Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.12 no.1 Montevideo 2023 Epub June 01, 2023
https://doi.org/10.22235/ech.v12i1.3018
Original articles
Types of care for people with mental health disorder from the perspective of family members
1Prefeitura Municipal de Camaçari, Brasil, leizanazareth@yahoo.com.br
2Universidade Federal da Bahia; Universidade do Estado da Bahia, Brasil
Objective:
To identify the types of daily care for people with mental health disorder from the perspective of family members.
Method:
This is an exploratory and descriptive study with a qualitative approach. Data collection was carried out using semi-structured interviews with fifteen family members of people with mental health disorder followed up in a specialized mental health service in a city in the Northeast of Brazil. The data was organized and analyzed according to the thematic content analysis technique and discussed based on the literature.
Results:
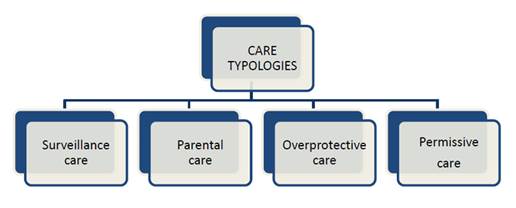
The profile of the family members interviewed was characterized by a majority of female gender, black race, residing in the same household as the person with mental health disorder, with the mother being the main caregiver and with support from the other family members in the care. The main types of care were identified as: 1) vigilant care; 2) parental care; 3) overprotective care; 4) permissive care.
Conclusion:
The family cares for the person with mental health disorders according to their possibilities, however, some factors such as lack of knowledge, stigmas and prejudices can negatively interfere in the psychosocial rehabilitation and autonomy of the person. It is important that the health team provides guidance and support for family members, in order to promote integral care.
Keywords: standard of care; family; caregivers; mental health assistance
Objetivo:
Identificar os tipos de cuidados cotidianos às pessoas com transtorno de saúde mental na perspectiva dos familiares.
Método:
Trata-se de um estudo exploratório e descritivo de abordagem qualitativa. A coleta de dados foi realizada utilizando-se da entrevista semiestruturada com quinze familiares de pessoas com transtorno de saúde mental acompanhadas num serviço especializado de saúde mental numa cidade no Nordeste do Brasil. Os dados foram organizados e analisados segundo a técnica de análise de conteúdo temática e discutidos com base na literatura.
Resultados:
O perfil dos familiares entrevistados caracterizou-se pela maioria do gênero feminino, raça negra, residentes no mesmo domicílio que a pessoa com transtorno de saúde mental, sendo a mãe a principal cuidadora e com apoio dos demais familiares nos cuidados. Foram identificados como principais tipos de cuidados: 1) cuidado de vigilância; 2) cuidado parental; 3) cuidado superprotetor; 4) cuidado permissivo.
Conclusão:
A família cuida da pessoa com transtorno de saúde mental de acordo com suas possibilidades, entretanto alguns fatores como a falta de conhecimento, os estigmas e os preconceitos podem interferir negativamente na reabilitação psicossocial e autonomia dessa pessoa. É importante que a equipe de saúde forneça orientações e suporte aos familiares de modo a promover um cuidado integral.
Palavras-chave: padrão de cuidado; família; cuidadores; atenção à saúde mental
Objetivo:
Identificar los tipos de cuidados cotidianos de las personas con trastorno de salud mental desde la perspectiva de los familiares.
Método:
Se trata de un estudio exploratorio y descriptivo con enfoque cualitativo. La recopilación de datos se realizó mediante entrevistas semiestructuradas con quince familiares de personas con trastorno de salud mental que son acompañadas en un servicio especializado en salud mental en una ciudad del Nordeste de Brasil. Los datos se organizaron y analizaron según la técnica de análisis de contenido temático y se discutieron con base en la literatura.
Resultados:
El perfil de los familiares entrevistados se caracterizó por ser mayoritariamente del género femenino, de raza negra, y por vivir en el mismo domicilio que la persona con trastorno de salud mental, siendo la madre la cuidadora principal, con apoyo de otros familiares en el cuidado. Los principales tipos de cuidado identificados fueron: 1) cuidado vigilante; 2) cuidado parental; 3) cuidado sobreprotector; 4) cuidado permisivo.
