Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Enfermería: Cuidados Humanizados
versión impresa ISSN 1688-8375versión On-line ISSN 2393-6606
Enfermería (Montevideo) vol.11 no.2 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22235/ech.v11i2.2820
Original Articles
Effect of a Virtual Educational Intervention to Promote Early Initiation of Breastfeeding in Pregnant Women from Lima, Peru
1Universidad Católica Sedes Sapientiae, Perú
2Universidad Católica Sedes Sapientiae, Perú
3Universidad Católica Sedes Sapientiae, Perú
4Universidad Católica Sedes Sapientiae, Perú
Objective:
The present research consisted of evaluating the effect of a virtual educational intervention to promote the early beginning of breastfeeding (ITLM, for its Spanish acronym) in pregnant women who are users of Los Libertadores health center, located in Lima (Peru), in 2021.
Materials and methods:
An analytical, longitudinal, and prospective study of the virtual educational intervention method was carried out on pregnant women in a health institution in Lima from January 26thto February 9th, 2021. The sample consisted of 40 pregnant women who live in Lima. For data collection, a questionnaire made up of 12 questions was applied, which was previously validated by five expert judges obtaining good reliability: Cronbach's Alpha was 0.90. In addition, the flipchart got a Cronbach's Alpha of 0.831.
Results:
There was an increase in knowledge after the educational intervention (p<0.05) and 83.33% of the pregnant women who belonged to the experimental group started breastfeeding early after the intervention (p<0.001).
Conclusion:
The virtual educational intervention shows a positive impact on the increase in knowledge of pregnant women from the early initiation of breastfeeding in the experimental group to when their children were born. So, it was recommended that this program should be promoted from the prenatal care stage.
Keywords: breast feeding; pregnant women; prenatal education
Objetivo:
El presente trabajo de investigación consistió en evaluar el efecto de una intervención educativa virtual para promover el inicio temprano de la lactancia materna (ITLM) en gestantes usuarias del centro de salud Los Libertadores, ubicado en la ciudad de Lima (Perú), en el año 2021.
Materiales y métodos:
Se realizó un estudio analítico, longitudinal y prospectivo de método intervención educativa virtual a gestantes de un establecimiento de salud de Lima en el período de 26 de enero a 9 de febrero de 2021. La muestra estuvo conformada por 40 gestantes residentes en Lima. Para la recolección de datos se empleó un cuestionario conformado por 12 preguntas, este fue previamente validado por cinco jueces expertos y con buena confiabilidad: el Alfa de Cronbach resultó 0.90. Asimismo, el rotafolio tuvo un Alfa de Cronbach de 0.831.
Resultados:
Hubo un aumento en los conocimientos tras la intervención educativa (p<0.05). Y el 83.33 % de las gestantes que pertenecieron al grupo experimental realizaron el inicio temprano de lactancia materna después de la intervención (p<0.001).
Conclusión: La intervención educativa virtual tuvo un impacto positivo en el aumento de conocimientos de las embarazadas sobre el inicio temprano de la lactancia materna en el grupo experimental, y cuando fueron madres realizaron el ITLM. Por ende, se recomienda que se debe promover esta temática desde la atención prenatal.
Palabras clave: lactancia materna; mujeres embarazadas; educación prenatal
Objetivo:
O objetivo desta pesquisa foi avaliar o efeito de uma intervenção educativa virtual para promover o início precoce da amamentação (sigla em espanhol ITLM) em gestantes usuárias do centro de saúde Los Libertadores, localizado na cidade de Lima (Peru), no ano de 2021.
Materiais e métodos:
Um estudo analítico, longitudinal e prospectivo foi realizado utilizando um método de intervenção educativa virtual para mulheres grávidas, em um centro de saúde em Lima, de 26 de janeiro a 9 de fevereiro de 2021. A amostra consistia de 40 mulheres grávidas vivendo em Lima. Um questionário de 12 perguntas foi utilizado para a coleta de dados, que foi previamente validado por cinco juízes especialistas e tinha boa confiabilidade: o alfa do Cronbach era de 0,90. Da mesma forma, o flipchart tinha um Alfa de Cronbach de 0,831.
