Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Enfermería: Cuidados Humanizados
versión impresa ISSN 1688-8375versión On-line ISSN 2393-6606
Enfermería (Montevideo) vol.11 no.2 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22235/ech.v11i2.2798
Original articles
Descriptive Study of Obstetric and Neonatal Outcomes in Two Models of Delivery Assistance in Primiparous Women
1 Universidad de Murcia, España, mb.conesaferrer@um.es
2 Hospital de Huércal Overa, España
3 Hospital Universitario de Torrevieja, España
4 Hospital Universitario de Torrevieja, España
5 Hospital General Universitario Reina Sofía de Murcia, España
Introduction:
In the 20th century, childbirth went from being attended at home to the hospital setting. Inappropriate and unnecessary interventions were uncritically adopted, leading to a dehumanization of childbirth. This is the model that currently exists in most Spanish hospitals, which has been questioned by the World Health Organization as early as 1996.
Objective:
The aim is to describe the differences in obstetrical and neonatal results across two different models of maternity care (biomedical model and humanised birth).
Method:
A correlational descriptive and multicenter study was carried out. A convenience sample of 205 primiparous women, 110 biomedical model and 95 humanised model, were recruited. Obstetrical and neonatal results were compared in two hospitals with different models of maternity care in Spain.
Results:
The humanised model of maternity care produces better obstetrical outcomes (spontaneous beginning of labour, normal vaginal birth, intact perineum and I degree tear and less episiotomies) than the biomedical model. There were no differences in neonatal outcomes.
Conclusion:
The benefits of implementing a humanised model of delivery care should be considered by health policy makers and reflected in the woman and her baby.
Keywords: humanising delivery; perinatal care; midwife; pregnancy outcome
Introducción:
En el siglo XX el parto pasó de ser atendido en casa al ámbito hospitalario. Se adoptaron de forma acrítica intervenciones inapropiadas e innecesarias que condujeron a una deshumanización del parto. Este es el modelo que existe actualmente en la mayoría de los hospitales españoles y que fue cuestionado por la OMS ya en 1996.
Objetivo:
Describir las diferencias que existen en los resultados obstétricos y neonatales en primíparas en dos modelos distintos de asistencia al parto (biomédico y humanizado).
Método:
Se llevó a cabo un estudio descriptivo, de corte transversal. Se obtuvo una muestra por conveniencia de 205 primíparas, 110 del modelo biomédico y 95 del humanizado. Se compararon los resultados obstétricos y neonatales en dos hospitales con modelos diferentes de asistencia al parto en España.
Resultados:
En el modelo humanizado de asistencia al parto se obtuvieron unos mejores resultados obstétricos (inicio espontáneo, parto eutócico, periné íntegro o desgarro de I grado y menos episiotomías) que en el biomédico. No hubo diferencias en los resultados neonatales.
Conclusión:
Los beneficios de instaurar un modelo humanizado de asistencia al parto deberían ser considerados por los responsables de políticas sanitarias y reflejados en la mujer y su criatura.
Palabras claves: parto humanizado; atención perinatal; matrona; resultado del embarazo
Introdução:
No século XX, o parto deixou de ser realizado em casa para ser realizado no ambiente hospitalar. Intervenções inadequadas e desnecessárias foram adotadas acriticamente, levando a uma desumanização do parto. Este é o modelo que existe atualmente na maioria dos hospitais espanhóis e que foi questionado pela Organização Mundial da Saúde já em 1996.
Objetivo:
O objetivo principal desse estudo é descrever as diferenças existentes nos resultados obstétricos e neonatais em primíparas em dois modelos distintos de assistência ao parto (biomédico e humanizado).
Método:
Foi realizado um estudo descritivo, transversal. Obteve-se uma amostra por conveniência de 205 primíparas, 110 do modelo biomédico e 95 do modelo humanizado. Os resultados obstétricos e neonatais foram comparados em dois hospitais com diferentes modelos de assistência ao parto na Espanha.
Resultados:
No modelo humanizado de assistência ao parto obtiveram-se melhores resultados obstétricos (início espontâneo, parto eutócico, períneo íntegro ou laceração grau I e menos episiotomias) do que no modelo biomédico. Não houve diferença nos resultados neonatais.
