Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.13 no.1 Montevideo 2024 Epub June 01, 2024
https://doi.org/10.22235/ech.v13i1.3220
Original Articles
Evidence for the Treatment of Wounds in Newborns: An Integrative Review
1Universidade Federal da Bahia, Brasil, josielson.silva@ufba.br
2Universidade Federal da Bahia, Brasil
3Instituto Federal da Bahia, Brasil
4Universidade Federal de São Paulo, Brasil
5Universidade Federal da Bahia, Brasil
6Universidade Federal da Bahia, Brasil
Introduction:
Given the particularities and challenges in the management and treatment of wounds in newborns, it becomes important for nurses to know, indicate and evaluate the efficacy and safety of dressings and products, even in the analysis of products for the neonatal population.
Objective:
To identify in the literature the main dressings and products used to treat wounds in newborns.
Methodology:
This is an integrative literature review, with articles published between 2018 and 2022, which addressed the topics of dressings and products used in the treatment of wounds in newborns. Data collection was carried out through consultation in Biblioteca Virtual de Saúde and in the Scientific Electronic Library Online. The “newborn”, “wounds” and “bandage” descriptors were used. The analysis was carried out according to the PICO strategy and structured following PRISMA.
Results:
Given the findings, it was possible to identify 13 articles that addressed products and dressings intended for treating wounds in newborns. Fourteen types of dressings/products and devices that use negative pressure therapy were found.
Final considerations:
The literature indicates the use of products and dressings with passive, active and biological principles for the treatment of wounds in newborns, including premature neonates, and it is worth highlighting the importance of considering the safe use of dressings that are suitable for this population.
Keywords: newborns; wounds; dressings; nursing care
Introdução:
Diante das particularidades e desafios no manejo e tratamento de feridas em recém-nascidos torna-se importante para o enfermeiro conhecer, indicar e avaliar a eficácia e segurança das coberturas e produtos, inclusive na análise dos produtos para o público neonatal.
Objetivo:
Identificar na literatura as principais coberturas e produtos utilizados no tratamento de feridas em recém-nascidos.
Metodologia:
Trata-se de uma revisão integrativa de literatura, com artigos publicados entre os anos de 2018 a 2022, que abordaram os temas de coberturas e produtos utilizados no tratamento de feridas em recém-nascidos. A coleta de dados foi realizada por meio de consulta na Biblioteca Virtual de Saúde e Scientific Eletronic Library Online. Foram utilizados os descritores “newborn”, “wounds” e “bandage”. A análise foi realizada conforme a estratégia PICO e estruturados pelo PRISMA.
Resultados:
Diante dos achados foi possível identificar 13 artigos que abordavam produtos e coberturas destinados ao tratamento de feridas em neonatos. Foram encontrados 14 tipos de coberturas/produtos e dispositivos que utilizam a terapia por pressão negativa.
Considerações finais:
A literatura indica o uso de produtos e cobertura com princípios passivos, ativos e biológicos para o tratamento de feridas em neonatos, inclusive no prematuro, valendo destacar a importância em considerar o uso seguro de coberturas adequadas a esse público.
Palavras-chave: recém-nascidos; feridas; curativos; cuidado de enfermagem
Introducción:
Dadas las particularidades y desafíos en el manejo y tratamiento de heridas en recién nacidos, es importante que los enfermeros conozcan, indiquen y evalúen la efectividad y seguridad de apósitos y productos, incluido el análisis de productos para el público neonatal.
Objetivo:
Identificar en la literatura los principales apósitos y productos utilizados para el tratamiento de heridas en recién nacidos.
Metodología:
Se trata de una revisión integrativa de la literatura, con artículos publicados entre 2018 y 2022, que abordaron los temas de apósitos y productos utilizados en el tratamiento de heridas en recién nacidos. La recolección de datos se realizó mediante consulta en la Biblioteca Virtual en Salud y Biblioteca Científica Electrónica en Línea. Se utilizaron los descriptores “newborn”, “wounds” y “bandage”. El análisis se realizó según la estrategia PICO y estructurado por PRISMA.
Resultados:
Teniendo en cuenta los hallazgos, fue posible identificar 13 artículos que abordaron productos y apósitos destinados al tratamiento de heridas en recién nacidos. Se encontraron 14 tipos de revestimientos/productos y dispositivos que utilizan terapia de presión negativa.
Consideraciones finales:
La literatura indica el uso de productos y coberturas con principios pasivos, activos y biológicos para el tratamiento de heridas en recién nacidos, incluidos los prematuros, y cabe resaltar la importancia de considerar el uso seguro de coberturas adecuadas para esta población.
