Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.22 no.36 Montevideo 2020 Epub 01-Dez-2020
https://doi.org/10.22592/ode2020n36a6
Translations
Perception of the oral health status of drug-dependent individuals
1Cátedra de Fisiología General y Bucodental, Facultad de Odontología, Udelar, Montevideo, Uruguay
2Cátedra de Odontopediatría, Facultad de Odontología, Udelar, Montevideo, Uruguay
3Servicio de Registro y Admisión de Pacientes, Facultad de Odontología, Udelar, Montevideo, Uruguay
4Programa APEX- Cerro, Udelar, Montevideo, Uruguay
5Programa APEX, Udelar, Montevideo, Uruguay
6Facultad de Odontología, Udelar, Montevideo, Uruguay
7Programa Minessota y Junta Nacional de Drogas (Presidencia de la República), Montevideo, Uruguay
General objective:
To determine the perception of adolescents and young adults regarding drug abuse as a result of drug dependence.
Materials and methods:
a qualitative research model was proposed. The theoretical sample by saturation included adolescents and young adults treated at Portal Amarillo. Inclusion criteria: a) aged between 15 and 24, b) in treatment for drug use. Exclusion criteria: a) non-lucid patients, b) non-collaborating patients.
Results:
Participants viewed oral health as having clean, white and aligned teeth; and caries, bleeding gums and communicable diseases as disease; chewing, aesthetics and taste were seen as altered functions. Before drug dependence, their oral hygiene was regular, after meals, and following the instructions received. With addiction, hygiene became irregular, only if they remembered to do it and without instruction reinforcement. Before drug consumption, participants were students or held a job; they had a good family life, with a partner, or in search of one. After consumption, they report self-marginalization, loss of contact with partners and children, isolation from the family, and social discrimination. Consumption makes it difficult for them to seek dental care, except in emergency situations.
Conclusions:
Young people in treatment for drug dependence are aware that addiction damages oral health, deteriorating aesthetics, affecting oral functions, self-esteem, and quality of life.
Keywords: oral health; drug dependence; adolescent; young adult
Objetivo general:
conocer la percepción de adolescentes y adultos jóvenes vinculados al consumo abusivo de drogas a partir de la situación de dependencia.
Material y método:
se planteó un modelo de investigación cualitativo. La muestra teórica por saturación fue población adolescente y adulta joven que se asistió en régimen de internación en el Portal Amarillo. Criterios de inclusión: a) tener entre 15 y 24 años, b) estar en tratamiento por consumo de drogas. Criterios de exclusión: a) pacientes no lúcidos, b) pacientes no colaboradores.
Resultados:
los participantes refieren como salud bucal tener los dientes limpios, blancos y alineados; como enfermedad caries, sangrado de encías y enfermedades transmisibles; y como funciones alteradas la masticación, la estética y el gusto. Antes de la situación de dependencia la higiene bucal era regular, después de las comidas y con instrucción recibida, a partir de la dependencia la higiene fue muy irregular, si se acordaban y sin refuerzo de la instrucción. Previo al consumo eran individuos integrados al estudio o al trabajo, con vida familiar ordenada, con pareja o en procura de tenerla; posteriormente al consumo relatan automarginación con pérdida de contacto con la pareja e hijos, aislamiento de la familia y discriminación social. El consumo dificulta el acceso a la atención odontológica, excepto en situaciones de urgencia.
Conclusiones:
Las personas jóvenes en tratamiento por dependencia a las drogas perciben el deterioro de su salud bucal a partir de la situación de consumo, alterando la estética, las funciones orales, la autoestima y la calidad de vida.
