Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.12 no.2 Montevideo 2023 Epub Dec 01, 2023
https://doi.org/10.22235/ech.v12i2.3213
Original Articles
Sleep Quality and Chronotype and its Relationship with Obesity in the Adult Population. Narrative Bibliographic Review
1 Universidad Católica del Uruguay, Uruguay
2 Universidad Católica del Uruguay, Uruguay, cate.torterolo@gmail.com
3 Universidad Católica del Uruguay, Uruguay
Introduction:
As a result of the high prevalence of obesity worldwide and nationally, and because of the incidence of this disease in the development of comorbidities, studying the factors that contribute to its development is necessary. The lack or disrupted sleep that is affecting our civilization, has been associated with the worldwide epidemic of obesity, being a modifiable factor to include in its therapy.
Objective:
To find recent evidence about the underlying mechanisms that build a possible relationship between sleep duration and/or quality with the development of obesity in adults.
Methods:
The search of articles was carried out by using virtual platforms of bibliographic databases, which were filtered by: age (18 to 64 years), human studies, full text, English and Spanish language and publications no longer than 5 years. Studies that evaluated sleep quality had to apply the Pittsburgh Sleep Quality Index (PSQI) and those that evaluated chronotype had to use the Horne and Ostberg’s Morningness - Eveningness Questionnaire or the Munich Chronotype Questionnaire
Results:
Individuals with insufficient sleep duration and/or quality were more likely to become obese. Underlying mechanisms found were hormonal and metabolic alterations and an increase in food intake, mainly during the biological night
Conclusions:
According to the selected bibliography, there is scientific evidence linking sleep duration and/or quality with the possible development of obesity in adults
Keywords: sleep; obesity; chronotype; energy metabolism; review
Introducción:
Debido a la alta prevalencia de obesidad a nivel mundial y nacional, y de la incidencia de esta enfermedad en el desarrollo de comorbilidades, estudiar los factores que contribuyan a su desarrollo resulta pertinente. La falta de sueño o el sueño interrumpido pueden estar asociados a la epidemia mundial de la obesidad, y resulta un factor modificable a incluir en su terapéutica.
Objetivo:
Conocer la evidencia reciente acerca de los mecanismos subyacentes que conforman una posible relación entre la cantidad y/o calidad de sueño con el desarrollo de obesidad en personas adultas
Metodología:
Revisión bibliográfica de artículos científicos en plataformas virtuales de bases de datos. Se aplicaron distintos filtros: edad (18 a 64 años), estudios realizados en humanos, texto completo, idioma inglés y español, y publicaciones no mayores a 5 años. Los estudios de evaluación de la calidad de sueño debían haber aplicado el Índice de Calidad de Sueño de Pittsburgh, y los de evaluación del cronotipo el Horne and Ostberg’s Morningness - Eveningness Questionnaire o el Munich Chronotype Questionnaire
Resultados:
Individuos con una insuficiente cantidad y/o calidad de sueño fueron asociados con una mayor probabilidad de desarrollar obesidad. Los principales mecanismos subyacentes encontrados fueron: alteraciones hormonales, metabólicas y un aumento de la ingesta de alimentos principalmente en la noche biológica
Conclusiones:
Según la bibliografía seleccionada se concluye que existe evidencia que relaciona la cantidad y/o calidad de sueño con el posible desarrollo de obesidad en población adulta.
Palabras clave: sueño; obesidad; cronotipo; metabolismo energético; revisión
Introdução:
Devido à alta prevalência da obesidade no mundo e no país e à incidência dessa doença no desenvolvimento de comorbidades, é relevante estudar os fatores que contribuem para o seu desenvolvimento. A falta de sono ou o sono interrompido pode estar associado à epidemia global de obesidade e é um fator modificável a ser incluído em sua terapia
Objetivo:
Verificar as evidências recentes sobre os mecanismos subjacentes que compõem uma possível relação entre a quantidade e/ou a qualidade do sono e o desenvolvimento da obesidade em adultos
Metodologia:
Revisão bibliográfica de artigos científicos em plataformas de bancos de dados virtuais. Foram aplicados diferentes filtros: idade (18 a 64 anos), estudos em humanos, texto completo, idioma inglês e espanhol e publicações com no máximo 5 anos. Os estudos que avaliaram a qualidade do sono deveriam ter aplicado o Índice de Qualidade do Sono de Pittsburgh, e os que avaliaram o cronotipo deveriam ter aplicado o Horne and Ostberg’s Morningness - Eveningness Questionnaire ou o Munich Chronotype Questionnaire
Resultados:
Os indivíduos com quantidade e/ou qualidade de sono insuficiente foram associados a uma maior probabilidade de desenvolver obesidade. Os principais mecanismos subjacentes encontrados foram: distúrbios hormonais, metabólicos e aumento da ingestão de alimentos, principalmente na noite biológica
Conclusões:
Segundo a bibliografia selecionada, há evidências que relacionam a quantidade e/ou a qualidade do sono com o possível desenvolvimento de obesidade na população adulta
Palavras-chave: sono; obesidade; cronotipo; metabolismo energético; revisão
Introduction
Obesity (OB) is a metabolic disorder caused by several factors. Is characterized by the excess of body fat which can be harmful to health. Since 1975, its prevalence worldwide has almost tripled. Currently, more than 650 million adults over 18 years old have OB, which is why the World Health Organization (WHO) classifies this disease as a pandemic global public health problem. Latest studies in Latin America from 2021 indicate that OB affects 24.2 % of the Latin American population, which means that 1 in 4 adults suffer from this disease. In Uruguay, 27.6 % of the population has OB, which means that 3 out of every 10 adults are obese. 1,2,3,4,5
Within this context of multicausality, inadequate sleep -both in quantity, quality and regularity- is one of the factors that influences energy metabolism through two mechanisms. On the one hand, it affects energy expenditure and on the other hand it affects caloric consumption. The influence on energy expenditure is linked to the presence of drowsiness, and as a consequence of this alteration, there is a decrease in movement and therefore energy expenditure. Regarding caloric consumption, it is altered by the imbalance of the hormones that mediate appetite and satiety. 6
Lack of sleep or interrupted sleep has been associated with negative health effects, in addition to those related to obesity, type 2 diabetes, development of cardiovascular diseases (CVD), weakening of the immune system, cognitive impairment and mental health problems (such as anxiety and depression). This is why sleep fulfills an essential biological function in our body. 7