Palabras clave: recién nacidos; heridas; apósitos; cuidado de enfermería
Introduction
The skin is the largest human organ and performs several functions. The three layers that make up the skin organ, known as epidermis, dermis and hypodermis, are attached to and supported by the subcutaneous tissue. The epidermis, the outermost layer, consists of the stratum corneum responsible for preventing loss of fluids and protecting against the invasion of harmful agents, as its function is of a barrier and protective agent for the skin, as well as preventing transepidermal loss of fluids. (1,2
In turn, the dermis is made up of collagen and elastin fibers that provide support, elasticity and resistance to the skin. (1 These characteristics can vary according to each person’s age since, when compared to adult skin, the dermis of Newborns (NBs) has fewer elastic fibers. In addition to that, NBs have a more immature and deficient dermoepidermal junction, in addition to greater permeability related to their greater body surface in comparison to their weight. For these reasons, they are at a higher risk of developing injuries and absorbing chemical agents, as well as a greater percutaneous reaction to irritating substances. 3
NBs’ skin requires careful and continuous evaluation because, in addition to representing the body surface, it is one of the criteria for evaluating their maturity according to gestational age and skin appearance. Thus, premature infants have thin and gelatinous skin whereas full-term ones have smoother skin, with a shiny and moist appearance. Finally, post-term neonates may have dry, wrinkled skin with apparent peeling. For physiological purposes, the skin has a direct relationship with thermoregulation and guarantees vitality at birth. 1
It is important to maintain newborns’ skin integrity since, in addition to essential thermoregulation for extrauterine adaptation, it also acts as a protective barrier for the body. Preserving its natural protective functions can prevent the emergence of infections caused by disruption of the epithelial tissue. In this context, nurses develop fundamental actions in the prevention and treatment of wounds; considering that these professionals work directly in the assessment of skin integrity, as well as in the care and dressing of wounds in newborns, mainly in the hospital setting. 2
Some studies point to the incidence and prevalence of wounds in the neonatal population, with emphasis on those that affect newborns when hospitalized: wounds resulting from congenital malformations; 3 dermatitis associated with diaper use; 2 drug infiltrations and extravasations; traumatic injuries evidenced by hematomas, erythemas, abrasions and ecchymosis; oximeter burns; and pressure injuries related to clinical devices in Intensive Care Units (ICUs). Most of these harms can be prevented, oftentimes resulting from unplanned care. 2,3,4
Although various studies address preventive measures for the emergence of wounds in the neonatal population, 1,2,3) there is no standardized consensus for treating them. The existing data are still limited for newborns; therapeutic approaches are based on evidence for adults, which makes wound treatment difficult and/or compromised in such a specific population group, in addition to scarce guidelines for neonatal skin care, which limits adherence to best management practices for neonatal skin ruptures. 5
The literature describes some efficient dressings for treating wounds in newborns, but with weaknesses considering that the vast majority of these products were developed for use in the adult population, making it necessary to pay attention to patient safety as a guiding principle in Neonatology care, taking as first ground the objective of not causing harm.3,6,7) Furthermore, there is also no standard for comparing the benefits of different types of dressings in relation to each other, in addition to the associated pain levels, clinical assessment, or presence of infection required for treatment planning. Finally, the gaps in the literature point to the need to carry out more prospective studies that seek to evaluate safety of these products in Neonatology. 5
Thus, this study aims at identifying in the literature the main dressings and products used for the treatment of wounds in newborns.
Methodology
Type of study
This integrative review study aims at systematizing and analyzing the results obtained from publications in scientific electronic databases from 2018 to 2023 in order to include the most current materials in the literature.
Study selection
The review consisted of six stages. 1) Identification of the topic and choice of the research question to prepare the integrative review; 2) Indication of the sample inclusion and exclusion criteria; 3) Data collection, organization of the sample information; 4) Data evaluation and analysis; 5) Interpretation and discussion of results; and 6) Synthesis of the content and description of the results found in the analysis of the articles. 8
The PICO strategy was used for the selection and identification process of publications that answered the study guiding question, as follows: P = neonatal population (0-28 days), I = dressings and products used, C = non-intervention, and O = wound treatment.9) This study was guided by the following question: Which dressings and products have been recommended in the scientific literature for treating neonatal wounds?
The article selection process was carried out in Biblioteca Virtual de Saúde (BVS), which is part of the Medical Literature Analysis and Retrieval System (MEDLINE) and the Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS) bibliographic index, in addition to the Scientific Electronic Library Online (SCIELO). For the search process, the Descriptors in Health Sciences (Descritores em Ciências da Saúde, DeCS) were used, resulting in the following combinations: “newborn” AND “wounds” AND “bandage”; the entire search process took place in pairs by the research team involved in conducting this paper, with the findings validated by both participants.
Inclusion criterio
As inclusion criteria, original articles, case reports and update articles were adopted, which had full texts and were available for analysis, in any language, published from 2018 to 2023 and directly related to the study object. Clinical guides and protocols were excluded, as well as literature reviews and duplicate studies.
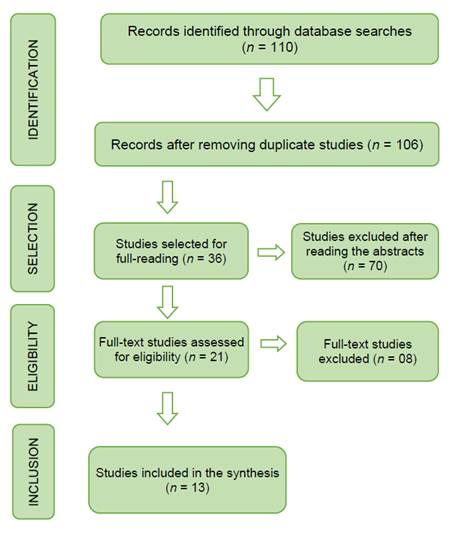
The data extraction process was systematized with the support of a previously prepared instrument, organized by internal and external indicators: author, title, year of publication, journal, objective, type of study and main findings. Thus, search and selection of the manuscripts was carried out through pair search, applying the PRISMA guideline. 10 At the end of this search, 110 articles were identified, of which 4 were excluded for being duplicates and 70 for not meeting the study inclusion criteria.