Conclusão: Os benefícios da implementação de um modelo humanizado de assistência ao parto devem ser considerados pelos formuladores de políticas de saúde e refletidos na mulher e em seu bebê.
Palavras-chave: parto humanizado; assistência perinatal; matrona; resultado da gravidez
Introduction
The rapid technological expansion that emerged in the mid-20th century influenced childbirth care, applying this technology to obstetrics. Childbirth went from being attended at home to being assisted in the hospital setting. With the intention of improving childbirth assistance, inappropriate and unnecessary interventions were uncritically adopted and, often, risky, without verifying their effectiveness and safety. 1-3 This model of childbirth care in the hospital environment in which the medical and interventionist part predominates is the biomedical model, which currently predominates in most Spanish hospitals.
Faced with this situation, the World Health Organization (WHO) draws up some recommendations in which a new model of childbirth care appear, the humanised model. At the International Conference on Humanisation in Brazil (2000), the concept of humanisation was defined, and it was emphasized that it could be applied to childbirth, evidencing the humanisation of childbirth as an urgent need.4 Humanised childbirth means putting the woman at the center of the process, promoting her control and her active participation.5 Humanising childbirth also means considering the beliefs, values and feelings of the woman and respecting her autonomy and dignity during the birth process.6-8) In addition, this new delivery care paradigm aims to reduce the use of technological interventions in normal childbirth because it is considered a physiological process and not a potentially pathological one. 6,9
In 2006, the Society of Gynecology and Obstetrics drafted a document recommending the selective use of episiotomy and not performing pubic shaving, these practices were performed systematically in all deliveries.10 The Federation of Midwifery Associations of Spain drafted a consensus document based on scientific evidence called "Initiative for Normal Childbirth". This was used as a guide for professionals who attend normal childbirth.11
The Spanish National Health System approved the Normal Childbirth Care Strategy in all the Autonomous Communities. This document presents a vision of childbirth as a physiological process. It highlights the importance of performing holistic care that integrates biological, emotional, and family aspects based on scientific evidence and respecting the active role of women. 12 In 2010, the Spanish Ministry of Health and Social Policy developed a Clinical Practice Guideline on Normal Childbirth Care. It stated that there should be a valid reason to intervene in normal childbirth, which is considered a natural process. 13
We are currently witnessing the birth of a new paradigm in childbirth assistance demanded, on the one hand, by health professionals, by women and their families; and, on the other, by the health systems of the different countries of the world. People want to be treated, not only in their biological facet, but in an integral way, as biopsychosocial beings, for this reason the biomedical model of childbirth care is being questioned by the users of health services. 14) Medicine based on scientific evidence is showing that the current model does not obtain the expected perinatal results, on the other hand, a humanised model could improve them and, most importantly, can achieve greater satisfaction for the woman and the family because it places them as the center of this birth process, which is one of the most important moments of her life.15,16
The objective of this study is to identify the differences that exist in the obstetric and neonatal results in primiparous women in two different models of delivery assistance (biomedical and humanised). The hypothesis that is proposed is that the humanised model of normal childbirth care presents better obstetric results than the biomedical model with similar neonatal results.
Method
Study design
A descriptive cross-sectional study was carried out in which the differences that exist in the obstetric and neonatal results in primiparous women in two different models of delivery assistance (biomedical and humanised) are exposed.
Scenery
The study was conducted between April 2013 and October 2013 in two hospitals in southeastern Spain, one located in Murcia and the other in Alicante.
Description of the hospitals in the study
Hospital A is a public hospital with private management that covers the Department 22 of Health of the Valencian Health Agency. In 2013 there were a total of 1189 births. The physical environment consists of 5 individual dilation rooms, used both for the dilation process, expulsive and immediate puerperium (first 2 hours), 2 delivery rooms and an operating room. In hospital A, the humanised model is used.