Conclusión:
La familia cuida a la persona con trastorno de salud mental de acuerdo a sus posibilidades, sin embargo, algunos factores como la falta de conocimiento, estigmas y prejuicios pueden interferir negativamente en la rehabilitación psicosocial y autonomía de esa persona. Es importante que el equipo de salud brinde orientación y apoyo a los familiares para promover una atención integral.
Palabras clave: nivel de atención; familia; cuidadores; atención a la salud mental
Introduction
The act of caring is intrinsic to the human condition and occurs in a specific manner depending on the historical, social and cultural environment. Generally, caring is associated with the production of life and support. 1 In this process, it is perceived that the family plays a fundamental role in informal care. It is non-professionalized, the caregiver is not remunerated, it can be undertaken by a family member, a friend or neighbor. It is important to note this care is mainly performed by women, especially mothers, but also wives, sisters, daughters-in-law, and sisters-in-law. 2
When a family member has a mental health disorder, family members need to adapt to new behaviors and understanding, and this can cause ambivalent feelings in relation to the care given to the person. In this context, the definition of a mental health disorder is defined as severe psychic impairment that significantly affects the person’s life in several dimensions, namely: work, leisure, personal and family life. Consequently, these impairments bring suffering to the person with the disorder and their family. 3
In this scenario, caring for a loved one with a mental health disorder can be a very challenging experience and is often surrounded by stigma and prejudice. There are many fictions concerning mental health disorders, these are generally related to mental incapacity and the person being dangerous and unstable. These are a result of the historical conception which associated “madness” with evil spirits and the disturbance of the social order. 3) So historically, the family were removed from caring of people with mental health disorders, since they were “treated” in asylums and the presence of the family was prohibited, since it was held responsible for the mental illness of their loved one. 4
The Psychiatric Reform Movement in Brazil, instituted in the late 1970s, culminated in the Psychosocial Care Model. This focuses on the centrality of care for the person with a mental health disorder within a social context by looking at where they live and work. In this new paradigm, the family gained prominence in caring for users of substitutive services, especially within the Psychosocial Care Centers structure (CAPS). 4
In the context of the Brazilian Psychosocial Care Model, the CAPS are health centers that serve people with severe and/or persistent mental health disorders within their communities, CAPS offers psychosocial and clinical care, social and family reintegration (based on the strategies of access to work, citizenship and leisure), thus avoiding hospitalization of those with a mental health disorder. 4,5
The CAPS modalities vary according to complexity and population coverage, and function as follows: CAPS I: psychosocial care service that serves municipalities with a population of over 15,000 inhabitants, offering care to all age groups and people with psychological distress related to the use of psychoactive substances; CAPS II: present in municipalities with a population of over 70,000 inhabitants, assisting intense psychic suffering related to severe and persistent mental suffering or the use of psychoactive substances; CAPS III: serves municipalities with a population of over 150,000 inhabitants. CAPS III operates 24 hours a day, including holidays and weekends, offering night care for other mental health services, including CAPS ad (alcohol and drugs). 6
It is important to highlight that the CAPS, in addition to working directly with service users, also plays a fundamental role in the organization of care. In this CAPS, professionals work in partnership with the Family Health Strategy teams, an assistance model of Primary Health Care, to promote and trigger inter-sectoral resources necessary for comprehensive care. The actions aimed at the use of community spaces and territory should be privileged by psychosocial care services, thus enabling social inclusion of people with mental health disorders in the community. 6,7
To achieve this, it is important that the family is utilized in the process as a partner, welcoming the family member with a mental health disorder and contributing to the positive evolution of their treatment and care plan. Living with a family member with a mental health disorder requires behavioral changes in family life, and can affect social, work and leisure life, there may have to be a reduction in working hours, or a family member having to leave their job, thus accentuating existing financial difficulties, and generating contradictory feelings such as anxiety, concern, shame, revolt, guilt, and fear. (7,8
These changes in the family environment interfere in the daily lives of these people, as all the actions that are shared on a daily basis, the oppression of the present, the overload of life and the difficulties of living, as well as the drastic disruption to be experienced for these families. 9
It is worth noting the feelings that emerge in these families in their daily lives from the diagnosis of a family member’s mental health disorder are intensified, due to the prejudice, exclusion and stigma directed at people with a mental health disorder which extends to the family nucleus, which may promote discrimination against people within the family itself. 9
And, in moments of crisis experienced by these individuals, the picture becomes more dramatic, since crises in people with mental health disorders are associated with aggression, justifying acts of punishment for these people who, in many cases, are victims of violence and humiliation, causing more exclusion and also impacting the daily lives of their families. 4
It is clear that society has difficulties in receiving and caring for people with mental health disorders, which leads to their marginalization. It is important to emphasize that, in many cases, the family environment can replicate exclusion and prejudice, due to lack of understanding or sensitivity regarding mental health, with family members believing that behaviors presented by their loved ones can be controlled or are intentional.8
Thus, it demonstrates the relevance of the study with a view to a discussion about the family members, so that they receive instruction, guidance, and support, so they may understand their feelings in relation to a member with a mental health disorder. In addition to understanding the importance of their role in achieving an effective standard of care for that person; enabling social inclusion and preventing the family space from becoming yet another place of prejudice and stigma.