Resultados:
Houve um aumento no conhecimento após a intervenção educacional (p<0,05) e 83,33% das mulheres grávidas, que pertenciam ao grupo experimental, tiveram um início precoce de amamentação após a intervenção (p<0,001).
Conclusão:
A intervenção educacional virtual teve um impacto positivo no aumento do conhecimento das mulheres grávidas sobre o início precoce da amamentação no grupo experimental e, quando se tornaram mães, realizaram o ITLM. Portanto, é recomendável que este tópico seja promovido a partir do pré-natal.
Palavras-chave: aleitamento materno; gestantes; educação pré-natal
Introduction
Early beginning of breastfeeding (ITLM, for its Spanish acronym) is defined as “breastfeeding newborns within the first hour of life”; and contributes to the survival of the newborn, because this first breastfeeding provides vital nutrients to make the immune system stronger. 1 This is confirmed by the study carried out by Smith et al., 2 whose neonates who had received human milk within an hour of life had more chances of surviving compared to those who breastfeed after the first hour. This means, a longer time without receiving human milk causes a higher risk of infection and neonatal mortality rates, possibly doubling.
Instant skin-to-skin contact is important to ease the early beginning of breastfeeding, helping to regulate the body temperature of newborns, 3-5 and also improves the emotional bond between mother and newborn.1 Regarding the benefits of early initiation of breastfeeding for the mother, it includes the low risk of postpartum depression 6 and the stimulation of the release of oxytocin that helps the uterus to contract and, consequently, reduces the risk of hemorrhage postpartum. 7 In addition, thanks to ITLM, the possibilities of maintaining exclusive breastfeeding are augmented. (8
Despite the benefits of ITLM, lack of awareness causes a lower percentage of mothers who breastfeed their newborns in the first hour of their baby’s life. According to the United Nations Children's Fund (UNICEF) in 2018, the ITLM percentage worldwide was 42 %, which means two out of every five newborns receive breast milk within the first hour of life, and in Latin America and the Caribbean it was 52 %. 1 In Peru, since 2013 through the Technical Standard NTS No. 106 - MINSA / DGSP (Ministry of Health / General Management of Health) it is indicated that it is a responsibility of health personnel and a right of the healthy newborn to have the promotion of ITLM during the first hour of life. 9 Despite this, the National Institute of Statistics and Informatics (INEI) through the Demographic and Family Health Survey (ENDES) 2020 showed that less than half of children around Perú began to breastfeed within the first hour of life after birth (47.8 %). 10 In addition, in a study carried out on mothers in a public hospital in Lima Norte, the ITLM percentage was only 37.5 %.11
The WHO and UNICEF mention that there is a worldwide need for the promotion and support of breastfeeding programs, including interventions that have an impact on the early beginning of breastfeeding.1 It is recognized that health care providers, especially nurses, are key to the implementation of ITLM and to provide information and support for mothers in positioning the baby for breastfeeding after delivery. (11, 12) However, one study showed that health care providers do not have suitable skills to help and support mothers to begin breastfeeding.7
In Peru, through MINSA, there is a Ministerial Resolution since 2013 stating that it is a duty of the health professional in charge of prenatal care to provide pregnant women with training on maternal care and breastfeeding. 9) A training flipchart has been created for health personnel called “Promotion and Support of Breastfeeding”, 13 consisting of many layers that specify how to promote, and explain the importance of, ITLM. However, it is not entirely clear what teaching materials this staff would use to provide an effective educational workshop on this topic, including the time spent, the method of educational intervention and the evaluation of learning, according to the needs of each pregnant woman.14
Considering the above, the promotion of ITLM is considered of great importance, not only for mothers during childbirth but also when they are pregnant, because through prenatal education of the practice of ITLM, they will develop knowledge and confidence in the process, and be ready for the first hour of life of their newborn. In Peru, there are not any studies that report on this subject in pregnant women and mothers, consequently, the objective was to evaluate the effect of a virtual educational intervention, adapted with virtual instruction in the context of COVID-19, to promote the early beginning of breastfeeding in pregnant women who are users of the Los Libertadores health center in Lima in 2021.
