Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.23 no.37 Montevideo 2021 Epub 30-Abr-2021
https://doi.org/10.22592/ode2021n37a2
Research
Oral health and noncommunicable diseases in patients at a higher education institution. Montevideo, Uruguay. Part 2
1Servicio de Epidemiología y Estadística. Cátedra de odontología Social, Facultad de Odontología, Universidad de la República, Uruguay. serepistat@gmail.com
2Instituto de Estadística, Facultad de Ciencias Económicas, Universidad de la República, Uruguay
Noncommunicable diseases (NCDs) share behavioral and metabolic risk factors with oral diseases. Both are also public health issues.
Objective:
To determine the prevalence of caries, gum conditions, and tooth loss in patients treated at UdelaR’s School of Dentistry.
Methods:
A sample of individuals treated at the School of Dentistry answered a questionnaire on sociodemographic characteristics and habits related to behavioral risk factors. Anthropometric measurements, blood pressure, and capillary blood glucose were recorded, and an oral exam was performed.
Results:
Six hundred and two individuals were surveyed. The average DMFT was 16, the prevalence of untreated caries, 72.8%, and the prevalence of periodontitis, 42.9%.
Conclusions:
We recommend implementing a joint preventive-care program run by the School of Dentistry and the health area of UDELAR that integrates the promotion and prevention of oral and noncommunicable diseases.
Keywords: noncommunicable diseases; oral health; epidemiology; interdisciplinary
Las enfermedades no transmisibles (ENT) comparten factores de riesgo conductuales y metabólicos con las enfermedades bucales. Ambas representan también un problema de salud pública.
Objetivo:
determinar la prevalencia de caries, paradenciopatías y pérdida dentaria en personas que demandan atención en la facultad de odontología de la udelar.
Metodos:
se relevó una muestra de los pacientes de la facultad de odontología, que respondieron un cuestionario sobre características sociodemográficas y hábitos vinculados a factores de riesgo comportamentales, se les realizaron mediciones antropométricas, de presión arterial, de glicemia capilar y un examen bucal.
Resultados:
fueron encuestados 602 individuos, el cpod promedio fue de 16, la prevalencia de caries no tratada fue de 72,8 % y la prevalencia de periodontitis 42,9 %.
Conclusiones:
Se recomienda la instalación de un programa preventivo-asistencial conjunto entre Facultad de Odontología y área salud de la UDELAR que integre la promoción y prevención de las enfermedades bucales y las no transmisibles.
Palabras Clave: Enfermedades no transmisibles; Salud Bucal; Epidemiología; Interdisciplinario
As doenças não transmissíveis (DCNT) compartilham fatores de risco comportamentais e metabólicos com as doenças bucais. Ambos também representam um problema de saúde pública.
Objetivo:
determinar a prevalência de cárie, paradenciopatias e perda de dente em pessoas que exigem atenção na faculdade de odontologia da udelar.
Métodos:
foram avaliados 602 adultos, que responderam a um questionário sobre características sociodemográficas e hábitos relacionados a fatores de risco comportamentais, medidas antropométricas, pressão arterial, glicemia capilar e realização de exame oral.
Resultados:
foram pesquisados 602 indivíduos com média de 16 cáries, prevalência de cárie não tratada de 72,8% e prevalência de periodontite de 42,9%.
Conclusões:
Recomenda-se a instalação de um programa de cuidados preventivos conjuntos entre a Faculdade de Odontologia e a área da saúde da UDELAR que integre a promoção e prevenção das doenças bucais e não transmissíveis.
Palavras-chave: Doenças não comunicáveis; Saúde Oral; Interdisciplinar
Introduction
Noncommunicable diseases (NCDs) are a set of pathologies linked to our modern lifestyle that can be explained by analyzing demographic and epidemiological transition. The four NCDs with the highest mortality rates globally are cardiovascular disease (CVD), cancer, chronic respiratory diseases, and diabetes1. Of NCD deaths, 75% occur in low- and middle-income countries. In Uruguay, NCDs account for almost 7 out of 10 recorded deaths2.
The burden of periodontal disease for an individual with a noncommunicable disease can exacerbate disease development or the patient's decompensation while treating periodontal disease can reduce systemic inflammation and improve glycemic control in diabetic patients or endothelial dysfunction in patients with CVD3. In turn, lack of treatment leads to tooth loss, nutritional status deterioration, and low self-esteem and quality of life.