Hospital B is a public hospital that covers Area I of the Murcian Health Service. In 2013 there were a total of 7288 births. The physical environment consists of 4 double dilation rooms, which are used for the dilation process, and an individual one, which is not located next to the rest and is used for preparation of women with scheduled cesarean section or in situations where the woman should be alone, such as in case of miscarriage or fetal death. There is also an epidural room, 3 delivery rooms and a recovery service for mothers, where they stay for two hours after delivery. In hospital B, the biomedical model is performed.
Description of delivery care models
Humanised model: In this model, low-risk midwife-led childbirth assistance is provided in accordance with the recommendations of the Ministry of Health and Social Policy. No routine interventions are performed during childbirth, if the birth remains within the limits of normality. In normal childbirth care, women are given the possibility of freedom of movement, both in the process of dilation and expulsion, and the presence of a companion of their choice is allowed throughout the process. Alternative pain relief methods are applied (postural, massage, local heat, hydrotherapy, sterile water injection, Entonox), feeding is allowed during labor, and skin-to-skin contact between mother and newborn is provided in all births, including those performed by cesarean section. The newborn is not separated from its mother until two hours postpartum, after which it is weighed, and ocular prophylaxis and vitamin K are administered; it is dressed when it goes up to the maternity ward. Early breastfeeding is promoted.
Biomedical model: In this model there is low-risk delivery care with a high level of intervention. It is a shared care model (professional midwives and gynecologists). The presence of a companion of the woman's choice is allowed throughout the entire process, except in the mothers' recovery room, which is common to all postpartum women. Expulsion is performed in the delivery room, after which the newborn is placed on top of its mother to establish the first contact with its parents. The newborn is then picked up for weighing and dressing in the delivery room. Ocular prophylaxis and vitamin K are administered on the maternity ward. Early initiation of breastfeeding is encouraged.
Population
The reference population was women who gave birth in these hospitals. In hospital A there were a total of 1189 births and in hospital B a total of 7288 births in the year 2013.
The inclusion criteria were women who were in the process of giving birth, primiparous women who understood Spanish or English to be able to complete the questionnaire on sociodemographic data and sign the informed consent.
The exclusion criteria were women admitted for scheduled cesarean section.
A convenience sampling was performed with a sample size adjusted for the test of equality of two proportions for a significance level of 5% and a power of 80 % that would detect a difference of 15 % between both proportions with a sample size of 188. Allowing for a loss of 10 %, a further 10 % was selected.
Data collection technique
After delivery, information on delivery data was collected from the computerized medical record. The sociodemographic data were collected in the questionnaire that the women filled out during their postpartum stay in the hospital.
The document Perinatal care in Spain: Analysis of physical and human resources, activity and quality of hospital services, 2010-2018 was taken as a reference, in which better results of childbirth care are described, obtaining higher rates of normal deliveries, normal deliveries after cesarean sections, and lower rates of amniotomies, Kristeller maneuver, cesarean sections, instrumented deliveries, with vacuum, forceps or spatulas, inductions, episiotomies and normal deliveries with the use of oxytocin during the same.
Ethical aspects
The study was approved by the Ethics and Research Committees of both centers. The ethical principles of the Declaration of Helsinki regarding research involving human beings were respected. The women were informed that their participation was voluntary and that the information they provided would be confidential. The women who agreed to participate in the study previously signed an informed consent. Women under 18 years of age were asked for informed consent signed by them and their legal guardian.
Data análisis
The statistical program SPSS version 25.0 for Windows was used to analyze the data obtained. First, descriptive statistics were performed using frequency tables to expose the sociodemographic data, obstetric and neonatal results of the sample. Then, a comparison of the study variables between the two delivery care models was made through contingency tables using Pearson's Chi-square test to analyze whether there were statistically significant differences between the qualitative variables of the study. In addition, the observed frequency, the expected frequency, and the corrected residuals were obtained. Statistically significant differences between the two care models were considered to exist when p<0.05, corrected residuals > or equal to 2, and expected frequency > 5. A logistic regression analysis was performed to assess possible confounding variables.
