Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Enfermería: Cuidados Humanizados
versão impressa ISSN 1688-8375versão On-line ISSN 2393-6606
Enfermería (Montevideo) vol.11 no.1 Montevideo jun. 2022 Epub 01-Jun-2022
https://doi.org/10.22235/ech.v11i1.2552
Original Articles
Accompanying Breastfeeding with eHealth: Integrative Review
1 Universidad de Chile, Chile, p.carrasco.salazar@gmail.com
2 Pontificia Universidad Católica de Chile, Chile
3 Pontificia Universidad Católica de Chile, Chile
Introduction:
The World Health Organization recommends exclusive breastfeeding during the first 6 months of life, as well as continuing it supplemented with appropriate foods up, to 2 years and more. Therefore, the need of professional support around it is observed for mothers during pregnancy and once breastfeeding has begun. The World Health Assembly recognized the potential of digital technologies to improve public health, highlighting that the use of eHealth has transformed health, allowing the delivery of care in people’s homes remotely.
Objective:
To determine if professional support through eHealth is a strategy that favors the support to mothers who are going through the breastfeeding process and improves their breastfeeding results.
Methodology:
A integrative review was carried out seeking to understand the phenomenon or topic of interest from different perspectives. To carry it out in June 2020, the databases Pubmed, Scopus, CINAHL, ProQuest, ClinicalKey and Science Direct were consulted.
Results:
They were organized into two groups: professional support strategies through eHealth to mothers in breastfeeding process and results of eHealth as a tool for professional support to mothers in breastfeeding process.
Conclusion:
eHealth is an effective tool to provide meaningful support to pregnant or breastfeeding women.
Keywords: eHealth; telehealth; mHealth; breastfeeding; review literature
Introducción:
La Organización Mundial de la Salud recomienda la lactancia materna exclusiva durante los primeros 6 meses de vida, así como continuar complementada con alimentos apropiados hasta los 2 años y más. Es por esto, que se observa la necesidad del apoyo profesional en torno a esta, para las madres durante el embarazo y una vez iniciado el amamantamiento. La Asamblea Mundial de la Salud, reconoció el potencial de las tecnologías digitales para la mejora de la salud pública, destacando que el uso de eHealth ha transformado la salud, permitiendo la entrega de cuidados en los hogares de las personas de manera remota.
Objetivo:
Determinar si el apoyo profesional por medio de eHealth es una estrategia que favorece el acompañamiento a las madres que viven el proceso de amamantamiento y mejora sus resultados en la lactancia materna.
Metodología:
Se realizó una revisión integrativa buscando la comprensión del fenómeno o tema de interés desde diversas perspectivas. Para llevarla a cabo en junio de 2020 se consultaron las bases de datos Pubmed, Scopus, CINAHL, ProQuest, ClinicalKey y Science Direct.
Resultados:
Se organizaron en dos grupos: estrategias de acompañamiento profesional a través de eHealth a las madres en proceso de amamantamiento y resultados de eHealth como herramienta para el acompañamiento profesional a las madres en proceso de amamantamiento.
Conclusión:
La eHealth es una herramienta efectiva para brindar apoyo a mujeres embarazadas o en proceso de amamantamiento.
Palabras clave: eHealth; telehealth; mHealth; lactancia materna; revisión de literatura
Introdução:
A A Organização Mundial da Saúde recomenda o aleitamento materno exclusivo durante os primeiros 6 meses de vida, e também que seja complementado com alimentos apropriados até os 2 anos ou mais. É por isso que se faz necessário o apoio profissional às mães neste processo, desde a gestação até o início da amamentação. A Assembléia Mundial da Saúde reconheceu os benefícios das tecnologias digitais para o aprimoramento da saúde pública, destacando a ferramenta eHealth, cuja utilização transformou a saúde e permitiu um atendimento especializado nos lares das pessoas, de maneira remota.
