Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Enfermería: Cuidados Humanizados
versión impresa ISSN 1688-8375versión On-line ISSN 2393-6606
Enfermería (Montevideo) vol.12 no.2 Montevideo 2023 Epub 01-Dic-2023
https://doi.org/10.22235/ech.v12i2.3198
Original Articles
Criteria related to newborns’ safe hospital discharge: An integrative review
1 Universidade Federal da Bahia, Brasil, cintiaraujo2019@hotmail.com
2 Universidade Federal da Bahia, Brasil
3 Universidade Federal da Bahia, Brasil
4 Universidade Federal da Bahia, Brasil
5 Universidade Federal da Bahia, Brasil
6 Universidade Federal da Bahia, Brasil
Keywords: patient discharge; newborn; patient discharge summary; nursing; neonatology
Palavras-chave: alta do paciente; recém-nascido; sumário de alta do paciente; enfermagem; neonatologia
Palabras claves: alta del paciente; recién nacido; resumen del alta del paciente; enfermería; neonatología
Introduction
Qualified hospital discharge, also known as transitional care, is defined as a set of actions aimed at ensuring care continuity and coordination for patients transferred between different health care services or levels, having education for patients and their families as a strategy for safe transitions. (1,2 This is because newborns (NBs) need intensive care in the first days of life and, in some cases, may need technological devices to help maintain comfort and survival in extrauterine life; therefore, it is fundamental to have an action plan with the objective of ensuring NBs a safe transition between the hospital and their home. (2,3
In this sense, the NB safe hospital discharge process must be initiated upon admission of the newborn and their mother, as well as the father, if present in Rooming-In, including welcoming and preparing them for home-based care. In this environment, caregivers will be guided on care with hygiene, nutrition, touch, behavior, interaction and sleep, among other needs and desires of the infant and family. The aim is to reduce the anxiety and stress levels in the family members and the number of health problems and readmissions of newborns, in addition to developing competencies and identifying community resources for monitoring after hospital discharge. (4,5
However, the World Health Organization 6 refers to some recommendations that detail the minimum hospitalization period after the birth of a NB and provide guidelines on discharge criteria. It also advocates respecting the necessary time for the mother/newborn dyad to establish a bond, the birth experience and any health problems that may occur. In addition, it states that post-birth contacts are recommended for healthy mothers and newborns between 48 and 72 hours, between 7 and 14 days and during the sixth week after birth. It is worth noting that, if risks to the health of the dyad are identified after a multiprofessional evaluation, a closer approach by the professionals and hospital services in home monitoring of the NB and their family arrangements after the first six weeks of the NB’s life is recommended.
Absence of this care can collaborate with preventable health problems such as choking, hypothermia, infections, and opportunistic diseases due to delays in the vaccination schedule, among other causes that contribute to neonatal morbidity and mortality. In this context, in preparing for discharge, it is up to nurses to guide, train and supervise the family for NB care continuity at home, as failures in this communication can increase the risk of readmissions and unnecessary rehospitalizations. (1
In the world, according to a study carried out in Italy, the number of rehospitalizations of neonates reaches 34.3 % of the extremely premature infants and 24.4 % of the moderately premature infants in relation to the number of NBs, with a sample of 90,545 newborns. In absolute numbers, this rate corresponds to 25,336 rehospitalized NBs.7 In Brazil, a study carried out in Pelotas showed that this number is 557 rehospitalized NBs, from a sample of 4,231 NBs, equaling approximately 13.17 % of the rehospitalizations, which can be increased when evaluated by regions of greater vulnerability in view of the health services provided. (8
These data can be reflections of a disqualified discharge process, as NBs are more susceptible to hospitalizations and readmissions due to problems arising from childhood, and lack of information and/or ineffective and clear communication can generate space for erroneous and mistaken interpretations, in addition to imposing greater risks of complications due to preventable causes. According to the Brazilian Society of Pediatrics (1 (Sociedade Brasileira de Pediatria, SBP), eight out of every ten newborn deaths could have been avoided; such data refer to the difficulties faced by these families at important moments regarding the transition between the place of birth and their home.