Results
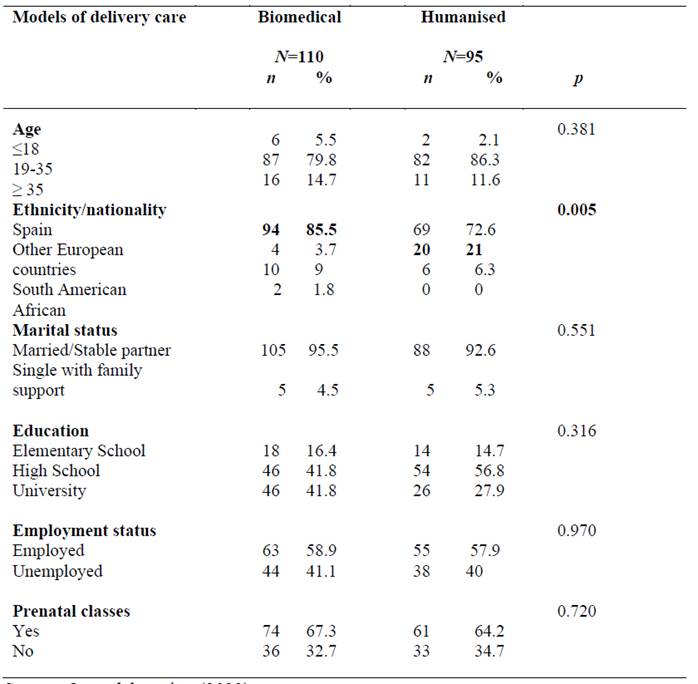
A total of 205 primiparous women participated in the study, of which 110 gave birth in Hospital B and 95 in Hospital A. The sociodemographic characteristics are compared in Table 1. Differences between both groups are only observed in the country of origin of the participants. In the humanised model, more women from the rest of Europe were found, and in the biomedical model, more Spanish women were found. After the logistic regression analysis, the same statistically significant differences were observed between both models, including the ethnicity variable.
As can be seen in Table 1, some sociodemographic data have been lost because the participants did not complete them in the questionnaire: missing data on age (1 in the biomedical model), marital status (2 in the humanised model), in educational level (1 in the humanised model), employment status (3 in the biomedical model and 2 in the humanised model), in attendance at childbirth preparation classes (1 in the humanised model).
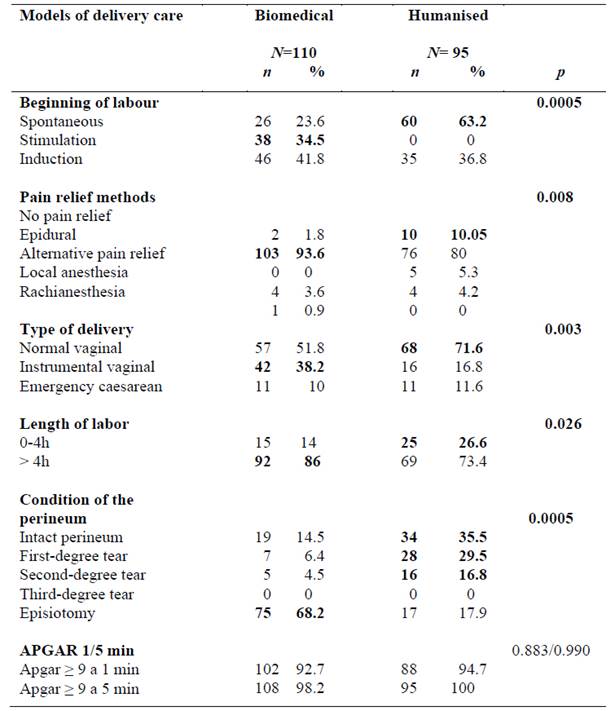
The delivery data of the sample are compared in Table 2. Those factors in which there is a statistically significant difference appear in bold. In hospital B 76.3 % of deliveries start with induction or stimulation, however, in hospital A 63.2 % of them start spontaneously.
Regarding pain relief methods, in hospital A women may choose to use other alternative methods. Regarding the type of delivery, we observed that in hospital A, 71.6 % of the women had a normal delivery, with a greater number of instrumental deliveries in hospital B.
Although more stimulations are performed in hospital B, the duration of labor is not shorter, but in hospital A there is a greater proportion of women whose labor lasts less than 4 hours.