Objetivo:
Determinar se o apoio profissional por meio da eHealth é uma estratégia que favorece o acompanhamento às mães que estão atravessando o processo de amamentação e melhora seus resultados do aleitamento.
Metodologia:
Foi realizada uma revisão integrativa, procurando compreender o fenômeno ou tópico de interesse a partir de diferentes perspectivas. Para implementá-la em junho de 2020 foram consultadas as bases de dados Pubmed Scopus, CINAHL, ProQuest, ClinicalKey e Science Direct.
Resultados:
Eles foram organizados em dois grupos: estratégias de apoio profissional por meio da eHealth para mães em processo de amamentação e resultados da eHealth como ferramenta de apoio profissional para mães em processo de amamentação.
Conclusão:
A eHealth é uma ferramenta efetiva oferecem um suporte significativo às gestantes e às mães durante o aleitamento.
Palavras-chave: eHealth; telehealth; mHealth; aleitamento materno; revisão de literatura
Introduction
The World Health Organization (WHO) has described breastfeeding as the cornerstone of infant survival, nutrition and development and maternal health, and recommends exclusive breastfeeding for the first 6 months of life, followed by appropriate complementary feeding for up to 2 years of age and beyond. 1
Considering this recommendation, the WHO committed itself to support countries in the implementation and follow-up of the "Comprehensive implementation plan on maternal, infant and young child nutrition", adopted by member states in May 2002. The plan has six targets, one of which is to increase exclusive breastfeeding at 6 months of age to at least 50 percent by 2025. In 2018, the WHO estimated that 33 countries had met this target; therefore, by 2018, 68 countries still had exclusive breastfeeding rates at 6 months of life below 50 %. 2
In this scenario and with the aim of improving breastfeeding rates, the need to increase efforts at the health system, political and community levels was emphasized, the latter level of action being considered crucial for strategies to have a chance of success. 3
This is not a recently visualized need, as WHO and the United Nations Children's Fund (UNICEF) jointly published a statement in 1989 on the protection, promotion and support of breastfeeding, where they presented the ten steps towards a happy and natural breastfeeding, which were the basis for the Baby-Friendly Hospital Initiative, published in 1991. 4
In 2018, WHO and UNICEF published an update of these ten steps, explaining how health facilities should have a clear breastfeeding policy, trained professionals and antenatal and postnatal care services, reaffirming the idea that supporting mothers during pregnancy, immediately after birth and once breastfeeding is initiated, has positive effects on breastfeeding outcomes. 5
The above mentioned underpins the importance of reaching mothers in the breastfeeding process with this support, overcoming existing community barriers such as literacy, geography and access to technology, and based on this, considering support strategies that are meaningful to mothers experiencing the breastfeeding process. (4
In this regard, the World Health Assembly in 2018 recognized the enormous potential of digital technologies for improving public health, and urged Member States to prioritize their development and use as a means to promote Universal Health Coverage and advance the Sustainable Development Goals (SDGs). 6
Digital health was defined by the WHO as "a broad umbrella that includes the use of information and communication technologies (ICTs), as well as emerging areas, such as the use of advanced computer science in big data and artificial intelligence". 7
The use of ICTs in support of health is called eHealth, a term which in turn includes, as a subset, the use of mobile wireless technology (mHealth), so that the use of video calls, text messages, remote monitoring as a means of delivering care would be included in this group, among others. 7
In 2019, the WHO reiterated the great contribution of digital technologies in strengthening health systems and stressed that the use of eHealth had transformed health, allowing, among other things, the delivery of care remotely in people's homes, making it essential to harness the potential of digital technologies not as an end in themselves, but as essential tools for achieving universal health coverage. 7
However, the WHO recognizes the overwhelming diversity of digital tools and the limited understanding of their impact on people's health and well-being. Thus, there is a need to demonstrate the benefits of including digital technologies in health systems so that their incorporation is sustainable over time 6,7. Therefore, the research question posed is the following: Is professional support through eHealth a strategy that favors the accompaniment of mothers in the breastfeeding process and improves their breastfeeding outcomes?