Methodology
An analytical, longitudinal and prospective study of the educational intervention method was applied in Los Libertadores Health Center, located in San Martín district in Lima - Peru during January and February in 2021. The population consisted of 93 pregnant women who carry out their prenatal check-ups at the health center. Pregnant women who were called to participate in the study had the option of participating or not, and those who wanted to participate were included. In this way, the effective sample was 40 pregnant users and was divided into two groups randomly, the first was the experimental group consisting of 20 pregnant women who received the educational intervention on the ITLM, while the second one was the control group consisting of 20 pregnant women who only received the brochure.
The dependent variable was knowledge about early beginning of breastfeeding. A questionnaire with 12 questions was used, each one with four options to mark, divided into four parts. The first part was Generalities about the ITLM, with four questions about the ITLM concepts, colostrum, its properties and the physiology of breastfeeding. The second part, called Benefits of ITLM to the infant, had three questions about the physiological and psychological benefits of ITLM and colostrum. The third part was about the Benefits of the ITLM to the mother and the newborn and included two questions about the physiological and psychological benefits that the ITLM provides to the mother and the second about the emotional connection that benefits to both. The last part was called Requirements that must be fulfilled to start breastfeeding Early, in this part it was highlighted that before starting breastfeeding early the baby must be in skin-to-skin contact with the mother, considered a healthy newborn and that no one should force this procedure. About validation, the instrument was submitted to the criteria of five expert judges, from this, in the Cronbach's Alpha coefficient test, 0.90 was obtained, and in Aiken's V coefficient, the result was 0.95, which ensures that the instrument is reliable and valid.
The independent variable was the educational intervention that was carried out through the management of a digital flipchart entitled “First Drop of Life” which contains 10 sheets with images and information found from organizations such as the United Nations Children's Fund (UNICEF) 15 and the Ministry of Health of Peru (MINSA).16 The content of the flipchart was synchronized with the 12-question questionnaire. Equally, tertiary variables were considered in which a data sheet was used in order to measure the sociodemographic characteristics (age, level of education, place of origin, type of family) and the prenatal characteristics of the pregnant women (gestational age, number of children, start of prenatal care, number of check-ups and training in early initiation of breastfeeding, the latter indicating whether the pregnant woman received any information about the ITLM before the study, either at the health center or in the community). The flipchart was evaluated by five judges, obtaining 0.83 of Cronbach's Alpha.
Concerning data collection, firstly, authorization was asked from Dirección de Redes Integradas de Salud Lima Norte (DIRIS) before going to the health center. Once the authorization was obtained, the personnel working in the health center were asked for the register of pregnant women throughout January and February 2021. The pregnant women were then contacted by telephone inviting them to the educational intervention, then the consent form was sent, along with the weblink with the data sheet and the form with the 12 questions to both groups. Then, the educational intervention was carried out with the support of a nurse and a nutritionist, starting with a friendly dynamic to create an environment of trust. The intervention was carried out via Zoom due to the pandemic situation (COVID-19), since the R.M. No. 146-2020-MINSA accepted the Administrative Directive for the implementation of Tele-orientation and Tele-monitoring Services,17 and the information provided on each part lasted only 10 minutes, the time necessary to record the needed information without burdening the pregnant women with too many questions. In addition, listeners were advised to turn their microphones off during the presentation to avoid interruptions, and in case of questions or comments, they were told to use the Zoom hand raise function. Finally, to avoid bias due to immediate response, the same questionnaire was sent after two weeks to measure knowledge about the ITLM to both groups, the group that received the full intervention and information (including the flipcharts and Zoom meetings), and to the other group that only received a brochure (which had the same information as the flipcharts without Zoom meetings). In relation to the ITLM realization variable, after a few months all the participants were called by telephone to verify if during the first hour of life they breastfed their baby (Yes/No).
The research study was accepted by the Health Research Ethics Committee of the Universidad Católica Sedes Sapientiae with the code CE-528.
In the analysis plan, the data was administered with the statistical package STATA version 12, in which a mean and a standard deviation were used for quantitative variables, while frequencies and percentages were used for qualitative variables. The T-Student test for related samples was used to verify the impact of the educational intervention.
