Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.22 no.36 Montevideo 2020 Epub 01-Dez-2020
https://doi.org/10.22592/ode2020n36a7
Research
Oral Health and Non communicable Diseases in patients of a higher education institution, Montevideo, Uruguay 2016. Part 1
1Servicio de Epidemiología y Estadística, Cátedra de odontología Social, Facultad de Odontología, Universidad de la República, Montevideo, Uruguay
2Departamento de Nutrición Clínica, Escuela de Nutrición, Universidad de la República, Montevideo, Uruguay
3Cátedra de Odontología Social, Facultad de Odontología, Universidad de la República, Montevideo, Uruguay
4Instituto de Estadística. Facultad de Ciencias Económicas, Universidad de la República. Montevideo, Uruguay
5Cátedra de Endodoncia, Facultad de Odontología, Universidad de la República. Montevideo, Uruguay
6Servicio de Registro y Admisión de Pacientes, Facultad de Odontología, Universidad de la República, Montevideo, Uruguay
7Cátedra Patología y Semiología Buco Maxilar y Clínica Estomatológica, Facultad de Odontología, Universidad de la República. Montevideo, Uruguay
8Facultad de Enfermería, Universidad de la República, Montevideo, Uruguay
9Práctica privada. Facultad de Odontología, Universidad de la República, Montevideo, Uruguay
Non-communicable diseases (NCD) share behavioral and metabolic risk factors with oral diseases and both represent a public health problem.
Objective:
to find out the prevalence of NCD and its behavioral and metabolic risk factors in people who attend at College of Odontology of the University of the Republic.
Methods:
A Cross-sectional study was conducted and a questionnaire related to socio-demograhic characteristics and habits linked to behavioral risk factors was applied. Anthropometric measurements of arterial pressure and capillary glucose were taken,
Results:
The final sample were 602 individuals. A high prevalence of physical inactivity, problematic alcohol intake, excessive salt consumption, hypertension and diabetes was found. These figures were larger than those found at the national level.
Conclusions:
Due to the high prevalence of various risk factors, the installation of a preventive-educational program in the waiting rooms of the Faculty is recommended.
Keywords: Non-communicable diseases; Oral Health; Epidemiology; Interdisciplinary
Las enfermedades no transmisibles (ENT) comparten factores de riesgo conductuales y metabólicos con las enfermedades bucales y ambas representan un problema de salud pública.
Objetivo:
Determinar la prevalencia ENT y sus factores de riesgo conductuales y metabólicos en personas que concurrieron a la Facultad de Odontología de la Universidad de la República.
Metodos:
Estudio transversal en el que se aplicó un cuestionario sobre características sociodemográficas y hábitos vinculados a factores de riesgo comportamentales. Se realizaron mediciones antropométricas, de presión arterial y glicemia capilar.
Conclusiones:
En función de las prevalencias elevadas de varios factores de riesgo, se recomienda la instalación de un programa preventivo-educativo en las salas de espera de la Facultad.
Palabras clave: Enfermedades no transmisibles; Salud Bucal; Epidemiología; Interdisciplinario
As doenças não transmissíveis (DNT) compartem fatores de risco comportamentais e metabólicos com as doenças bucais, as duas representam um problema de saúde pública.
Objetivo:
Determinar a prevalência DNT e os fatores de risco comportamentais e metabólicos em pessoas que concorreram à Faculdade de Odontologia da Universidade da República.
Métodos:
Foi realizado um estudo transversal, onde foi aplicado um questionário relativo às características sociodemográficas e hábitos ligados com fatores de risco comportamentais. Se realizaram medições antropométricas, de pressão arterial e glicemia capilar.
Resultados:
Foram pesquisados 602 indivíduos. Constatou-se uma alta prevalência de inatividade física, ingestão problemática de álcool, consumo excessivo de sal, hipertensão e diabetes. Estes valores foram acima dos encontrados a nível nacional.
Conclusão:
Dada a alta prevalência encontrada de vários fatores de risco, recomenda-se a instalação de um programa educacional-preventivo nas salas de espera da Faculdade.