Initially, 36 publications were selected and subjected to a thorough reading process, of which 15 were discarded because they were not associated with the theme, with 21 remaining for the eligibility assessment. In the end, 08 articles were excluded for not responding to the objective proposed in this research, resulting in 13 manuscripts to comprise the synthesis of this review, according to the PRISMA flowchart 10 (Figure 1).
Results
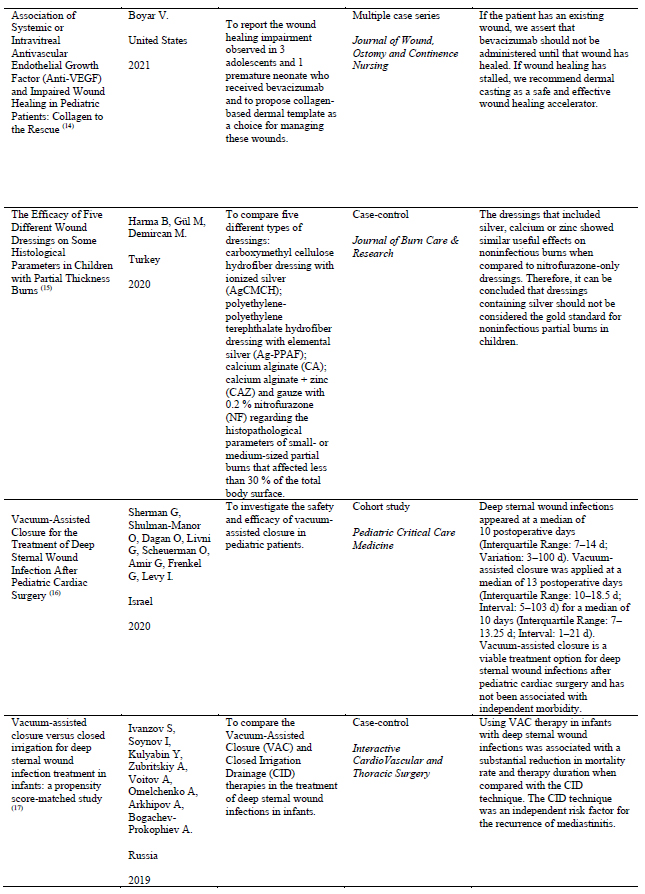
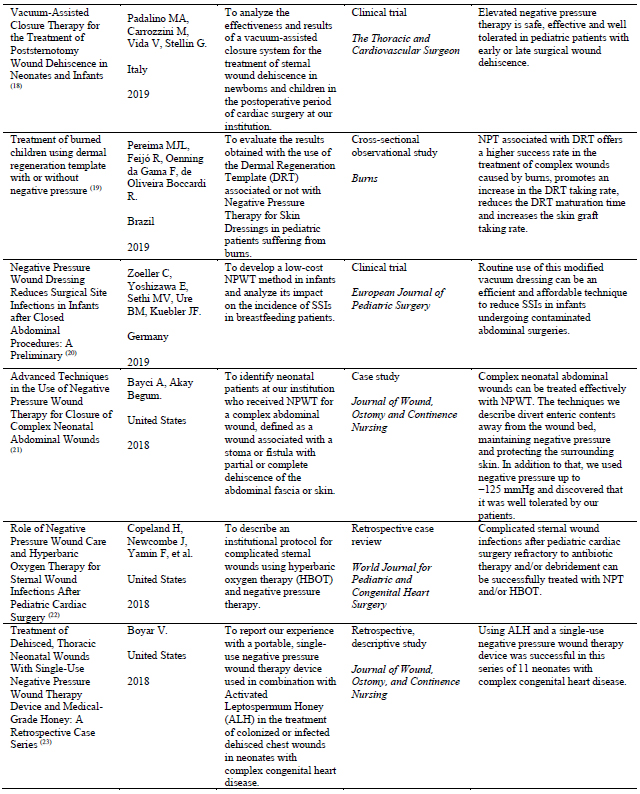
The sample was made up of 13 international articles and only one Brazilian publication on the topic. Depending on where the studies were carried out, four took place in the USA, two no Iran, one in Argentina, one in Turkey, one in Israel, one in Russia, one in Italy, one in Germany and one in Brazil. The review included four case reports, three clinical trials, two case-control intervention studies, three cross-sectional observational studies and one cohort study. The publications ranged from 2018 to 2022. Table 1 2,3 presents data from each study and the variables analyzed.