Methodology
Research question broken down
- P: Mothers who are experiencing breastfeeding
- I: Professional support through eHealth
- C: On-site accompaniment
- O: Accompanying mothers in the breastfeeding process | Breastfeeding outcomes
To answer the research question, the integrative review method was chosen, as it includes both empirical and theoretical publications, thus allowing the understanding of the phenomenon or topic of interest from different perspectives, so the information extracted will be synthesized in a narrative and critical way. 8
A search was conducted in the Pubmed, Scopus, CINAHL, ProQuest, ClinicalKey and Science Direct collections with the MeSH and DeCS descriptors: Breastfeeding, Telehealth and Telemedicine.
The search strategy incorporated the Boolean operators AND and OR, and automatic filters were used to obtain the primary articles available in full text, published between 2016-2021.
The inclusion criteria for the articles also considered that the research population included pregnant women, healthy women and infants who were recipients of care through eHealth in all or some of the stages of their breastfeeding process.
Subsequently, and once the articles had been selected by title and abstract, a critical reading was carried out using the instruments for the analysis of clinical trials, qualitative and observational studies of the Critical Reading Skills Program in Spanish (CASPe), so that all those that did not meet the established criteria of methodological rigor were eliminated from the sample, triangulating the information between authors in the event of controversy.
Results and discussion
The initial search yielded 539 available articles from which only primary research articles were selected, resulting in a total of 240 studies. After reading the title and abstract, 32 articles were selected that met all the established inclusion criteria.
After a critical reading of the full version of the selected studies, a total sample of 19 was obtained. Figure 1.