A qualified discharge process with strategic actions can reduce the number of infections, empower parents to safely care for their children, reduce the distress and anxiety caused by returning to a health institution and reduce the hospital costs generated by a readmission. Therefore, an unplanned discharge process, discussed and systematized in view of biological criteria, effective communication and monitoring in the care network, can provide emergency returns of NBs and their caregivers to maternity hospitals. (1
To this end, on October 21st, 2016, the Ministry of Health published Ordinance No. 2,068, which establishes basic guidelines for the organization of comprehensive and humanized care for women and newborns in Rooming-In. This ordinance addresses the minimum criteria for a safe discharge process and proposes that, before discharge, the woman receives all the necessary guidelines to feel safe and capable of taking care of herself and the NB at her home in this new routine. The ordinance also proposes that a Singular Therapeutic Plan must be carried out for discharge, considering the hospitalization time and the individual needs of each of the individuals involved. (9
In this sense, the Ministry of Health of Brazil (Ministério da Saúde, MS) and the SBP highlight some important criteria for safe discharge and for the multiprofessional evaluation of newborns’ physical and biological issues, which may extend to the mothers’, as well as the promotion of effective communication with the parents and support network, resulting in guarantees of connecting the dyad to the basic health unit assigned for the NB follow-up, collaborating to avoiding possible health problems. (1,2
Thus, knowing the main criteria grounded on the literature involved in newborns’ safe discharge can ensure qualified actions. In addition to that, approximation of the practice with to the transitional care theory legitimizes the assistance provided from the hospital to the home. (2,3 This practice contributes to reducing the rehospitalization and morbidity and mortality rates due to situations and health problems that might be identified while still in the maternity ward. (10 Therefore, this study is necessary to synthesize the knowledge about the criteria used to assist in decision-making at the time of newborns’ safe discharge, with a view to developing a discharge protocol and an app targeted at the multiprofessional team.
Faced with the problem presented combined with the morbidity scenario in newborns, potentiated by the increase in rehospitalization in birth units, which can be prevented, increase hospital expenses and disrupt family arrangements, the following question arises: Which are the criteria evidenced by the literature that guide NBs’ safe discharge? The objective of this study was to identify the main criteria involved in newborns’ safe hospital discharge.
Methodology
This is an integrative review with a descriptive approach based on secondary data to obtain an overview of the state-of-the-art regarding the theme. The article was extracted from the Master's Degree thesis entitled “Development of a safe discharge protocol for newborns” from the Graduate Program in Nursing at the Federal University of Bahia and is one of the constructs added as a result of the current research. This study constitutes the first phase for carrying out a methodological study and consists of the content selection stage for later elaboration of technologies aimed at NBs’ safe discharge. This type of review enables a methodological approach regarding reviews, as it allows including experimental and non-experimental studies to fully understand the phenomenon analyzed. (11
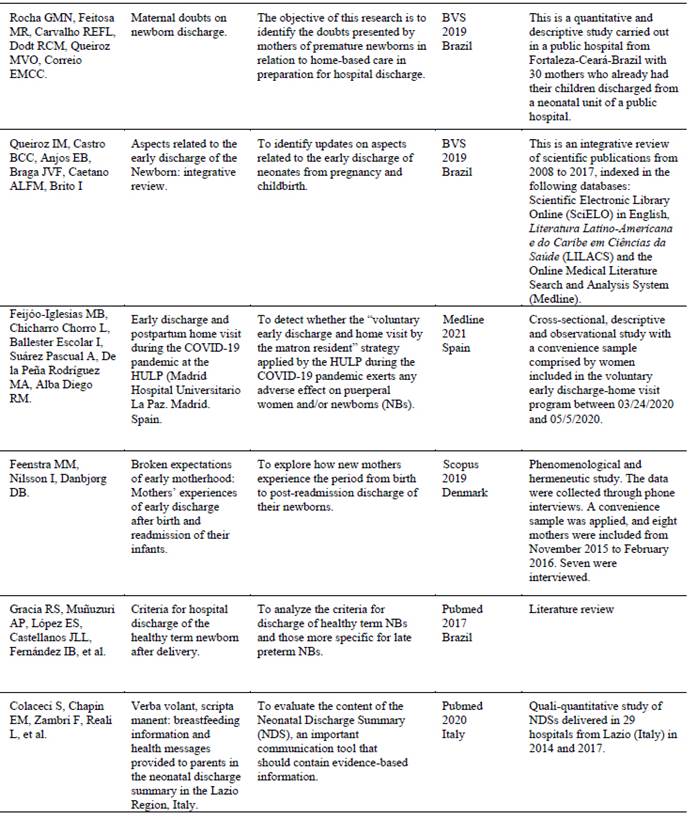
The study followed the steps for elaborating an integrative review proposed by Mendes, Silveira and Galvão (2008) (12 shown in Figure 1.

Figure 1: Stages for carrying out the integrative review on patient discharge in Neonatology in 2021
From this, a review protocol was prepared in order to guide and systematize the searches and selection of studies, characterized by containing the research question and the study objective, the search strategies and Boolean operators to be used in each database, as well as other inclusion and exclusion criteria.
Initially, the research question that guided this review was formulated based on the researchers’ concern: Which are the criteria evidenced by the literature that guide NBs’ safe discharge?
The studies were collected in December 2021 from the PubMed/Medline, BVS, Scopus and LILACS databases, using descriptors that are included in the Health Sciences Descriptors database (Descritores em Ciências da Saúde, DeCS) and in the Medical Subject Headings (MeSH), with the following search strategy: “patient discharge summaries” OR “patient discharge” AND “newborn”. The “OR” and “AND” Boolean operators were used in the bibliographic search strategy (Table 1).