Results
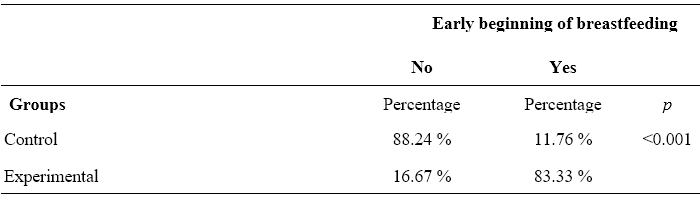
In Table 1, concerning the sociodemographic characteristics, the average age of the control group was 27.5 years, 50 % of the pregnant women had completed secondary education, 75 % were from urban origin and 75 % came from a nuclear family. Regarding the prenatal characteristics of the control group, the average number of controls was 2.3, 75 % of the pregnant women did not receive training on ITLM, 60 % were in the 2nd trimester of pregnancy, 50 % were first-time mothers and 45 % of pregnant women began their prenatal controls in the second month of pregnancy.
On the other hand, in the same Table 1, in the experimental group, in relation with the sociodemographic characteristics, the mean age of the pregnant women was 28.4 years, 50 % of the pregnant women had completed high school, 90 % were from urban areas, 75 % had a nuclear family. Regarding the prenatal characteristics of the experimental group, the average number of controls of the pregnant women was 2.7, 80 % did not receive training on the ITLM, 50 % were in the 3rd trimester of pregnancy, 55 % were first-time mothers and finally, 40 % started their prenatal controls in the second month of pregnancy.
Table 1: Descriptive statistics of the sociodemographic and prenatal characteristics of the pregnant women
Source: Own elaboration (2021)
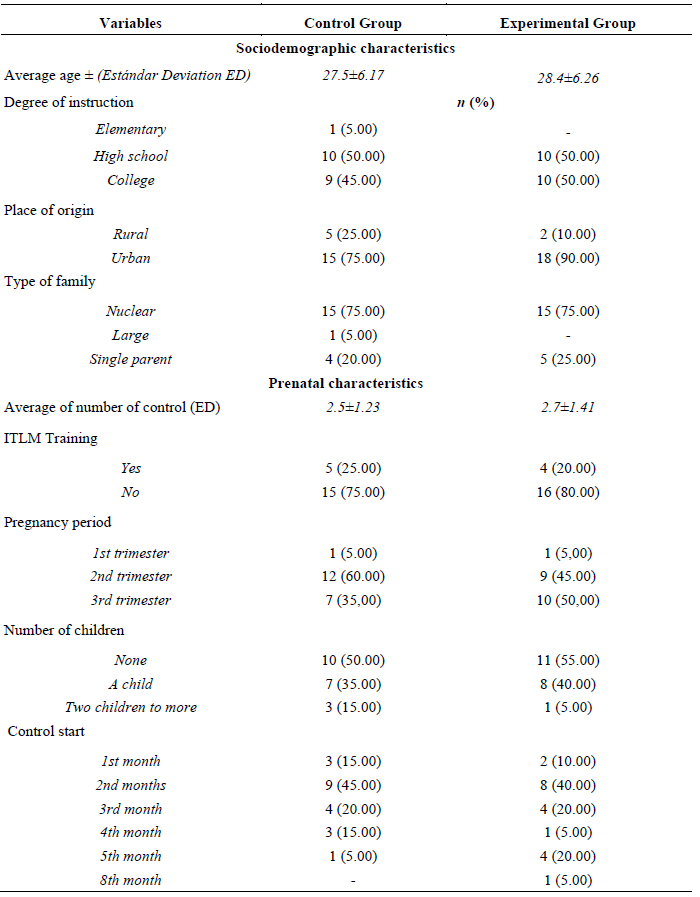
Table 2 shows that before the educational intervention, the experimental group had an average knowledge of the ITLM of 6.25 and after the intervention an average of 9.55, obtaining a difference of 2.9 (p<0.001). However, the control group at first had a knowledge about the ITLM of 5.85 and after the brochure an average of 6.00 where the difference was 0.15, but it was not significant (p=0.74).