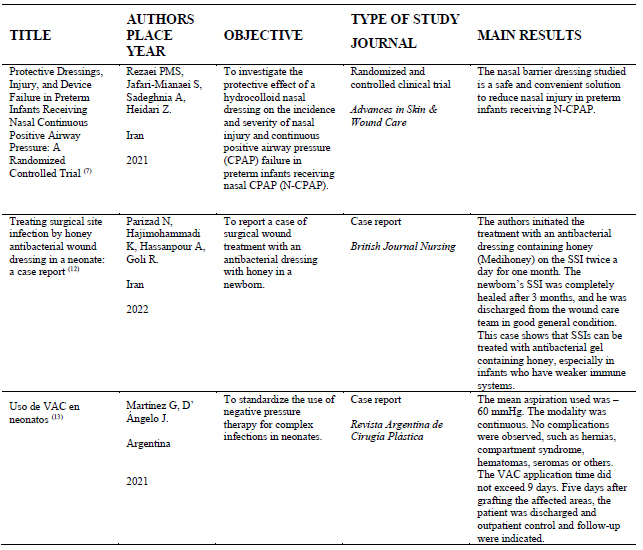
Table 1: Summary of the articles selected structured by title, authors, country, year, objectives, type of study and main results. Salvador, Bahia, Brazil, 2023
The articles included in this review evidenced the most common wounds that affect the neonatal population. Therefore, the total was 14 types of wounds reported in the studies, of which five studies referred to the treatment of complex congenital wounds, four to surgical wounds, three to burns, one study pointed to the treatment of injuries due to leaks and infiltration and one to device-related pressure injury. Figure 2 below stratifies the main complex injuries evaluated for treatments in newborns.
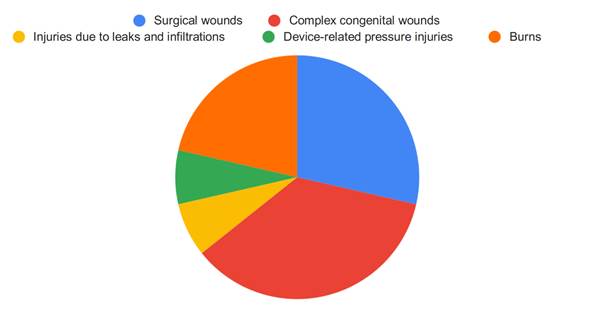
Figure 2: Main types of complex wounds that affect newborns according to the number of studies published in the 2018-2023 period, Bahia, Brazil, 2023.
The research made it possible to list 16 types of products or dressings associated or not with Negative Pressure Therapy (NPT), also cited as vacuum, used for the treatment of injuries in newborns. Table 2 describes the types of dressings and their classification according to the model proposed by Fan et al., 11 in addition to presenting the number of studies that reported their use and the types of wounds treated in the neonatal population.
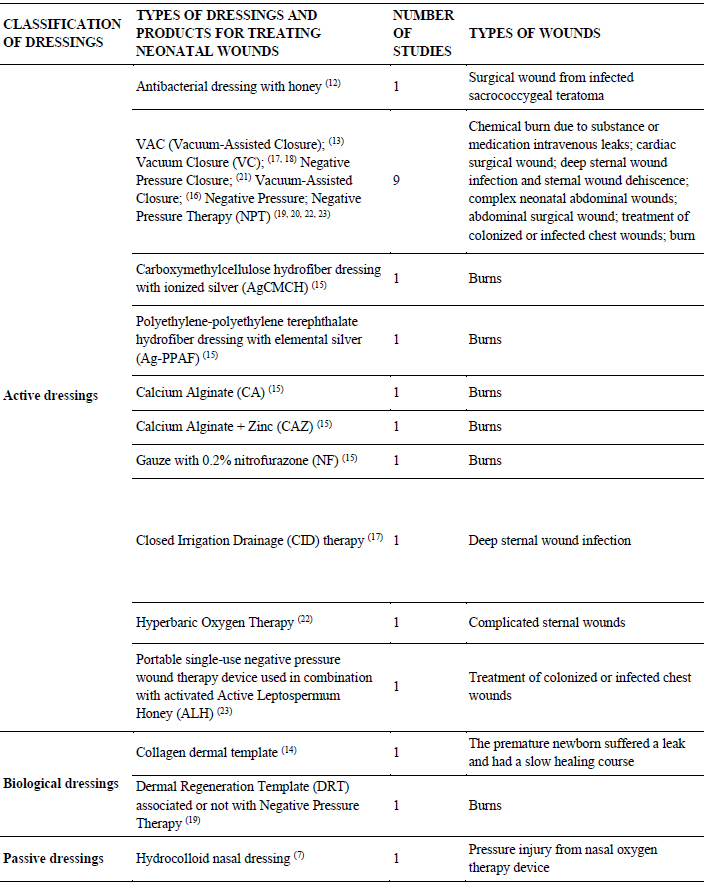
Table 2: Types of dressings and products used in the treatment of neonatal wounds structured according to the model proposed by Fan et al., 2011. 11 Bahia, Brazil, 2023
Discussion
Although the literature presents many publications on the treatment of wounds in the adult population, few studies were found involving the same theme in the Neonatology field, mainly in the area related to the safe use of dressings. Knowing the anatomy and physiology of newborns’ skin becomes an important aspect for planning safe and individualized care. Due to the peculiarities and sensitivities of this organ in newborns, the risks for percutaneous absorption of substances, infections and wounds are increased. Skin injuries expose newborns to infectious agents, which can not only cause death but also irreversible sequelae and scars. In this context, constant skin evaluation by nurses and/or a multiprofessional team becomes necessary to prevent and treat complex wounds in this population segment. 1,14
A study demonstrates the relevance of nurses’ work in the care (28), prevention and maintenance of newborns’ skin integrity. 1,2,3 However, the evolution of the care process, the dynamics and changes in habits and customs driven by the growing technological development in health have proposed gains in the treatment of wounds, mainly in the work of surgeons. 13,16,17,18,19,20,21,22,23 Therefore, the therapeutic process of this problem in newborns is still a challenge for the professionals who work in this context, which indicates both technical and educational investments.