Regarding the state of the perineum, it is observed that there is a higher proportion of episiotomies (68.2 %) in hospital B, while in hospital A, 65% of the women present a complete perineum or I-grade tear.
Table 2 shows that some data are missing because they have not been entered in the computerized clinical history: in the duration of labor (1 is missing from the humanised model and 3 from the biomedical model), in the state of the perineum (4 are missing from the biomedical), in the Apgar test at one minute (8 missing in the biomedical model and 7 in the humanised model) and in the Apgar test at 5 minutes (2 missing in the biomedical model).
Discussion
In the comparison of childbirth data, the difference that exists between both models of childbirth assistance is observed, one being a biomedical model where medicalization predominates and the other a humanised model where childbirth is considered a physiological process, and it is not performed no intervention if it is a normal delivery. 11,13
In the present study, it is observed that in the humanised model a greater number of pregnant women initiate labor spontaneously in contrast to the biomedical model in which the greater proportion of pregnant women initiate it with stimulation. Routine artificial amniorrhexis, accompanied or not using oxytocin, is a common procedure in normal delivery care in Spain. However, in the Clinical Practice Guideline on Assistance for Normal Childbirth of the Spanish Ministry of Health and Social Policy, its routine use is not recommended because it has not been observed that it improves the results in vaginal deliveries that progress normally. In addition, there are questions about unintended effects on the mother and fetus. 13 The WHO does not recommend labor augmentation, amniorrhexis, and the use of oxytocin routinely as measures for normal progressing labor.3 Various studies have shown that in models led by midwives, they are less interventionist, observing less use of oxytocin.18-22 In addition, the present study shows that, despite the greater use of oxytocin for labor stimulation in the biomedical model, the duration of labor is longer than in the humanised model. A review study conducted in 2015 also showed no difference in the duration of labor between the midwife-assisted group and the obstetrician-assisted group. 22
Regarding the number of inductions, no statistically significant difference was observed. This is consistent with a study carried out in Brazil, in which midwife-led delivery assistance models were compared with other models. 23
Regarding the methods used for pain relief in labor, in this study in the humanised model various pharmacological and non-pharmacological means of pain relief were observed (freedom of movement, heat, immersion in water, injection of sterile water, etc.), while in the biomedical model pharmacological methods are used. The WHO, the Spanish Ministry of Health and Social Policy and the Spanish Federation of Midwives Associations recommend the use of alternative methods for pain relief in childbirth in addition to pharmacological methods.3,11,13The use of non-pharmacological methods for pain relief has been observed in models of midwife-led delivery assistance. 24
In the present study, in the humanised model, the woman is allowed to eat during the active period of labor if it is a normal delivery, this is also found in the literature in midwife-assisted deliveries. 24
In the results obtained according to the type of delivery, in our study it is observed that in the humanised model of childbirth care there is a greater number of eutocic deliveries than in the biomedical model where a greater number of instrumental deliveries is observed. Several systematic reviews of the literature comparing midwife-led models of delivery with obstetrician-led models also found that midwifery models produced fewer interventions, fewer operative deliveries, and more spontaneous deliveries. 17,23 In these reviews, no differences were observed in the number of caesarean sections between both groups, as was the case in our study. A retrospective cohort study and Cochrane review including 15 randomized clinical trials involving a total of 17,674 women found that there was a lower proportion of caesarean sections in the midwife-led model. 22,27
Regarding the state of the perineum after childbirth, there are important differences between the two models compared in this study. In the biomedical model there is a higher proportion of episiotomies than in the humanised model. The WHO recommends not performing more than 20 % of episiotomies, in the quality indicators of the Spanish National Health System the quality standard for episiotomies is 15 % and the Federation of Midwifery Associations of Spain advises not to exceed the 10 % of episiotomies in normal deliveries.11,25 As can be seen, the percentage of episiotomies is much higher than that recommended in the biomedical model, this is also observed in various studies, in midwife delivery care model fewer episiotomies are performed, even in one study a higher economic cost was associated due to the greater use of it in models of childbirth assistance directed by doctors. 23,24,27
Neonatal outcomes were compared using the Apgar test. In this study, no statistically significant differences were found between both delivery care models. In other studies, it was also concluded that delivery assistance models are just as safe as those led by obstetricians in terms of neonatal outcomes because no differences have been observed between them and they also increase women's satisfaction with their delivery process. 19,23,26,27
This study has some limitations, including the fact that the sample collected was small and by convenience. The use of a convenience sample is justified by the lower economic cost and the fact that it could have been carried out in a shorter period. Due to the sample size, the results obtained cannot be generalized. More similar studies would be needed to extrapolate and generalize the results.