By highlighting this issue, the present study is justified in view of its importance in understanding and discussing the family’s perspective for the care of the family member with a mental health disorder, and allowing a description of how this care can be given in its diversities and different social contexts. It is based on the assumption that expectations are to produce professional care, from an interdisciplinary perspective, directed by a Psychosocial Care Network through access, reception and bonding 10 to the person with mental health disorder and their family.
The present study aims to contribute to the production of knowledge about the subject, since there is a lack of studies that identify the main types of care offered to people with mental health disorders from the perspective of family members. This is relevant when one considers the need to propose interventions that contribute to improving the quality of life of users and their families, attending to the singularities of all involved individuals. Thus, the study aims to identify the types of daily care for people with mental health disorders from the perspective of family members.
Method
This is an exploratory and descriptive study, with a qualitative approach, which aims to discuss care directed at people with mental health disorders. For this, the qualitative approach is specified, given that the researched phenomenon is not quantifiable, and requires greater depth and subjectivity in order to seek the interrelationship with experiences, values, beliefs and motivations of the participants. 11
The construction of the manuscript followed the recommendations of COREQ (Consolidated Criteria for Reporting Qualitative Research) meeting the scientific requirements for the development of studies with a qualitative approach. 12 Fifteen family members of people with mental health disorders who were followed up at a specialized mental health service participated in the study. The choice of location was made because it is a reference unit in a medium-sized municipality in Northeast Brazil, with more than 300,000 inhabitants, and which has four substitutive mental health services, including a CAPS modality III that must operate for 24 hours a day.
Data collection took place between the months of February and August 2021, the participants were identified according to the patient registration at the health unit and data collection was ended when it showed signs of saturation, when it was not possible to observe new information about the studied phenomenon. The following inclusion criteria were defined: being a caregiver of a person with a mental health disorder and over 18 years of age, and as exclusion criteria, the family caregiver who received remuneration for the provision of care.
For data collection, a semi-structured interview was used, which consisted of an instrument, prepared by the authors, contemplating in the first part the characterization of each participant according to the variables: age, sex, education (years of study), race, religion, occupation, marital status, degree of kinship, how long you have been caring for your loved one, if you are the main caregiver, if you receive care support, if you live in the same household, in addition to the clinical diagnosis of the person with a mental health disorder .
The second part consisted of a semi-structured script with the following open questions: 1) Talk about how you take care of a person with a mental health disorder. 2) How do you interact with the psychological and organic signs and symptoms presented by him/her? 3) What are the most common feelings related to the care provided by you? At some points do you feel guilty, ashamed, angry, sad about this experience? 4) Do you have any difficulties taking care of him/her? 5) What do you notice that helps or facilitates you in taking care of him/her?
The interviews took place in a private environment, with an average duration of 20 minutes, were audio-recorded and later transcribed and processed.
Data analysis was performed based on its organization according to the thematic content analysis technique (CAT), proposed by Bardin (13 and, based on the construction of the textual corpus resulting from the responses of all participants in an artisanal method. This methodological procedure is called ‘artisanal’, that is without the aid of software, and each step of the CAT technique was conducted bit by bit, using tables, charts and marking resources, use of different colors and word count in the editor of Microsoft Word v. 2016.
