Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.25 no.42 Montevideo 2023 Epub 01-Dez-2023
https://doi.org/10.22592/ode2023n42e328
Actualizaciones
Lasertherapy as an adjuvant to the treatment of grade II furcation involvements
1Departamento de Periodoncia, Universidad Católica del Uruguay
2Hemato-oncología, Fundación Pérez Scremini, Hospital Pereira Rosell
Objective:
to evaluate the evidence of the efficacy of the adjuvant use of laser in the surgical treatment of grade II furcation lesions and to demonstrate the clinical importance of the findings for decision making.
Materials and methods:
a manual bibliographic search was carried out where the following databases were consulted: PORTAL TIMBO FOCO, PUBMED, SciELO, BVS and GOOGLE SCHOOL. This search was restricted to the last 15 years and the selected articles are in English.
Results:
105 articles that addressed the subject were selected and the search was completed by searching and reading the referenced bibliography in those articles.
Conclusions:
Low-power laser, both for biostimulation and as an anti-inflammatory has so far only shown positive short-term results as an adjunct to regenerative periodontal treatment in grade II furcation lesions. However, its long-term results are not clear due to methodological weaknesses and the insufficient number of existing studies. On the other hand, photodynamic therapy could be an alternative to control bone loss in furcation lesions caused by periodontitis. However, more studies are needed to elucidate the action of photodynamic therapy and photobiomodulation as adjuvants in the treatment of furcation lesions.
Keywords: Furcation Lesions; Periodontal Treatment; Periodontitis; Photochemotherapy; Photodynamic Therapy
Objetivo:
evaluar la evidencia del láser como coadyuvante en el tratamiento quirúrgico de lesiones de furca grado II y reflejar la importancia clínica de los hallazgos para la toma de decisiones.
Materiales y métodos:
se realizó una búsqueda bibliográfica manual, se consultaron las siguientes bases de datos: PORTAL TIMBO FOCO, PUBMED, BVS, SciELO y GOOGLE SCHOOLAR. Esta búsqueda fue restringida a los últimos 15 años y los artículos seleccionados están en inglés.
Resultados:
Se seleccionaron 105 artículos que abordan la temática y se completó la búsqueda con el rastreo y la lectura de la bibliografía referenciada en esos artículos.
Conclusiones:
El láser de baja potencia tanto para la bioestimulación así como su efecto anti-inflamatorio, solo ha mostrado hasta ahora resultados positivos a corto plazo como coadyuvante del tratamiento periodontal regenerativo en lesiones de furca grado II. Sin embargo, sus resultados a largo plazo no son claros debido a la debilidad metodológica y al número insuficente de estudios existentes. Por otro lado, la terapia fotodinámica podría ser una alternativa para el control de pérdida ósea en lesiones de furca causadas por periodontitis. Por lo tanto, hacen falta más estudios para dilucidar la acción del la terapia fotodinámica y de la fotobiomodulación coadyuvantes del tratamiento de las lesiones de furca.
Palabras clave: Fotoquimioterapia; Lesiones de Furca; Periodontitis; Terapia Fotodinámica; Tratamiento Periodontal
Objetivo:
avaliar a evidência do laser como adjuvante no tratamento cirúrgico das lesões de furca grau II e refletir a importância clínica dos achados para a tomada de decisão.
Materiais e métodos:
foi realizada busca bibliográfica manual, consultadas as seguintes bases de dados: PORTAL TIMBO FOCO, PUBMED, BVS, SciELO e GOOGLE SCHOOL. Esta busca foi restrita aos últimos 15 anos e os artigos selecionados estão no idioma inglês.
Resultados:
foram selecionados 105 artigos que abordam o assunto e a busca foi concluída por meio de busca e leitura da bibliografia referenciada nesses artigos.
Conclusões:
O laser de baixa potência, tanto para a bioestimulação como para o seu efeito anti-inflamatório, apenas apresentou resultados positivos a curto prazo como adjuvante do tratamento periodontal regenerativo em lesões de furca grau II. No entanto, seus resultados a longo prazo não são claros devido a deficiências metodológicas e número insuficiente de estudos existentes. Por outro lado, a terapia fotodinâmica pode ser uma alternativa para controlar a perda óssea em lesões de furca causadas por periodontite. Portanto, mais estudos são necessários para elucidar a ação da Terapia Fotodinâmica e da fotobiomodulação como adjuvantes no tratamento da lesões de furca.
Palavras chave: Fotoquimioterapia; Lesões de Furca; Periodontite; Terapia Fotodinâmica; Tratamento Periodontal
Introduction
Periodontitis is a chronic disease that leads to tissue destruction1. Periodontal treatment involves a first stage that halts progression by reducing pathogenic microorganisms and eliminating the inflammatory process1. Conventional and resective therapies can slow disease progression but have not been shown to eliminate microorganisms located in soft tissues or hard-to-reach areas such as Furcation Involvements (FI)2-4.