According to current recommendations, healthy adults should sleep an average of 7 to 9 hours per night. It is estimated that 35.2 % of the American adult population sleeps on average less than 7 hours, according to the American Sleep Association (ASA). Of the general proportion of adults with OB, 3 to 5 % could be attributable to lack of sleep. Current lifestyle is one of the main factors that has affected the quantity and quality of sleep, altering circadian rhythms (CR) and causing repercussions on health. Sleep is considered one of the main markers of these rhythms, which are responsible for helping certain body processes to be optimized at different times during the 24 hours of a day. (8,9,10,11,12,13
If the duration and/or quality of sleep are altered, and therefore the CR are also affected, then the processes coordinated by this system will be compromised. It is observed that sleep plays a significant role in the modulation of weight gain, in neuroendocrine signals, and consequently in the homeostatic regulation of glucose and insulin. As a result, alterations in the duration and/or quality of sleep are considered risk factors for the development of OB. 12,13
In Uruguay, government documents issued by the Ministry of Public Health (MPH) mention short sleep duration as a risk factor for the development of OB, indicating that this essential component in people's health should be considered within the pillars of the treatment of this disease. 14
Obesity in its treatment must be managed due to the characteristics it presents: a chronic, epidemic, complex, heterogeneous and stigmatized health problem. In Latin America, there is the “Argentine Clinical Practice Guide on Diagnosis and Treatment of Obesity” that provides updated information regarding the management of this disease. This document proposes an approach that faces the problem from the paradigm of complexity, understanding that it cannot be treated with isolated measures. Its treatment requires a multidisciplinary view and an interdisciplinary approach. Reversing the high numbers of OB will have an impact on the morbidity it presents and the health costs associated with it. 15
Worldwide, 2.8 million people die each year due to comorbidities associated with OB. Therefore, since it is a non-communicable disease (NCD) and at the same time a risk factor for the development of other NCDs, treating it may indirectly affect the morbidity and mortality of these others, such as: type 2 diabetes mellitus, high blood pressure, CVD, dyslipidemia, among others. 14,16
Previous reviews have already established a relationship between sleep and OB. According to Chamorro et al. and Noh, both the alteration of the quantity and quality of sleep are considered factors that influence the development of OB and other NCDs. As expressed by Cooper et al., in individuals whose sleep duration is regularly less than 7 hours per night there is a greater probability of developing OB or having a higher Body Mass Index (BMI), compared to individuals who have more hours of sleep per night. 6,17,18
According to the reviews mentioned above, they share the following results that reveal the presence of a link between sleep disturbance and OB. Firstly, numerous studies share in their findings anthropometric variations related to increases in BMI, waist circumference (WC) and weight, when the quantity and/or quality of sleep are affected. In this way, it has been seen that a greater state of fatigue, due to a decrease in hours of sleep, can reduce physical activity levels, causing lower energy expenditure. Another factor that can contribute to a positive energy balance is the alteration that occurs at the endocrine level in the hormones ghrelin (orexigenic hormone) and leptin (anorexigenic hormone), where ghrelin is increased and leptin is decreased. On the other hand, in order to balance a longer time awake, it has been observed that there is an increase in intake, related to hedonic appetite, which is especially linked to a greater desire for foods with high energy density. Likewise, it is observed that a greater food intake during the biological night is associated with unwanted weight gain. 6,17,18
The objective of this review is to understand the recent evidence about the underlying mechanisms that make a possible relationship between the quantity and/or quality of sleep with the development of OB in adults.
Method
The bibliography presented in this narrative review was extracted from different virtual bibliographic database platforms such as: PubMed, Medline Plus, Scielo, Timbó, MDPI, Mendeley and Elsevier. Regarding the type of publications, articles from scientific journals, reviews (narrative and systematic), clinical trials, randomized clinical trials and meta-analysis were used. Likewise, to extract specific data or figures, publications and files issued by health entities such as: WHO, Food and Agriculture Organization of the United Nations (FAO), Uruguayan Ministry of Health, Official Site of Uruguay (GUB), World Bank, Sleep Foundation, National Sleep Foundation, American Academy of Sleep Medicine (AASM), Sleep Research Society (SRS), ASA, Argentine Ministry of Health.
The selected bibliography must have a range of no more than five years to the current date (2017 to 2022).
The information search was filtered by full text, English and Spanish languages, studies conducted in humans, male and/or female sex, and adult age from 18 to 64 years, or the average in that range.
As a condition, articles that present studies that evaluate sleep quality must apply the Pittsburgh Sleep Quality Index (PSQI). While the studies that evaluated chronotype had to apply Horne and Ostberg’s Morningness-Eveningness Questionnaire or Munich Chronotype Questionnaire. These evaluation instruments have been validated for their application in the adult population.
Controlled vocabulary was applied to search information, using health science descriptors (DeCS and MeSH terms), such as: “circadian dysregulation”, “circadian clocks”, “chronobiology rhythm disorder”, “sleep disturbance”, “sleep deprivation”, “obesity”, “central obesity”, “body mass index”, “weight gain”, “adults”, “circadian rhythm sleep disorders”, “chronobiology disorder”. Likewise, these terms were implemented to search studies in Spanish language, using their respective translations in these idioms. Finally, the articles selected were those whose titles and abstracts qualified as potentially relevant were selected, meeting the inclusion criteria.
Results
After the bibliographic search, it was decided to subdivide the evidence found into different sections, based on the results obtained.