To this end, the following stages were developed: 1) pre-analysis, when the entire material resulting from the interviews was read exhaustively; 2) the exploration of the material, where a synoptic table was created with the corpus of the research contemplating all the participants’ answers, allowing the researcher to make segmentations in record units (RU), searching for their convergences and divergences. The units were separated by color to facilitate identification and visualization. From this table, it was possible to categorize and codify the units of meanings (US) and, finally, 3) the treatment of the results, which allowed to aggregate and privilege the thematic categories (TC) pertinent to the object of study, in order to be analyzed and discussed based on the literature. 13
During the analysis process as described about the CAT and based on the coding of the US, four TC emerged, namely: 1) surveillance care; 2) parental care; 3) overprotective caregiving and 4) permissive care.
When presenting the RU in the results, to ensure confidentiality, the participants were identified with the names of Brazilian trees, such as Quaresmeira, Ipê, Araçá, Jacarandá, among others. The tree analogy was adopted with the understanding that trees are symbolically associated with family structure and connection.
The study was appreciated and approved by the Ethics and Research Committee of the State University of Bahia, under opinion n.º 4.427.991. All participants received the necessary clarifications and upon accepting to participate in the study, they signed the Free and Informed Consent Form (TCLE).
Results
Characterization of the participants
Of the 15 participants, the majority (12) were female, aged between 20 and 75 years. Regarding race, 11 of them declared themselves to be black and the same number were those who lived with the person with a mental health disorder. Among the caregivers, mothers prevailed, eight of them in total, but there were also sisters, aunts, husbands, children and fathers. “Schizophrenia” was the predominant medical diagnosis in the medical records of 11 of the users, followed by three people diagnosed with depression and one with bipolar mood disorder. Among the interviewees, nine have family support in care and six do not receive any kind of support.
From the record units, four thematic categories representative of the types of care emerged: F1
Category 1: Surveillance care
This care was the most mentioned by the caregivers, being understood as a need to maintain constant attention to the behaviors presented by the person with a mental health disorder and based on discipline measures such as medication containment and protection through control and surveillance. It was a form of care based on the fear that the person will show unpredictable, aggressive behavior or new crises.
Today his care is only surveillance (Araçá).
So, my care is a lot of attention, it’s being around all the time, I’m talking to her, even random things! Things she likes to talk about, trying to do things she likes to do, is always near her even when she’s sleeping. Be careful to give her the medicine at the right time (...). So, the care is basically 24 hours a day (Jacaranda).
Attention is the main thing (...) we have to be very careful with her! We care about every detail of her day to day, at home (Lent).
I watch him a lot (...) when he is sleeping and awake, I watch him a lot (Jatobá).
I stay vigilant, watching him in and out of the house. I can’t and I don’t even go out to work because I have to be looking at him (Pitangueira).
Category 2: Parental care
Parental care is characterized by actions and concerns of the family member in maintaining the daily life of their loved one with a mental health disorder, with the development of care measures such as hygiene, food, help with daily activities and medication administration.
I wake up the day (...) I’ll take care of (making) a vitamin or porridge, give her medication, (...) when she gets up, I watch her doing her hygiene (Araucaria).
It’s taking them to the doctor because they don’t go alone. Look for services that include both, right? The maintenance of the house is obviously up to me and that’s more it (Carvalho).
The care I have with him is, at the right time I give him the medicine, at breakfast time (...) when he takes the medicine, I always take his coffee in bed (Oranjeira).
It’s like this, he wakes up, I’m going to put his coffee on, I’m with him all the time because I can’t work, there’s no one to help me stay with him to give him the medication. He takes the wrong medication, if I leave it at home and then, I take care of him all the time (Pitangueira).
Category 3: Overprotective care
In this type of care, the family member tries to protect their loved one against all possible risks, based on the assumption that the person with a mental health disorder does not know how to defend himself, or that if they don’t have overprotection, they may have another crisis. It was expressed as a fear of a difficult imminent crisis, and the cause of extensive suffering for the family member. With over protection the family member assumes a maternal/paternalistic role.
I take care of him with the greatest love in the world, for me, I don’t want to let him get hurt, anything happens to him. I worry about him going out alone, after he got this disability, when I need to be away, leave him (...) my mind keeps thinking about him. I’m afraid he’ll freak out like it was the first time. (...) Afraid to let the gate open for a slip and he would leave (Ingá).