Guided tissue regeneration (GTR) has been proposed as an effective method for treating anatomical defects resulting from periodontitis, including Grade II FI5.
Nowadays, there is a consensus that Guided Tissue Regeneration (GTR) procedures in mandibular Grade II FI lead to significant gains in attachment levels, both horizontally and vertically6,7. Although the combination of xenografts with collagen membranes has demonstrated positive clinical outcomes in furcation involvement, the concept of periodontal regeneration is intricate and demands complex coordination of cellular activities. Consequently, there are notable variations in its clinical predictability8.
Despite the potential clinical and biological benefits of regenerative therapies in the treatment of FI and intraosseous defects, combined modalities of treatment with GTR are being investigated for better and more accurate results. One of them is the combination of GTR with a low-level laser8.
It has been suggested that low-level laser can increase the amount of adenosine triphosphate (ATP) and simplify angiogenesis and collagen synthesis, as well as alter the behavior of cellular activity9. Laser biostimulation has also been reported to induce metabolic changes, resulting in faster cell division, increased proliferation, fibroblast migration and matrix production. It may also be effective in the repair and regeneration of bone metabolism10-12.
Low-level laser is used in periodontics for bone surgery, intraosseous defects, gingivectomies, flaps, and scaling and root planing (SRP), but virtually no studies have been found on the clinical or biochemical effect of low-level laser on GTR-treated FI1.
On the other hand, recent evidence-based scientific information identified potential applications of infrared laser tools for the treatment of periodontitis13.
Lasers have been shown to promote periodontal wound healing and regeneration. This is generally achieved by thorough debridement and decontamination of diseased tissues and by modulating or activating cellular metabolism in surrounding tissues14. During the last decade, photodynamic therapy (PDT) has also been used to reduce or eliminate periodontopathogenic bacteria as an adjunct to mechanical debridement in patients with periodontitis14.
PDT principles involve the use of a non-toxic light-sensitive dye called a photosensitizer (PS) combined with harmless (low-energy) visible light of an appropriate wavelength to match the absorption spectrum of the PS15. This procedure stimulates the dye to form singlet oxygen-free radicals that act as toxic agents to the bacteria/cell16. An increasing number of studies are examining the clinical efficacy of PDT when used as an adjunct to conventional surgical and non-surgical treatments for patients with periodontitis16. The objective of this review is to assess the scientific quality of evidence regarding laser treatment as an adjunct to mechanical instrumentation in Grade II furcation involvements, aiming to assist clinicians in decision-making.
Materials and Methods
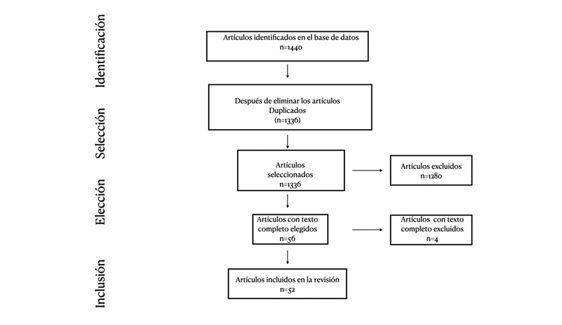
In the preparation of this literature review, the databases PORTAL TIMBO FOCO, PUBMED, BVS, SciELO, and GOOGLE SCHOLAR were consulted. The following MeSH descriptors were employed in English: Photochemotherapy, Photodynamic Therapy, Furcation involvement, Periodontitis, Periodontal treatment, along with their corresponding Spanish terms for the search. Boolean operators were not utilized; instead, the search was conducted for each of the mentioned MeSH descriptors. The search was restricted to the past 15 years, with the exception of certain articles used for background information. A total of 105 articles addressing the topic were selected, and the search was supplemented by reviewing the bibliographies referenced in those articles. (Figure 1)
Laser Foundations in the Treatment of Grade II Furcations: Photobiomodulation
There is a consensus that, in mandibular Grade II FI, as well as in certain intraosseous defects, GTR procedures have resulted in significant clinical attachment gains, both horizontally and vertically6.
There are some limitations to clinical, histological, and radiographic evaluation after GTR treatment6. The response of periodontal tissues to this intervention is crucial and can be assessed through biochemical measurements, such as levels and composition of gingival crevicular fluid1. Particularly in lower molars, the access to the furcation is often smaller than the diameter of the standard Gracey curette17.
To achieve periodontal regeneration, attachment to the cementum is necessary, requiring the prevention of epithelial cell migration, which is typically accomplished through the use of collagen membranes18.
