoplasia can be identified in several teeth, unlike MIH, which is mainly observed in the first molars and incisors, hence its name 5,6.
The general clinical examination revealed that the patient under study exhibited growth retardation, with his height falling within the 25th percentile. Patients who experience kidney issues from an early age often exhibit growth retardation. This growth failure becomes increasingly apparent as the child ages and, in some cases, may be the only clinical abnormality. Costa et al., in their findings, suggested that renal tubular acidosis could serve as a predictor of enamel issues in permanent dentition 14. While the literature reviewed mentions enamel alterations in patients with distal renal tubular acidosis (16,17, it does not specifically describe patients with MIH and this condition.
Restorative treatment poses a challenge in cases of MIH. One alternative approach involves the topical application of fluoride varnish with frequent 3 to 6-month check-up intervals and preventive measures. This allows the dentist to closely monitor the affected teeth 22. The patient received topical fluoride applications during the initial appointments to promote remineralization and reduce sensitivity. Another important consideration is that MIH enamel lacks the strong structural support found in healthy enamel. Furthermore, marginal gaps in restorations are common due to inadequate adhesion between the tooth substrate and the restorative material, a result of the hypomineralization 23. This suggests that restoring residual MIH enamel adjacent to cavities may require the use of fracture-resistant and flexurally strong restorative materials 22.
Glass ionomer and amalgam cements have been used with caution. Adhesive restorations require acid etching, and their use is restricted depending on the extent of dental unit involvement 21. The mother mentioned that she first sought consultation when the child reported sensitivity, and the dentist placed resins in DU 3.6 and 4.6, which remained in the mouth for only 2 months. This information aligns with Martignon et al.'s findings, as they reported that teeth affected by MIH require nearly 10 times more intervention than the teeth of unaffected individuals at the age of 9. By the age of 18, affected molars had been treated 4.2 times more frequently than control patients without this condition 21.
At the age of 10, it was decided to use composite resins with absolute isolation, and the patient has since been under the care of their treating dentist. Over this 11-year period, there have been gradual changes in the color of the restorations, but no sensitivity nor discomfort has been reported in any of the units. According to the literature, the use of resins is a viable option with high success rates when placed under isolation with a rubber dam to ensure proper humidity control (22.
CONCLUSIONS
Early identification of MIH enables the application of preventive measures to ensure the permanence of affected teeth in the oral cavity and to strengthen hygienic practices, particularly on the affected surfaces, concomitantly with the application of necessary restorative materials, minimally invasive treatment, and a continuous monitoring program. Therefore, adopting a preventive approach from the beginning of treatment is essential.
Knowledge of the patient's medical history is crucial. In this case, distal renal tubular acidosis is of particular significance due to its implications for dental enamel, as it provides valuable information for diagnosis, thus facilitating appropriate treatment.
The choice of the most suitable treatment option should be made on an individual basis, considering the severity of the lesions, the symptoms of the affected tooth, the patient's dental age, and their short- and long-term expectations.
REFERENCES
1. Wright JT, Carrion IA, Morris C. The molecular basis of hereditary enamel defects in humans. J Dent Res. 2015;94(1):52-61. [ Links ]
2. Lopes LB, Machado V, Mascarenhas P, Mendes JJ, Botelho J. The prevalence of molar-incisor hypomineralization: a systematic review and meta-analysis. Sci Rep. 2021;11(1):22405. doi:10.1038/s41598-021-01541-7 [ Links ]
3. Bandeira Lopes L, Machado V, Botelho J, Haubek D. Molar-incisor hypomineralization: an umbrella review. Acta Odontol Scand. 2021;79(5):359-69. doi:10.1080/00016357.2020.1863461 [ Links ]
4. Elhennawy K, Manton DJ, Crombie F, Zaslansky P, Radlanski RJ, Jost-Brinkmann PG, Schwendicke F. Structural, mechanical and chemical evaluation of molar-incisor hypomineralizationaffected enamel: a systematic review. Arch Oral Biol. 2017; 83: 272-81 [ Links ]
5. Almulhim B. Molar and Incisor Hypomineralization. JNMA J Nepal Med Assoc. 2021;59(235):295-302. doi:10.31729/jnma.6343. [ Links ]