Palavras-chave: Doenças não comunicáveis; Saúde Oral; Interdisciplinar
Introduction
Noncommunicable diseases (NCDs) are a set of pathologies linked to our modern lifestyle that can be explained by analyzing demographic and epidemiological transition. This phenomenon occurred in the 1920s, when we moved from a model of agricultural-cultural influence, where the main causes of death were infectious diseases, to a model of industrial and post-industrial society, where NCDs are the main causes of death.(1-2) Therefore, this new productive model shapes the general determinants of health and disease, influencing the specific level of the lifestyles of social groups, which in turn determines individuals and how their lifestyles are expressed.(3)
The NCDs with the highest mortality rates globally are four: cardiovascular disease (CVD), cancer, chronic respiratory diseases, and diabetes. Of NCD deaths, 75% occur in low- and middle-income countries.(4) In Uruguay, NCDs account for almost 7 in 10 recorded deaths.(5) Although these diseases are associated with old age, an increasing number of people under 70 are dying of these diseases, especially in the poorest regions.(6) The classical epidemiological approach states that these diseases share four behavioral risk factors: unhealthy diet (high sodium, refined sugar, saturated and trans fats, and low in fiber), smoking, harmful alcohol use, and physical inactivity. Exposure to these behavioral risk factors leads to metabolic risk factors developing over time: obesity, high blood pressure, high fasting blood sugar, and high cholesterol. Behavioral and metabolic risk factors can be modified, making these pathologies preventable. This results in a significant decrease in the number of premature deaths.(7) Although oral pathologies such as periodontal disease, caries, inflammation of the mucosa, and tooth loss do not have high mortality rates, they are included in the global burden of chronic diseases and share many of the risk factors for NCDs.(8) So much so that oral disease, kidney and eye diseases have been included in Article 19 of the NCD Report since 2011.(9)
According to Watt R. (2012),(10) the common approach recognizes the risk factors shared by NCDs and oral diseases, which would allow for more efficient public health joint work. Furthermore, a broader epidemiological approach, such as the social determinants of health, has some differences with the risk approach, questioning its comprehensive explanatory power. Authors such as Breilh(3), working from the social determination paradigm, argue that referring to risk factors implies a fragmented approach to reality since factors capture only part of the complex causality of health and disease processes, decontextualizing them and separating them from higher causal hierarchy levels (lifestyles and social structure). This prevents us from understanding how these pathologies occur and develop.
There are few studies on the joint approach of NCD risk factors in Uruguay.(11) According to the Second National NCD Risk Factors Survey(12) conducted by the Ministry of Public Health of Uruguay, 50% of adults have three or more risk factors combined. No nationwide studies have been found to implement a common approach including risk factors for oral disease and NCDs. This work aimed to determine the sociodemographics, the prevalence of NDC risk factors, and the most frequent oral diseases (caries and gum conditions) in users treated at the School of Dentistry, UDELAR. This first part presents only the results of NCD prevalence among patients treated at the School of Dentistry.
Methodology
This is a descriptive, cross-sectional study conducted at the Patient Admission and Registry Department of the School of Dentistry for the August 2015 - May 2016 period.
The sampling strategy considered the seasonality of patient attendance for registration at the School of Dentistry and the three shifts in which the department operates (morning, afternoon, and evening). The fieldwork was conducted from August to November (2015) and from March to May (2016). Therefore, in the data collection period, patient recruitment followed a sequential sampling logic, including all the patients who had an appointment for that shift and on that day. Therefore, given the logistics that the research team considered the best in terms of available human resources, a mixed design was implemented: it is sequential, but a previously calculated sample size of 800 patients was set at the beginning of the study. This sample size was reached considering the simple random sampling technique, making it possible to estimate a prevalence of up to 30% with 95% confidence and 5% error, considering up to two estimation domains (by sex or age group). It was also self-weighting. These requirements for margins of error, confidence and prevalence levels involved about 320 patients per domain: 640 patients in total. If we assume a non-response rate of 20%, the final number of the original 800 was reached.
1) Data collection
Participants answered a questionnaire on sociodemographic information (sex, age, education, monthly income, type of work, and health care coverage), behavioral and metabolic risk factors. Besides, anthropometric measurements (weight, height, and waist circumference), capillary blood glucose, blood pressure, and information on oral pathologies (caries, gum conditions, mucosal lesions, and tooth loss) were recorded. Patient height was measured with a stadiometer (SECAR brand), with the individual barefoot, standing, back against the measuring bar, heels together, in contact with the stadiometer. The measurement was taken after the patient had taken a deep breath and keeping the head in the Frankfort horizontal plane. Waist circumference was measured by edging the abdominal circumference at the midpoint level between the costal margin and the iliac crest with an inextensible tape measure. Blood glucose was measured via finger prick with single-use lancets and test strips for subsequent measurement on a digital glucose meter (Bayer Contour TS) following the manufacturer’s recommendations. An aneroid device (RIESTER brand, verified by LATU - No. 333075, 06/2015) was used to measure blood pressure (BP). It was necessary to prepare the participants: they were asked to sit quietly for 15 minutes before taking their blood pressure. The cuff was selected according to arm perimeter. A thorough dental examination was conducted to assess oral condition. It was performed on a dental chair, with mirror, pliers, and CPI probe, crown and root decay were recorded, as well as periodontal pockets (WHO manual, 2013),(13) and attachment loss per sextant.