Most studies involving GTR have indicated that the depth and width of the intraosseous components of the defect influence the extent of clinical and bone attachment increase19. Specifically, when GTR is applied to defects with 3, 2, and 1 intraosseous walls, it results in 95%, 82%, and 39% bone fill, respectively20.
While some similar studies have demonstrated that the deeper the defect, the greater the attachment increase and bone repair19, others have shown that the wider the defect, the lower the clinical improvement20,21.
This substantially lower increase in one-wall defects may be explained by the reduced number of progenitor cells available for repopulation in the wound area or the difficulty in placing membranes in the correct position, maintaining the required space between the membrane and the remnant bone19.
In the treatment of FI, the GTR predictability also improves if the defect presents a deep vertical component and maintains the interproximal bone level close to the cemento-enamel junction (CEJ), facilitating membrane retention in the correct position and allowing coronal repositioning of the flap with total membrane coverage19.
The horizontal depth of FI also influences clinical outcomes, and in most studies of Grade II FI, the preoperative probing depth (PD) correlates with the magnitude of clinical attachment gain and bone repair achieved after one year19.
Treatment predictability is enhanced when complete debridement of the exposed root surface in the FI area is achieved19. Factors affecting the operator's ability to debride in this area, such as root proximity or deformities, could influence the results of guided tissue regeneration (GTR)19. Additionally, lower molar roots often present deep concavities and the presence of enamel pearls that may hinder proper debridement 19. The anatomy of the upper molars is even less favorable, which may contribute to less predictable results in these teeth17.
It has been demonstrated that the dimension of the root trunk is correlated with the presence of FI17. This dimension may influence the selection of a better therapeutic approach; a longer root trunk facilitates the placement of the barrier membrane under the cementoenamel junction (CEJ) to achieve complete coverage of the FI and flap repositioning by fully covering the membrane19.
Gingival phenotype has also been linked to the amount of recession obtained after GTR in FI22. Anderegg et al. demonstrated that sites with a thicker phenotype exhibited less gingival recession compared to thinner phenotypes22. A thicker mucoperiosteal flap has more resistance to ischemia when placed on a non-vascularized surface, such as the membrane19.
Moreover, repositioning the flap with the aim of completely covering the membrane can apply excessive tension and induce ischemia. In the presence of thin gingiva, these factors can lead to increased recession, thus reducing attachment gain levels19.
Other factors that may influence the outcome of GTR are related to the surgical procedure, as it requires certain principles and care described for the treatment of intraosseous defects 23. These include flap design, proper preparation of the root surface, correct membrane placement, good wound closure, and optimal postoperative care5.
The most common complications that worsen treatment outcomes are exposure of biomaterials and loss of the interdental papilla. These complications are associated with surgical techniques requiring a papillary incision24.
To avoid such complications, various approaches have been proposed, including the use of enamel-derived proteins (EMDOGAIN®), alternative flap designs (papilla preservation techniques), and minimally-invasive techniques24.
Tooth mobility has long been considered an important factor for periodontal regeneration25. A multivariate analysis of a multicenter controlled clinical trial demonstrated that increased tooth mobility is negatively associated with clinical outcomes of regeneration25.
A recent secondary analysis of three previously reported trials evaluated regenerative outcomes of mobile teeth and concluded that teeth with an initial mobility of < 1 mm horizontally could be successfully treated by periodontal regeneration, whereas severe and uncontrolled tooth mobility (Miller grade II) may affect regenerative outcomes and require splinting for regeneration25.
Based on these results, it can be concluded that GTR treatment achieves the most significant and predictable results in deep and narrow intraosseous defects in vital or successfully endodontically treated teeth25. The influence of defect anatomy seems to be reduced to some extent when a more stable flap design is applied25.
A clinical trial, published in 2016, assessed 33 grade II FIs in patients with chronic periodontitis. Among them, 17 received GTR along with low-level laser, while 16 underwent GTR alone1. Long-term results revealed that both GTR alone and GTR plus low-level laser led to significant improvements in the treatment of grade II FIs, with reductions in PD and horizontal PD (p=0.0001) and attachment gain (p=0.0001) compared to baseline1. The study evaluated clinical and biochemical parameters to observe the effect of low-level laser as an adjunct for periodontal regeneration of grade II FIs (maxillary and mandibular) and demonstrated significant differences between GTR and GTR plus low-level laser application1. The recorded parameters included PD, clinical attachment level (CAL), horizontal PD, alkaline phosphatase (ALP), and Osteocalcin (OC) levels in the gingival crevicular fluid (GCF) at baseline, 3, and 6 months after the procedure1.
Photodynamic Therapy
Photodynamic therapy (PDT) has emerged in recent years as a novel non-invasive treatment modality for bacterial, fungal, and viral infections. It is defined as a photochemical, oxygen-dependent reaction that occurs following light-mediated activation of a PS, leading to the generation of cytotoxic reactive species, predominantly singlet oxygen26.