Table 2: Average of knowledge about the early initiation of breastfeeding in the experimental and control groups before and after the intervention
Source: Own elaboration (2021)
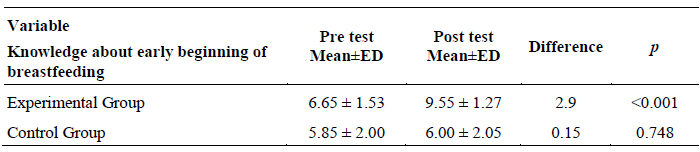
In Table 3 it can be observed in the experimental group, the general dimensions about the ITLM, benefits of the ITLM to the infant and requirements to start breastfeeding early, which were significant (p<0.05) where in the first dimension it increased from 1.95 to 3.05; the second dimension from 1.25 to 2.40 and the fourth dimension from 2.65 to 3.00 increased respectively.
Table 3: Average of the dimensions of knowledge about the early beginning of breastfeeding in the experimental group before and after the intervention
Source: Own elaboration (2021)
In Table 4, the analysis of the dimensions of knowledge about the early beginning of breastfeeding in the control group was carried out, however, the null hypothesis was accepted, because no dimension showed significance (<0.005).
Table 4: Average of the dimensions of knowledge about ITLM in the control group before and after the intervention
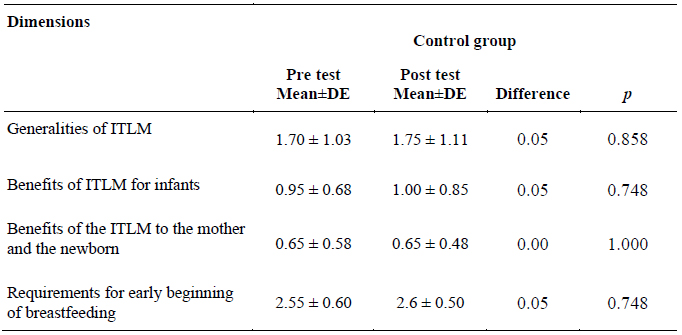
Source: Own elaboration (2021)
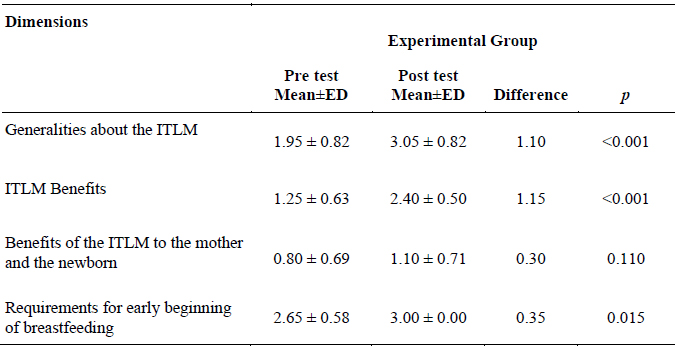
In Table 5 of the total number of pregnant women belonging to the experimental group, 83.33 % performed the ITLM after the intervention. This relationship between the groups and the ITLM was significant (p<0.001).