2) Ethical issues
Under the regulations in force in Uruguay, the research project was presented and approved by the Research Ethics Committee of the School of Dentistry. There was a conversation to help patients understand the study and administer the questionnaire where prospective participants decided whether to participate. If they agreed, they were requested to sign a written informed consent. Participants were informed of their measurements (weight, size, waist circumference, capillary blood glucose, and blood pressure) and advised on the need for medical consultation when appropriate.
3) Training and calibration
The questionnaire criteria were standardized (four joint meetings with the professionals participating in the study). An instructions booklet to record research form answers was designed, and the interviewers were trained in the use of various brochures (food, alcoholic beverages, and physical activity).
A training session in anthropometry was held, where instructors explained how to assemble and place the stadiometer. Height was recorded by measuring the same individual twice; if there was a difference greater than 0.5 cm, the patient was measured a third time, and the average of the two closest figures was recorded. The same procedure was conducted to measure waist circumference. Standardization was not necessary for weight measurement as it was done with an electronic scale (direct reading from the display).
Interviewers were trained in capillary sampling to monitor blood glucose and in using the glucose meter. Interviewers used a digital device with the corresponding test strips and lancets for disposable puncture. The relevant procedure and the manufacturer’s recommendations were followed to measure capillary blood glucose.
As for calibration for BP measurement, three different operators took the pressure of ten individuals on three occasions. A degree of agreement was obtained, and each interviewer’s margin of error when measuring BP was acceptable, with an intraclass correlation coefficient between 0.73 and 0.91.
For oral pathology training and calibration, the work team followed the 2013 WHO Oral Health Surveys - Basic Methods(13) and the National Oral Health Survey conducted in Uruguay in 2011(14-15).
4) Variables and indicators
Behavioral variables: Fruit and vegetable consumption: less than five servings a day was considered insufficient. Alcohol consumption: a variable was developed considering the frequency and number of drinks, with the following categories: "no consumption," "very low consumption," "low consumption," "moderate," "high," and "very high." The categories “high” and “very high” were considered excessive consumption. Tobacco use: daily tobacco consumption was considered a risk factor. Physical activity: insufficient physical activity: less than 75 minutes of vigorous physical activity per week or less than 150 minutes of moderate physical activity per week. High salt intake: When participants stated they added salt to salted food "always" and "almost always," these frequencies were considered a risk factor.
Regarding metabolic risk factors: for hypertension, a systolic blood pressure (SBP) greater than or equal to 140mmHg and/or diastolic blood pressure (DBP) greater than or equal to 90mmHg11, or self-reported hypertension. Impaired fasting glycaemia (IFG) was considered for those with capillary blood glucose greater than or equal to 200 mg/dl with or without fasting; or a history of diabetes diagnosed by a physician or self reported (MSP, 2007) 11.
Altered nutritional status: Altered waist circumference in women greater than 88 cm, and in men, greater than 102 cm. Body mass index (weight to height ratio (kg/m2) - BMI): overweight: 25-29.9 kg/m2; obesity: 30 kg/m2 or more 16.
For oral pathologies, caries was used as a DMFT indicator, and for gum conditions, periodontal pocket and attachment loss ratio was used.
Results
Six hundred and two patients were examined. Finally, the 800 patients were not needed as the non-response rate was well below expectations (20%). The “no response” analysis did not show a selection bias. The participation rate was 95%.