Nutrition also plays a significant role in caries: refined sugars such as sucrose in beverages (soft drinks, juices, etc.), honey, and molasses used in the industrialized food industry increase the risk of caries onset and progression. Conversely, consuming vegetables, fruits, and whole grains decreases such a risk. Fruit and vegetable consumption has also been shown to help prevent oropharyngeal cancer(4. According to the Second National NCD Risk Factors Survey(5 conducted by the Ministry of Public Health of Uruguay, 50% of the adult population (25-64 age range) has three or more combined risk factors.
Regarding oral health, the data from the First National Survey of Oral Health among Uruguayan young people and adults 2010-20116) indicate that caries prevalence (DMFT ≥ 1) among young people (15-24), adults (35-44), and older adults (65-74) is 80.5%, 99.5%, and 99.6%, respectively. The average number of decayed, missing, and filled teeth (DMFT) is 4.1, 15.2, and 24.1 for ages 15-24, 35-44, and 65-746,7. The prevalence of periodontal disease (pathological pockets ≥ 4mm) is 11%, 29%, and 25% for the above ages6,8.
There are data on the Uruguayan population regarding NCDs and oral diseases. However, they lack a common approach to risk factors that consider both pathologies. This work aimed to determine the prevalence of NDC risk factors and the most frequent oral diseases (caries and gum conditions) in users treated at the School of Dentistry, UdelaR. This paper presents the oral health descriptive data; the data on NCDs have already been published9.
Methodology
This is a descriptive, cross-sectional study conducted at the Patient Admission and Registry Department of the School of Dentistry for the August 2015 - May 2016 period.
The sampling strategy considered the seasonality of patient attendance for registration at the School of Dentistry and the three shifts in which the department operates (morning, afternoon, and evening). Therefore, in the data collection period, patient recruitment followed a sequential sampling logic, including all the patients who had an appointment for that shift and on that day. The research team decided to implement a mixed design given these logistics as it was the most appropriate one in terms of human resources. This sample size was reached considering a method similar to the simple random sampling technique, making it possible to estimate a prevalence of up to 30% with 95% confidence and 5% error, considering up to two estimation domains (by sex or age group). It was also self-weighting. This involved selecting 320 per domain, which required 640 patients. The full study methodology can be found in the previously published paper referring to the report on NCD prevalence in the surveyed population9.
Data collection
Participants answered a questionnaire on sociodemographic information (sex, age, education, monthly income, type of work, and health care coverage), behavioral and metabolic risk factors. In addition, anthropometric measurements. Capillary blood glucose and information on oral pathologies (caries, gum conditions, mucosal lesions, and tooth loss) were recorded.
A thorough dental examination was conducted to assess oral condition. It was performed on a dental chair, with mirror, pliers, and CPI probe, crown, and root decay were recorded, as well as periodontal pockets (WHO manual, 2013)10 and attachment loss per sextant.
Training and calibration
The questionnaire criteria were standardized (four joint meetings with the professionals participating in the study). An instructions booklet was designed to record research form answers, and the interviewers were trained in the use of various brochures (food, alcoholic beverages, and physical activity).
For oral pathology training and calibration, the work team followed the 2013 WHO Oral Health Surveys - Basic Methods10 and the National Oral Health Survey conducted in Uruguay in 20116. The training sessions took place in March 2015, and six examiners participated. It included three stages: first, the diagnostic criteria of three of the pathologies to be surveyed (caries, periodontal disease, and erosion) were standardized. This was done with the collaboration of reference tutors specialized in the clinical disciplines related to each pathology.
In the second stage of practical clinical work, the professionals were trained on caries and periodontal disease. An inter-examiner calibration study was conducted, including six examiners and six recorders. The kappa coefficient was calculated for each variable. Values obtained: caries (crown): 0.85; caries (root): 0.79. As for the CPI indicator, periodontal pocket and attachment loss were calibrated, with a value of 0.71 and 0.79.
Variables and indicators
The following indicators were considered for oral pathologies:
Caries: the WHO cavitated caries criterion was used (year 2013). The DMFT index was used to report the DMFT % >O prevalence. The average DMFT in the population was also calculated, and the D component was used to report untreated caries.
Periodontal disease: reported according to the Community Periodontal Index (CPI) (index teeth, WHO, 1997). Periodontitis is defined as the presence of a periodontal pocket > 4 mm and clinical attachment loss (CAL) > 3 mm in any of the sextants(11. The indicator used was the ratio of people with periodontitis.
Tooth loss: the average number of teeth present per age group and the prevalence of non-functional dentition. Non-functional dentition is when an individual has fewer than 20 teeth12.
The prevalence of qualitative variables was summarized by calculating ratios, while averages were used for quantitative variables. Estimate uncertainty was assessed with 95% confidence intervals.