Discussion
The results show that the educational intervention had an impact on increasing the knowledge of the pregnant women in the experimental group about ITLM. However, no similar studies were found in the literature review. There was a quasi-experimental research project carried out on pregnant women in Iraq, to evaluate the role of nursing intervention in breastfeeding based on the theory of self-efficacy, which collected information on knowledge about breastfeeding through a questionnaire consisting of five parts, where the third included three questions about ITLM: Do you know about early skin-to-skin contact? When do mothers have to start BF after childbirth?, and: Should the baby be given colostrum? The result was, that in the experimental group there was a higher level of knowledge about breastfeeding, after face-to-face prenatal education, compared to pregnant women in the control group. 18
An important finding was that the educational intervention promoted the completion of the ITLM in the experimental group. That is, most of the women who participated in the educational intervention when they were pregnant were able to breastfeed their baby during the first hour of life. This is similar to a study conducted in a rural hospital in Mexico, where an educational intervention before delivery, carried out by trained health personnel, promoted early breastfeeding. This educational intervention explored the benefits, implications, and steps of early skin-to-skin contact and early breastfeeding.19 This is possibly because knowledge about timely initiation of breastfeeding during pregnancy and vaginal delivery is associated with ITLM.20 In addition, it is important to highlight that for the carrying out of the ITLM process it could be due to other factors such as the training of health personnel, the waiting time (between 45 minutes to one hour) for early breastfeeding to start,11 and the mother leaving work routines and starting maternity leave, since previously the nursing professional had to immediately transfer the mother from the delivery bed to the recovery bed, and therefore, the newborn was separated from the mother, for immediate care, interrupting skin to skin contact and the ITLM. Finally, it is important to note that in all pregnant women in this public health center, the health personnel promote natural childbirth, a protective factor for ITLM, because in cesarean delivery, especially unjustified ones, there is less probability of this initiation.21,22
Breastfeeding education for pregnant women is part of prenatal care, which includes both individual and group educational sessions led by previously trained health professionals, 23,24 and is also considered an important factor and resource to develop knowledge, skills and confidence in pregnant women, and therefore, self-efficacy to breastfeed when they become mothers.25-27 For this reason, it is necessary to select suitable didactic tools28) such as the use of the flipchart, which is an educational strategy recommended by WHO that is now used,23 because in each template there is an illustration (educational tool that shows situations and objects exactly as they are in reality) and in addition, a logical order of ideas is shown with short and simple words. 29 Also, as an emerging and versatile technology, virtual education compared to face-to-face education can also improve post-intervention knowledge. It has been shown that virtual education through a digital flipchart and videoconference, commonly used in times of pandemic, showed effectiveness in post-intervention knowledge.30
In this study, the interaction with the participants was important. Women with a higher educational level assimilate more information from this technology compared to those with lower levels of education.31 According to the present study, it is observed that, in the description of the sociodemographic and obstetric profile, most of the pregnant women in the experimental group were younger and without child on average, and according to the literature review it is mentioned that a young population that still does not have children shows greater interest in learning how to face a new experience.32) These results could support the explanation of why the educational intervention had an effect on the increase in knowledge and the completion of the ITLM. It is observed that the sociodemographic profile of pregnant women affects the impact of an educational intervention.
Conclusions
It is evident that the educational intervention influences the increase in ITLM knowledge in the pregnant women of the experimental group. Likewise, later, when they became mothers, most of this group started breastfeeding early. The sociodemographic characteristics of the participants could explain the effectiveness of the virtual educational intervention. On the other hand, it is necessary to mention the importance of the digital flipchart as a virtual educational strategy, since in it the dimensions were captured with images and short and simple phrases, which facilitated understanding in pregnant women and mothers.
From this study, recommendations arise that could help other similar populations. Despite the context of COVID-19, it is recommended that educational interventions continue to be provided during prenatal check-ups, either in person with the relevant biosafety measures or virtual, with the help of the digital flipchart (images and main ideas). Equally, it is recommended that health personnel consider educational interventions as part of their professional routine. Interaction with pregnant women, including with their partners, and considering the sociodemographic and obstetric profile to enhance knowledge about the ITLM, and encouraging them to continue performing it during the motherhood of their infants, showed good results.
Based on these findings, it is necessary to carry out further studies in larger samples. In the same way, other sociodemographic variables should be considered, such as the type of religion, planned pregnancy, occupation and cultural characteristics, in order to promote equity in the population studied.
Carrying out this research at the time of the COVID-19 pandemic was a limitation, since it was difficult to contact pregnant women. On the other hand, it was difficult to find similar studies on the ITLM. A strength of the study is that it was the first carried out in a Peruvian population, being a topic of national interest. It is considered that the continued study and promotion of these interventions would have a positive impact on the educational work of nurses to promote ITLM and therefore encourage exclusive breastfeeding.