6. Rao MH, Aluru SC, Jayam C, Bandlapalli A, Patel N. Molar Incisor Hypomineralization. J Contemp Dent Pract. 2016;17(7):609-13. [ Links ]
7. Padavala S, Sukumaran G. Molar Incisor Hypomineralization and Its Prevalence. Contemp Clin Dent. 2018;9(Suppl 2):S246-S250. doi:10.4103/ccd.ccd_161_18 [ Links ]
8. Silva MJ, Scurrah KJ, Craig JM, Manton DJ, Kilpatrick N. Etiology of molar incisor hypomineralization - A systematic review. Community Dent Oral Epidemiol. 2016;44(4):342-353. doi:10.1111/cdoe.12229 [ Links ]
9. Sundfeld D, da Silva L, Kluppel OJ, Santin GC de Oliveira RC, Pacheco RR, Pini NI. Molar Incisor Hypomineralization: Etiology, Clinical Aspects, and a Restorative Treatment Case Report. Oper Dent. 2020;45(4):343-51. doi:10.2341/19-138-T [ Links ]
10. Garot E, Rouas P, Somani C, Taylor GD, Wong F, Lygidakis NA. An update of the aetiological factors involved in molar incisor hypomineralization (MIH): a systematic review and meta-analysis. Eur Arch Paediatr Dent. 2022 Feb;23(1):23-38. [ Links ]
11. Bagattoni S, Carli E, Gatto MR, Gasperoni I, Piana G, Lardani L. Predisposing factors involved in the aetiology of Molar Incisor Hypomineralization: a case-control study. Eur J Paediatr Dent. 2022;23(2):116-20. doi:10.23804/ejpd.2022.23.02.13. [ Links ]
12. Lacruz RS, Habelitz S, Wright JT, Paine ML. Dental Enamel Formation and Implications for Oral Health and Disease. Physiol Rev. 2017; 97(3): 939-993. doi:10.1152/physrev.00030.2016 [ Links ]
13. Ferreira SB, de Aquino SN, Pereira PC, Simões e Silva AC, Martelli-Júnior H. Dental findings in Brazilian patients with Fanconi syndrome. Int J Paediatr Dent. 2016;26(1):77-80. doi:10.1111/ipd.12183 [ Links ]
14. Costa SA, Souza SF, Nunes AM. Oral manifestations of renal tubular acidosis associated with secondary rickets: case report. J Bras Nefrol. 2019;41(3):433-5. doi:10.1590/2175-8239-jbn-2018-0105 [ Links ]
15. Gómez-Conde S, García-Castaño A, Aguirre M, Herrero M, Gondra L, Castaño L, Madariaga, L. Acidosis tubular renal distal hereditaria: correlación genotípica, evolución a largo plazo y nuevas perspectivas terapéuticas. Nefrología. 2021;41(4):383-90 [ Links ]
16. Misgar RA, Hassan Z, Wani AI, Bashir MI. Amelogenesis imperfecta with distal renal tubular acidosis: a novel syndrome? Indian J Nephrol. 2017;27(3):225-7. [ Links ]
17. Ravi P, Ekambaranath TS, Arasi SE, Fernando E. 2013. Distal renal tubular acidosis and amelogenesis imperfecta: a rare association. Indian J Nephrol. 23(6):452-455. (PMC free article) (PubMed) [ Links ]
18. Dourado DG, Lima CCB, Silva RNC, Tajra FS, Moura MS, Lopes TSP, De Deus Moura LF, de Lima MD. Molar-incisor hypomineralization in quilombola children and adolescents: A study of prevalence and associated factors. J Public Health Dent. 2021;81(3):178-187. doi:10.1111/jphd.12429 [ Links ]
19. Corral C, Rodríguez H, Cabello R, Bersezio C, Cordeiro R, et al. Impacto de la hipomineralización incisivo molar en la experiencia de caries en escolares de 6-12 años en Santiago, Chile. Rev Clin Periodoncia Implantol Rehabil Oral. 2016;9(3):277-283. doi: 10.1016/j.piro.2016.10.003 [ Links ]
20. Buchgraber B, Kqiku L, Ebeleseder KA. Molar incisor hypomineralization: proportion and severity in primary public school children in Graz, Austria. Clin Oral Investig. 2018;22(2):757-62. doi:10.1007/s00784-017-2150-y [ Links ]
21. Martignon S, Bartlett D, Manton DJ, Martinez-Mier EA, Splieth C, Avila V. Epidemiology of Erosive Tooth Wear, Dental Fluorosis and Molar Incisor Hypomineralization in the American Continent. Caries Res. 2021;55(1):1-11. doi:10.1159/000512483 [ Links ]
22. Lygidakis NA, Garot E, Somani C, Taylor GD, Rouas P, Wong FSL. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralization (MIH): an updated European Academy of Paediatric Dentistry policy document. Eur Arch Paediatr Dent. 2022;23(1):3-21. doi:10.1007/s40368-021. [ Links ]
23. Romo-Pérez C, Lobo-Cortés L, Morales-Rojas MJ, San Martín-López AL, Ramírez-Vera KG. Efecto de la hipomineralización incisivo molar en la calidad de vida relacionada con la salud bucal de niños y adolescentes: una revisión sistemática. Rev Cient Odontol (Lima). 2022;10(4): e130. doi: 10.21142/2523-2754-1004-2022-130 [ Links ]
Conflict of Interest Statement: The authors have no conflict of interest in the publication of the article
Authorship contribution note: 1.Study conception 2.Data acquisition 3.Data analysis 4.Discussion 5.Manuscript drafting and editing 6.Approval of the final manuscript version IL has contributed in: 1, 2, 3, 4, 5, 6. MQ has contributed in: 1, 3, 4, 5, 6. HJ has contributed in: 3, 4, 5, 6.
Received: April 24, 2023; Accepted: June 16, 2023











 texto em
texto em