Palabras clave: salud bucal; drogodependencia; adolescente; adulto joven
Introduction
According to the World Health Organization (WHO): “A drug is any therapeutic substance or not that, introduced into the body by any route of administration (inhalation, ingestion, friction, parenteral, intravenous administration), produces an alteration, in some way, of the natural functioning of the central nervous system of the individual, and it is also capable of creating psychological, physical dependence or both.”1
The use of psychoactive substances (PAS), commonly known as psychoactive drugs, can alter consciousness, mood, or the individual's thinking processes.2 Many of these substances have been used in humankind's history for religious, cultural, recreational, and medicinal purposes. Whether legal or illegal, natural or synthetic, all substance use carries risks that vary according to age, sex, forms, frequency of use, personal contexts, and circumstances.3 Substance abuse refers in general to problems related to the use of PAS.4)
There are different consumption patterns, including experimental, occasional, and regular; there are even abuse and dependence cases. Any type of consumption can be problematic.3 Initially, upbeat and pleasant effects prevail when consumption is under control.5-6 The motivation for consumption changes gradually in some people and the amount of substance and dose frequency increases as a way to experience pleasure or avoid discomfort. Finally, a percentage of the population loses control, becomes compulsive, and unable to abandon drugs despite being aware of the consequences.6 Drug consumption is a form of consumption that poses more significant risks due to the combination of various PAS.7 Consumption patterns vary according to the drug market's supply, the search for change and the relational context.8
Drug abuse has been defined as “the persistent or sporadic excessive drug use inconsistent with or unrelated to acceptable medical practice”.4 The term medication dependence was extended to the concept of drug dependence.9 The WHO recommended replacing the term drug addiction or drug habit by drug dependence, given the derogatory connotation of the term drug addict.
The global outlook for drug use is unclear because many people, who consume either occasionally or regularly, tend to use more than one substance simultaneously or alternately.10 The chain of consumption in adolescents frequently begins with alcohol and tobacco, followed by illicit drugs.11-12 The most commonly used illegal drugs are cannabis, amphetamine-type stimulants, opioids, and cocaine-related substances.10 Drug patterns include injection of opioids, amphetamines and cocaine derivatives, with the risk of contracting and transmitting communicable diseases.13
Current epidemiological situation in Uruguay
The Seventh National Survey on Drug Consumption among High School Students conducted in Uruguay in 2016 highlights: a) the high consumption of alcohol and energy drinks with a high caffeine content, followed by tobacco and marijuana, and to a lesser extent tranquilizers without medical prescription, cocaine, hallucinogens, and amphetamine-type stimulants.14
The risk perception indicators included in this survey, according to student statements, identify the perception of high risk as a protection factor. In contrast, a low perception of risk increases the probability of the use/abuse of some substances. In general, it was found that the substances associated with lower risk were alcohol, tobacco, and marijuana, both in occasional and frequent consumption.14
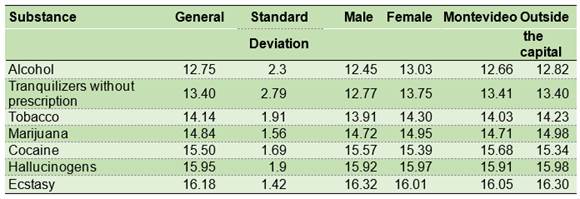
The mean age of consumption onset varies with sex, substance, and residence (Montevideo and outside the capital). (Table 1) 14
Table 1: Mean consumption starting age by substance according to sex and area of residence. High school students. Uruguay Survey 2016 (%) 14
The Sixth National Household Survey on Drug Consumption showed that males had a higher prevalence of consumption than women at all age ranges. However, the gap is smaller in the younger population, except for the use of tranquilizers, hypnotics, and antidepressants with or without medical prescription.15
The Government of Uruguay passed a law in 2013 to regulate the growth, production, sale, and recreational consumption of cannabis. Since then, the government has enacted other decrees and ordinances concerning the application of regulations on specific elements such as the medicinal use of cannabis, marketing, and sale for recreational use in pharmacies, and the inclusion of recreational consumers in a register.7