The articles included in this review come from 15 different journals, 79 % (n=15) of which are quantitative studies.
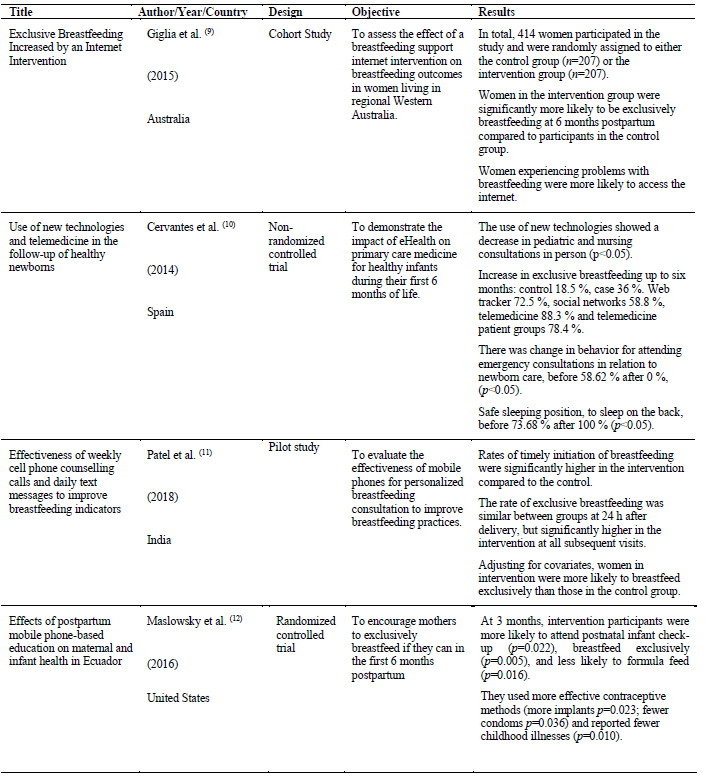
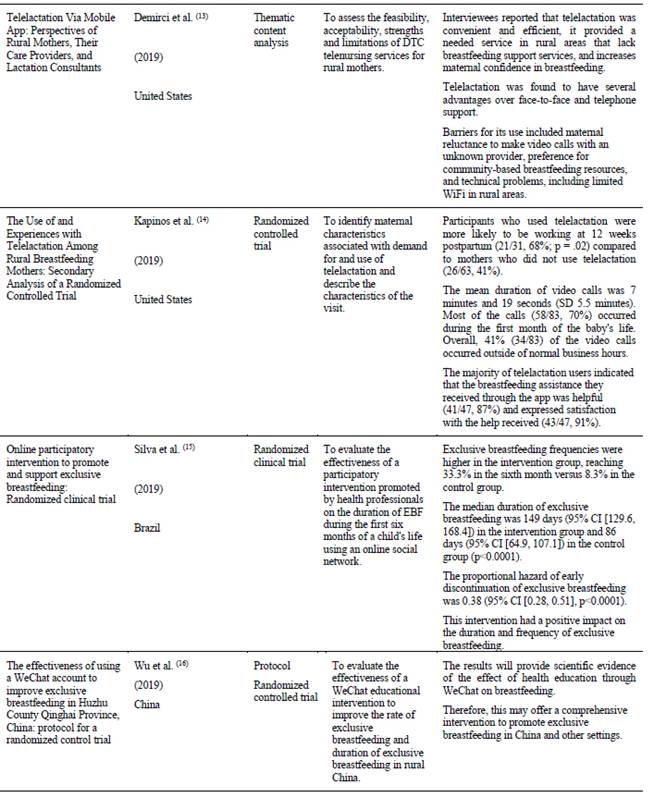
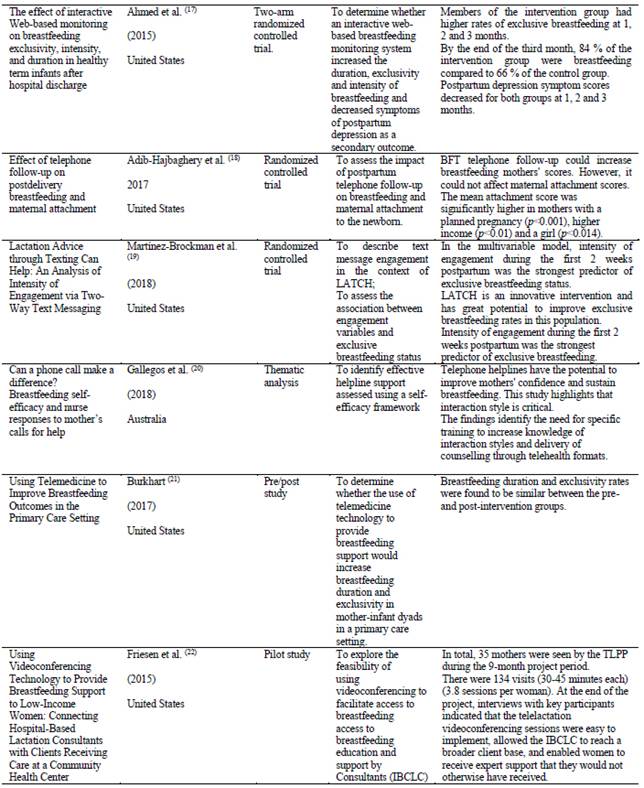
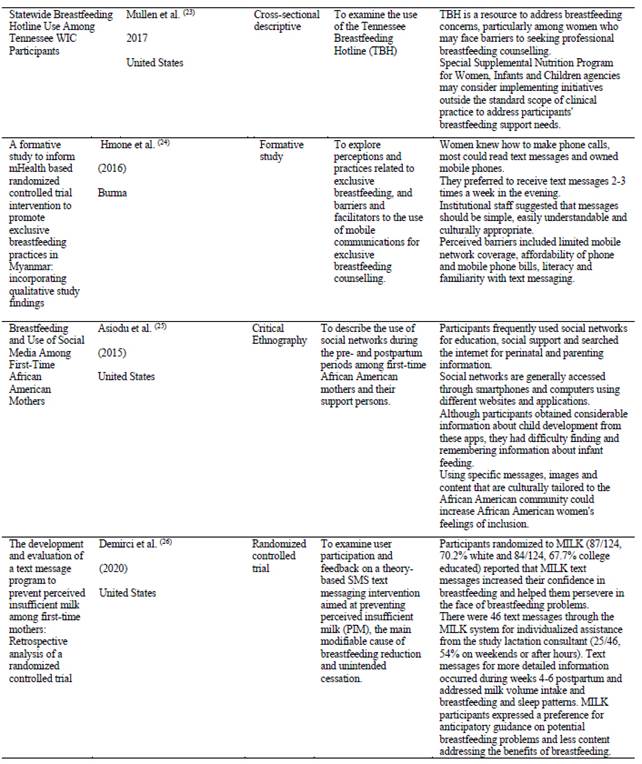
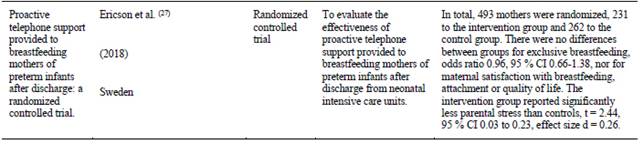
The United States is the country where 58 % (n=11) of the selected articles were published, followed by 11 % (n=2) of articles published in Australia. In this review only 11 % (n=2) of the articles contain data from Latin America, with Brazil and Ecuador being the countries where this research was conducted. Table 1. Part 1 Part 2 Part 3 Part 4 Part 5
The results of this study were organized into two groups: Strategies for professional accompaniment of breastfeeding mothers through eHealth and Results of eHealth as a tool for professional accompaniment of breastfeeding mothers.
Professional accompaniment strategies through eHealth for breastfeeding mothers
Within the eHealth strategies in the studies analyzed, synchronous interventions such as telephone calls and video conferences were distinguished, as well as asynchronous ones such as text messages, use of social networks, telephone applications and digital platforms.
Regarding the modalities, a greater openness to receive professional support via telephone, email and text messages was reported, compared to video calls. However, when compared to face-to-face support, they tended to be less time-consuming, which emerged as a welcome feature for mothers in more urbanized areas, who also expressed gratitude for the flexible hours.9,10
Patel et al.11 on strategies used to promote breastfeeding concluded that any pre- and postnatal support strategy increased exclusive breastfeeding rates by almost 6 times compared to no intervention.