I always try to do something specific that she likes to be able to eat (...) the very strong medication she takes, and she needs to have a diet that helps, a diet that does not make her obese, a diet that will keep her little body elegant (Araucaria).
After dealing with this disease, his hands turn white from washing so much. I put a bottle of liquid soap and it ends right away because it’s a hand wash. And I look like that, but I don’t say anything, so I don’t abuse him (Sapucaia).
Category 4: Permissive care
It presents characteristics of care based on initiatives that completely fulfil the wishes of the person with a mental health disorder, in order to avoid confrontations. With an attitude that always pleases the person without antagonizing them.
I do things the way she likes, everything the way she likes (Araucaria).
I direct her towards something, and she directs her towards another, and I end up giving in so as not to further complicate her problem (...) she (says) “my husband, I want to go see (so-and-so)”. Then I provide (meet her request); “husband I’m not well, I want to go see the doctor”. Then I arrange (take her to the doctor) (Ipê).
Sometimes we let him (leave the house) and then when he says something like, “I want to go out”, we have to let him out and we follow him (...) (Jatobá).
Discussion
The evolution of care has played an elemental role in the preservation of the human species and the act of caring has always been present in everyday practices. Regarding health-related issues, the act of caring first emerged in the family environment, exercised mainly by the women of the family and later, in modern society, caring gained in the public space, has become an occupation. Regardless of the scope in which it is exercised, the act of caring demands accountability, concern, and emotional involvement with the recipient of the care given. 4
Regarding people with mental health disorders, care is generally exercised by the family and, often, family ties are the most important or the only means of social support experienced by these people. Knowing who these family members are and how they take care of their loved ones, allows us to identify and reflect on how they provide care and what the difficulties or support needs are for the health team, in order to perceive how they can facilitate or hinder the process of deinstitutionalization. 3
Considering the profile of the participants in this study and recognizing gender issues are familiar in care scenarios, where the woman plays the role of caregiver. This is a common profile in similar studies. Research carried out in Colombia aimed to point out the overload of caregivers of people with mental health disorders. 2) Another study carried out in Portugal3 deals with the challenges of deinstitutionalization and the trajectories of people with severe mental health disorders and their families. As well as a survey carried out in a state in the North of Brazil on mental health disorders and family care 4 and, finally, an investigation into the overload of informal care in Hungary, Poland and Slovenia with an emphasis on the health of caregivers, in which more than half of the respondents, in the three countries, were women. 7
It is clear that women have assumed the responsibility for the family care of people with mental health disorders in different social and cultural contexts.
Thus, it is important to discuss how care for family members is related to this gender issue, a situation that was imposed on women as those destined to take care of the home and family, regardless of whether it is in a context of illness or not, in addition to the resistance of the men to occupy this situation. 2 Concentrating and personifying care for people with mental health disorders on women can have consequences for their female carers physical and emotional health, compromising their quality of life. 14
Continuing the profile of family caregivers who participated in the study, it was observed a majority representation who self-declared as black. This data is a cross-section of the Brazilian sociodemographic profile, since the population that access the public health service, (which includes the CAPS), and consists of people with a low income or who are socially vulnerable. This is a result of colonization, and Brazil developed and implemented discrimination throughout history towards its black population. 15
Most of the interviewees claim to receive support from other family members, which does not concur with other studies, such as an investigation carried out in Portugal, 4) where care was provided only by the family of origin or marital family. Another study carried out in the southern region of Brazil 16 observed that care was performed by a single caregiver, usually female.
When adopting the presentation regarding the typology of care, it is worth noting that the four emergent categories are didactically represented separately, but are not dissociated, on the contrary, this care is interconnected in the daily experiences of each family caregiver.
The interactions of each carer for the family member with a mental health disorder is based on their sociocultural territory with the family member. 9 As a scenario for surveillance care it is based on fear that harm can be caused to the carer or another person; by parental age that reinforces the bond and concern of the family with their loved one ; by overprotectiveness linked to the idea that the family member is omnipotent in protecting their loved one, and by the permissiveness as a way of not contradicting the person and thus avoiding the emergence of new crises.