People who use substances are mostly young, ranging between 16 and 25 years old, with the onset and public manifestation of that behavior increasingly early, and even before the age of 14. Problematic consumption presents risk factors and protective factors. Risk factors include the normalization of consumption among youngsters, the limited control of the educational system that leads to dropping out of formal education, the lack of personal projects aggravated by social marginalization.16
The UNODC World Drug Report of 2009 indicated that most people began using drugs in their youth. Young people could respond to changes in drug availability or social perceptions of consumption to a greater extent than adults. In addition, the early onset of consumption increases the risk of negative social and health consequences along with an increased risk of committing felonies or crimes under the influence of drugs or of getting money to buy them.17
The consumption of PAS affects all areas of health: social, biological, psychological, cognitive, emotional, and cultural.18 According to the American Academy of Pediatric Dentistry (AAPD), drug abuse frequently coexists with psychiatric conditions such as depression, anxiety, attention deficit, challenging behavior, bipolar disorder, post-traumatic stress, bulimia nervosa, social phobia, and schizophrenia.19
It has also been observed that illegal drug use has a negative impact on hygiene habits and the prevalence of decay, gingivitis, and periodontitis compared to the general population.20-25
The protective factors for the regular use and dependence on drugs include the subject's qualities (attributes, self-esteem, life projection), which play a significant role; the family, its constitution and the role of its members; and the stability of social ties (educational-work, cultural, family, partner).16
Health is considered a dynamic event known as health-disease-care-process (HDCP). The HDCP representations in young people include the oral component as part of general health, not only for physical pain but also for its aesthetic importance.26 Oral health is closely related to people's overall health status and quality of life, as it may affect oral functions and social interactions. For example, tooth decay can cause poor chewing, decreased appetite, sleep problems, and reduced school and work performance.27
Oral health is multifaceted and includes, among other aspects, the ability to speak, smile, smell, taste, touch, chew, swallow, and show a series of emotions through facial expressions.28
A study conducted in Cartagena de Indias, Colombia, showed a negative impact on the quality of life related to oral health in young adults due to losing teeth, by having less than 19 teeth, root debris, tartar accumulation, and absence of health care services.29
This study's general objective was to determine the oral health status perception of adolescents and young adults in drug dependence treatment.
Specific objectives:
a) to determine the knowledge of the health-disease-care process and expectations about the oral health status.
b) to identify problems of access to dental care services in the target population.
2. Materials and methods
A qualitative research model was used. The techniques used were personal interviews and focus groups of young people who were in-patients at the Portal Amarillo Center during the three months of fieldwork. This institution has been the Uruguayan National Reference Center of the Drug Network since 2006, combining outpatient treatment, daily and residential center for the care of patients covered under the State Health Services Administration (ASSE).30 The COREQ guide (consolidated criteria for reporting and publishing on qualitative research) and the checklist according to the three domains:
Exclusion criteria:
A total of 18 interviews were carried out, and three discussion groups were formed, with 32 participants.
The interview was scripted based on a pilot experience in a previous stage with people treated at the Portal Amarillo Center. In this last experience, the research team members were also calibrated in their interviewer or observer roles.
All the activities were recorded without disclosing the names of the participants. Their attitude and interest in the interview were also registered.
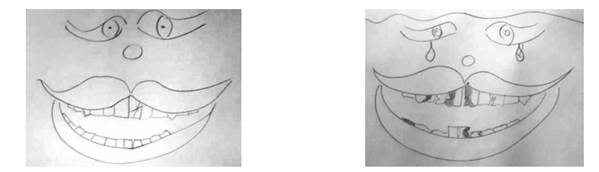
When the subjects' interest turned into boredom, fatigue, or silence, it was necessary to resort to a complementary strategy, using another tool, since the interviews lasted between 15 and 20 minutes. In this sense, they were asked to draw their mouths in a state of health and illness, under the sole supervision of educators. The research team members described and classified the drawings.
For the analysis of the recorded information, the data obtained was transcribed, organized, and ordered. Categories and subcategories were created from the recorded texts to analyze the statements.