This therapy can be topically applied to a periodontal pocket or intraosseous defect, thereby avoiding overdose. Additional advantages of PDT include a reduced likelihood of adverse effects associated with systemic administration of antimicrobial agents and the minimization of microbial resistance27,28. PDT also diminishes the activities of virulence factors in Gram-negative bacilli 29. Among the PS, cationic phenothiazinium dyes such as toluidine blue (TB) and methylene blue (MB) have demonstrated phototoxicity against Gram-negative bacilli when exposed to red light30,31.
Several in vitro30,31 and in vivo32,33 experimental studies have demonstrated satisfactory results using PDT to eliminate periodontopathic bacteria. The mechanism by which PDT eliminates certain microorganisms, such as Porphyromonas gingivalis (Pg), Prevotella intermedia (Pi), Aggregatibacter actinomycetemcomitans (Aa), and Fusobacterium nucleatum (Fn), has been established34,35. The lethal PS of these microorganisms involves changes in membrane or membrane plastid proteins and singlet oxygen-mediated DNA damage34-37.
Previous experimental studies in animals38-40 and humans4,41 evaluated PDT in periodontal treatment and the progression of inflammatory periodontal disease. However, there is a shortage of in vivo studies evaluating the effect of PDT on the progression of bone loss in the furcal area4.
To assess the impact of this therapy during the treatment of FI, one study investigated the role of PDT combined with non-surgical mechanical debridement in the treatment of grade II furcations42. Previous research has shown that PDT, when associated with non-surgical debridement, achieved greater reductions in PD and attachment gain in non-furcation sites41. However, these clinical advantages promoted by PDT in non-furcation sites were not observed in the study conducted by Luchessi in grade II FI42. This study showed a significant reduction in PD of 1.59 mm and an average clinical attachment level (CAL) gain of 0.78 mm in the test group, while in the control group, the respective numbers were 1.50 mm and 1.00 mm (p > 0.05)42. The absence of significant differences between the therapies may be related to the fact that PS was applied to the control sites (without laser application), which may have optimized the clinical results in the control group, contrary to previous studies4,41,43,44, which compared the performance of PDT plus SRP with mechanical debridement alone42. There is evidence showing that subgingival application of PS as monotherapy can exhibit bactericidal action, and even in sites with chronic periodontitis, it achieved superior microbiological benefits compared to controls42.
Chondros et al (2009) demonstrated that the combination of PDT with non-surgical therapy leads to a significant reduction in BOP compared to debridement alone during maintenance therapy45. In fact, research has emphasized the effect of low-level laser on cells and tissues (photobiomodulation). Light has a positive influence on supporting tissues and cells during healing, positively affecting tissue repair and decreasing inflammation due to potential biomodulatory effects45,46. These positive effects associated with laser use may have contributed to the reduction in BOP in PDT-treated FI in Luchesi's study42. Furthermore, these biomodulatory effects of PDT may also be related to the positive results observed in the study regarding the levels of markers regulating immune response and bone metabolism42. Most notably, PDT has been shown to achieve improvements in the modulation of local levels of inflammatory mediators during 6 months of follow-up42.
Laser Parameters that Influence Treatment Outcomes
In recent years, the beneficial impact of laser irradiation on bone regeneration has been documented11,12,46. It is known that low-level laser application involves specific variations such as dose, wavelength, energy density, application time, and intervals between applications1.
Among these parameters, the applied dose emerges as one of the most crucial factors to consider 1. At low doses (2-4 J/cm2), low-level laser stimulates cell proliferation and the production of basic growth factors by fibroblasts. However, both activities are deactivated at higher doses exceeding 16 J/cm2 (47.
Regarding wavelength, Almeida-Lópes investigated the effects of different diode laser wavelengths (670nm, 692nm, 780nm, and 786nm) at a fixed dose of 2 J/cm2 on fibroblasts48. Regardless of the wavelength used, cell proliferation increased in all groups by the end of the study (48.
The laser application period constitutes another pivotal factor 1. A sole application at the wound and defect site may prove insufficient to stimulate cells and reach the edges of the surgical bed. Consequently, multiple irradiations are more efficient than a singular irradiation1.
The irradiation frequency plays a crucial role in both bone formation and fibroblast growth1. Furthermore, employing laser light during the initial stages of healing demonstrated greater effectiveness in achieving complete defect filling compared to later stages, which primarily contribute to maintaining bone volume1.
Discussion
The use of PDT in periodontal therapy has demonstrated promising results in previous studies(49, 50). Consequently, it is crucial to assess the impact of this therapy during the treatment of FI42.