The wounds that affect NBs can be congenital 22,23) and most of them result from the hospitalization process and/or neglected care, evidenced by pressure injuries, 7 dermatitis associated with diaper use, 2,4,5 infiltration and chemical leaks, 13,19 exposure to medical devices, 7 multiple invasive procedures and even surgical procedures to correct conditions.12,16,18,20,21,22
Thus, it becomes indispensable to invest in the in-hospital care process to minimize harms and risks to newborns, in addition to expanding knowledge on curative practices that accelerate the wound healing process in the neonatal population, contributing to reducing the hospitalization times and, consequently, the hospital costs. 24,25
Hospitalization units focused on neonatal patients leave them more vulnerable to errors. 19,25,26,27 Wounds caused by leaks of solutions or drugs can be frequent, mainly when dealing with neonates with a severe clinical profile that requires the use of vesicant and irritating drugs, in addition to parenteral nutrition.20,21,22
For this type of wound, the literature indicates using the vacuum grafting and healing method. 13 The use of Dermal Regeneration Template techniques, 19 in addition to carboxymethylcellulose hydrofiber dressing with ionized silver (AgCMCH), polyethylene-polyethylene terephthalate hydrofiber dressing with elemental silver (Ag-PPAF), calcium alginate (CA), calcium alginate + zinc (CAZ) and gauze with 0.2 % nitrofurazone (NF) were compared and proved to be effective, despite highlighting that dressings containing silver should not be considered as the gold standard for noninfectious partial burns in children. 15 Even so, all of them showed satisfactory wound healing responses, reducing necrotic tissue and increasing granulation tissue growth.
Hydrocolloid was indicated to prevent injuries caused by the use of a nasal oxygen therapy device. 12 However, it is known to have diverse uses in adult wounds; this material is recommended both as a preventive measure and as a dressing applied to the site. It is a carbohydrate polymer that both protects the wound and controls its exudation. Occlusion accelerates epithelialization, preserves the acute wound fluid under the occlusive bandage that contains substances, such as growth factors, stimulating the proliferation of fibroblasts and endothelial cells, promoting the formation of granulation tissue. 31
Another aggravating factor that affects newborns with wounds is exposure to infectious agents that can colonize the wound site, compromising the healing process and increasing the risk of a generalized infection capable of leading to death and, therefore, they should be strictly monitored. In this context, although little used in the Neonatology area, silver was instituted, even in premature newborns that had first-degree burns. 25,26 Silver is an excellent antimicrobial agent; however, this active ingredient can be systematically absorbed and cause hyponatremia and hypokalemia, in addition to nitrate being converted into nitrite with oxidizing power capable of damaging the cell. 27,28
In view of the above, the use of silver should be carefully indicated with possible monitoring and serum control. In the case of neonates, who commonly present hydroelectrolyte changes when seriously ill, there is an urgent need for professionals to monitor the electrolyte levels when this type of therapy is instituted, as well as strict control of any exchanges.
Another product recommended for the neonatal population with infectious wounds is calcium alginate. Although widely used in Neonatology, it should not be employed randomly and without adequate monitoring, as it releases sodium and calcium into the lesion bed, which can be absorbed systemically. 29 However, this passive dressing can accelerate debridement and maintain a physiologically moist microenvironment which allows gas exchange; in addition, it controls exudate and minimizes colonization by microorganisms, promoting healing and the formation of granulation tissue, requiring successive evaluations by the Nursing team. 30,31
According to a study carried out in Turkey, active products were used in the presentation of ointments, gels and solutions to treat injuries in this population group. Calcium Alginate (CA) and Calcium Alginate + Zinc (CAZ) 15 are cited, respectively, with important healing results such as stimulation of granulation tissue growth, maintenance of moisture and favoring exchanges, and debriding actions, as well as antibacterial activity in the treatment of burns.
Although incipient, the search for new products to treat wounds in newborns has been gaining prominence. Studies developed in Iran (12 and the United States 23) employed Leptospermum Honey, a type of honey with anti-inflammatory and antibacterial properties, effective even when used on multi-resistant bacteria such as methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa, in addition to promoting wound debridement. 12,23,24,28,30
In addition to being used in treatments, the dressings applied in the care of neonatal wounds stand out for their preventive action, mainly with regard to pressure injuries and friction caused by medical devices. 7,31 The market already offers a variety of carboxymethylcellulose hydrofiber dressings with ionized silver (AgCMCH), as well as polyethylene-polyethylene terephthalate hydrofiber dressings with elemental silver (Ag-PPAF), in addition to paraffin gauze and gauze with 0.2 % nitrofurazone (NF), cited in studies that use these resources in the therapeutic processes of burns 15,30,31 in the neonatal population. 29 Thus, foams and silicones act to control exudates, accelerate the epithelialization process through the occlusive system and can avoid routine dressing exchanges.