Relationship between lifestyle and urbanization with the quantity and quality of sleep
A study carried out in Brazil investigated the influence of artificial light on sleep behavior. The results show that the activity phase and sleep behavior have changed because of the use and incorporation of electricity, added to the influences of modern life. Those people who live without electricity and those who have recently acquired it tend to fall asleep an hour earlier compared to more urbanized communities. In turn, sleep duration tended to be longer. 19)
Another investigation in Mexico sought to examine the association between three lifestyle behaviors (amount of sleep, physical activity and screen time) with BMI in 6419 adults. The variables of short sleep duration, prolonged screen time, and lack of intense physical activity were classified as “unhealthy phenotype.” The results showed that the main modifiable lifestyle factors with the greatest association with overweight (OW) and OB were: screen time (TV, cell phone, computer and tablets), physical activity and sleep duration. Likewise, participants with OW and OB (type 1 and 2) reported less sleep time per day compared to normal weight participants. It was concluded that 37 % of the participants were obese and that factors specific to the “unhealthy phenotype” were significantly associated with OB. 20
Investigating lifestyle factors, a relationship was seen between stress and sleep. In a cross-sectional study carried out on 263 medical students in Saudi Arabia, the prevalence and relationship between poor sleep quality and the presence of stress was evaluated. The results showed a high prevalence of stress (53 %) and poor sleep quality (76 %), with a significant statistical association between both variables. Likewise, it was observed that most students slept an average of 5.8 ± 1.3 hrs. In conclusion, the study shows that high levels of stress are an important predictor and contributor to poor sleep quality. 21)
It has been seen that young adults are more predisposed to developing “social jet lag” (SJL) because during the week they usually start their activities early and the time allocated to sleep is short. This situation can cause a mismatch between the internal biological clock and social life. Bodur et al. in a study carried out on 710 university students had the objective to compare anthropometric (BMI, WC and neck circumference) and quality measures of sleep, in individuals with and without SJL, also comparing aspects of dietary intake between school and non-school days in the different groups (with and without SJL). Contrasting both groups, those with SJL showed lower levels of diet quality, poorer sleep quality, and higher BMI values.22
The influence of the different chronotypes on eating habits and sleep
There are several circadian markers, among them, chronotype is the one that reflects the preferred time or moment of the day for a person to carry out its activities, including rest hours. People can be classified as morning, intermediate and evening chronotype. It has been discovered that chronotype can play a modifying role between meal times and OB. 23
On a sample of 1854 participants in Finland, the association between chronotype, energy intake schedule and macronutrients was studied. Within the findings of the study, the evening chronotype showed to postpone the intake (towards the evening) of energy and macronutrients, with a tendency towards a greater consumption of sucrose, fats and saturated fatty acids, but with a lower protein intake than the morning chronotype. Likewise, the evening chronotype showed a more irregular eating pattern, presenting more accumulated energy intake at night than in the morning. It was also observed that a high proportion of these individuals reported sleeping less than 5 hours per night, experiencing insufficient sleep and insomnia. It was concluded that postponing the timing of energy intake in people with an evening chronotype with unfavorable dietary patterns may expose them to a high risk of developing OB and metabolic disorders in the future. 24
In another study conducted in Pittsburgh, 872 individuals participated. Meal timing was defined in relation to the sleep/wake cycle (as an indicator of circadian time) and therefore the relationship between meal timing and BMI depending on chronotype was investigated. The results of this study showed that people with a diurnal chronotype had a higher consumption of the total daily intake in the morning, associating it with a lower probability of OW and OB. Unlike the evening chronotype, whose results showed that there is a greater probability of OW and OB if the consumption of the total daily intake is focused on the night. These associations were stronger for carbohydrate (CARBS) and protein intake than for lipids. (23
Finally, a study carried out in Finland whose sample was 1097 individuals is included. Chronotype was first independently examined with timing of energy intake and anthropometric changes. Next, we studied whether chronotype modifies the association between the time of intake and the risk of OB. The proportion of individuals who gained more weight tended to be higher in the evening chronotype than in the daytime chronotype, with 26 % of obese people prevailing in the evening chronotype and 17 % in the daytime chronotype. It was seen that women with an evening chronotype had greater weight gain (3 times more) than women with a daytime chronotype. Those participants with a higher nocturnal intake were almost twice as likely to have OB at the beginning and at the end of follow-up than those whose intake was lower. Therefore, it is concluded that energy consumption at night may play a role in the development of OB regardless of their chronotype. 25
Metabolic and neuroendocrine behavior: how are they affected by sleep disturbances?