Table 1: Bibliographic search strategy in the databases
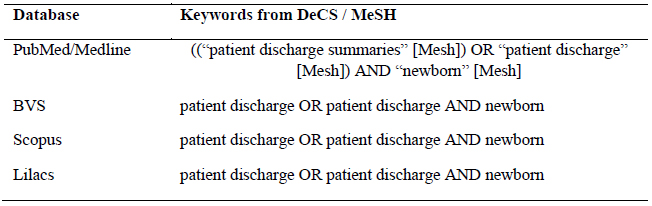
Note: PubMed: Medical Literature Analysis and Retrieval System Online; BVS: Biblioteca Virtual em Saúde; Scopus; Lilacs: Literatura Latino Americana e do Caribe em Ciências da Saúde
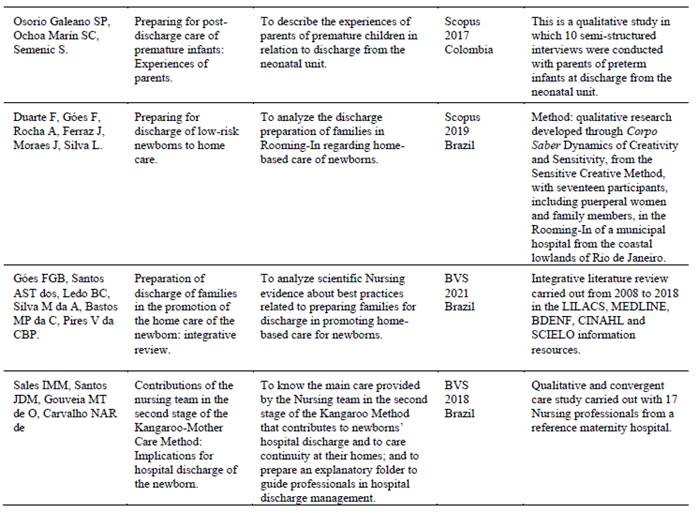
In order to obtain current and relevant evidence for the research scope, eligibility criteria were adopted, and the inclusion criteria were as follows: articles available in full, published in the last 5 years in English, Spanish and Portuguese and dealing with NB care, hospital discharge or discharge of neonatal patients. All articles that did not meet the research objective and/or were not related to the topic under study were excluded, according to the methodological procedures set forth in the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (12 and the flowchart shown in Figure 2.
Figure 2: Study selection flowchart adapted from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 13
An adaptation of the Cochrane Collaboration Checklist (14 was used for data extraction; the articles were read by pairs of researchers, critically analyzed and organized according to the following criteria: author, title, year of publication, journal, objective, method and main results according to the objectives of this research. In turn, the critical evaluation was performed by mapping the loci where the studies were carried out, as well as publication journals according to Qualis.
After extracting all the information, the data related to the parameters were synthesized by categorization, according to a second analysis instrument that contained the description of the parameter identified, the items evaluated, the study title and year of publication. Data analysis was carried out through content analysis (15, in light of Transitional Care. (4
As it contains a methodological approach that does not involve direct research with human beings, the current study did not require submission of the research project to any Research Ethics Committee (Comitê de Ética e Pesquisa, CEP), as advocated by the recommendations set forth in Resolution No. 466 of the National Health Council of December 12th, 2012, which determines the guidelines and regulatory standards for research studies involving human beings. (14 In addition, when selecting the articles, precautions was taken to evaluate those that complied with the ethical precepts of research studies with human beings with approval by the ethics committee and, if applicable, informed consents.
Results
A total of 94 articles were obtained from the search in the databases. Of these, 75 studies were excluded for not meeting the inclusion criteria and 2 for not responding to the objective proposed in this research. Initially, 17 publications submitted to a critical reading process were selected, of which 05 were discarded for not being associated with the theme, resulting in 12 studies included to comprise the review.
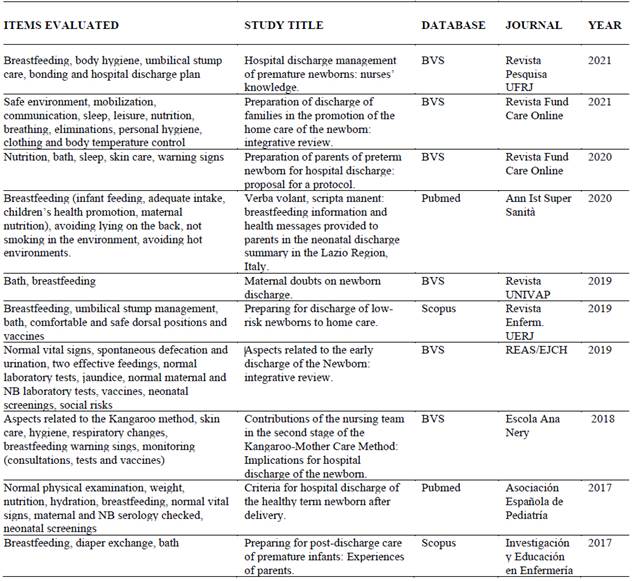
Table 2 describes the publications according to their main aspects, such as author, title of the paper and objectives, as well as indexing database, year of publication and study characterization. Qualification of the journals based on the CAPES classification criteria is noted, with most publications in journals, having two articles in A1 and A2 classification journals, and ten articles in B journals. t7, t8
Table 2: Synthesis of the articles selected according to author, title, objective, database, year, country of publication and characterization of the studies. Salvador, Bahia, Brazil, 2022.