Results
Dental caries
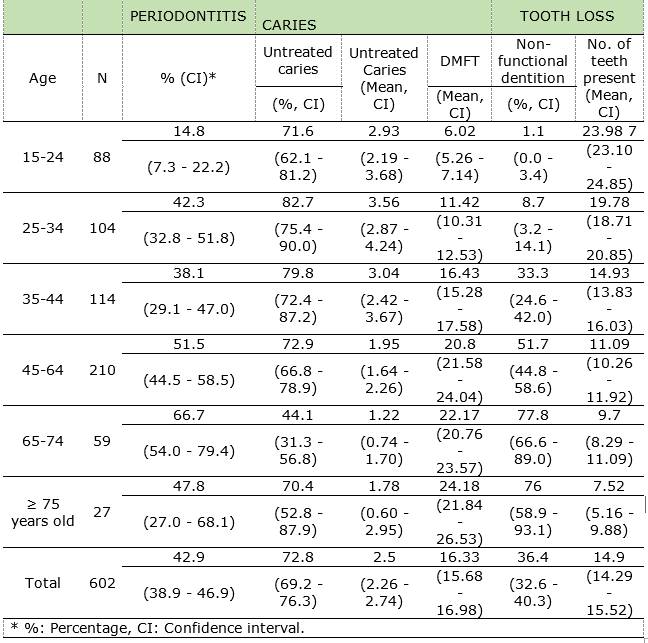
The prevalence of untreated caries was 72.8%. Most age groups had a similar prevalence, except the 25-34 group, which had the highest prevalence, and the 65-74 group, which had the lowest (82.7 and 44.1 respectively). Two groups are observed regarding the average number of teeth with an untreated carious lesion. The first three age groups have an average of three untreated lesions, and the last three age groups, an average lower than two. The 45-64 and 65-74 groups showed a significant increase compared to the three younger groups.
Furthermore, when analyzing the average number of teeth with caries compared to the average number of teeth, the resulting value is 17% for all ages (the values were 12%, 20%, 16%, and 13% for ages 15-24, 35-44, 45-64 and 65-74).
Increased DMFT values were observed with age, with an average of 16 teeth affected.
Periodontal disease
The prevalence of periodontitis showed a significant difference between young people (14.8%) and the other ages considered, ranging from 38.1% to 66.7%. Although prevalence increases with age, it is not monotonous.
Tooth loss
In total, 63.6% of respondents had functional dentition. The prevalence of non-functional dentition increases monotonously with age, except in the last section (≥ 75 years), with a significant increase observed in ages 45-64 and 65-74 (Table 1).
Discussion
We address the three age groups recommended by the WHO for international comparison: 15-24 (young people), 35-44 (adults), and 65-74 (older adults)10.
Both periodontitis and untreated caries prevalence were significantly higher in adult patients treated at the School of Dentistry than the same age group nationwide. This was expected because the population studied is precisely the one seeking oral health care.
DMFT is higher among young people and adults in this group than in national data, recording values of 4.15 (CI: 3.8-4.49) and 15.2 (CI: 14.24-16.16) respectively6,7.
As for the D component in DMFT, it is impossible to compare the prevalence of untreated caries in young people because of the lack of nationwide published data. However, it is expected to be higher because these patients seek care in a healthcare facility. For adults and older adults, component D values in relation to national survey values (1.7 (CI: 1.39-2.00) and 0.66 (CI: 0.48-0.84), respectively) were significantly higher among the patients treated at the School of Dentistry(7.
Periodontitis prevalence increases by 157% when going from the 15-24 group to the 35-44 group (66.7/14.8). Additionally, it increases by 75% when going from the 35-44 group to the 65-74 group (66.7/38.1). When comparing periodontitis in adults and older adults to nationwide prevalence-21.8- (CI: 17.9-26.3)8, we observed a 140% relative increase (52.4/21.8) in patients treated at the School of Dentistry. This confirms that this population has a higher burden of disease.
The prevalence of non-functional dentition among patients treated at the School of Dentistry compared to nationwide values in the 35-44 and 65-74 groups was similar12. It might be the case the School of Dentistry’s patients do not have the highest proportion of tooth loss because they seek restorations, periodontal therapy, and partial rather than complete prostheses. The values corresponding to the average number of teeth in the mouth are similar in older adults nationwide (9.73 CI: 8.77-10.69) compared to patients treated at the School of Dentistry (9.7 CI: 8.29-11:09).
The highest level of oral pathology in the population treated at the School of Dentistry compared to nationwide data coincides with the highest level of pathologies found regarding NCDs nationwide, as was recently published(9.