Individual perception of oral health status was studied before and after the drug dependence period according to each subject's memory and representations.
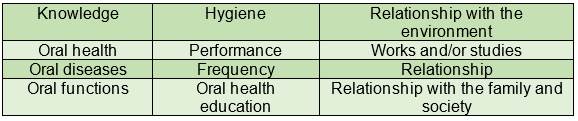
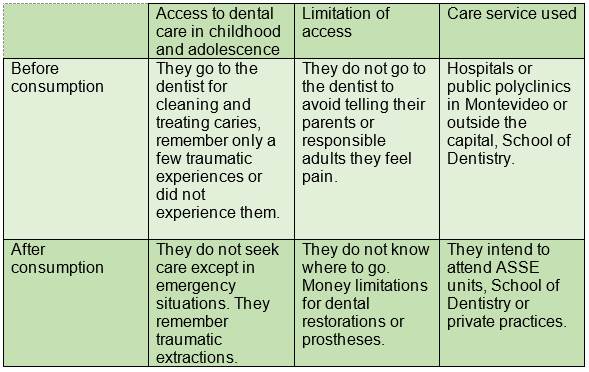
The categories that emerged after examining the recordings' text were hygiene and relationship with the environment. Subcategories are derived from these and are listed in Chart 1.
Ethical considerations: The research protocol was approved by the Research Ethics Committee of the School of Dentistry, file number 315/16. Participants were informed of the aims of the research and asked to sign the consent. They were assured of the absolute privacy and anonymity of the data collected.
3. Results
The following findings were obtained from the qualitative data collected and analyzed and the information collected from the medical records of the 32 patients.
The mean age of the subjects was 20 years old with a predominance of young men in rehabilitation at the Portal Amarillo Center, in agreement with epidemiological data found in the same care center that can probably be extrapolated to other populations of similar characteristics.30-31
According to data collected from the medical records, the primary substances underlying the study subjects' hospitalization were marijuana and cocaine paste, followed by cocaine hydrochloride, alcohol, nicotine, hallucinogens, psychoactive drugs, and “bazuco” (a type of crude cocaine paste).
The interviews conducted individually were shorter than originally planned. The answers were brief, with manifestations of boredom and difficulty in formulating the sentences. In the focus groups consisting of 4 to 5 individuals each, all participants contributed and respected each other's intervention. Some subjects' participation was longer and others were shorter, giving rise to convergent responses and comments to those expressed in the individual interviews.
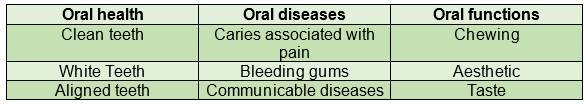
Considering the "knowledge" category, the following results on health, disease, and oral functions were found (Chart 2).
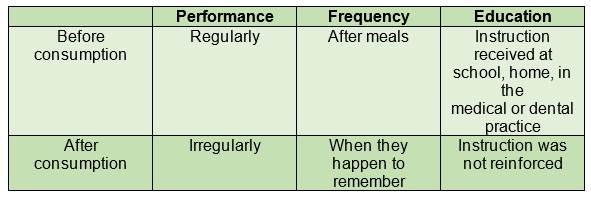
Under the "hygiene" category, the results on performance, frequency, and education received are listed in Chart 3.
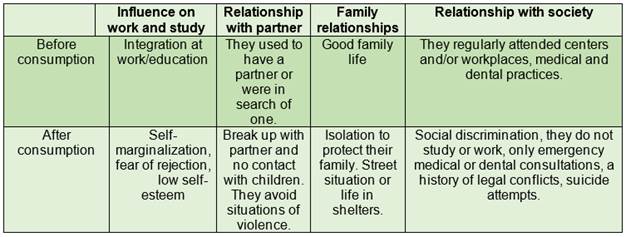
The following results were found for the category "relationship with the environment" regarding influence in work and study, relationship with partner, family, and social relationships before and after consumption. (Chart 4)
The participants' knowledge of oral health-disease was related to whiteness, correct alignment, and cleaning of teeth. The best-known oral diseases were dental caries, bleeding gums, and communicable infectious diseases such as HIV and syphilis. According to their stories, the most affected oral functions were chewing, aesthetics, and taste from the usual consumption PAS.