REFERENCES
1. Fondo de las Naciones Unidas para la Infancia, Organización Mundial de la Salud. Capturar el momento: Inicio temprano de la lactancia materna: El mejor comienzo para cada recién nacido (Internet). Nueva York: UNICEF; 2018 (citado 21 sep 2021). Disponible en: Disponible en: https://www.unicef.org/lac/media/3031/file/PDF%20Capturar%20el%20momento.pdf [ Links ]
2. Smith, E, Hurt, L, Chowdhury, R, Sinha, B, Fawzi, W, Edmond, K. Delayed breastfeeding initiation and infant survival: A systematic review and meta-analysis. PloS one. 2017;12(7):1-16. [ Links ]
3. NEOVITA Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob Health. 2016;4(4):266-275. [ Links ]
4. Smith, E, Locks, L, Manji, K, Christine, M, Kupka, R, Kisenge, R, et al. Delayed breastfeeding initiation is associated with infant morbidity. The Journal of pediatrics. 2017;191:57-62. [ Links ]
5. Khan, J, Vesel, L, Bahl, R, Martines, J. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: effects on neonatal mortality and morbidity-a systematic review and meta-analysis. Maternal and child health journal. 2015;19(3):468-479. [ Links ]
6. Chiu, H, Wang, H, Hsiao, J, Tzeng, I, Yiang, G, Wu, M, et al. Early breastfeeding is associated with low risk of postpartum depression in Taiwanese women. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2020;40(2):160-166. [ Links ]
7. Sobhy, S, Mohame, N. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. The Journal of the Egyptian Public Health Association. 2004;79(1-2):1-12. [ Links ]
8. Organización Mundial de la Salud. ¡El inicio temprano de la lactancia materna: la clave para supervivencia y desarrollo! (Internet). Washington: OPS; 2010 (citado 03 ago 2022). Disponible en: Disponible en: https://www.paho.org/uru/dmdocuments/Resumentecnico.pdf [ Links ]
9. Ministerio de Salud. Norma técnica Atención Integral de la Salud Neonatal (Internet). Perú: MINSA; 2013 (citado 25 sep 2021). Disponible en: Disponible en: http://bvs.minsa.gob.pe/local/MINSA/3281.pdf [ Links ]
10. Instituto Nacional de Estadísticas e Informática. Encuesta Demografica y de Salud Familiar (Internet). Perú: MINSA ; 2020 (citado 21 oct 2021). Disponible en: Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1795/ [ Links ]
11. Ortiz, Y, Ortiz, K, Mucha, R. ¿Se asocian los procedimientos neonatales de las enfermeras al inicio temprano de la lactancia materna? Evidentia. 2018;15(1):1-7. [ Links ]
12. Karim, F, Billah, S, Chowdhurz, M, Zaka, N, Manu, A, Arifeen, S, et al. Initiation of breastfeeding within one hour of birth and its determinants among normal vaginal deliveries at primary and secondary health facilities in Bangladesh: A case-observation study. PloS one. 2018;13(8):1-15. [ Links ]
13. Ministerio de Salud. Promoción y apoyo a la Lactancia Materna (Internet). Perú: MINSA ; 2019 (citado 28 may 2022). Disponible en: Disponible en: http://bvs.minsa.gob.pe/local/MINSA/4929.pdf [ Links ]
14. Sen, K, Mallick, T, Bari, T. Gender inequality in early initiation of breastfeeding in Bangladesh: a trend analysis. International Breastfeeding Journal. 2020;15(18):1-11. [ Links ]
15. Fondo de las Naciones Unidas para la Infancia. Lactancia Materna (Internet). Honduras: UNICEF; 2012 (citado 28 may 2022). Disponible en: Disponible en: https://www.unicef.org/ecuador/media/2611/file/Lactancia%20materna.pdf [ Links ]
16. Ministerio de Salud. Guía técnica para la consejería en la lactancia materna (Internet). Perú: MINSA ; 2017 (citado 21 sep 2021). Disponible en: Disponible en: http://bvs.minsa.gob.pe/local/MINSA/4173.pdf [ Links ]
17. Curioso, W, Galán, E. El rol de la telesalud en la lucha contra el COVID-19 y la evolución del marco normativo peruano. Acta médica. 2020;37(3):366-375. [ Links ]