Surveillance care arises with the concept that a family member with a mental health disorder cannot produce, and thus destabilizes the capitalist order of rationality and productivity. 3 In this logic, they must be kept under surveillance and control and the family needs to pay them constant attention to guarantee the protection of their loved one or prevent them from exhibiting inappropriate behavior. Some family members discussed the use of strategies that seek to keep the person with a mental health disorder entertained as a means of guaranteeing control and is based on a belief that it is necessary to keep the mind “occupied”. Excessive control over the behaviors of people with mental health disorders is very common in an attempt to protect them, which ends up compromising their autonomy in addition to producing overload for the family caregiver. 17
Many family members, according to the registration units, demonstrate attitudes that aim to predict inappropriate behavior of the person with a mental health disorder in social environments, this acting by “anticipation” prevents the person’s social activity., This practice not positive because it restricts the freedom of the sick person and therefore, the family caregiver, who no longer goes to places that were previously part of their routines.1
It is important to emphasize that this caring method is a remnant of the asylum rationale, where the purpose of hospitalization was to avoid disturbance and maintain social order.1,3) It then make it important to discuss with family members the possible effects of this type of care. It is interesting that this type of care was the most mentioned by the three male caregivers, two of whom were husbands of the sick wives, and may indicate that there is greater social control from men over the behaviors presented by women.
Research 18 on the experiences husbands who are the family caregivers to their wives with mental health disorders shows different ideas regarding care. Some see their role as the wife’s caregiver is a task to be exercised, while others see the act of caring for the wife as a negative experience, causing hopelessness, illness, suffering and frustration, with the desire for the wife to be hospitalized as a form of relief for the husband.
Parental care is usually carried out by the family of origin, especially the mother and/or father, and based on material, social, financial, and emotional support, provide a family member with a mental health disorder with helpful resources. It is important to highlight that the provision of these resources can have a double impact, since it can strengthen autonomy, as well as increase these people’s dependence on family relationships, thus reducing their independence. 3
Another important point that needs to be discussed in relation to this care is the constant search by family members for resources associated with medicalization as a main care strategy, such as the excessive or inappropriate use of medication in order to contain a possible crisis. This can form a protective care for those with mental health disorders in the family, and may be associated with restrictive practices, bringing this care method closer to surveillance care. 16
In this study all caregivers of the three people who had a diagnosis of depression refer to parental care as the main way of caring for their sick loved one, reporting concerns medication times, hygiene care and eating. This demonstrating less concern in monitoring and/or controlling the behavior of their loved ones. In comparison to the discourse of relatives of those diagnosed with schizophrenia, who perceived their relative as aggressive and requiring continuous attention. This attitude can make us reflect on the stigmatization of psychotic subjects.
Parental care was also the most cited by those who do not have a support network to care for the person with a mental health disorder, which may be associated with the centralization of basic care to a single family member responsible for the sick person.
It was observed that overprotective care appeared as part of the daily lives of caregivers who are mothers, with the aim of protecting their children from any type of situation that could put them at risk but could compromise their freedom and prevent the autonomy of the person who suffers psychically. Research shows that some family members believe that those who suffer psychologically are incapable of dealing with social life, being more exposed to risks, 4 which possibly explains the attitudes of these mothers participating in the study.
Another problem related to overprotective care involves family caregivers doing lots of tasks for the person to prevent then going through difficult situations or exacerbating their suffering. A study 17 that sought to evaluate the way in which the family member deals with their loved one with a mental health disorder shows that the act of overprotecting the subject can invalidate the person’s desires, and intensity the stigmatization of dependence. This can hinder their social interaction and bring unwanted implications for the family caregiver.
Permissive care was shown in this study to be performed mainly by family members of people diagnosed with schizophrenia, in association with surveillance and parental care. These family members also reported not having any support to care for their loved ones, which may lead us to think that family members resort to this type of care when other possibilities do not have the expected effects.
A study 19 points out that some families which use strategies such as tolerance, understanding and patience, start with the assumption that the person with a mental health disorder does not have a psycho-emotional balance. In addition, these caregivers also try to avoid confrontation, preferring negotiation, emphasizing the importance of dialogue. However, when negotiation becomes difficult, it is common for the family member to comply with the subject’s wishes, giving in to what is requested to avoid the recurrence of crises, thus characterizing permissive care, also identifiable as tolerant care.