Some studies report that extensive wounds in neonates require innovative treatments such as the use of Dermal Regeneration Template (DRT) associated or not with Negative Pressure Therapy 19 and collagen dermal template. 14 These products consist of a piece of collagen-based tissue and were indicated for the treatment of premature newborns who suffered leaks and had a slow healing course, reducing inflammatory responses and promoting tissue growth and regeneration. DRT associated with NPT offers a higher success rate in the treatment of complex wounds caused by burns, promotes an increase in the DRT taking rate, reduces the DRT maturation time and increases the skin graft taking rate. A number of research studies conclude that skin allografts 5 are used in the treatment of large skin defects for temporary wound dressing, minimizing water, electrolyte, heat and protein losses and as a physical barrier against infections. 27
There is a strong association between dressings and products and other therapeutic modalities in the treatment of injuries, such as Negative Pressure Therapy (NPT). 19,25,26 Thus, several denominations and nomenclatures are used to highlight the use of this treatment, such as: CAV (cicatrización asistida por vacío); 13 Vacuum Closure (VC); 17,18 Negative Pressure Closure;21 Vacuum-Assisted Closure; 16 Negative Pressure; 25 and Negative Pressure Therapy (NPT). 19,20,22,23
These research studies indicate that NPT not only reduces biofilm formation in the wound bed but also accelerates the granulation tissue growth process, favoring wound closure. Diverse evidence shows that this therapy reduces edema and vascular permeability, in addition to increasing angiogenesis and blood flow to the wound borders. 19,25,26
In turn, the use of Hyperbaric Oxygen Therapy (HBOT) was found in a study 22 for the treatment of complicated sternal wound infections after pediatric cardiac surgery refractory to antibiotic therapy and/or debridement, which can be successfully treated with NPT and/or HBOT. The most common bacterium isolated from blood or wound cultures was Staphylococcus aureus.
Although not reported in the studies included in the review, physiological serum (0.9 %) is widely used in wound care because it has important properties that do not alter the healing process, do not damage tissues, and do not cause sensitivity reactions or allergies, in addition to not altering the normal bacterial flora of the skin. 28,29,30 Therefore, in the case of neonates, crystalloid solutions are more indicated.
Finally, it is worth noting the need for a thoughtful analysis of the conditions of neonatal patients, as well as the characteristics of the injuries that require treatment. 4,6,28 Thus, it is possible to establish a care plan that involves everything from adapting the most suitable dressing to implementing actions that guarantee safety in the treatment of wounds, as it is necessary to have products for health services suitable for Neonatology, without improvisations for skin hygiene, catheter fixation and hand hygiene products, 7,28,29,30 among other procedures that can prevent and treat wounds in Neonatology.
Study limitations
The study limitations consist in the use of specialized databases giving a more specific focus to the studies included in this review, which may be expanded according to a survey in multidisciplinary databases that allow the inclusion of international studies. The vast majority of the studies are presented through case reports, requiring other methodological designs involving the neonatal population, resulting in a survey that requires greater depth. In addition, it is noted that the inclusion of studies might expand the results by grounding subsequent studies that boost evidence for Neonatology and wound care.
Contribution of the study to the practice
The discussions considered in this integrative review result in a survey of the main useful dressings reported in the literature for the practice of professionals who work in the care of wounds in newborns. The products and dressings indicated to treat different types of wounds were characterized, in addition to reporting therapeutic modalities that assist nurses in decision-making, prescriptions and monitoring regarding dressings, seeking safe care for the neonatal population.
Final considerations
The study concludes that discussions about wound treatment practices in newborns are still incipient when compared to treatments aimed at the adult population. Different dressings and products contribute to satisfactory healing processes in newborns, including premature ones. Advances in the area already point to the use of innovative therapeutic modalities, resorting to different types of dressings for NBs.
Therefore, as a result of the incipient discussion regarding the safety of neonatal patients when treating wounds, it is worth noting the gap identified and its importance in considering the prevention of errors that result in injuries, as well as the safe use of adequate dressings for newborns in view of the composition of the products, in addition to the need for specific care measures such as serum monitoring of substances that might cause poisoning in this population segment.