Regarding oral hygiene, it was noted that before drug dependence, they performed it regularly after the main meals and received oral and dental hygiene instructions at home, in school or medical or dental practices. After drug dependence, hygiene became irregular, only done when remembered, and their knowledge regarding the subject was not reinforced.
Regarding the relationship with the environment before the onset of problematic consumption, subjects were in school or had a job; they had a partner or were searching for one. They regularly attended teaching centers and/or workplaces and visited medical and dental practices. After substance abuse, they manifested self-marginalization events due to fear of rejection, low self-esteem, break-ups with their partner, or no contact with their children, if they had them, to avoid situations of violence. They also opted for isolation from their family to protect their loved ones, living in the streets or shelters, in addition to giving up medical or dental care when feeling marginalized or discriminated against, having suicide attempts and legal problems that could lead to police custody.
Regarding access to dental care, differences are recognized before and after PAS addiction. (Chart 5)
Before drug consumption, access to dental care was done regularly and based on preventive criteria, possibly curative, preferably in public health care services or at the School of Dentistry. Once they became dependent on PAS, health care became sporadic and only in emergency cases, with sedative or surgical therapies, often traumatic for the patient. They report a desire to improve their oral health status, although costs and lack of resources are obstacles.
There follow the results of the drawings made under the supervision of educators and without research team members. For the analysis, we considered the work of Paul Ekman and Freitas-Magalhaes as a reference to interpret the smile as body language that shows "the inner soul".32-33 Three groups are distinguished in the images: the first with brightly colored smiles in red, pink or even with yellow hues, showing cheerful, open mouths, with teeth, and sometimes flowers such as roses.
Another group showed smaller, sad, gray smiles (black and white).
The third group also drew in black and white using some shade of red and green. Smiles with eyes, noses, hearts, elephants, legs, flowers, and tears on the face when the mouth is damaged can be observed.
The drawings of mouths with alterations show missing teeth, caries represented by dark spots, yellow tooth pigmentations, chapped lips (Figs 1,2,3).
4. Discussion
The analysis performed based on the grounded theory, through constant comparison, allowed researchers to reach similar results to other studies carried out in which individuals undergoing drug dependence perceive a deterioration of their oral health due to substance abuse. On the other hand, it contrasts with studies that analyze young people's perception without drug dependence.
Therefore, the results of the target population undergoing drug dependence differ from research carried out in children and adolescents with no consumption reported in the region of Navarra, Spain, in 2007. That research indicated that the subjective perception of oral health was good, attendance to a dental practice in the previous year was high, with more than one daily oral brushing, and belief in the need for some dental treatment, such as orthodontics among adolescents.34
According to another qualitative study conducted in Australia with patients in drug consumption treatment, knowledge about access to oral health services was limited, and the search for care occurred only in emergency situations, without adequate health promotion, similar to the findings of this study.35
According to a multicenter study conducted in a general population over 18 years of age not hospitalized in the cities of Santiago, Tucumán, and Porto Alegre, the frequency of brushing, interdental hygiene and regular preventive dental consultation are essential indicators of gingival health, while the self-report of gingival bleeding is an indicator of the disease, also agreeing with our findings.36
Another study carried out in the State of São Paulo, Brazil, agrees with this one, in the sense that the interviewed school adolescents related their perception of oral health with hygiene, aesthetics or appearance, and regular dentist appointments.37
According to quantitative and qualitative studies carried out in Tacuarembó, Uruguay, the consequences of drug use also included general health problems; family, neighborhood, and labor conflicts; situations of insecurity, and social violence that could lead to legal problems.16
5. Conclusions
Young people in drug dependence treatment are aware that addiction damages their oral health, deteriorating aesthetics, and affecting oral functions and self-esteem. The oral health status reduces the quality of life of young drug users, making them more vulnerable and discriminated against by society.