PDT, when combined with non-surgical debridement, has proven to achieve a more substantial reduction in PD and CAL gain in teeth without furcations51. However, these clinical benefits of PDT in teeth without furcations were not observed in a study evaluating its effects in sites with grade II FI42. In this study, there was a significant reduction in PD of 1.59 mm and CAL of 0.78 mm in the test group, while in the control group, the respective numbers were 1.50 mm and 1.00 mm (p>0.05)42.
Respectively, conservative therapy for FI, involving debridement combined with the local application of antimicrobial agents, has not provided any evidence of promising results during either initial or maintenance periodontal therapy42.
In a 2013 study by Luchesi42, investigating the effect of PDT on grade II FI as an adjunct to mechanical therapy (with a test group and a control group receiving only mechanical therapy), the absence of clinical differences between the two therapies could be related to the photosensitizer in the control sites. This factor could have optimized clinical outcomes in these groups, contrary to other studies that compared the development of PDT plus SRP with SRP alone(42, 51).
It is worth noting that the PS alone can also exhibit bactericidal action, and that subgingival application of methylene blue as monotherapy in periodontitis sites achieved greater benefits in microbiological parameters compared to control sites that received sterile water42.
Another investigation also showed that the application of toluidine blue O (TBO) alone resulted in a significant reduction of periodontopathogens on contaminated surfaces of dental implants42. However, it may be hypothesized that the maintenance of reduced levels of periodontopathogens throughout the re-evaluation period depends on the PDT approach42.
In terms of Porphyromonas gingivalis (Pg) and Tannerella forsythia (Tf) reduction, advantages were observed for the PDT group42. It was shown that the decrease in Tf from baseline was achieved only in the PDT group, 6 months after therapy42. Furthermore, although a decrease in Pg levels was observed from baseline and after 3 months for both treatments, this reduction was maintained until 6 months after therapy only in the PDT group42.
These microbiological profile changes are in line with the reduction in BOP at these sites42.
In this study, the significant reduction in BOP-positive sites detected for both therapies at 3 months was only maintained with lower levels at 6 months in the PDT group42.
In line with the results obtained, it was also shown that the combination of PDT with non-surgical therapy promoted a greater reduction in BOP scores compared to non-surgical debridement used alone during maintenance therapy42.
In fact, researchers have noted the effect of low-level lasers on cells and tissues, an effect known as "photobiomodulation"42.
Light has a positive influence on surrounding tissues and cells during tissue healing, successfully influencing tissue repair and decreasing periodontal inflammation as a result of possible biomodulatory effects42. These positive effects associated with laser use may have contributed to a reduction in BOP in PDT-treated FI sites throughout this investigation42.
These PDT biomodulatory effects may be related to the positive results observed in this study in terms of the levels of key markers regulating immune response and bone metabolism42. Scarce and conflicting data are available on the role of PDT in the inflammatory mediator profile during periodontal therapy42.
Recently, Giannopoulou et al.52, comparing the effects of PDT, diode low-level laser, or SRP on local levels of various cytokines and acute-phase proteins in residual pockets therapy, revealed that significant changes were achieved regardless of the treatment modality over 6 months. However, no differences were observed between the three treatment modalities at any time point42.
Additionally, in an experimental rat model of periodontitis, it was demonstrated that animals treated with PDT exhibited decreased bone resorption, reduced neutrophil migration, and decreased TNF-α expression compared to animals treated with photosensitizer alone, aligning with the results presented here42.
An important aspect to discuss in the Luchesi 2013 trial is the number of PDT episodes 42. In this study, a single application of PDT was used as an adjunct to mechanical therapy, and this approach did not yield clinical benefits for the treated sites in terms of Probing Pocket Depth (PPD) reduction or CAL gain42.
Conversely, it has also been revealed that additional PDT sessions following non-surgical therapy provided benefits in clinical outcomes in residual pockets during maintenance periodontal treatment, supporting the use of repeated PDT applications42.
It may be speculated that the effects of PDT as a single-episode adjunct, as conducted in this study, might not suffice to contribute to clinical improvements in FI42. Further investigations are needed to elucidate whether multiple courses of PDT could enhance treatment outcomes42) .
No data from controlled clinical studies evaluating the performance of PDT in combination with SRP for the treatment of grade II FI are available in the literature42. Thus, considering the limitations of the therapeutic approaches studied so far to manage FI, additional studies with more longitudinal follow-up periods are required42.
Moreover, it is crucial to note that topical therapeutic strategies offer several advantages compared to the use of systemic antibiotics as adjunctive therapy42.
Negative aspects related to the use of systemic antimicrobials in treating sites with periodontal disease should be acknowledged, particularly, side-effects for individual patients such as gastrointestinal disorders, and the development of bacterial resistance—a significant global public health concern. For these reasons, patient compliance may also be compromised42.