REFERENCES
1. Albahrani Y, Hunt R. Newborn Skin Care. Pediatric annals. 2019 (acesso em 2023 fev 07);48(1):e11-e15. doi: 10.3928/19382359-20181211-01 [ Links ]
2. Grosvenor J, Dowling M. Prevention of neonatal pressure injuries. J Neonatal Nurs. 2018 (acesso em 2023 jul 07); 24(3);122-125. doi: 10.1016/j.jnn.2017.09.004 [ Links ]
3. Johnson E, Hunt R. Infant skin care: updates and recommendations. Curr Opin Pediatr. 2019 (acesso em 2023 fev 7);31(4):476-481. doi: 10.1590/S0080-62342011000100018 [ Links ]
4. Faria TF, Kamada I. Lesões de pele em neonatos em cuidados intensivos neonatais. Enfermería Global. 2017 (acesso em 2020 fev 2);17(1):220-228. doi: 10.6018/eglobal.17.1.273671 [ Links ]
5. Amer Y, Bridges C, Marathe K. Epidemiology, Pathophysiology, and Management Strategies of Neonatal Wound Care. Neoreviews (acesso em 2023 ago 07);22(7):e452-e460. doi: 10.1542/neo.22-7-e452 [ Links ]
6. Parizad N, Hajimohammadi K, Hassanpour A, Goli R. Treating surgical site infection by honey antibacterial wound dressing in a neonate: a case report. British Journal of Nursing. 2022 (acesso em 2023 ago 07);31(4). doi: 10.12968/bjon.2022.31.4.S8 [ Links ]
7. Rezaei PMS, Jafari-Mianaei S, Sadeghnia A, Heidari Z. Protective Dressings, Injury, and Device Failure in Preterm Infants Receiving Nasal Continuous Positive Airway Pressure: A Randomized Controlled Trial. Advances in Skin & Wound Care. 2023 (acesso em 2023 fev 07);34(9):1-6. doi: 10.1097/01.ASW.0000767344.37591.b6 [ Links ]
8. Soares CB, Hoga LAK, Peduzzi M, Sangaleti C, Yonekura T, Silva DRAD. Integrative review: concepts and methods used in nursing. Rev Esc Enferm USP. 2014 (acesso em 2023 jul 08);48(2):335-345. doi: 10.1590/S0080-623420140000200020 [ Links ]
9. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. Journal of The Medical Library Association. 2018;106(4):420-431. doi: 10.5195/jmla.2018.345 [ Links ]
10. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 (acesso em 2020 feb 07);372(71). doi: 10.1136/bmj.n71 [ Links ]
11. Fan K, Tang J, Escandon J, Kirsner RS. State of the art in topical woundhealing products. Plast Reconstr Surg. 2011 (acesso em 2020 fev 07)127(Suppl.1):44S-59S. doi: 10.1097/PRS.0b013e3181fbe275 [ Links ]
12. Parizad N, Hajimohammadi K, Hassanpour A, Goli R. Treating surgical site infection by honey antibacterial wound dressing in a neonate: a case report. Br J Nurs. 2022 (acesso em 2023 set 10);31(4). doi: 10.12968/bjon.2022.31.4.S8 [ Links ]
13. Martínez G, D' Ángelo J. Uso de VAC en neonatos. Rev. argent. cir. Plást. 2021 (acesso em 2023 set 01);27(2):86-89. doi: 10.32825/RACP/202102/0086-0089 [ Links ]
14. Boyar V. Association of Systemic or Intravitreal Antivascular Endothelial Growth Factor (Anti-VEGF) and Impaired Wound Healing in Pediatric Patients: Collagen to the Rescue. Journal of Wound, Ostomy and Continence Nursing. 2021 (acesso em 2023 set 01);48(3):256-261. doi: 10.1097/WON.0000000000000764 [ Links ]
15. Harma B, Gül M, Demircan M. The Efficacy of Five Different Wound Dressings on Some Histological Parameters in Children with Partial Thickness Burns. Journal of Burn Care & Research. 2020 (acesso em 2023 set 01);41(6):1179-1187. doi: 10.1093/jbcr/iraa063 [ Links ]
16. Sherman G, Shulman-Manor O, Dagan O, Livni G, Scheuerman O, Amir G, et al. Vacuum-Assisted Closure for the Treatment of Deep Sternal Wound Infection After Pediatric Cardiac Surgery. Pediatric Critical Care Medicine. 2020 (acesso em 2023 set 01);21(2):150-155. doi: 10.1097/PCC.0000000000002131 [ Links ]
17. Ivanzov S, Soynov I, Kulyabin Y, Zubritskiy A, Voitov A, Omelchenko A, et al. Vacuum-assisted closure versus closed irrigation for deep sternal wound infection treatment in infants: a propensity score-matched study. Interactive CardioVascular and Thoracic Surgery. 2019 (acesso em 2023 set 01);29(5):776-782. doi: 10.1093/icvts/ivz167 [ Links ]
18. Padalino MA, Carrozzini M, Vida V, Stellin G. Vacuum-Assisted Closure Therapy for the Treatment of Poststernotomy Wound Dehiscence in Neonates and Infants. Thorac Cardiovasc Surg. 2019 (acesso em 2023 set 01);67:055-057. doi: 10.1055/s-0037-1603933 [ Links ]
19. Pereima MJL, Feijó R, Oenning da Gama F, de Oliveira Boccardi R. Treatment of burned children using dermal regeneration template with or without negative pressure. Burns. 2019 (acesso em 2023 set 02);45(5):1075-1080. doi: 10.1016/j.burns.2018.08.009. [ Links ]