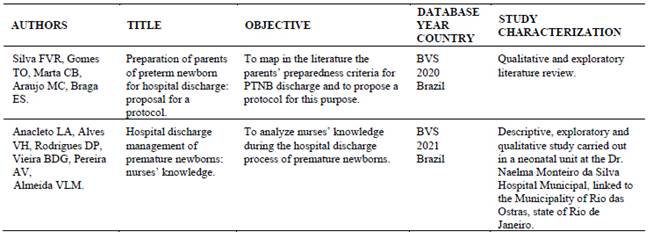
It was found that the twelve studies selected were published between 2017 and 2021, with 75 % of the sample (n=9) being published in the last three years, corresponding to three in 2021, two in 2020 and four in 2019. The other articles (25 % of the selection) were published as follows: two in 2017 and one in 2018, resulting in three articles. As for the loci where the research studies were conducted, most were carried out in Brazil, with three in Rio de Janeiro, (16,17,25 one in Ceará, (18 one in Minas Gerais (19 and one in Piauí. (27 As for the international studies, it was possible to identify one study from each of these countries: Italy, (23 Colombia (24 and Denmark, (21 and two from Spain. (20,22 With regard to the type of study, 66.6 % corresponded to field research studies, five of which were qualitative,16,17,24,25,27 two quantitative (18,20 and one with a mixed approach.(23 Four reviews were included: two integrative, (19,26 one documentary (21 and one bibliographical.20 The qualitative synthesis was carried out based on data collection, with the main biophysiological parameters highlighted and related to newborns’ hospital discharge listed in Table 3 .
Discussion
The discussion of the results was divided into three thematic categories. Of the articles analyzed (n=12), ten provided support for the first category: Biophysiological parameters; (16,17,18,19,20,21,22,23,24,25,26 eight served the second, entitled Communication and guidelines for parents: weaknesses and strengths of the family; (16,18,19,21,23,24,25,26 and seven of them were related to the third, called Post-discharge care: network follow-up. (17,18,20,21,22,27,28
Biophysiological parameters
With regard to an assessment centered on morphofunctional issues with a focus on biophysiological balance in safe hospital discharge processes, a careful evaluation of the mother-newborn dyad is necessary, as well as of the health status of both for a possible combined hospital discharge. However, there are cases in which NBs need to remain hospitalized to confirm and/or exclude diagnoses, as well as to solve health changes that can be observed according to some specific parameters.
Therefore, some fundamental physiological aspects need to be ensured before NBs’ safe hospital discharge. Initially, one of the main aspects refers to the healthy birth condition, without any morphological alteration that might compromise NBs’ adaptation and development with extension to the vital data within a normal pattern for their gestational age. (2 Subsequently, the focus is on monitoring and encouraging breastfeeding (16,18,25 and effective feedings (25 as parameters that make up the list of criteria used to support the discharge decision.
In turn, seen more broadly, nutrition (17,22,27 can encompass both breastfeeding and the need to provide formulas and/or referrals to milk banks. These components are cited both as criteria for preventing excessive weight loss accompanied by dehydration, (26 and as part of the criteria evaluated in the discharge process.
Other criteria are related to hyperbilirubinemia and laboratory tests, (21,23 as they are identified as determining factors for the return of NBs to hospital units. It is important to emphasize that severe bilirubin levels and their evolution imply monitoring by maternity hospitals regarding outpatient returns in the neonates’ first week of life. Performing universal neonatal screening tests(21,27 and screening for metabolic disorders in the presence of maternal and/or neonatal risk factors are also important components that make it possible to intervene early in time and prevent complications referring to neonatal morbidity and mortality.
Addressing risk factors and review of maternal and gestational history for the detection of early neonatal sepsis in asymptomatic NBs are also pointed out as criteria, in addition to performing serology tests for congenital infections. (21,26 Allied to this, it is also important to carry out a review of the NB physical and clinical evolution examination, in order to monitor dystocias and health problems that may occur during the post-birth period.1,21,24 This approach is very important, as they are essential to define the appearance of health problems and negative outcomes in NBs’ clinical evolution, especially in the first weeks of life.