The knowledge of oral health that these young people have is limited to caries, gingivitis, and orally transmitted diseases, mainly sexually transmitted infections.
As for the affected oral functions, they are mainly related to chewing, taste, and aesthetics.
Dental care was associated with emergency situations in public services and in the School of Dentistry, without complying with periodic check-ups.
It would be advisable to propose strategies for dentists and their teams to pay special attention to the prevention and promotion of health among these subjects as part of the drug dependence treatment.
Acknowledgments:
This research was authorized by the Board of Portal Amarillo.
REFERENCES
1. WHO 2016. Organización Mundial de la Salud. Disponible en: http://www.who.int/es/ [ Links ]
2. Organización Panamericana de la Salud. Neurociencia del consumo y dependencia de sustancias psicoactivas. Washington: Organización Mundial de la Salud; 2004. Disponible en: https://www.who.int/substance_abuse/publications/neuroscience_spanish.pdf [ Links ]
3. Uruguay. Junta Nacional de Drogas. Drogas: más información menos riesgos. 11ª ed. Montevideo: IMPO; 2016. [ Links ]
4. CEF. Comité de Expertos de la OMS en Farmacodependencia: Serie de informes técnicos, Nº 915-33º-Informe-OMS (2003). Disponible en: apps.who.int/medicinedocs/es/d/Js4898s/ [ Links ]
5. Pereira T. Neurobiología de la adicción. Rev Psiquiatr Urug. 2008; 73 (1): 9-24. [ Links ]
6. Organización de los Estados Americanos. El problema de las drogas en las Américas: Estudios drogas y salud pública. Washington: Organización de los Estados Americanos; 2013. Disponible en: http://www.cicad.oas.org/drogas/elinforme/informeDrogas2013/drugsPublicHealth_ESP.pdf [ Links ]
7. Oficina de las Naciones Unidas contra la Droga y el Delito. Resumen, conclusiones y consecuencias en materia de políticas: Informe Mundial sobre las Drogas 2017. Viena: UNDOC; 2017. Disponible en: https://www.unodc.org/wdr2017/field/WDR_Booklet1_Exsum_Spanish.pdf [ Links ]
8. Sánchez Antelo V. La dimensión temporal del consumo de drogas: análisis sociológico desde una categoría clave para el estudio de los procesos de salud-enfermedad-atención-cuidado. Salud Colec. 2016; 12 (1): 41-54. [ Links ]
9. Berruecos Villalobos L. Drogadicción, farmacodependencia y drogodependencia: definiciones, confusiones y aclaraciones. Cuicuilco. 2010; 17 (49): 61-81. [ Links ]
10. Oficina de las Naciones Unidas contra la Droga y el Delito. Informe Mundial sobre las Drogas 2016. New York: UNDOC; 2016. Disponible en: https://www.unodc.org/doc/wdr2016/V1604260_Spanish.pdf [ Links ]
11. Toledo M. Perfil clínico epidemiológico de adolescentes consumidores de drogas en el Hospital Hermilio Valdizan. Rev. de Psiqu. Salud Mental Hermilio Valdizan. 2003; 4 (1): 19-28. [ Links ]
12. Ortega-Pérez CA, da Costa-Júnior ML, Pereira Vasters G. Perfil epidemiológico de la drogadicción en estudiantes universitarios. Rev. Latino-Am. Enfermagem. 2011; 19: 665-72. [ Links ]
13. Degenhardt L, Peacock A, Colledge S, Leung J, Vickerman P. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV and HCV in people who inject drugs: a multistage systematic review. The Lancet Global Healt. 2017; 5 (12): e 1192- e1207. Disponible en: https://www.thelancet.com/lancetgh vol5 december 2017 [ Links ]