Conclusions
Although low-level laser is widely recommended for biostimulation and as an anti-inflammatory agent, to date, it has only demonstrated positive short-term outcomes as an adjunct to regenerative periodontal treatment in grade II FI. It is evident that GTR yields favorable results in FI, showcasing both clinical and biochemical improvements. The integration of low-level laser can enhance GTR effects, exhibiting attachment gain and reductions in both vertical and horizontal probing depths. However, the long-term efficacy remains unclear due to methodological weaknesses, a scarcity of comprehensive studies, and the absence of standardized parameters.
PDT could be an alternative for controlling bone loss in FI caused by periodontitis. Nevertheless, further studies are imperative to elucidate the mechanisms of action for PDT, low-level laser, and the effects of different photosensitizers as adjuncts in FI treatment. Clinical trials featuring better study designs, adequate sample sizes, extended follow-up periods, and standardized parameters are necessary to assess the effectiveness of laser therapy as an adjunct in the quest to enhance the treatment strategy for grade II FI, ultimately improving the prognosis of these lesions.
These locally applied therapies, in combination with SRP, could emerge as a significant and safe strategy in treating FI, offering an alternative to conventional chemotherapies, even those tested in this type of periodontal defect.
REFERENCES
1. Dogan GE, Aksoy H, Demir T, Laloglu E, Özyildirim E, Saglam E, et al. Clinical and biochemical comparison of guided tissue regeneration versus guided tissue regeneration plus low-level laser therapy in the treatment of class II furcation defects: A clinical study. J Cosmet Laser Ther Off Publ Eur Soc Laser Dermatol. 2016;18(2):98-104. [ Links ]
2. Smith DH, Ammons WF, Van Belle G. A longitudinal study of peridontal status comparing osseous recontouring with flap curettage. I. Results after 6 months. J Periodontol. julio de 1980;51(7):367-75. [ Links ]
3. Egelberg J. Regeneration and repair of periodontal tissues. J Periodontal Res. mayo de 1987;22(3):233-42. [ Links ]
4. de Almeida JM, Theodoro LH, Bosco AF, Nagata MJH, Oshiiwa M, Garcia VG. In vivo effect of photodynamic therapy on periodontal bone loss in dental furcations. J Periodontol. junio de 2008;79(6):1081-8. [ Links ]
5. Caffesse RG, SMith BA, Duff B, Morrison EC, Merrill D, Becker W. Class II furcations treated by guided tissue regeneration in humans: case reports. J Periodontol. agosto de 1990;61(8):510-4. [ Links ]
6. Jepsen S, Eberhard J, Herrera D, Needleman I. A systematic review of guided tissue regeneration for periodontal furcation defects. What is the effect of guided tissue regeneration compared with surgical debridement in the treatment of furcation defects? J Clin Periodontol. 2002;29 Suppl 3:103-16; discussion 160-162. [ Links ]
7. Meyle J, Gonzales JR, Bödeker RH, Hoffmann T, Richter S, Heinz B, et al. A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part II: secondary outcomes. J Periodontol. septiembre de 2004;75(9):1188-95. [ Links ]
8. Mester E. (The use of the laser beam in therapy). Orv Hetil. 29 de mayo de 1966;107(22):1012-6. [ Links ]
9. Marques MM, Pereira AN, Fujihara NA, Nogueira FN, Eduardo CP. Effect of low-power laser irradiation on protein synthesis and ultrastructure of human gingival fibroblasts. Lasers Surg Med. 2004;34(3):260-5. [ Links ]
10. Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. junio de 2015;68(1):217-69. [ Links ]
11. AboElsaad NS, Soory M, Gadalla LMA, Ragab LI, Dunne S, Zalata KR, et al. Effect of soft laser and bioactive glass on bone regeneration in the treatment of infra-bony defects (a clinical study). Lasers Med Sci. mayo de 2009;24(3):387-95. [ Links ]
12. Ozcelik O, Cenk Haytac M, Seydaoglu G. Enamel matrix derivative and low-level laser therapy in the treatment of intra-bony defects: a randomized placebo-controlled clinical trial. J Clin Periodontol. febrero de 2008;35(2):147-56. [ Links ]
13. Chambrone L, Ramos UD, Reynolds MA. Infrared lasers for the treatment of moderate to severe periodontitis: An American Academy of Periodontology best evidence review. J Periodontol. julio de 2018;89(7):743-65. [ Links ]