In a study with a randomized crossover design, a small sample of participants underwent an 8-day laboratory evaluation, where active ghrelin levels and hunger/appetite levels were measured before and after identical test meals. The results found that active ghrelin levels were higher in the biological afternoon than in the biological morning, matching with the circadian variation of hunger in the participants. It was observed that in participants with altered CR, postprandial active ghrelin levels increased. Given this situation, these people may have a positive energy balance. Likewise, this alteration resulted in an increased appetite for high-calorie-dense foods. 26
Studies have indicated the existence of an endogenous circadian rhythm in the body. It has been observed that plasma glucose and insulin levels vary during the day, even if the same meal is consumed at different times. Leung et al. investigated postprandial glucose and insulin levels after eating a low glycemic index meal, thus comparing the results obtained between morning and evening in a group of healthy adults. The findings show higher postprandial levels of glucose and insulin at night than in the morning, after eating the same low-glycemic index meal. 27
Similar results have been found in 10 studies included in a meta-analysis where postprandial plasma levels of glucose and insulin were evaluated after an identical ingestion of test meals, consumed by the same individuals, at different times of the day (morning/night). It was concluded that the insulin and glucose response was higher at night than in the morning, thus marking the existence of a postprandial difference in both variables during the day. 28
The cross-sectional study carried out by Hashemipour et al. evaluated in a population of 612 obese people or with PS the possible association between sleep quality and insulin resistance (IR). The results show that sleep quality was rated as poor in the group with IR compared to the group without IR. This marks an existing association among people with OB or OW between sleep quality and IR. 29
Chrononutrition: meal timing and their metabolic effect
Through the following cross-sectional observational study, it was sought to investigate the associations between meal timing and frequency with OB and metabolic syndrome in a population of 14,279 Korean adults. The results obtained allowed to conclude that having a higher calorie consumption in the morning than at night, avoiding eating after 9:00 p.m., together with an adequate sleep schedule (between 7-8 hrs.), can be useful to reduce the risks of OB and metabolic syndrome, regardless of the duration of fasting. 30
Another study carried out in a sample of 20 participants, aimed to study the impact of late dinner (10:00 p.m.) on nighttime metabolism compared to a routine dinner (6:00 p.m.). This randomized crossover trial found that late eating caused a 4-hour shift in the postprandial phase, overlapping with the sleep phase because participants had to go to bed at 11:00 p.m. Through blood tests, it was observed that the postprandial period of people who had a “late” dinner was characterized by higher glucose levels, a delay in the peak of triglycerides and a lower oxidation of exogenous fatty acids and free fatty acids (approx. 10 % compared to control group). This caused an anabolic state during sleep, prioritizing lipid storage over mobilization and oxidation. These effects found could promote OB if they occur chronically. 31
Through a cross-sectional study applied in a sample of 110 participants, the existing relationships between the clock time of food intake and the endogenous circadian rhythm (measured by the beginning of the secretion of melatonin, a sleep-regulating hormone), the energy content of intake and body composition were evaluated. The results showed that individuals with the highest level of body fat consumed the most calories (relative to a day) near the beginning of melatonin secretion, which indicates the beginning of the biological night, compared to individuals with low body fat percentage. This means that the body composition of the participants was associated with the circadian moment rather than with the clock time in which the intake took place. Therefore, the results show evidence that food consumption near the beginning of the biological night has a relevant role in body composition, beyond other factors such as the amount or content of the intake or physical activity. 32
Relationship between diet quality and dietary pattern with quantity or quality of sleep
Different associations have been observed between different dietary patterns and sleep. In a cross-sectional study carried out in Tehran in a population of 304 women with OW and OB, the relationship between a low-CARBS diet and sleep quality was evaluated with the mediating effect of inflammatory markers such as C-reactive protein (CRP), sleep capacity and total antioxidant. The researchers maintain that the restriction of CARBS in the diet, especially before going to bed, leads to a decrease in the secretion of inflammatory markers such as CRP, which consequently leads to an increase in the expression of clock genes and a better sleep regulation. Likewise, it was seen that the effects of consuming a diet high in CARBS on sleep quality are associated with a decrease in melatonin synthesis. The results of the study showed that a diet low in CARBS has an important association with sleep quality. The findings suggest that a diet low in carbohydrates or reducing their consumption reduces the probability of poor quality sleep by up to 43 %. Based on the results of this study, it was concluded that total antioxidant capacity and CRP could be two mediating factors that influence these findings. 33
In the following randomized controlled feeding study, the main objective was to evaluate the effects of a healthy American dietary pattern on PSQI. Fiftyone adults with OW and OB participated, classified as having sleep problems using the PSQI and whose objective sleep quality was assessed using wrist actigraphy and saliva samples to evaluate melatonin levels. Under a calorie restriction regimen, participants were randomly distributed to receive a diet according to the American dietary pattern versus a group whose protein intake was increased. It was concluded that although objective sleep quality may not improve, consuming a healthy dietary pattern recommended by American guidelines, or higher in protein during the hypocaloric regimen, is associated with improvements in perceived sleep quality and daytime sleepiness among adults with OW and OB. 34
Studies have linked sleep quality with the Mediterranean diet (MD). The studies carried out by Godos et al. and Muscogiuri et al. investigated the association between adherence to the MD and sleep quality. Both studies were carried out in Italy in the adult population. The findings obtained by Muscogiuri et al. show that subjects with better sleep quality obtained significantly greater adherence to the MD, compared to individuals with poorer sleep quality. Likewise, the latter showed higher values of BMI, WC, which suggests that poorer sleep quality was more prevalent in subjects with OB. On the other hand, Godos et al. using a larger sample of individuals (n = 1936), reported that better adherence to the MD was linked to a better sleep quality. Sleep latency was significantly associated with greater adherence to this type of diet. Finally, through a more exhaustive analysis, it was found that the association between sleep quality and high adherence to the MD was found among individuals with a nutritional status of normal weight or OW and not in obese participants. 35,36