Conclusion
Better obstetric results are obtained in the humanised model of delivery care than in the biomedical model (higher percentage of spontaneous labor onset, shorter labor duration, greater use of alternative methods of pain relief and less use of epidural analgesia, more eutocic deliveries, higher percentage of intact perineum and I degree tears and fewer episiotomies. The neonatal results in both models are optimal with no differences between them.
This is important for health professionals involved in childbirth care, especially for midwives, because they are the most appropriate professionals for normal childbirth care. Humanised childbirth care model tries to prevent the unnecessary use of medical interventions. Excellent obstetric results are obtained, and it conforms to current WHO recommendations, being equally safe for the mother and the newborn. It also encourages professionals to establish an empathic relationship with women, taking an interest in their expectations and needs.
For the administrators and managers of the health system, this study can be a reference model to implement in the hospital environment because it produces important benefits for the woman and her child, such as a high level of satisfaction.
Among the benefits that have been evidenced in the humanised models of childbirth assistance for the woman and her baby is that it is a model centered on the woman, the child and the family, who are offered information during labor assistance. This increases their perception of internal and external control, as well as facilitating their understanding of the care provided and enabling their participation in the decisive processes. In addition, the privacy and dignity of the patient and family are respected. Better obstetric outcomes (more euthyroid deliveries and fewer episiotomies) result in better postpartum recovery, less postpartum pain, greater ability to perform activities of daily living and a more satisfactory initiation of breastfeeding.
REFERENCES
1. Cerdán-Jiménez, MD, Carballo-Aliseda, MD, Gómez-Fernández, A, Heredia-Prim, F, Salgado-Poveda, I, Cayuela-Font, E. Proceso de humanización de la atención a las cesáreas: instauración de un procedimiento para acompañamiento de las gestantes e inicio de la lactancia materna en quirófano. Musas Revista de Investigación en Mujer, Salud y Sociedad (Internet). 2017 (citado 23 mar 2022);2(1):42-56. DOI: 10.1344/musas2017.vol2.num1.3 [ Links ]
2. Luces Lago, AM, Mosquera Pan, L, Freire Barja, N, Pena Fernández, D, Tizón Bouza, E. Humanización del parto: prácticas recomendadas en partos de bajo riesgo. Tiempos de enfermería y salud (Internet). 2019 (citado 23 mar 2022);2(7):36-41. Disponible en: Disponible en: https://tiemposdeenfermeriaysalud.es/journal/article/view/78 [ Links ]
3. Borges Damas, L, Sixto Pérez, A, Sánchez Machado, R. Influencia del desempeño de los profesionales de enfermería en la atención humanizada al parto. Revista Cubana de Enfermería (Internet). 2018 (citado 23 mar 2022);34(2). Disponible en: Disponible en: http://revenfermeria.sld.cu/index.php/enf/article/view/1426/357 [ Links ]
4. Macías Intriago, MG, Tacoamán Acurio, IJ, Giler Saltos, LA, Quimis Guerrido, WM, Choez Reyes, ML, Álvarez Lara, MM. Parto humanizado como estrategia de salud pública en atención primaria de salud. Revista Científica Mundo de la Investigación y el Conocimiento (Internet). 2018 (citado 23 mar 2022);2(3):730-45. DOI: 10.26820/recimundo/2.(3).septiembre.2018.730-745 [ Links ]