14. Uruguay. Junta Nacional de Drogas 2016. VII Encuesta nacional sobre consumo de drogas en estudiantes de Enseñanza Media -2016 https://www.gub.uy/jnd/comunicacion/publicaciones/vii-encuesta-nacional-sobre-consumo-de-drogas-en-estudiantes-de [ Links ]
15. Uruguay. Junta Nacional de Drogas. (2016) VI Encuesta Nacional en Hogares sobre Consumo de Drogas. Disponible en: https://www.gub.uy/junta-nacional-drogas/sites/junta-nacional-drogas/files/documentos/publicaciones/201609_VI_encuesta_hogares_OUD_ultima_rev.pdf [ Links ]
16. Steffano D. Diagnóstico sobre el consumo de drogas en la zona del centro de la ciudad de Tacuarembó-Departamento de Tacuarembó. CICAD- OEA. JND. Junta Departamental de Drogas de Tacuarembó. [ Links ]
17. Oficina de las Naciones Unidas contra la Droga y el Delito. Informe Mundial sobre las Drogas 2009. Nueva York: UNDOC; 2009. Disponible en: https://www.unodc.org/documents/wdr/WDR_2009/World_Drug_Report_2009_spanish.pdf [ Links ]
18. Muñoz Astudillo MN, Gallego Cortes C, Wartski Patino CI, Álvarez Sierra LE. Familia y consumo de sustancias psicoactivas: una búsqueda de lo ausente.Index Enferm, online. 2012; 2 (3): 136-140. [ Links ]
19. American Academy of Pediatric Dentistry. Policy on substance abuse in adolescent patients. Reference manual. 2016; 39 (6): 17-18. [ Links ]
20. Barrios CE, Vila VG. Estado de salud bucodental en consumidores de marihuana. Rev. Fac. Odon. 2009; 2 (1): 30-35. [ Links ]
21. Brown C, Krishnan S, Hursh K, Yu M, Johnson P, Page K, Shiboski CH. Dental disease prevalence among methamphetamine and heroin users in an urban setting: a pilot study. J Am Dent Assoc. 2012; 143: 992-1001. [ Links ]
22. Gigena PC, Bella MI, Cornejo LS. Salud bucal y hábitos de consumo de sustancias psicoativas en adolescentes y jóvenes drogodependientes en recuperación. Odontoestomatología 2012; 14(20): 49-59 [ Links ]
23. Gupta T, Shah N, Mathur VP, Dhawan A. Oral health status of a group of illicit drug users in Delhi, India. Community Dental Health. 2012; 29(1): 49-54. [ Links ]
24. Rotemberg E, Salveraglio I, Piovesán S, Kreiner M, Smaisik K, Ormaechea R, Varela A. Estado dental y periodontal de población en tratamiento por consumo de drogas. Estudio piloto. Odontoestomatología. 2015; 17 (25): 34-39. [ Links ]
25. Chaparro-González NT, Fox-Delgado MA, Pineda-Chaparro RT, Perozo-Ferrer BI, Díaz-Amell AR, Torres-Quintero VC. Manifestaciones bucales y maxilofaciales en pacientes con adicción a las drogas. Odontoestomatología . 2018; 20 (32): 24-31. [ Links ]
26. Barnetche MM, Cornejo LS. Calidad de vida y proceso salud enfermedad atención a nivel del componente bucal de jóvenes alojados en centros socioeducativos del Área Penal Juvenil de la Provincia de Córdoba. Tesis de Doctorado. Facultad de Odontología. Universidad Nacional de Córdoba, 2017. [ Links ]
27. Federación Dental Internacional. Salud buco-dental y calidad de vida. Bankok: FDI; 2015. Disponible en: https://www.fdiworlddental.org/es/resources/policy-statements-and-resolutions/salud-bucodental-y-calidad-de-vida [ Links ]
28. Federación Dental Internacional. FDI´s definition of oral health. Enero, 2019. Disponible en: https://www.fdiworlddental.org/oral-health/fdi-definition-of-oral-health [ Links ]