Consistent with this, other research also highlighted that eHealth support interventions enabled mothers who received them to be more likely to breastfeed exclusively and even more so when interventions were implemented with mothers in rural or hard-to-reach areas.9,12 -14
Silva et al.15 in their study commented that these interventions, grouped as eHealth in this research, do not require expensive technologies or large investments in infrastructure, especially considering the large number of mobile phones worldwide, as recognized by Maslowsky et al. 12
In the same vein, Wu et al. 16 highlighted that smartphones have become the new channels and tools for information acquisition and exchange, to which users have enthusiastically adapted and as mentioned by other authors, the use of mobile technologies and the internet are viable, innovative, accessible and increasingly popular options among people. 12,15,17,18
In line with the above, the research by Ahmed et al. 17 makes explicit the idea that the integration of mobile phones in the accompaniment of breastfeeding women is an innovative strategy to improve postpartum care, offering information and support through the creation of people networking, promoting breastfeeding and especially exclusive breastfeeding.
A number of studies have reported an increase and improvement in the practice of exclusive breastfeeding, which is directly related to the frequency of contacts and the number of difficulties encountered. 12,15,17,19
Regarding the above, Patel et al. 11 reported that their mobile phone text messaging intervention substantially increased exclusive breastfeeding rates from birth to 6 months of age, where 95% of infants in the intervention group were exclusively breastfed compared to 48.5% of infants in the control group.
Silva et al. 15 noted that inclusion of mothers in a social network group promoted by health professionals reduced rates of early discontinuation of exclusive breastfeeding during the first 6 months of life by 62 % compared to mothers who did not participate in this group.