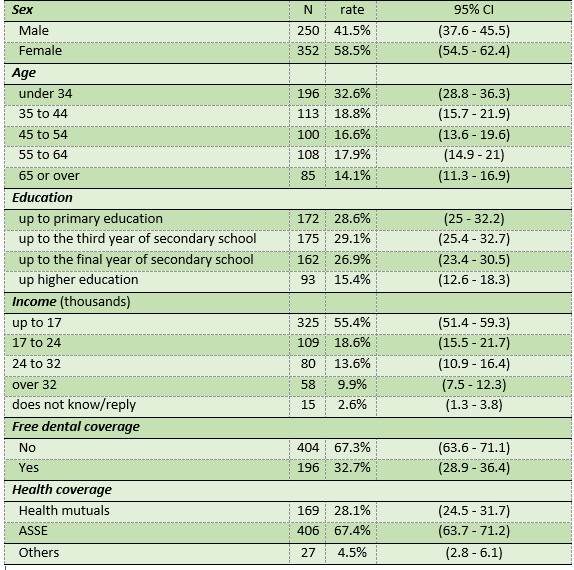
Most respondents were female (three in five), only 40% were married, or in a free union, 32.6% were aged between 18 and 34, 53.3% were aged between 35 and 64, and 14.1% were over the age of 65. The mean age of the population studied was 44 (± 16.8) (Table 1).
Socioeconomic characteristics of the population studied: 75% had completed primary or secondary education, and only 15% had completed higher education (Table 1).
Two in three participants were treated at the State Health Services Administration (ASSE) regarding access to health services. Two in three participants stated that when they have oral health problems, they seek care at the private sub-sector (health mutuals, cooperatives, health offices).
Behavioral and metabolic factors
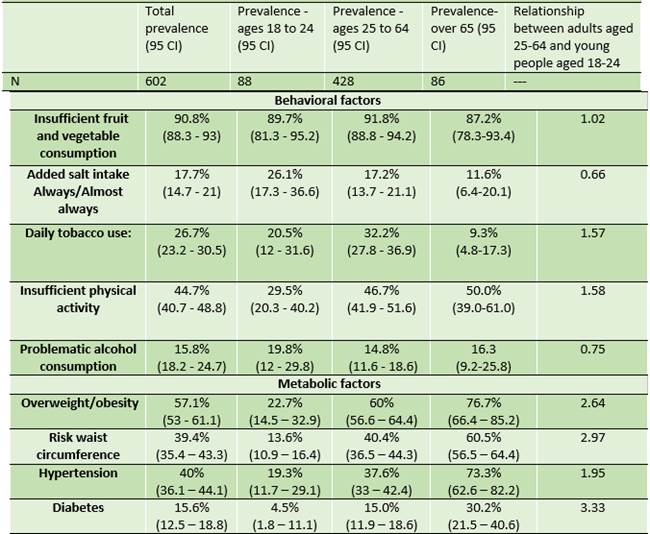
Regarding behavioral factors (Table 2), almost 91% of participants failed to consume the recommended five servings a day of fruit and/or vegetables, with similar consumption in the 18-24 and 25-64 age groups. Furthermore, 44.7% reported insufficient physical activity. In relative terms, 58.0% more middle-aged individuals than young people reported insufficient exercise.
As for smoking habits, the most considerable difference appeared between older and middle-aged adults, who smoke three times more than older adults daily.
Regarding added salt intake, adults consumed ⅓ less than young people.
As for problematic alcohol consumption, no significant differences were observed among the age groups (Table 2).
Adults had approximately a 164% higher prevalence of being overweight and obese than younger individuals. While there was a risk waist circumference in 39.4% of all cases, the relative prevalence in adult versus younger individuals was 4.4 (340%).
Adult individuals with high blood pressure almost doubled the number of younger participants with the condition.
The prevalence of diabetes was 15.6%, which increased with age. Adults had a prevalence that was three times higher than young people. (Table 2).
Discussion
This study analyzes a specific population of patients who sought dental care at the School of Dentistry in the 2015-2016 period. It is the first national study that attempts to jointly determine the prevalence of NCD risk factors and the most frequent oral diseases. There was a high level of participation (95%). There was a high prevalence of physical inactivity, problematic alcohol consumption, excessive salt consumption, hypertension, and diabetes. These figures were higher than those found nationwide.
The sociodemographic profile of the people that seek care at the School of Dentistry is as follows: adults, mostly aged between 18 and 64, having primary school as the highest level of education, with an income level that does not exceed three minimum wages and whose health is cared for generally in the public subsector (70%). This proportion is almost the opposite to that of the Uruguayan population as a whole, where the proportion of individuals who sought health services in the public sector-in the year when this survey was conducted-was approximately 30%.(17)Regarding oral health care, the participants state they seek care in the private sector (66%) when they can afford the cost. This shows that the school treats patients who remain marginal in the Uruguayan society as their right to oral health is not protected as it should, according to Law 18211 that sets forth the National Integrated Health System. The law’s content is limited by the catalogue of benefits provided for oral health(18-19.