Sleep quantity and quality linked to weight gain
A cross-sectional study conducted in Korea by Park et al. investigated the association between sleep duration, quality, and BMI categories. Data were extracted from 107,718 individuals who participated in a previous health study. The results of this research showed that short sleep duration was closely related to OB categories. Likewise, poor sleep quality indicated an important association with OB, predominating in women more than in men. 37
In another cross-sectional study, the objectives were to determine whether poor sleep quality was related to abdominal adiposity and not total body adiposity. In this study 101 individuals participated with an average BMI of 29.35 ± 6.93kg/m2. The results associated poorer sleep quality with higher levels of visceral fat and leptin. The group of individuals with a higher PSQI score, that is, with poorer sleep quality, presented more abdominal visceral fat than the group with normal sleep quality, but there were no differences in the total amount of body fat. This study was one of the first to find an association between poor sleep quality with higher levels of abdominal adiposity and leptin. 38
González et al., through a systematic review, investigated the evidence available between the relationship among habitual sleep (approximately 8 hours) versus nocturnal sleep restriction (< 6 hours), and its effects on dietary intake in the adult population. The evidence found showed a positive relationship between the total energy consumed and a short sleep duration, without confirming a specific meal time. Therefore, the review concluded that individuals with partial sleep restriction had an increase in total energy and macronutrient intake when compared to the control group (usual sleep). 39
In another cross-sectional study conducted by Hur et al., it was evaluated how diet quality could interfere in the relationship between sleep status (quality and quantity) and OB. The study was conducted on a large sample of Korean adults. The results showed that in comparison, obese women presented higher levels of insufficient sleep (< 7 hrs per day) and poorer sleep quality (PSQI > 5 points) than non-obese women. Likewise, women revealed poorer sleep quality and lower levels of diet quality than men. The findings of this study allowed to conclude a significant association between sleep quality and OB, being this relationship potentially influenced by the quality of the diet in women. 40
In a population of 63 shift workers, it was sought to evaluate the relationship between the quality, duration and hygiene of sleep with the control of hedonic appetite. On average, women presented OW and men OB. Through different online surveys to evaluate each of the variables, it was found that 84 % reported weight gain since the beginning of shift work. An association was found between poorer quality and shorter duration of sleep with greater food cravings. On the other hand, a greater hedonic drive due to the consumption of palatable foods is associated with poorer sleep quality and hygiene. Consequently, the study suggests that in shift workers who have sleep disturbances, hedonic appetite may be a cause of weight gain in these individuals. 41
Another study showed the relationship between sleep pattern, nutritional status and dietary intake of 130 security agents in Panama City. The results showed a high proportion of abdominal OB (44.6 %), excess weight (85.4 %), OB (53.9 %), insomnia (19.2 %) and drowsiness (94.6 %). Likewise, 43.1 % of individuals had difficulty sleeping and 56.9 % slept less than 7 hours per day. The conclusions showed a high proportion of malnutrition due to excess according to BMI, abdominal OB according to WC, and also alterations in sleep quality. Regarding the diet, it was seen that it was excessive in calories, fat, CH, and deficient in vitamin C, vitamin A, calcium and fiber. 42
Discussion
In Western societies, sleep has been considerably modified in relation to its 24-hour context. Light is one of the most important synchronizing stimuli for proper development of the CR, with the sleep/wake cycle being a component thereof. During the night, exposure to light can be a disruptive factor for the circadian system. Within the results section, referring to lifestyle and urbanization, according to the study by Pilz et al., the incorporation of electricity and artificial light were events that modified nighttime sleep. On the other hand, Kolovos et al. found that shorter sleep time was associated with higher levels of BMI due to greater time spent using screens and a lack of physical activity. On the other hand, poorer sleep quality was related to higher levels of stress according to Almojali et al. Finally, presenting an accumulated sleep debt, known as the SJL, added to a poor quality of diet and poor quality of sleep as expressed by Bodur et al. In their study, they are factors that were associated with weight gain and possible development of OB. 6,17,19)F2
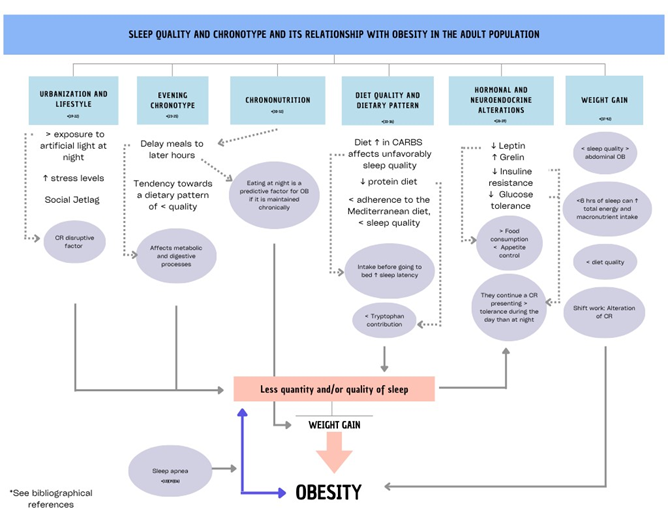
Figure 1: Scheme of factors that influence the quantity and/or quality of sleep for the development of obesity in the adult population.
Through the section referring to chronotype, it can be concluded that a tendency is observed in the evening chronotype to delay energy intake to later times at night and presenting a dietary pattern of lower quality, which together would increase the probability of developing OB due to weight gain. Food is a powerful synchronizer of the CR, commanded by the central biological clock (or pacemaker), located in the suprachiasmatic nucleus in the area of the hypothalamus. It is characterized that eating food during the biological night can affect metabolic and digestive processes. However, while evidence shows the importance of the timing of energy intake in metabolic health, the role of chronotype within this association needs further study.6,24,25
According to the results in the chrononutrition section, eating at night is a predictive factor for OB if it is maintained chronically. It is interesting to note that eating food at unusual times can result in the development of OB. Chrononutrition encompasses the effects of timing (time of day) in food and the composition of intake (energy and macronutrients), in relation to how the CRs are organized throughout the day. The modern lifestyle has led to 40 % of humans currently delaying their energy intake towards the evening. Therefore, according to the study by Ha and Song, allocating a greater consumption of total daily energy in the morning, in conjunction with adequate hours of sleep (7-8 hours), may be a useful recommendation to reduce the risk of OB and metabolic syndrome. 6,17,27