In this context, one of the most used ways to evaluate effectiveness of NBs’ safe hospital discharge refers to the hospital readmission rate of these neonates, a fact that confirms lack of attention and accuracy regarding the biophysiological criteria listed by national and international bodies, or indicated by scientific evidence, combined with the absence of care protocols aimed at humanizing and systematizing qualified discharge of these patients and their families. (16
In view of this, it is important to note the actions of nurses who, through the consultations and adopting the frameworks of basic human needs, can assess NBs inorder to ensure greater accuracy in the effectively conducting a safe discharge process. Therefore, instruments such as clinical examination and evaluation of laboratory tests can be important strategies that establish accuracy and safety so that nurses can make an adequate assessment.
Finally, all the parameters listed will provide support for decision-making that contributes to effectively conducting a safe discharge process. Thus, the appropriate moment will be conditioned to achieving clinical stability in the NB, (18 although it needs to be combined with the criteria and factors listed in the cited studies.
Communication and guidelines for parents: weaknesses and strengths of the family
Effective multiprofessional communication is considered a facilitator in the process and preparation of newborns’ safe hospital discharge. The hospitalization process requires the multiprofessional team to welcome the neonates’ parents and family arrangements, from hospitalization to preparation for the NBs’ hospital discharge. (17
The guidelines on the NBs’ biophysiological parameters should include aspects such as hygiene, nutrition, handling, behavior, interaction, sleep and rest, among other basic needs. (4,5 These guidelines can comprise the families’ preparation for home-based care of the newborn sin the discharge process from the maternity hospital and should be initiated when the dyad is admitted to Rooming-In, or even in other care sectors that may favor opportune moments for the life guidelines.
In this way, the Nursing team, especially nurses, plays a relevant role in interprofessional and family communication regarding the hospitalization and can assume NBs’ safe hospital discharge process, (17 as it guides parents and other family members to solve daily difficulties with regard to child care, mainly aiming to remedy possible issues through the guidelines.
Therefore, the studies pointed to using educational technologies such as explanatory folders, booklets, videos, storyboards, checklists, home supervision programs(28 and focus group dynamics(15,18 as strategies that enable integration and communication, in addition to clear and accessible guidelines for parents in the NB discharge context.
In this sense, involvement between the family and the multiprofessional team is necessary in order to reduce nurses’ exclusive duty regarding information and guidance at the time of discharge,(17 having to consider the importance of each category involved in this procedure, as they have knowledge that enables this communication between the subjects. Therefore, these educational practices need to have an interdisciplinary focus and should be adopted in an integrated and articulated way with a view to safe NB home-based care.
In a descriptive study (18 carried out with 30 mothers who had already scheduled their children’s hospital discharge in a neonatal unit of a public hospital, 18 of them (60 %) would like to know more about bathing. Doubts about breastfeeding ranked second, being reported by 17 participants (56.7 %). In turn, choking was third as the most frequent doubt.
Also according to this study, (17 when these mothers were asked about previous guidelines on their newborns’ hospital discharge, only 12 of the 33 surveyed were instructed on the topic. In turn, in relation to safety in the daily care of the child at home, only 11 of them answered that they were prepared or confident and regarding breastfeeding, whereas 10 answered that they felt prepared.
Regarding the relationship issues, one study (16 shows that communication is an important factor and is part of every health professional’s routine. In the NB hospitalization process, the anxiety and stress of the parents and relatives generated by the hospitalization can make it difficult to assimilate the diverse information provided by the professionals, leading to an erroneous feeling of Nursing team disarticulation in relation to the patient’s family arrangements.
The limitations that hinder communication refer to some specific characteristics of the parents. Thus, in the context of mothers who use drugs, with intellectual and cognitive limitations(26,27 and with low schooling levels, teenage mothers and the absence of caregivers at the hospital due to financial and social issues, (18,19,23,24 negatively interfere with the assimilation of important guidelines at the time of hospital discharge, thus making it unfeasible at that moment.
In addition, the processes of communication and inclusion of parents and caregivers related to preparation for hospital discharge show health maintenance at home(25,26,27and thus, in addition to providing a space for identification and intervention in the face of social risks, (20 they contribute to preventing readmissions. From this, it is sought to reduce the mothers’ anxiety and stress levels and family arrangements, health problems and rehospitalizations of NBs, in addition to contributing to the development of competencies and the identification of community resources for monitoring after hospital discharge. (4,5
Based on this assumption, preparation for hospital discharge needs to be constructed from a problematizing perspective, based on people’s concrete reality. It is fundamental to break with the verticality of relationships and the mere transmission of information -without involvement- to establish a transversal and dialogical relationship between nurses, parents and their families.