5. Jiménez Hernández, GE, Peña Jaramillo, YM. Adherencia a las recomendaciones de la OMS en la atención del parto y nacimiento humanizado. Medellín, Colombia. Rev Univ Ind Santander Salud (Internet). 2018 (citado 23 mar 2022);50(4):320-7. DOI: 10.18273/revsal.v50n4-2018005 [ Links ]
6. Franco Coffre, JA, Calderon Intriago, LG, Cujilan Alvarado, MC, Salazar Menéndez, JP. Conocimiento del Parto Humanizado en mujeres gestantes del Hospital de Yaguachi “Dr. José Cevallos Ruíz”. Revista Científica Mundo de la Investigación y el Conocimiento (Internet). 2018 (citado 23 mar 2022);2(1):716-36. DOI: 10.26820/recimundo/2.1.2018.716-736 [ Links ]
7. Lanero, S, Lanero, A. La humanización obstétrica desde la perspectiva de la mujer: percepción de apoyo y creencias sobre las prácticas de atención al parto. Matronas Prof. 2020;21(2):54-61. [ Links ]
8. Behruzi, R, Hatem, M, Goulet, L, Fraser, W. The facilitating factors and barriers encountered in the adoption of a humanized birth care approach in a highly specialized university affiliated hospital. BMC Women’s Health. 2011;11(1):53. DOI: 10.1186/1472-6874-11-53 [ Links ]
9. Martín-Castañeda, LB. “Lo más natural posible”: Narrativas de matrona de atención primaria y hospitalaria en el paradigma del parto humanizado. Musas Revista de Investigación en Mujer, Salud y Sociedad (Internet). 2021 (citado 23 mar 2022);6(1):38-58. DOI: 10.1344/musas2021.vol6.num1.3 [ Links ]
10. Biurrun Garrido, A. La humanización de la asistencia al parto: Valoración de la satisfacción, autonomía y del autocontrol (Tesis de doctorado). Barcelona: Universitat de Barcelona; 2017. Disponible en: http://diposit.ub.edu/dspace/handle/2445/118125 [ Links ]
11. Ministerio de Sanidad y Consumo. Estrategia de Atención al Parto Normal en el Sistema Nacional de Salud (Internet). 2008 (citado 2 ene 2022). Disponible en: Disponible en: http://www.060.es . [ Links ]
12. Grupo de Trabajo de la Guía de Práctica Clínica sobre la Atención al Parto Normal. Guía de Práctica Clínica sobre la Atención al Parto Normal (internet). País Vasco: Ministerio de Sanidad y Política Social; (citado 18 ene 2022). Disponible en: Disponible en: https://www.sanidad.gob.es/organizacion/sns/planCalidadSNS/pdf/equidad/guiaPracticaClinicaParto.pdf [ Links ]
13. McCourt, C. Technologies of birth and models of midwifery care. Rev Esc Enferm USP. 2014;48(Esp):168-77. [ Links ]
14. Cifre, RL. Humanización de la atención obstétrica: qué opinan las matronas. Matronas Prof. 2018;19(1):12-20. [ Links ]
15. Mayra da Silva Lira, I., Santos e Silva Melo, S., Teles de Oliveira Gouveia, M., Cipriano Feitosa, V., Maria Melo Guimarães, T. Intervenção educacional para melhoria na assistência ao trabalho de parto normal. Enfermería Global(Internet). 2020 (citado 23 mar 2022);19(2):226-56. Disponible en: Disponible en: https://revistas.um.es/eglobal/article/view/382581 [ Links ]
16. Souter, V, Nethery, E, Kopas, ML, Wurz, H, Sitcov, K, Caughey, AB. Comparison of Midwifery and Obstetric Care in Low-Risk Hospital Births. Obstet Gynecol. 2019 Nov;134(5):1056-1065. PMID: 31599830. DOI: 10.1097/AOG.0000000000003521. [ Links ]