In relation to diet quality and dietary pattern, several results have been highlighted in this section. Within the therapeutic pillars of the OB, diet plays an essential role. Not only should caloric intake be reduced to promote negative energy expenditure, but it is also essential to improve dietary quality. Regarding sleep, diet plays a substantial role in its regulation. It has been seen that a diet high in CARBS can unfavorably impact sleep quality. Thus, according to Tavakoli et al., reducing its consumption would reduce the probability of poor quality sleep by 43 %. Likewise, it is highlighted that a high intake of CARBS before going to bed increases sleep latency (component of sleep quality). The findings by Hudson et al. maintain that a healthy American-style dietary pattern high in protein improves the subjective quality of sleep and daytime sleepiness in adults with OW and OB. Specifically, regarding the protein, it stands out that tryptophan, being a precursor of melatonin and serotonin, manages to improve the quality of sleep. Its consumption depends on dietary protein intake as it is an essential amino acid. As obtained in the studies of Muscogiuri et al. and Godos et al., the presence of proteins rich in tryptophan in the Mediterranean diet may result in a good mechanism to promote better quality of sleep. Regarding fats, no studies are mentioned since the results are inconsistent and controversial, requiring more research on the matter. 15,17,33,34,35,36
Sleep is highlighted as an important modulator within neuroendocrine and metabolic functions, and alterations in its architecture can trigger hormonal modifications, such as ghrelin and leptin, hormones involved in the regulation of appetite and energy expenditure. Leptin is secreted by adipose tissue and acts on receptors in the hypothalamus, inhibiting appetite and generating a feeling of satiety. Ghrelin is secreted by the stomach and pancreas, and is responsible for stimulating appetite. Ghrelin levels circulating in the blood vary throughout the day and depend on food intake. It stands out that people who sleep little have low levels of leptin, high levels of ghrelin and greater body weight, unlike individuals who sleep between 7 and 9 hours. As a result, sleep restriction can lead to greater food consumption due to lack of appetite control, increasing the risk of developing OB. The above coincides with the results obtained by Qian et al., where individuals with altered CR presented increased postprandial active ghrelin. 17,18,26,42
On the other hand, sleep disruption can cause alterations in glucose tolerance. It has been seen, as confirmed in two different studies by Leung et al., that glucose metabolism follows a circadian rhythm. It is observed that there is a greater tolerance to glucose during the day than at biological night, where it decreases. The same happens with insulin, which decreases its sensitivity towards the night. This mechanism can be explained since the lower insulin sensitivity at night, the lower glucose tolerance will also be. This is how it was seen in the study by Hashemipour et al. that subjects with OB and OW associated worse sleep quality with IR. This suggests that improvements in the quantity and/or quality of sleep can promote metabolic health. (17,18,27,28,29
In order to combat NCDs, developing prevention policies and programs that consider other elements than diet and exercise are necessary. Aspects such as sleep hygiene and the obesogenic environment are some of the nutritional considerations to integrate into the approach in relation to sleep and OB. There are several studies that show a relationship between poor quality and/or lack of sleep with weight gain, Sweatt et al. shows in its findings that the lower the quality of sleep, the greater association of abdominal adiposity. The importance of this statement lies in the fact that abdominal OB increases the risk of mortality and suffering from cardiometabolic diseases. Likewise, González et al. observed that a sleep restriction of less than 6 h can lead to an increase in total energy and macronutrient intake. Therefore, this association suggests that sleep restriction increases total daily energy intake, but not energy expenditure. 38,39,42
As mentioned above, metabolic alterations occur after sleep restriction. Metabolic behavior differs depending on sex, so Park et al. noted that lower sleep quality is associated more in women with OB than in men. Likewise, Hur et al. observed that women with OB had poorer sleep quality, enhanced by poor diet quality. The origin of this gender disparity is not clear, however it could be explained due to inequalities in metabolic hormones involved in the sleep-wake cycle, such as leptin, as well as in eating behavior between different genders. 37,40
Finally, shift workers are a population strongly affected due to their work schedules, which necessarily modifies their CR, altering their sleeping and eating hours. In the study by Vidafar et al., it was found that 84 % of individuals reported weight gain since they began shift working, in whom the quality and duration of sleep decreased. On the other hand, Herrera et al. found similar results in his research. Undoubtedly incorporating sleep as one of the therapeutic pillars of OB will be useful in patients with this disease, or in people exposed to a circadian imbalance such as these workers. 6,41,42
It is necessary to highlight that OB per se causes alterations in the organization of sleep, being a risk factor for the development of respiratory disorders such as sleep apnea. Therefore, this relationship reflects a bidirectionality between OB and the quantity and/or quality of sleep. 6,14,15
As the main limitation, it is highlighted that the present review mainly presents studies with a cross-sectional design, which does not allow us to establish a causal correlation between the variables. Despite the methodological differences between the various studies used, similar results are obtained, which consolidate a relationship between the quantity and/or quality of sleep with OB.
Conclusions
It is concluded that there is current evidence that relates the quantity and/or quality of sleep with OB in the adult population. There are several underlying mechanisms that explain this link. The reduction in the quantity and/or quality of sleep results in an alteration in neuroendocrine and metabolic functions. About neuroendocrine considerations, hormonal changes in ghrelin and leptin affect the control of appetite and satiety. On the other hand, at the metabolic level, an increase in IR and a decrease in glucose tolerance is generated. Sleeping between 7 and 9 hours per night would be recommended in order to maintain homeostasis in these processes. Other factors such as increased stress, SJL, a poor quality dietary pattern, delaying meals towards the evening, high exposure to artificial light at night, shift work and presenting an evening chronotype, could alter the quantity and/or quality of sleep and result in weight gain. Still, more research is required, in particular clinical trials to elucidate a causal relationship between sleep and OB. In our country, due to the high prevalence of OB, it is important to carry out studies that evaluate the topic of the present review. Having data on the sleeping habits of the Uruguayan population will allow health professionals to integrate sleep as another pillar to be addressed within the prevention and treatment of OB at a public health level.