29. Díaz- Cárdenas S, Meisser-Vidal MA, Tirado-Amador LR, Fortich-Mesa N, Tapias-Torrado L, González-Martínez FD. Impacto de salud oral sobre calidad de vida en adultos jóvenes de clínicas odontológicas universitarias. Int. J. Odontostomat. 2017; 11 (1): 5-11. [ Links ]
30. Triaca J, Cardeillac V, Idiarte Borda C. Características de los primeros usuarios que consultaron en el Centro de Referencia Nacional de la Res Drogas Portal Amarillo. Rev Psiquiatr Urug. 2009; 73 (1): 37-48. [ Links ]
31. Riva R, Rotemberg E, Sanguinetti M, Rodríguez A, Massa F. Drogodependencia, Bruxismo y Trastornos Témporo-Mandibulares. Análisis comparativo en dos poblaciones: muestra nacional y población en tratamiento por consumo problemático de drogas en Portal Amarillo Odontoestomatología. 2014; 16 (24): 26-33. [ Links ]
32. Ekman P, Friesen WV . Manual for the Facial Action Code. Palo Alto, CA: Consulting Psychologist Press; 1978. [ Links ]
33. Freitas-Magalhães A Facial expression of emotion. In V. S. Ramachandran (Ed.), Encyclopedia of Human Behavior Vol. 2, 2012. 173-183. [ Links ]
34. Artazcóz J, Cortés FJ, Rosel E, González Rodríguez P, Bravo M. Percepción y hábitos de salud bucodental en niños y adolescentes de Navarra 2007 An Sist Sanit Navar. 2010; 33 (1): 51-64. [ Links ]
35. Cheah Alison Li Sun, Pandey Ram, Daglish Mark, Ford Pauline J, Patterson Sue. A qualitative study of patients' knowledge and views of about oral health and acceptability of related intervention in an Australian inpatient alcohol and drug treatment facility. Health Soc Care Community. 2017; 25(3): 1209-1217. [ Links ]
36. Gómez MV, Toledo A, Carvajal P, Gomes SC, Costa RSA, Solanes F, Oppermann SV, Rosing CK, Gamonal J, Romanelli H. A multicenter study of oral health behavior among adult subject from three South American cities. Braz. Oral Res. 2018; 32:e22. [ Links ]
37. Saliba-Garbin CA, Isper-Garbin AJ, Moreira-Arcieri R, Saliba NA, Goncalves PE. La salud bucal en la percepción del adolescente. Rev Salud Pública. 2009. 11 (2): 268-277. [ Links ]
Note of republication: This article is a republication from: Rotemberg E, Salveraglio I, Piovesán S, Almaráz M, Ferreira B, Smaisik K and Mazzuco M. Percepción del estado de salud bucal de adolescentes y adultos jóvenes en tratamiento por drogodependencia. J Oral Res 2019; 8(5): 378-385. Disponible en: https//revistas.udec.cl/index.php/journal_of_oral_research/article/view/1877
Note financial support: study funded by the Uruguayan Society for Dental Research (SUIO) after obtaining the first prize for a research project at SUIO's 12th Annual Meeting held in Montevideo in August 2017. All co-authors declare no conflict of interest with the subject matter.
Authorship contribution: 1. Conception and design of study 2. Acquisition of data 3. Data analysis 4. Discussion of results 5. Drafting of the manuscript 6. Approval of the final version of the manuscript ER has contributed in 1, 2, 3, 4, 5, 6. SP has contributed in 1, 2, 3, 4, 5, 6. IS has contributed in 1, 2 y 4. MTA has contributed in 1 y 2. BF has contributed in 1 y 2. KS has contributed in 1 y 2. MCM has contributed in 1,2 y 4.
Received: June 19, 2020; Accepted: June 19, 2020











 texto em
texto em