Thus, it is perceived that the different ways of caring have their relevance, depending on the context experienced by the family. Surveillance care can guarantee the safety of a person in crisis, parental care, as already described, materially and symbolically instrumentalizes the person with a mental health disorder, overprotection care may be necessary in more complex situations, or may be perceived as an affectionate mode of attention, and permissive care can be an alternative for the family member to maintain a good relationship with their sick loved one. That said, it is inferred that there is no single model and/or ideal of care, but rather, there are possible arrangements within the life trajectories and daily routine of each family, so that each type of care has importance from the context experienced at a given moment and in the face of circumstances that arise in the daily lives of the caregivers.
Final considerations
From the results obtained, it is clear that families take care of the family member with a mental health disorder in the way they can or manage from the social and emotional resources they have, often, due to stigmas, prejudices or lack of understanding about mental illness, the way of caring can be an obstacle to the main objective of psychosocial care, which is the inclusion of the person with a mental health disorder in the community, the reconstruction of affective bonds, and their autonomy. However, it is recognized that the forms of care are relevant within the system of each family’s arrangements.
It was noticed, during data collection, that the family members felt comfortable in carrying out the interviews, which may suggest that a listening space is important for the discussion of the difficulties and feelings related to the role of caring. In this sense, mental health teams, community spaces (neighborhood associations, churches, health centers, assistance services, among others) and public policies can support caregivers, so that there is an improvement in the quality of life for these family members and people who suffer psychologically.
Other important data were collected in this study, such as the care role placed on women, and the predominance of the black race, which makes us reflect on gender and race inequalities among caregivers of people with mental health disorders in the Brazilian structure.
Thus, the importance of carrying out other studies in the area that favor understanding about the mental health disorder and the repercussions on family caregivers is highlighted.
Some limitations in the development of the study deserve to be considered, such as the scenario of the SARS-CoV-2 pandemic, which somewhat hindered closer contact with the participants. In addition to the pandemic scenario, another possible limitation may center on the fact that the research was carried out in a single Psychosocial Care Centre, thus not allowing the comparison of results with the perception of users of other mental health devices within the municipality or of other cities and/or states of the federation.
REFERENCES
1.Yasui, S, Luzio, CA, Amarante, P. Atenção psicossocial e atenção básica: a vida como ela é no território. Revista Polis e Psique. 2018 (citado 2022 Out 13);8(1):173-190. doi: 10.22456/2238-152X.80426. [ Links ]
2.Salazar-Torres, LJ, Castro-Alzate, ES, Dávila-Vásquez, PX. Caregiver burden in families of people with mental illness linked to the day hospital programme of a tertiary institution in the city of Cali (Colombia). Revista Colombiana de Psiquiatría. 2019 (citado 2022 Abr 6);48(2):88-95. doi: 10.1016/j.rcp.2017.08.002. [ Links ]
3.Hespanha, P, Portugal, S, Nogueira, C, Pereira, JM, Hespanha, MJ. Doença mental, instituições e famílias: os desafios da desinstitucionalização em Portugal. Coimbra: Edições Almedina-CES: políticas, sociais; 2012. [ Links ]
4.Rosa, LCS, Silva, SLC. Família(s) e (Des)Institucionalização na Saúde Mental: Contexto e Perspectivas. Rev. FSA. 2020 (citado 2022 Nov 10);17(11):348-371. doi: 10.12819/2020.17.11.18. [ Links ]