REFERENCES
1. Ceballos, JJ, Pérez, R, Flores, J, Vargas, J, Ortega, G, Madriz, R, et al. Obesidad. Pandemia del siglo XXI. Rev Sanid Milit (Internet). 2018 (citado 2022 feb 17);72(5-6):332-338. Disponible en: Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0301-696X2018000400332&lng=es&nrm=iso&tlng=es [ Links ]
2. Organización Mundial de la Salud. Obesidad y sobrepeso (Internet). 2021 (citado 2022 feb 17). Disponible en: Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight [ Links ]
3. Ministerio de Salud Pública. 2da Encuesta Nacional de Factores de Riesgo de Enfermedades No Transmisibles (Internet). Montevideo; 2018 (citado 2021 nov 20). Disponible en: Disponible en: https://www.gub.uy/ministerio-salud-publica/comunicacion/publicaciones/2da-encuesta-nacional-de-factores-de-riesgo-de-enfermedades-no [ Links ]
4. Ministerio de Salud Pública. Sobrepeso y obesidad (Internet). Montevideo; 2019 (citado 2021 nov 20). Disponible en: Disponible en: https://www.gub.uy/ministerio-salud-publica/comunicacion/noticias/sobrepeso-y-obesidad [ Links ]
5. FAO, FIDA, OPS, WFP, UNICEF. Panorama de la Seguridad Alimentaria y la Nutrición en América Latina y el Caribe (Internet). 2021 (citado 2022 feb 17). doi: 10.4060/cb7497es [ Links ]
6. Chamorro, R, Farías, R, Peirano, P. Circadian rhythms, eating patterns, and sleep: A focus on obesity. Rev Chil Nutr. 2018;45(3):285-92. doi: 10.4067/s0717-75182018000400285 [ Links ]
7. Sleep Foundation. How Sleep Works: Understanding the Science of Sleep (Internet). 2022 (citado 2022 feb 17). Disponible en: Disponible en: https://www.sleepfoundation.org/how-sleep-works [ Links ]
8. Sleep Foundation. How Much Sleep Do We Really Need? (Internet). 2022 (citado 2022 feb 17). Disponible en: Disponible en: https://www.sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need [ Links ]
9. National Center for Chronic Disease Prevention and Health Promotion. Data and Statistics (Internet). CDC; 2022 (citado 2022 may 30). Disponible en: Disponible en: https://www.cdc.gov/sleep/data_statistics.html [ Links ]
10. American Sleep Association. Sleep Statistics: Data About Sleep Disorders (Internet). 2022 (citado 2022 may 30). Disponible en: Disponible en: https://www.sleepassociation.org/about-sleep/sleep-statistics/ [ Links ]
11. Pot, GK. Sleep and dietary habits in the urban environment: The role of chrono-nutrition. Proc Nutr Soc (Internet). 2018 (citado 2022 may 30);77(3):189-198. doi: 10.1017/S0029665117003974 [ Links ]
12. Koren, D, Taveras, EM. Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metabolism (Internet). 2018 (citado 2022 may 30);84:67-75. doi: 10.1016/j.metabol.2018.04.001 [ Links ]
13. Sleep Foundation. What Is Circadian Rhythm? (Internet). 2022 (citado 2022 feb 17). Disponible en: Disponible en: https://www.sleepfoundation.org/circadian-rhythm [ Links ]
14. Ministerio de Salud Pública. Nutrición, Alimentación y Actividad Física para la prevención de enfermedades No Transmisibles (Internet). Montevideo; 2017 (citado 2022 may 30). Disponible en: Disponible en: https://www.gub.uy/ministerio-salud-publica/comunicacion/publicaciones/nutricion-alimentacion-actividad-fisica-para-prevencion-enfermedades [ Links ]
15. Victoria, M, Posadas, L, Valenti, L. Guía de Práctica Clínica Nacional Sobre Diagnóstico y Tratamiento de la Obesidad (Internet). Buenos Aires; 2017 (citado 2022 abr 12). Disponible en: Disponible en: http://www.msal.gob.ar/images/stories/bes/graficos/0000000302cnt-2013-11_gpc_obesidad-2013.pdf [ Links ]
16. Organización Mundial de la Salud. Estadísticas sanitarias Mundiales. Una instantánea de la salud mundial (Internet). 2012 (citado 2022 abr 12). Disponible en: Disponible en: http://apps.who.int/iris/handle/10665/70887 [ Links ]
17. Noh, J. The Effect of Circadian and Sleep Disruptions on Obesity Risk. J Obes Metab Syndr (Internet). 2018 (citado 2022 abr 11);27(2):78-83. Disponible en: Disponible en: https://www.jomes.org/journal/view.html?doi=10.7570/jomes.2018.27.2.78 [ Links ]
18. Cooper, CB, Neufeld,,EV, Dolezal, BA, Martin, JL. Sleep deprivation and obesity in adults: A brief narrative review. BMJ Open Sport Exerc Med. 2018;4(1): e000392. doi: 10.1136/bmjsem-2018-000392 [ Links ]
19. Pilz, LK, Levandovski, R, Oliveira, MAB, Hidalgo, MP, Roenneberg, T. Sleep and light exposure across different levels of urbanisation in Brazilian communities. Sci Rep (Internet). 2018 (citado 2022 abr 26);8(1):11389. doi: 10.1038/s41598-018-29494-4 [ Links ]
20. Kolovos, S, Jimenez-Moreno, AC, Pinedo-Villanueva, R, Cassidy, S, Zavala, GA. Association of sleep, screen time and physical activity with overweight and obesity in Mexico. Eat Weight Disord (Internet). 2021 (citado 2022 abr 26);26(1):169-79. doi: doi: 10.1007/s40519-019-00841-2 [ Links ]
21. Almojali, AI, Almalki, SA, Alothman, AS, Masuadi, EM, Alaqeel, MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health (Internet). 2017 (citado 2022 abr 29);7(3):169-74. doi: 10.1016/j.jegh.2017.04.005 [ Links ]
22. Bodur, M, Baspinar, B, Özçelik, AÖ. A cross-sectional evaluation of the relationship between social jetlag and diet quality. Chronobiol Int (Internet). 2021 (citado 2022 may 13);38(11):1557-1568. doi: 10.1080/07420528.2021.1935990 [ Links ]
23. Xiao, Q, Garaulet, M, Scheer, FAJL. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes (Internet). 2019 (citado 2022 abr 29);43(9):1701-1711. doi: 10.1038/s41366-018-0284-x [ Links ]