14. Cheng Y, Chen JW, Ge MK, Zhou ZY, Yin X, Zou SJ. Efficacy of adjunctive laser in non-surgical periodontal treatment: a systematic review and meta-analysis. Lasers Med Sci. enero de 2016;31(1):151-63. [ Links ]
15. Dai T, Fuchs BB, Coleman JJ, Prates RA, Astrakas C, St Denis TG, et al. Concepts and principles of photodynamic therapy as an alternative antifungal discovery platform. Front Microbiol. 2012;3:120. [ Links ]
16. de Oliveira RR, Schwartz-Filho HO, Novaes AB, Taba M. Antimicrobial photodynamic therapy in the non-surgical treatment of aggressive periodontitis: a preliminary randomized controlled clinical study. J Periodontol. junio de 2007;78(6):965-73. [ Links ]
17. Hou GL, Tsai CC. Types and dimensions of root trunk correlating with diagnosis of molar furcation involvements. J Clin Periodontol. febrero de 1997;24(2):129-35. [ Links ]
18. Aghazadeh A, Rutger Persson G, Renvert S. A single-centre randomized controlled clinical trial on the adjunct treatment of intra-bony defects with autogenous bone or a xenograft: results after 12 months. J Clin Periodontol. julio de 2012;39(7):666-73. [ Links ]
19. Sanz M, Giovannoli JL. Focus on furcation defects: guided tissue regeneration. Periodontol 2000. febrero de 2000;22:169-89. [ Links ]
20. Bower RC. Furcation morphology relative to periodontal treatment. Furcation entrance architecture. J Periodontol. enero de 1979;50(1):23-7. [ Links ]
21. Machtei EE, Schallhorn RG. Successful regeneration of mandibular Class II furcation defects: an evidence-based treatment approach. Int J Periodontics Restorative Dent. abril de 1995;15(2):146-67. [ Links ]
22. Anderegg CR, Metzler DG, Nicoll BK. Gingiva thickness in guided tissue regeneration and associated recession at facial furcation defects. J Periodontol. mayo de 1995;66(5):397-402. [ Links ]
23. Gottlow J, Nyman S, Lindhe J, Karring T, Wennström J. New attachment formation in the human periodontium by guided tissue regeneration. Case reports. J Clin Periodontol. julio de 1986;13(6):604-16. [ Links ]
24. Aslan S, Buduneli N, Cortellini P. Entire Papilla Preservation Technique: A Novel Surgical Approach for Regenerative Treatment of Deep and Wide Intrabony Defects. Int J Periodontics Restorative Dent. 2017;37(2):227-33. [ Links ]
25. Cortellini P, Tonetti MS. Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000. junio de 2015;68(1):282-307. [ Links ]
26. Ochsner M. Photophysical and photobiological processes in the photodynamic therapy of tumours. J Photochem Photobiol B. mayo de 1997;39(1):1-18. [ Links ]
27. Hamblin MR, Hasan T. Photodynamic therapy: a new antimicrobial approach to infectious disease? Photochem Photobiol Sci Off J Eur Photochem Assoc Eur Soc Photobiol. mayo de 2004;3(5):436-50. [ Links ]
28. Wainwright M. Photodynamic antimicrobial chemotherapy (PACT). J Antimicrob Chemother. 1 de julio de 1998;42(1):13-28. [ Links ]
29. Gad F, Zahra T, Hasan T, Hamblin MR. Effects of growth phase and extracellular slime on photodynamic inactivation of gram-positive pathogenic bacteria. Antimicrob Agents Chemother. junio de 2004;48(6):2173-8. [ Links ]
30. Kömerik N, Wilson M, Poole S. The effect of photodynamic action on two virulence factors of gram-negative bacteria. Photochem Photobiol. noviembre de 2000;72(5):676-80. [ Links ]
31. Nussbaum EL, Lilge L, Mazzulli T. Effects of 630-, 660-, 810-, and 905-nm laser irradiation delivering radiant exposure of 1-50 J/cm2 on three species of bacteria in vitro. J Clin Laser Med Surg. diciembre de 2002;20(6):325-33. [ Links ]
32. Haas R, Baron M, Dörtbudak O, Watzek G. Lethal photosensitization, autogenous bone, and e-PTFE membrane for the treatment of peri-implantitis: preliminary results. Int J Oral Maxillofac Implants. 2000;15(3):374-82. [ Links ]
33. Shibli JA, Martins MC, Theodoro LH, Lotufo RFM, Garcia VG, Marcantonio EJ. Lethal photosensitization in microbiological treatment of ligature-induced peri-implantitis: a preliminary study in dogs. J Oral Sci. marzo de 2003;45(1):17-23. [ Links ]
34. Jori G. Photodynamic therapy of microbial infections: state of the art and perspectives. J Environ Pathol Toxicol Oncol Off Organ Int Soc Environ Toxicol Cancer. 2006;25(1-2):505-19. [ Links ]
35. Meisel P, Kocher T. Photodynamic therapy for periodontal diseases: state of the art. J Photochem Photobiol B. 13 de mayo de 2005;79(2):159-70. [ Links ]