20. Zoeller C, Yoshizawa E, Sethi MV, Ure BM, Kuebler JF. Negative Pressure Wound Dressing Reduces Surgical Site Infections in Infants after Closed Abdominal Procedures: A Preliminary Report. Eur J Pediatr Surg. 2019 (acesso em 2023 set 02);29(4):384-387. doi: 10.1055/s-0038-16604482019. [ Links ]
21. Bayci A, Akay B. Advanced Techniques in the Use of Negative Pressure Wound Therapy for Closure of Complex Neonatal Abdominal Wounds. Journal of Wound, Ostomy and Continence Nursing. 2018 (acesso em 2023 set 10);45(5):468-471. doi: 10.1097/WON.0000000000000471 [ Links ]
22. Copeland H, Newcombe J, Yamin F, Bhajri K, Ayer Mille V, Hasaniya N, et al. Role of Negative Pressure Wound Care and Hyperbaric Oxygen Therapy for Sternal Wound Infections After Pediatric Cardiac Surgery. World Journal for Pediatric and Congenital Heart Surgery. 2018 (acesso em 2023 set 12);9(4):440-445. doi: 10.1177/2150135118772494 [ Links ]
23. Boyar V. Treatment of Dehisced, Thoracic Neonatal Wounds With Single-Use Negative Pressure Wound Therapy Device and Medical-Grade Honey: A Retrospective Case Series. Journal of Wound, Ostomy and Continence Nursing. 2018 (acesso em 2023 set 12);45(2):117-122. doi: 10.1097/WON.0000000000000407 [ Links ]
24. Fras Zemljič L, Maver U, Kraševac Glaser T, Bren U, Knez Hrnčič M, Petek G, et al. Electrospun Composite Nanofibrous Materials Based on (Poly)-Phenol-Polysaccharide Formulations for Potential Wound Treatment. Materials (Basel). 2020 (acesso em 2023 set 12);13(11):2631. doi: 10.3390/ma13112631 [ Links ]
25. Jesus LE, Martins AB, Oliveira PB, Gomes F, Leve T, Dekermacher S. Negative pressure wound therapy in pediatric surgery: How and when to use. Journal of Pediatric Surgery. 2018 (acesso em 2023 set 12);53(4):585-591. doi: 10.1016/j.jpedsurg.2017.11.048 [ Links ]
26. Abdelgawad MA, Parambi DGT, Ghoneim MM, Alotaibi NH, Alzarea AI, Alanazi AS, et al. A meta-analysis showing the effect of surgical site wound infections and associated risk factors in neonatal surgeries. Int Wound J. 2022 (acesso em 2023 set 12); 19(8):2092-2100. doi: 10.1111/iwj.13814 [ Links ]
27. Qiao Y, Zhang T, Bai T, Peng X, Lin H, Zhang A. Effect of body mass index on surgical site wound infection, mortality, and postoperative hospital stay in subjects undergoing possibly curative surgery for colorectal cancer: A meta-analysis. Int Wound J. 2023 (acesso em 2023 set 12);20(1):164-172. doi:10.1111/iwj.13860 [ Links ]
28. Secco IL, Danski MTR, Pereira HP, Almeida TQR de, Cruz TR. Cuidados de enfermagem a recém-nascido com infecção de sítio cirúrgico incisional profunda: relato de caso. Rev Esc Enferm USP(Internet). 2021 (acesso em 2023 set 12);55:e03769. doi: 10.1590/S1980-220X2020047203769 [ Links ]
29. Santos SV, Ramos FR, Costa R, Batalha LM. Assessment of the quality of a software application for the prevention of skin lesions in newborns. Rev Latino-Am Enfermagem. 2020 (acesso em 2023 set 12);28:e3352. doi: 10.1590/1518-8345.3711.3352 [ Links ]
30. Catania VD, Boscarelli A, Lauriti G, Morini F, Zani A. Risk factors for surgical site infection in neonates: a systematic review of the literature and meta-analysis. Front Pediatr. 2019 (acesso em 2023 set 12);7(101). doi: 10.3389/fped.2019.00101 [ Links ]
31. Ferraz LCC, Guedes BLS, Lucio IML, Santos RCS. Desenvolvimento de protetor nasal anatômico para recém-nascidos em uso de pronga. Rev. esc. enferm. USP (online). 2020 (acesso em 2023 set 12);54:03618. doi: 10.1590/s1980-220x2019005603618. [ Links ]
How to cite:Silva JC da, Carvalho ES de S, Sales IPPM, Blanes L, Camargo CL de, Silva CT dos S. Evidence for the Treatment of Wounds in Newborns: An Integrative Review. Enfermería: Cuidados Humanizados. 2024;13(1):e3220. doi: 10.22235/ech.v13i1.3220
Authors’ contribution (CRediT Taxonomy):1. Conceptualization; 2. Data curation; 3. Formal Analysis; 4. Funding acquisition; 5. Investigation; 6. Methodology; 7. Project administration; 8. Resources; 9. Software; 10. Supervision; 11. Validation; 12. Visualization; 13. Writing: original draft; 14. Writing: review & editing. J. C. D. S. has contributed in 1, 2, 3, 5, 6, 7, 8, 9, 12, 13; E. S. D. S. C. in 11, 14; I. P. P. M. S. in 3, 11, 13, 14; L. B. in 11, 14; C. L. D. C. in 2, 5, 6, 7, 10, 11, 12, 13, 14; C. T. D. S. S. in 2, 9, 11, 13, 14.
Received: February 08, 2023; Accepted: November 13, 2023











 text in
text in 
 Curriculum ScienTI
Curriculum ScienTI