24. Maukonen, M, Kanerva, N, Partonen, T, Kronholm, E, Tapanainen, H, Kontto, J, et al. Chronotype differences in timing of energy and macronutrient intakes: A population-based study in adults. Obesity (Silver Spring) (Internet). 2017 (citado 2022 abr 1);25(3):608-615. doi: 10.1002/oby.21747 [ Links ]
25. Maukonen, M, Kanerva, N, Partonen, T, Männistö, S. Chronotype and energy intake timing in relation to changes in anthropometrics: a 7-year follow-up study in adults. Chronobiol Int (Internet). 2019 (citado 2022 ene 31);36(1):27-41. doi: 10.1080/07420528.2018.1515772 [ Links ]
26. Qian, J, Morris, CJ, Caputo, R, Garaulet, M, Scheer, FA. Ghrelin is Impacted by the Endogenous Circadian System and by Circadian Misalignment in Humans. Int J Obes (Lond) (Internet). 2019 (citado 2022 abr 21); 43(8):1644-1649. doi: 10.1038/s41366-018-0208-9 [ Links ]
27. Leung, GKW, Huggins, CE, Bonham, MP. Effect of meal timing on postprandial glucose responses to a low glycemic index meal: A crossover trial in healthy volunteers. Clin Nutr (Internet). 2019 (citado 2022 may 20);38(1):465-71. doi: doi: 10.1016/j.clnu.2017.11.010 [ Links ]
28. Leung,,GKW, Huggins, CE, Ware, RS, Bonham, MP. Time of day difference in postprandial glucose and insulin responses: Systematic review and meta-analysis of acute postprandial studies. Chronobiol Int (Internet). 2020 (citado 2022 may 19);37(3):311-26. doi: 10.1080/07420528.2019.1683856 [ Links ]
29. Hashemipour, S, Ghorbani, A, Khashayar, A, Olfati, H. Association of sleep quality with insulin resistance in obese or overweight subjects. Sleep Sci. 2021;14(Special 1):75-8. doi: 10.5935/1984-0063.20200084 [ Links ]
30. Ha, K, Song, Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients (Internet). 2019 (citado 2022 abr 29);11(10):2437. doi: 10.3390/nu11102437. [ Links ]
31. Gu, C, Brereton, N, Schweitzer, A, Cotter, M, Duan, D, Børsheim, E, et al. Metabolic Effects of Late Dinner in Healthy Volunteers-A Randomized Crossover Clinical Trial. J Clin Endocrinol Metab (Internet). 2020 (citado 2022 may 13);105(8):2789-2802. doi: 10.1210/clinem/dgaa354 [ Links ]
32. McHill, AW, Phillips, AJK, Czeisler, CA, Keating, L, Yee, K, Barger, LK, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr (Internet). 2017 (citado 2022 may 24);106(5):1213-1219. doi: 10.3945/ajcn.117.161588 [ Links ]
33. Tavakoli, A, Mirzababaei, A, Mirzaei, K. Association between low carbohydrate diet (LCD) and sleep quality by mediating role of inflammatory factors in women with overweight and obesity: A cross-sectional study. Food Sci Nutr. 2021 (2022 may 3);9(11):6252-6261. doi: 10.1002/fsn3.2584 [ Links ]
34. Hudson, JL, Zhou, J, Campbell, WW. Adults Who Are Overweight or Obese and Consuming an Energy-Restricted Healthy US-Style Eating Pattern at Either the Recommended or a Higher Protein Quantity Perceive a Shift from «Poor» to «Good» Sleep: A Randomized Controlled Trial. J Nutr (Internet). 2020 (2022 may 9);150(12):3216-3223. doi: 10.1093/jn/nxaa302 [ Links ]
35. Muscogiuri, G, Barrea, L, Aprano, S, Framondi, L, Di Matteo, R, Laudisio, D, et al. Sleep Quality in Obesity: Does Adherence to the Mediterranean Diet Matter? Nutrients (Internet). 2020 (citado 2022 feb 6);12(5): 1364. doi: 10.3390/nu12051364 [ Links ]
36. Godos, J, Ferri, R, Caraci, F, Cosentino, FII, Castellano, S, Galvano, F, et al. Adherence to the Mediterranean Diet is Associated with Better Sleep Quality in Italian Adults. Nutrients (Internet). 2019 (citado 2022 may 21);11(5):976. doi: 10.3390/nu11050976 [ Links ]
37. Park, SK, Jung, JY, Oh, CM, McIntyre, RS, Lee, JH. Association Between Sleep Duration, Quality and Body Mass Index in the Korean Population. J Clin Sleep Med (Internet). 2018 (citado 2022 feb 6);14(8):1353-1360. doi: 10.5664/jcsm.7272 [ Links ]
38. Sweatt, SK, Gower, BA, Chieh, AY, Liu, Y, Li, L. Sleep quality is differentially related to adiposity in adults. Psychoneuroendocrinology (Internet). 2018;98:46-51. doi: 10.1016/j.psyneuen.2018.07.024 [ Links ]
39. González, A, López, F, Valencia, M, Espinosa, Á. Partial sleep deprivation on dietary energy intake in healthy population: a systematic review and meta-analysis. Nutr Hosp (Internet). 2020 (citado 2022 ene 27);37(5):1052-60. doi: 10.20960/nh.03108 [ Links ]
40. Hur, S, Oh, B, Kim, H, Kwon, O. Associations of diet quality and sleep quality with obesity. Nutrients (Internet). 2021 (citado 2022 ene 24);13(9):3181. doi: 10.3390/nu13093181 [ Links ]
41. Vidafar, P, Cain, SW, Shechter, A. Relationship between Sleep and Hedonic Appetite in Shift Workers. Nutrients(Internet). 2020 (citado 2022 may 21);12(9):2835. doi: 10.3390/nu12092835 [ Links ]
42. Herrera, D, Ng, C, Durán-Agüero, S, Ríos-Castillo, I. Patrón de sueño, estado nutricional e ingesta dietética en agentes de seguridad de la Ciudad de Panamá: un estudio transversal. Rev Española Nutr Humana y Dietética (Internet). 2021 (citado 2022 feb 14);25(1):48-57. doi: 10.14306/renhyd.25.1.1062 [ Links ]
How to cite: Serra Laborde PL, Torterolo Pizzuti C, Calvo Pesce MS. Sleep Quality and Chronotype and its Relationship with Obesity in the Adult Population. Narrative Bibliographic Review. Enfermería: Cuidados Humanizados. 2023;12(2):e3213. doi: 10.22235/ech.v12i2.3213
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. P. L. S. L. has contributed in a, b, c, d, e; C. T. P. in a, b, c, d, e; M. S. C. P. in a, e.
Received: February 05, 2023; Accepted: October 25, 2023











 text in
text in 