18. Safiya, P, Hamdia, A. Impacts of antenatal nursing interventions on mothers’ breastfeeding self-efficacy: an experimental study. BMC pregnancy and childbirth. 2020;20(1):1-12. [ Links ]
19. Sanchez, L, Zuniga, G, Ramirez, J. An educational intervention to implement skin-to-skin contact and early breastfeeding in a rural hospital in Mexico. International Breastfeeding Journal . 2019;14(8):1-9. [ Links ]
20. Lyellu, Y, Hussein, H, Wandel, M, Pedersen, B, Mgongo, M, Msuya, S. Prevalence and factors associated with early initiation of breastfeeding among women in Moshi municipal, northern Tanzania. BMC Pregnancy Childbirth. 2020;20(285):1-10. [ Links ]
21. Hernández, A, Chacón, H. Determinants of early initiation of breastfeeding in Peru: analysis of the 2018 Demographic and Family Health Survey. Epidemiology and health. 2019;41:1-8. [ Links ]
22. Cozma, A, Badiu, I, Stanciu, O, Filip, L, Banc, R, Gavrilaş, L, et al. Determinants of early initiation of breastfeeding among mothers of children aged less than 24 months in northwestern Romania. Nutrients. 2019;11(12):1-13. [ Links ]
23. Organización mundial de la salud. Manual sobre educación sanitaria en atención primaria de salud (Internet). Ginebra: OMS; 1989 (citado 29 nov 2021). Disponible en: Disponible en: https://apps.who.int/iris/handle/10665/38660 [ Links ]
24. Loboa, N, Betancurth, D. El educador para la salud en la salud pública. Revista de Salud Pública. 2020;22(5):1-4. [ Links ]
25. Piro, S, Ahmed, M. Impacts of antenatal nursing interventions on mothers’ breastfeeding self-efficacy: an experimental study. BMC Pregnancy Childbirth . 2020;20(19):1-12. [ Links ]
26. Jeihooni, K, Kashfi, M, Harsini, A. Impact of an educational intervention on breastfeeding behaviour among pregnant women. British Journal of Midwifery. 2019;27(1):33-42. [ Links ]
27. Cardoso, A, Silva, A, Marín, H. Pregnant women’s knowledge gaps about breastfeeding in northern Portugal. Open Journal of Obstetrics and Gynecology. 2017;7(03):376-385. [ Links ]
28. Mostafa, A, Salem, R, Badr, M. Effect of an educational intervention on breastfeeding knowledge and attitude among interns at Cairo University Hospital. Journal of the Egyptian Public Health Association. 2019;94(1):1-7. [ Links ]
29. Abdulahi, M, Fretheim, A, Magnus, J. Effect of breastfeeding education and support intervention (BFESI) versus routine care on timely initiation and exclusive breastfeeding in Southwest Ethiopia: study protocol for a cluster randomized controlled trial. Pediatrics. 2018;18(313):1-14. [ Links ]
30. Kyaw, B, Saxena, N, Posadzki, P, Vseteckova, J, Nikolaou, C, George, P, et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(1):1-13. [ Links ]
31. Sayakhot, P, Carolan, M, Steele, Ch. Use of a web-based educational intervention to improve knowledge of healthy diet and lifestyle in women with Gestational Diabetes Mellitus compared to standard clinic-based education. BMC pregnancy and childbirth. 2016;16(1):1-12. [ Links ]
32. Menor, M, Aguilar, M, Mur, N. Efectividad de las intervenciones educativas para la atención de la salud. Revisión sistemática. Medisur. 2017;(1):71-84. [ Links ]
How to cite: Ortiz Romaní KJ, Vásquez Carbajal AM, Escobelo Encarnación JR, Ortiz Montalvo YJ. Effect of a virtual educational intervention to promote early initiation of breastfeeding in pregnant women from Lima, Peru. Enfermería: Cuidados Humanizados. 2022;11(2), e2820. DOI: 10.22235/ech.v11i2.2820
Contribution of the authors: a) Study conception and design, b) Data acquisition, c) Data analysis and interpretation, d) Writing of the manuscript, e) Critical review of the manuscript. K. J. O. R. has contributed in a, c, d, e; A. M. V. C. in a, b, c, d; J. R. E. E. in b, d, e; Y. J. O. M. in c, d, e.
Received: March 21, 2022; Accepted: July 21, 2022











 texto en
texto en