Post-discharge care: network follow-up
An important aspect for hospital discharge is the instructions for post-discharge follow-up as one of the aspects for proper transitional care in the network. (3,7 Thus, immediately after birth, it is necessary to establish the follow-up to be carried out through frequent contacts and periodic consultations, as well as carrying out tests at opportune times according to each newborn’s specificities, including administration of vaccines according to the recommended vaccination schedule. (17,18
In this context, during the hospital discharge period, in addition to favoring the development of competencies for caregivers and family members, it is necessary to encourage and guide them towards the identification of community resources for monitoring after hospital discharge to promote care in the home environment and in the connection to the care network. (4,5 Only then is it possible to establish an adequate transition that meets the needs during this period in which care is alternated between health professionals and home caregivers. (3,17,28
Some measures can be implemented even during the hospitalization period when newborn’s clinical stability is achieved, such as the development of educational interventions aimed at ensuring continuity of adequate care after hospital discharge. The literature shows that follow-up in programs such as the Kangaroo Method is observed as a family monitoring facilitator, in addition to enabling phone communication with the unit’s staff in case of doubts. (20
Several studies show that the recommendation for initiating follow-up is that the first post-discharge consultation should take place immediately, before the end of the first week of life.(21,28 For example, the American Academy of Pediatrics (29 recommends that all newborns discharged before 48 hours be evaluated within the first 48 hours after discharge, to encourage breastfeeding and ease the detection of jaundice, as well as of other health problems that are manifested and diagnosed in the first two days of life. (21
For these recommendations to be followed and enable better control, it is important to carry out these measures from hospitalization with educational activities that reinforce their proper application by the mother and family. (22 As an example, through the implementation of the child’s health booklet, it is possible to follow-up growth and development, monitor the immunization chart and record all parameters from birth, in addition to promoting scheduling of tests and screenings.
Other studies show how contact at home, whether by telephone or video calls, can be considered a useful strategy to provide guidelines and care measures. (27 In addition, a well-consolidated referral and counter-referral method is required, capable of promoting integration between the care levels and favoring resoluteness in welcoming NBs and family arrangements in the post-discharge context.
As a result, it is clear that the network follow-up is extremely important to enable continuity of the measures that encourage healthy growth and development in order to provide safe transitions. For this, in addition to initiatives during the hospitalization, communication across the care levels and effective monitoring are necessary, with provision of services and care in the network and at the children’s homes, in order to ease detection and early intervention in case health problems arise, thus avoiding readmissions.
Study limitations
Few articles were found in the literature, which consequently generates a scientific gap in relation to the topic, imposing limitations regarding the number of findings that reinforce the criteria listed, with greater emphasis on biophysiological criteria. Therefore, in addition to broadening the debate about the specificities related to newborns, it is also necessary to enable the implementation of tools capable of assisting in the effective implementation of this process.
In relation to patient safety, there is certain limitation in the ordinances, which still do not deal specifically with this topic, as the existing ordinances include protocols for patient safety but there is no specific protocol for newborns’ safe hospital discharge.
Conclusion
Qualified hospital discharge of newborns requires some specificities and organized, multiprofessional and intersectoral planning with the involvement of parents and family arrangements included in the newborn’s support network. Therefore, this review achieved the objective proposed by listing and discussing the main criteria involved in newborns’ safe hospital discharge. It is reasserted that evaluation and monitoring of biophysiological parameters based on the Theory of Basic Human Needs, effective and individualized communication directed at parents, enabling an interactive dialog between the professionals involved, in addition to post-discharge care and network follow-up, are crucial for establishing a qualified discharge process.
Thus, following these criteria favors improvements in the evaluation of hospital discharge, preventing readmissions in the units where the births took place. Thus, effective communication assists in carrying out timely practices and training options such as on bathing, diaper exchange, umbilical stump hygiene and breastfeeding promotion, among other actions that strengthen the safe discharge of newborns and families. In addition to that, the criteria aimed at post-discharge care guided by proper guidelines, as well as referrals to the support network with timely and objective referral to the care system and monitoring of NBs and families in Primary Care, favor guarantees in terms of returning to the maternity hospital in the face of any health problem.
It is also concluded that the study offers contributions to Nursing in transitional care, in the sense of improving health care and quality of the care provided to NBs based on the overview obtained on the theme. The need for further studies is highlighted in order to explore how these criteria are related to health outcomes in this population group in terms of morbidity and mortality, as well as to develop and implement protocols to qualify safe discharge processes that develop specific actions for this theory. Therefore, the “hospital discharge” topic represents a fertile field to be explored and can offer contributions to the literature that reflect on the care field.