36. Bhatti M, MacRobert A, Meghji S, Henderson B, Wilson M. A study of the uptake of toluidine blue O by Porphyromonas gingivalis and the mechanism of lethal photosensitization. Photochem Photobiol. septiembre de 1998;68(3):370-6. [ Links ]
37. Maisch T, Szeimies RM, Jori G, Abels C. Antibacterial photodynamic therapy in dermatology. Photochem Photobiol Sci Off J Eur Photochem Assoc Eur Soc Photobiol. octubre de 2004;3(10):907-17. [ Links ]
38. Kömerik N, Nakanishi H, MacRobert AJ, Henderson B, Speight P, Wilson M. In vivo killing of Porphyromonas gingivalis by toluidine blue-mediated photosensitization in an animal model. Antimicrob Agents Chemother. marzo de 2003;47(3):932-40. [ Links ]
39. de Almeida JM, Theodoro LH, Bosco AF, Nagata MJH, Oshiiwa M, Garcia VG. Influence of photodynamic therapy on the development of ligature-induced periodontitis in rats. J Periodontol. marzo de 2007;78(3):566-75. [ Links ]
40. Qin YL, Luan XL, Bi LJ, Sheng YQ, Zhou CN, Zhang ZG. Comparison of toluidine blue-mediated photodynamic therapy and conventional scaling treatment for periodontitis in rats. J Periodontal Res. abril de 2008;43(2):162-7. [ Links ]
41. Andersen R, Loebel N, Hammond D, Wilson M. Treatment of periodontal disease by photodisinfection compared to scaling and root planing. J Clin Dent. 2007;18(2):34-8. [ Links ]
42. Luchesi VH, Pimentel SP, Kolbe MF, Ribeiro FV, Casarin RC, Nociti FH, et al. Photodynamic therapy in the treatment of class II furcation: a randomized controlled clinical trial. J Clin Periodontol. agosto de 2013;40(8):781-8. [ Links ]
43. Braun A, Dehn C, Krause F, Jepsen S. Short-term clinical effects of adjunctive antimicrobial photodynamic therapy in periodontal treatment: a randomized clinical trial. J Clin Periodontol. octubre de 2008;35(10):877-84. [ Links ]
44. Christodoulides N, Nikolidakis D, Chondros P, Becker J, Schwarz F, Rössler R, et al. Photodynamic therapy as an adjunct to non-surgical periodontal treatment: a randomized, controlled clinical trial. J Periodontol. septiembre de 2008;79(9):1638-44. [ Links ]
45. Chondros P, Nikolidakis D, Christodoulides N, Rössler R, Gutknecht N, Sculean A. Photodynamic therapy as adjunct to non-surgical periodontal treatment in patients on periodontal maintenance: a randomized controlled clinical trial. Lasers Med Sci. septiembre de 2009;24(5):681-8. [ Links ]
46. Verma PK, Srivastava R, Gupta KK, Chaturvedi TP. Treatment strategy for guided tissue regeneration in various class II furcation defect: Case series. Dent Res J. septiembre de 2013;10(5):689-94. [ Links ]
47. Huang YY, Chen ACH, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose-Response Publ Int Hormesis Soc. 1 de septiembre de 2009;7(4):358-83. [ Links ]
48. Almeida-Lopes L, Rigau J, Zângaro RA, Guidugli-Neto J, Jaeger MM. Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence. Lasers Surg Med. 2001;29(2):179-84. [ Links ]
49. Lui J, Corbet EF, Jin L. Combined photodynamic and low-level laser therapies as an adjunct to nonsurgical treatment of chronic periodontitis. J Periodontal Res. febrero de 2011;46(1):89-96. [ Links ]
50. Campos GN, Pimentel SP, Ribeiro FV, Casarin RCV, Cirano FR, Saraceni CHC, et al. The adjunctive effect of photodynamic therapy for residual pockets in single-rooted teeth: a randomized controlled clinical trial. Lasers Med Sci. enero de 2013;28(1):317-24. [ Links ]
51. Andersen R, Loebel N, Andersen, Dane D. Meta-analysis of five photodisinfection clinical trials for periodontitis. Photodyn Ther Back Future. 2009; [ Links ]
52. Giannopoulou C, Cappuyns I, Cancela J, Cionca N, Mombelli A. Effect of photodynamic therapy, diode laser, and deep scaling on cytokine and acute-phase protein levels in gingival crevicular fluid of residual periodontal pockets. J Periodontol. agosto de 2012;83(8):1018-27. [ Links ]
Conflict of Interest Statement: The authors have no conflict of interest in the publication of the article
Authorship contribution note: 1. Study conception and design 2. Data acquisition 3. Data analysis 4. Results discussion 5. Manuscript drafting 6. Approval of the final manuscript version MVGO has contributed in 1,2,3,4,5,6. STG has contributed in 4,5,6.
Received: April 12, 2023; Accepted: June 21, 2023











 texto em
texto em