Regarding behavioral factors, insufficient fruit and vegetable consumption and smoking habits were similar to the results of the Second National NCD Risk Factors Survey (2nd ENFRENT),(11) both in the overall sample and in both age groups.
Furthermore, added salt intake among the total population of this study amounted to 17.7%, while in the 2nd ENFRENT, it was 14.1%. This shows a relative increase of 26% of individuals consuming added salt in the population treated at the School of Dentistry. Salt consumption in the youngest segment was 26.1%, while it was 19.3% nationwide. This reflects an increase of 35% in the relative prevalence of frequent salt users among the participants in this study. In the 25-64 age group, salt overuse was 17.2%, while it was 12.5% nationwide (37% more among the school’s patients). The higher frequency in both age groups may explain to some extent the higher overall prevalence of hypertension compared to the results of the 2nd ENFRENT. Similarly, when analyzing insufficient physical activity globally, this study found a higher number of individuals: 44.7%, while nationwide, it was only 21.6%, showing. This entails 2.1 times more relative prevalence of individuals with insufficient physical activity in this study.
Finally, when analyzing problematic alcohol consumption and insufficient physical activity without distinguishing age groups, this study’s figures double those that apply to the national population.
Regarding metabolic risk factors, the prevalence of overweight and obese patients (BMI>25kg/m2) in our study’s total population is very similar to nationwide results: 57.1% and 58.5% respectively, obesity prevalence being also similar in the 25-64 age group. Additionally, the prevalence of risk waist circumference in our population is also similar to the data collected in the 2nd ENFRENT. As for overweight-obesity in the youngest age group, the proportion of young people with this risk factor in this study is lower than that reported nationwide (40% lower). The question remains whether the young population is healthier in terms of overweight and obesity, which should be confirmed.
Hypertension had a higher relative prevalence in patients treated at the school: 34% compared to the national figure (40% and 29.8%). While the 25-64 age group has values similar to nationwide values, in the younger age group, the relative prevalence of hypertension is 2.2 times higher in patients treated at the school than the results found in the 2nd ENFRENT.
In this study, diabetes was determined when capillary blood glucose was greater than 200mg/dl (with or without fasting) or through self-reported diabetes, or when diagnosed by a physician. In the 2nd ENFRENT, diabetes was determined through fasting blood glucose equal to or greater than 126mg/dl, or self-reported diabetes or on diabetes medication. The prevalence for the 25-64 age group was 15.6 (40% higher) in this survey compared to the nationwide survey. Differences in the criteria applied could explain the higher prevalence of diabetes among the population surveyed in this study.
As this is a specific population seeking dental care in a non-profit university educational institution, both the sociodemographic characteristics and oral conditions restrict the potential comparisons with population based studies.
Conclusions
The high prevalence of behavioral risk factors-insufficient physical activity, problematic alcohol intake, and excessive consumption of added salt-as well as metabolic risk factors-hypertension and diabetes-in the population studied compared to nationwide prevalence figures pointed to the need for an integrated approach to health. This can be done by designing standard programs for people treated at the School of Dentistry to promote healthy habits and prevent noncommunicable and oral diseases. It should be possible to implement these programs in other healthcare centers too.