REFERENCES
1. Sociedade Brasileira de Pediatria. Recomendações para alta hospitalar do recém-nascido termo potencialmente saudável. (Internet); 2020 (acesso em 2022 jan 14). Disponível em: Disponível em: https://www.sbp.com.br/fileadmin/user_upload/22649c-DC_Recom_Alta_hospitalar_RN_TermoPotenc_Saudavel.pdf [ Links ]
2. Ministério da Saúde; Organização Pan-Americana da Saúde. Manual AIDPI Neonatal. 5a. ed. Brasília: Ministério da Saúde; Organização Pan-Americana da Saúde; 2014. [ Links ]
3. Lima, MADS, Magalhães, AMM, Oelke, ND, Marques, GQ, Lorenzini, E, Weber, LAF, et al. Care transition strategies in Latin American countries: an integrative review. Rev. Gaúcha Enferm. 2018;39:e20180119. doi: 10.1590/1983-1447.2018.20180119 [ Links ]
4. Alcântara, KL, Brito, LLMS, Costa, DVS, Façanha, APM, Ximenes, LB, Dodt, RGCM. Family guidelines needed for a safe hospital of the premature newborn: integrative review. Rev Enferm UFPE. 2017 (acesso em 2021 jan 25);11(2):645-55. doi: doi: 10.5205/reuol.10263-91568-1-RV.1102201720 [ Links ]
5. Falkenberg, MB, Mendes, TPL, Moraes, EP, Souza, EM de. Health education and education in the health system: concepts and implications for public health. Ciênc Saúde Coletiva. 2014 (acesso em 2022 jan 27); 19(3):847-52. doi: doi: 10.1590/1413-81232014193.01572013 [ Links ]
6. Organização Mundial da Saúde. A OMS pede atenção de qualidade para mulheres e recém-nascidos nas primeiras semanas cruciais após o parto. (Internet); 2022 (acesso em 2023 jul 08). Disponível em: Disponível em: https://www.paho.org/pt/noticias/30-3-2022-oms-pede-atencao-qualidade-para-mulheres-e-recem-nascidos-nas-primeiras-semanas [ Links ]
7. Corchia, C, Lapucci, E, Franco, F, Farchi, S, Petrou, S, Di Lallo, D. Gestational age and hospital utilization: three-years follow-up of an area-based birth cohort. Ann Ist Super Sanità. 2016;52(4):543-549. [ Links ]
8. Santos, IS, Barros, FC, Munhoz, T, Matijasevich, A. Gestational age at birth and behavioral problems from four to 11 years of age: birth cohort study. Pediatrics. 2017;(17):184. doi: 10.1186/s12887-017-0936-3 [ Links ]
9. Ministério da Saúde (Brasil). Portaria nº 2.068, de 21 de outubro de 2016. Institui diretrizes para a organização da atenção integral e humanizada à mulher e ao recém-nascido no Alojamento Conjunto. Diário Oficial da União 24 out 2016; Seção 1. [ Links ]
10. Harron, K, Gilbert, R, Cromwell, D, Oddie, S, van der Meulen, J. Newborn Length of Stay and Risk of Readmission. Paediatric and Perinatal Epidemiology. 2017 (acesso em 2022 jan 20);31(3):221-232. doi: doi: 10.1111/ppe.12359 [ Links ]
11. Whittemore, R, Knafl, K. The integrative review: update methodology. J AdvNurs. 2005 (acesso em 2022 fev 07);52(5):546-53. doi: doi: 10.1111/j.1365-2648.2005.03621.x [ Links ]
12. Mendes, KDS, Silveira, RCCP, Galvão, CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto Enferm. 2008 (acesso em 2022 fev 07);17(4):758-64. doi: doi: 10.1590/S0104- 07072008000400018 [ Links ]
13. Moher, D, Liberati, A, Tetzlaff, J, Altman, DG, Altman, D, Antes, G et al. Itens de relatório preferidos para revisões sistemáticas e meta-análises: a declaração PRISMA. Fisioterapia. 2009;89(9):873-880. [ Links ]
14. Cochrane. Checklist and Guidance. For disseminating findings from Cochrane intervention reviews (Internet); 2019 (acesso em 2021 out 11). Disponível em: Disponível em: https://training.cochrane.org/sites/training.cochrane.org/files/public/uploads/Checklist%20FINAL%20version%201.1-1_0.pdf [ Links ]
15. Minayo, MCS. O desafio do conhecimento: pesquisa qualitativa em saúde. 12ª ed. São Paulo: Hucitec; 2010. [ Links ]
16. Silva, FVR, Gomes, TO, Marta, CB, Araujo, MC, Braga, ES. Preparo dos pais de recém-nascido pré-termo para alta hospitalar: proposta de um protocolo. Rev Fun Care Online. 2020 (acesso em 2022 jan 24);12:386-392. doi: doi: 10.9789/2175-5361.rpcfo.v12.8264 [ Links ]