5.Almeida, MHS, Mendonça, ES. Um olhar à família: ressonâncias psicossociais em familiares que convivem com uma pessoa em situação de transtorno mental. Revista Barbarói. 2017 (citado 2022 Jun 4);(49):01-24. doi: 10.17058/barbaroi.v0i49.6617. [ Links ]
6.Sampaio, ML, Bispo, JP. Rede de Atenção Psicossocial: avaliação da estrutura e do processo de articulação do cuidado em saúde mental. Cad. Saúde Pública. 2021 (citado 2023 Mar 11);37(3):e00042620. doi: 10.1590/0102-311X00042620. [ Links ]
7.Nascimento, LA, Leão, A. Estigma social e estigma internalizado: a voz das pessoas com transtorno mental e os enfrentamentos necessários. Hist Cienc Saude, Manguinhos. 2019 (citado 2022 Abr 30);26(1):103-121. doi: 10.1590/S0104-59702019000100007. [ Links ]
8.Bajil, P, Coligcki, D, Prevolnik-Rupel, V, Brouwer, WBF, Zrubka, Z, Gulácsi, L, et al. The burden of informal caregiving in Hungary, Poland and Slovenia: results from national representative surveys. Eur J Health Econ. 2019 (citado 2022 Mai 2);20(1):05-16. doi: 10.1007/s10198-019-01058-x. [ Links ]
9.Kantorski, LP, Cardano, M, Borges, LR, Machado, RA. The daily practices as key in mental health intervention. Esc Anna Nery. 2021 (citado 2023 Mar 11);25(1):e20190373. doi: 10.1590/2177-9465-EAN-2019-0373. [ Links ]
10.Brito, PMC, Alves, MB, Oliveira, VM, Nóbrega, MPSS, Baptista, SCO, Silva, RS. Users of alcohol and other drugs in the psychosocial care network: nursing care. Enfermería (Montevideo). 2021 (citado 2023 Mar 11);10(2):175-190. doi: 10.22235/ech.v10i2.2546. [ Links ]
11.Minayo, MCS, Costa, AP. Fundamentos Teóricos das Técnicas de Investigação Qualitativa. Revista Lusófona de Educação. 2018 (citado 2022 Nov 20);40:11-20. doi: 10.24140/issn.1645-7250.rle40.01. [ Links ]
12.Souza, VR, Marziale, MH, Silva, GT, Nascimento, PL. Translation and validation into Brazilian Portuguese and assessment of the COREQ checklist. Acta Paul Enferm. 2021(citado 2022 Fev 2);34:eAPE02631. doi: 10.37689/acta-ape/2021AO02631. [ Links ]
13.Bardin, L.Análise de Conteúdo. São Paulo: Edições 70; 2016. [ Links ]
14.Magalhães, JJ, Lopes, RE, Nóbrega-Therrien, SM, Vasconcelos, SB. Caregiver Women’s Coping Strategies Toward Schizophrenia Bearing People. J. res. fundam. care. 2018 (citado 2022 Nov 20);10(3):793-800. doi: 10.9789/2175-5361.2018.v10i3.793-800. [ Links ]
15.Instituto Brasileiro de Geografia e Estatística. Desigualdades Sociais por Cor ou Raça no Brasil. Estudos e Pesquisas: Informação Demográfica e Socioeconômica. 2019(citado 2022 Fev 28);41:1-12. Disponível em: Disponível em: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101681_informativo.pdf . [ Links ]
16.Kantorski, LP, Jardim, VMR, Treichel, CAS, Andrade, APM, Silva, MSSJ, Coimbra, VCC. Gênero como marcador das relações de cuidado informal em saúde mental. Cad. saúde colet. 2019(citado 2022 Ago 1);27(1):60-66. doi: 10.1590/1414-462X201900010071. [ Links ]
17.Ramos, AC, Calais, SL, Zotesso, MC. Convivência do familiar cuidador junto à pessoa com transtorno mental. Contextos clínicos. 2019 (citado 2022 Ago 10);12(1):282-302. doi: 10.4013/ctc.2019.121.12. [ Links ]
18.Batista, EC. Experiências vividas pelo cônjuge cuidador da esposa em tratamento psiquiátrico. Fractal, Rev Psicol. 2020 (citado 2023 Mar 11);32(1):31-9. doi: 10.22409/1984-0292/v32i1/5646. [ Links ]
19.Reis, TL, Dahl, CM, Barbosa, SM, Teixeira, MR, Delgado, PGG. Burden and participation of family in the care of Psychosocial Care Centers users. Saúde em Debate. 2016 (citado 2022 Nov 20);40(109):70-85. doi: 10.1590/0103-1104201610906. [ Links ]
How to cite: Lisboa LNT, Silva RS. Types of care for people with mental health disorder from the perspective of family members. Enfermería: Cuidados Humanizados. 2023;12(1):e3018. doi: 10.22235/ech.v12i1.3018
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. L. N. T. L. has contributed in a, b, c, d; R. S. D. S. in a, c, d, e.
Received: August 21, 2022; Accepted: March 29, 2023











 text in
text in