REFERENCES
1. Misa A . Demografía. En: Benia W, Reyes I. (Coord). Temas de salud pública Montevideo: Oficina del libro FEFMUR; 2009. p. 17-46. [ Links ]
2. Dever A, Champagne F. Epidemiologia y Administración de Servicios de Salud. Organización Panamericana de la Salud. 1991. 417 p. [ Links ]
3. Breilh J. Debates y desafíos. Epidemiología crítica latinoamericana: raíces, desarrollos recientes y ruptura metodológica. En: Morales C, Eslava JC. Tras las huellas de la determinación. 1era. ed. Bogotá: Universidad Nacional de Colombia; 2014. p. 17-77 [ Links ]
4. WHO. Non communicable diseases. Fact sheet updated Junio 2018.; consultado 30 de octubre de 2018. Disponible en: http://www.who.int/mediacentre/factsheets/fs355/en/ [ Links ]
5. Uruguay. Ministerio de Salud Pública. Enfermedades No Transmisibles, en línea, consultado 30 de octubre de 2018. Disponible en:http://www.msp.gub.uy/noticia/enfermedades-no-transmisibles [ Links ]
6. Hosseinpoor AR, Bergen N, Kunst A, Harper S, Guthold R, Rekve D, d'Espaignet ET, Naidoo N, Chatterji S. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the World Health Survey. BMC Public Health. 2012; 12: 912 [ Links ]
7. World Health Organization. Global Action Plan for the prevention and control of noncommunicable diseases 2013-2020. Disponible en https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1 [ Links ]
8. Petersen PE, Ogawa H. The Global Burden of periodontal disease: Towards integration with chronic disease prevention and control. 2012. Periodontol 2000. 2012; 60 (1): 15-39. [ Links ]
9. Oral Disease Added to United Nations Declaration on Non communicable Diseases Essential Dental Knowledge. J Can Dent Assoc 2011;77:b138. Disponible en: http://www.jcda.ca/article/b138. [ Links ]
10. Watt RG. Social determinants of oral health inequalities: implications for action. Community Dent Oral Epidemiol. 2012; 40 (supp.2): 44-48. [ Links ]
11. Rubinstein AL, Irazola VE, Calandrelli M, Rubinstein A, Irazola V,* Calandrelli M, Elorriaga N, Gutierrez L, Lanas F, Manfredi J, Mores N, Olivera H, Poggio R, Ponzo J, Seron P, Chen C, Bazzano LA,Hef J. Multiple cardiometabolic risk factors in the Southern Cone of Latin America: a population-based study in Argentina, Chile, and Uruguay. Int J Cardiol. 2015; 183: 82-88. doi:10.1016/j.ijcard.2015.01.062 [ Links ]
12. Uruguay. Ministerio de Salud Pública. Segunda Encuesta Nacional de Factores de Riesgo de Enfermedades No Transmisibles. PPENT. Montevideo, 2013.en línea, consultado 30 de octubre de 2018. Disponible en: http://www.msp.gub.uy/publicaci%C3%B3n/2%C2%AA-encuesta-nacional-de-factores-de-riesgo-de-enfermedades-no-transmisibles [ Links ]
13. World Health Organization. Oral Health Surveys. Basic Methods. 4th Edition. Geneva: WHO, 2013 [ Links ]
14. Lorenzo S. Editorial: Primer Relevamiento Nacional de Salud Bucal en población joven y adulta uruguaya (Internet). Odontoestomatología 2014.;15(nspe)Disponible en: http://www.scielo.edu.uy/pdf/ode/v15nspe/v15nspea02.pdf [ Links ]
15. Lorenzo S, Álvarez R, Blanco S, Peres M. Primer Relevamiento Nacional de Salud Bucal en población joven y adulta uruguaya: Aspectos metodológicos. Odontoestomat. 2013; 15( spe ): 8-25. [ Links ]
16. WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894 [ Links ]
17. Oreggioni I. El camino hacia la cobertura universal en Uruguay: cobertura poblacional del Sistema Nacional Integrado de Salud. En: Economìa, política y economía política para el acceso y la cobertura universal de salud en el Uruguay. OPS 2015. Disponible en: https://www.paho.org/uru/index.php?option=com_docman&view=download&category_slug=publicaciones-sistemas-y-servicios-de-salud&alias=468-capitulo-2-pdf&Itemid=307 [ Links ]
18. Uruguay. Poder Legislativo. Ley No 18.211 sistema nacional integrado de salud. 2007. Disponible en: https://legislativo.parlamento.gub.uy/temporales/leytemp28458.htm [ Links ]
19. Uruguay. Ministerio de Salud Pública. Plan Integral de Atención en Salud (PIAS). 2008. Disponible en: http://www.msp.gub.uy/sites/default/files/Decreto_y_Anexo_I.pdf [ Links ]
Authorship contribution: 1) Conception and design of study 2) Acquisition of data 3) Data analysis 4) Discussion of results 5) Drafting of the manuscript 6) Approval of the final version of the manuscript SMLE has contributed in 1, 3, 4, 5, 6. ES has contributed in 1, 3, 4, 5, 6. MM has contributed in 2, 6. P.M. has contributed in 2, 6. RA has contributed in 1, 3, 4, 6. AF has contributed in 2, 3, 4, 5, 6. FM has contributed in 3, 4, 6. P.M. has contributed in 3, 4, 6. BV has contributed in 2, 6. SP has contributed in 2, 6. LC has contributed in 2, 6. FP has contributed in 2. RP has contributed in 2. RS has contributed in 2. MG has contributed in 2.
Received: November 12, 2019; Accepted: March 10, 2020











 texto em
texto em