Conclusions
Regarding the prevalence of oral diseases, individuals attending the School of Dentistry have higher levels of caries and periodontitis pathology compared to the general Uruguayan population. This highlights the social role of the university as an institution (a health provider outside the National Health System) and the need to design comprehensive prevention and health promotion programs that integrate the prevention of NCDs and oral diseases. The relationship between oral diseases and NCDs and their risk factors should be further researched.
REFERENCES
1. WHO. Noncommunicable diseases. Fact sheet updated Junio 2018, en linea, consultado 30 de octubre de 2018. Disponible en: http://www.who.int/mediacentre/factsheets/fs355/en/ [ Links ]
2. Uruguay. Ministerio de Salud Pública. Enfermedades No Transmisibles. en línea; consultado 30 de octubre de 2018. Disponible en:Disponible en:http://www.msp.gub.uy/noticia/enfermedades-no-transmisibles [ Links ]
3. Eke PI, Wei L, Thornton-Evans GO, Borrell LN, Borgnakke WS, Dye B, Genco RJ. Risk indicators for periodontitis in US adults: NHANES 2009 to 2012. J Periodontol 2016 Oct;87(10):1174-85 [ Links ]
4. Janket S-J, Baird AE, Chuang S-K, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95(5): 559-569 [ Links ]
5. Uruguay. Ministerio de Salud Pública. Segunda Encuesta Nacional de Factores de Riesgo de Enfermedades No Transmisibles. PPENT. Montevideo, 2013. en línea ;consultado 30 de octubre de 2018. Disponible en: Disponible en: http://www.msp.gub.uy/publicaci%C3%B3n/2%C2%AA-encuesta-nacional-de-factores-de-riesgo-de-enfermedades-no-transmisibles [ Links ]
6. Lorenzo-Erro S, Blanco S, Álvarez R, Massa F, Fabruccini-Fager A, Olmos P, Musto M, Ourens M. Primer Relevamiento Nacional de Salud Bucal de jóvenes y adultos uruguayos 2011. Facultad de Odontología. Universidad de la República. Montevideo, marzo 2018. Disponible:https://www.colibri.udelar.edu.uy/jspui/handle/20.500.12008/18508 [ Links ]
7. Álvarez L, Liberman J, Abreu S, Mangarelli C, Correa MB, Demarco FF, Lorenzo S, Nascimento GG.-Dental caries in Uruguayan adults and elders: findings from the first Uruguayan NationalOral Health Survey. Cad Saude Publica. 2015 Aug; 31(8):1663-72. doi: 10.1590/0102-311X00132214. [ Links ]
8. Lorenzo SM, Álvarez R, Andrade E, Piccardo V, Francia A, Massa F, Correa MB, Peres MA. Periodontal conditions and associated factors among adults and the elderly: findings from the first National Oral Health Survey in Uruguay.Cad Saude Publica. 2015 Nov; 31(11):2425-36. doi: 10.1590/0102-311X00012115. [ Links ]
9. Lorenzo-Erro SL, Skapino E , Musto M, Olmos P, Álvarez R, Fabruccinni A, Massa F, Moliterno P, Piovesán S, Cosetti L, Pisón F. Salud Bucal y Enfermedades no transmisibles en pacientes de un centro de enseñanza terciaria, Montevideo, Uruguay 2016. Parte 1. Odontoestomatología. 2020; 22(36) [ Links ]
10. World Health Organization. Oral Health Surveys. Basic Methods. 5th Edition.Geneva; 2013 [ Links ]
11. Vettore MV, Marques RA, Peres MA. Social inequalities and periodontal disease: multilevel approach in SB, Brasil 2010. Rev Saude Publica. 2013;47Suppl 3:29-39 [ Links ]
12. Nicola-Laguzzi P, Silveira-Schuch H, Derrégibus-Medina L, Rodríguez-de Amores A, Demarco FF, Lorenzo S. Tooth loss in the elderly in Uruguay. J Public Health Dent 2016; 76: 143-151. doi:10.1111/jphd.12123 [ Links ]
Ethics Committee approval Approved by the Ethics Committee of the Dentistry School (Exp n° 091900-000121-14)
Declaration of interests: The authors certify that they have no commercial interests that represents a conflict of interests in connection with the manuscript
Authors' contribution note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript. SMLE ha contribuido en: 1,3,4,5,6 RA ha contribuido en: 1,3,4,6 AF ha contribuido en: 2,3,4,5,6 FM ha contribuido en: 3,4,6
Received: August 13, 2020; Accepted: January 27, 2021











 texto em
texto em