17. Declercq, ER, Belanoff, C, Sakala, C. Intrapartum Care and Experiences of Women with Midwives Versus Obstetricians in the Listening to Mothers in California Survey. J Midwifery Womens Health. 2020 Jan;65(1):45-55. Epub 2019 Aug 26. PMID: 31448884; PMCID: PMC7028014. DOI: 10.1111/jmwh.13027. [ Links ]
18. Voon, ST, Lay, JTS, San, WTW, Shorey, S, Lin, SKS. Comparison of midwife-led care and obstetrician-led care on maternal and neonatal outcomes in Singapore: A retrospective cohort study. Midwifery. 2017 Oct;53:71-79. Epub 2017 Jul 18. PMID: 28778037. DOI: 10.1016/j.midw.2017.07.010. [ Links ]
19. Poškienė, I, Vanagas, G, Kirkilytė, A, Nadišauskienė, RJ. Comparison of vaginal birth outcomes in midwifery-led versus physician-led setting: A propensity score-matched analysis. Open Med (Wars). 2021 Oct 15;16(1):1537-1543. PMID: 34722889; PMCID: PMC8520123. DOI: 10.1515/med-2021-0373. [ Links ]
20. Raipuria, HD, Lovett, B, Lucas, L, Hughes, V. A Literature Review of Midwifery -Led Care in Reducing Labor and Birth Interventions. Nurs Womens Health. 2018 Oct;22(5):387-400. Epub 2018 Sep 6. DOI: 10.1016/j.nwh.2018.07.002. [ Links ]
21. Bartuseviciene, E, Kacerauskiene, J, Bartusevicius, A, Paulionyte, M, Nadisauskiene, RJ, Kliucinskas, M, et al. Comparison of midwife-led and obstetrician-led care in Lithuania: A retrospective cohort study. Midwifery . 2018 Oct;65:67-71. Epub 2018 Jun 21. DOI: 10.1016/j.midw.2018.06.017. [ Links ]
22. Sandall, J, Soltani, H, Gates, S, Shennan, A, Devane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews. 2016;(4):CD004667. DOI: 10.1002/14651858.CD004667.pub5. [ Links ]
23. Granado Nogueira da Gama, S, Fernandes Viellas, E, Alves Torres, J, Helena Bastos, M, Brüggemann, OM, Theme Filha MM et al. Labor and birth care by nurse with midwifery skills in Brazil. Reproductive Health. 2016;13(1):123. DOI 10.1186/s12978-016-0236-7. [ Links ]
24. Recio Alcaide, A. La atención al parto en España: Cifras para reflexionar sobre un problema. Dilemata (Internet). 2015;7(18):13-26. Disponible en: https://dialnet.unirioja.es/descarga/articulo/5106931.pdf [ Links ]
25. Neal, JL, Carlson, NS, Phillippi, JC, Tilden, EL, Smith, DC, Breman, RB, Dietrich, MS, Lowe, NK. Midwifery presence in United States medical centers and labor care and birth outcomes among low-risk nulliparous women: A Consortium on Safe Labor study. Birth. 2019 Sep;46(3):475-486. Epub 2018 Nov 11. PMID: 30417436; PMCID: PMC6511333. DOI: 10.1111/birt.12407. [ Links ]
26. Attanasio, LB, Alarid-Escudero, F, Kozhimannil, KB. Midwife-led care and obstetrician-led care for low-risk pregnancies: A cost comparison. Birth . 2020 Mar;47(1):57-66. Epub 2019 Nov 3. DOI: 10.1111/birt.12464. [ Links ]
27. Mattison, CA, Dion, ML, Lavis, JN, Hutton, EK, Wilson, MG. Midwifery and obstetrics: Factors influencing mothers' satisfaction with the birth experience. Birth . 2018 Sep;45(3):322-327. Epub 2018 Apr 24. DOI: 10.1111/birt.12352. [ Links ]
How to cite: Conesa Ferrer MB, Camacho Ávila M, Hernández Sánchez E, López Martínez EM, Marín Conesa E. Descriptive study of obstetric and neonatal outcomes in two models of delivery assistance in primiparous women. Enfermería: Cuidados Humanizados. 2022;11(2):e2798. DOI: 10.22235/ech.v11i2.2798
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. M. B. C. F. has contributed in a, b, c, d, e; M. C. A. in b, e; E. H. S. in d; E. M. L. M. in c; E. M. C. in a, b, e.
Received: January 26, 2022; Accepted: September 13, 2022











 texto en
texto en