17. Anacleto, LA, Alves, VH, Rodrigues, DP, Vieira, BDG, Pereira, AV, Almeida, VLM. O manejo da alta hospitalar do recém-nascido prematuro: saberes dos enfermeiros. Pesqui. (Univ. Fed. Estado Rio J., Online);13:634-639. doi: 10.9789/2175-5361.rpcfo.v13.9359 [ Links ]
18. Rocha, GMN, Feitosa, MR, Carvalho, REFL de, Dodt, RCM, Queiroz, MV de O, Chaves, EMC. Dúvidas maternas na alta hospitalar do recém-nascido. RevistaUnivap (Internet). 2019 (acesso em 2022 jun 17);25(49):93-103. doi: doi: 10.18066/revistaunivap.v25i49.1968 [ Links ]
19. Queiroz, IM, Castro, BC, Anjos, EB, Braga, JVF, Caetano, ALFM, Brito, II. Aspectos relacionados à alta precoce do Recém-Nascido: revisão integrativa. Revista Eletrônica Acervo Saúde. 2019 (acesso 2022 jun 17);(34):e1338. doi: doi: 10.25248/reas.e1338.2019 [ Links ]
20. Feijóo-Iglesias, MB, Chicharro Chorro, L, Ballester Escolar, I, Suárez Pascual, A, De la Peña Rodríguez, MA, Alba Diego, RM. Early discharge and postpartum home visit during the COVID-19 pandemic at the HULP (Madrid). Esp Salud Publica. 20,21 (acesso em 2022 jun 17);95:e202108105. PMID: 34408124. [ Links ]
21. Feenstra, MM, Nilsson, I, Danbjørg, DB. Broken expectations of early motherhood: Mothers' experiences of early discharge after birth and readmission of their infants. J Clin Nurs. 2019 (acesso em 2022 jun 17);28(5-6):870-881. doi: doi: 10.1111/jocn.14687. PMID: 30302846. [ Links ]
22. Gracia, RS, Muñuzuri, AP, López ES, Castellanos JLL, Fernández IB, Campillo CWR, et al. Critérios de alta hospitalia del recém-nascido a termo sano tras el parto. An. pediatr. 2017;86(5):289.e1-289.e6. doi: 10.1016/j.anpedi.2016.08.011 [ Links ]
23. Colaceci, S, Chapin, EM, Zambri, F, Reali, L, Cedrone, L, Del Brocco, A, et al. Verba volant, scripta manent: breastfeeding information and health messages provided to parents in the neonatal discharge summary in the Lazio Region, Italy. Ann Ist Super Sanita. 2020;56(2):142-149. doi: 10.4415/ANN_20_02_03. PMID: 32567563. [ Links ]
24. Galeano, SPO, Ochoa Marín, SC, Semenic, S. Preparing for post-discharge care of premature infants: Experiences of parents. Invest Educ Enferm. 2017;35(1):100-106. doi: 10.17533/udea.iee.v35n1a12. PMID: 29767929. [ Links ]
25. Duarte, F, Góes, F, Rocha, A, Ferraz, J, Moraes, J, Silva, L. Preparo de alta para o cuidado domiciliar de recém-nascidos de baixo risco. Revista Enfermagem UERJ. 2019;27:e38523. doi: 10.12957/reuerj.2019.38523 [ Links ]
26. Góes, FGB, Santos, AST dos, Ledo, BC, Silva, M da A, Bastos, MP da C, Pires, V da CBP. Preparo de alta de famílias na promoção dos cuidados domiciliares do recém-nascido: revisão integrativa. Revista Pesqui sa Cuidado Fundamental. 2021;13:1249-55. doi: 10.9789/2175-5361.rpcfo.v13.9458 [ Links ]
27. Sales, IMM, Santos, JDM, Rocha, SS da, Gouveia, MT de O, Carvalho, NAR de. Contributions of the nursing team in the second stage of the Kangaroo-Mother Care Method: Implications for hospital discharge of the newborn. Esc Anna Nery (Internet). 2018;22(4):e20180149. doi: 10.1590/2177-9465-EAN-2018-0149 [ Links ]
28. Aued ,GK, Bernardino, E, Silva, OBM da, Martins, MM, Peres, AM, Lima, LS de. Competências da enfermeira de ligação na alta hospitalar. Rev Gaúcha Enferm (Internet). 2021 (acesso em 2022 fev 7);42(1). doi: doi: 10.1590/1983-1447.2021.202002 [ Links ]
29. Committee on Fetus and Newborn. Hospital stay for healthy term newborns. Pediatrics. 2010 (acesso 2022 fev 3);125(2):405-409. doi: doi: 10.1542/peds.2009-3119 [ Links ]
How to cite: Araujo CMMO de, Silva CT dos S, Macedo FL de C, Silva JC da, Palombo CNT, Martins RDF. Criteria related to newborns’ safe hospital discharge: An integrative review. Enfermería: Cuidados Humanizados. 2023;12(2):e3198. doi: 10.22235/ech.v12i2.3198
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. C. M. M. O. D. A. has contributed in a, b, c, d; C. T. D. S. S. in a, b, c, d; F. L. D. C. M. in a, b, c, d; J. C. D. S. in d, e; C. N. T. P. in d, e; R. D. F. M. in d, e.
Received: February 01, 2023; Accepted: July 19, 2023











 texto en
texto en