Improvements in exclusive breastfeeding rates are directly related to the promotion of self-efficacy. In relation to this, Gallegos et al. 20 acknowledged in their research that professional support by telephone calls has the potential to promote breastfeeding self-efficacy, which was corroborated by other studies. 18,21
In addition to increased self-efficacy and willingness to breastfeed, the benefits of eHealth to support breastfeeding were found to include cost savings associated with seeking face-to-face support, providing greater access to care. 22
These benefits are also recognized by other authors who argue that remote professional support is an innovation in care delivery that, in addition to lowering costs, increases comfort and responsiveness to breastfeeding.13,14,23
In line with the above, it has been mentioned that eHealth has the potential to provide personalized support to breastfeeding mothers highlighting that face-to-face and individual breastfeeding support can be slow, costly and not always available, particularly in rural and remote areas. 9
The advent of the Internet and access to technology has provided an additional domain for the provision of services by health professionals, overcoming the aforementioned barriers of cost, isolation and time, which in more urbanized areas, was highlighted as an interfering factor. 9,15,22
It is important to mention that for this form of professional support for mothers to result in a successful breastfeeding process, studies highlight the need for organization and training of professionals for online monitoring. 15,18,20
As interfering factors for the success of exclusive breastfeeding, women's choice to supplement breast milk with other foods due to perceived insufficient milk production and the prescription of formula milk by physicians were mentioned. These reasons are amenable to counselling and support through eHealth. 11,14
With regard to the limitations of eHealth, the following were described: the need for the mother to keep the device switched on and charged, rejected calls, unanswered or received by someone other than the mother who requires accompaniment, loss of mobile phones or change of number; also, the possibility of misinterpretation of written messages, in addition to the existence of areas that do not yet have internet connection. 13,14
Results of eHealth as a tool for the professional accompaniment of breastfeeding mothers
When mothers feel supported during their breastfeeding process, they are more likely to breastfeed their children longer and exclusively. 21 This was reinforced by other studies which show that the support offered to mothers after discharge from hospital is decisive for the establishment, maintenance and exclusivity of breastfeeding. Therefore, it can be seen that the relevant use of eHealth-based support strategies can be a great contribution to professional support and thus help mothers to experience successful breastfeeding. 15,19-21
Understanding the importance of this, it is imperative to organize and train professional teams around this new form of support, because if the support is not comprehensive and even perceived as insensitive or unhelpful, it can lead to negative and potentially long-lasting consequences for both mother and child. 10,20
For interventions to be incorporated and bring about a change in health behaviors, evidence indicates that care must be person-centered, addressing the needs and particularities of the individual, leading to the delivery of culturally congruent care. 24,25
Related to this, for example, a study targeting African American women highlights that this population may be less receptive to forums that do not recognize their history and culture. Particularly in relation to the impact of slavery on African American understanding of the meanings related to breastfeeding, the use of culturally tailored messages, images, and content, could increase African American women's feelings of inclusion and consequently improve their adherence to support. 25
For there to be a real and positive influence on breastfeeding through eHealth, interventions must be mother-centered by responding to her beliefs, preferences, requests and concerns, contributing to the promotion of self-efficacy and thereby influencing the foundation for successful breastfeeding. 9,20,22,26
There are studies that highlight that breastfeeding support strategies that are oriented towards transmitting only technical-scientific knowledge and do not address the subjectivities and realities of each woman are superficial. Consequently, they do not meet the comprehensive care needs of women in the breastfeeding process. 13,15,19,21
In accordance with the above, it is also necessary to identify access to devices and internet, technological literacy and beliefs regarding the digital strategies that will be used to provide accompaniment. 10,20,24
The mobile phone, in particular the use of SMS text messaging, may provide an opportunity not only to improve breastfeeding rates, but also to improve health behaviors.24
Regarding this last point, other research also considered that monitoring through different eHealth strategies is a good method, not only to support mothers, increase their knowledge and improve their breastfeeding practice, but also to improve maternal and child health. 11,12,18
This refers to the fact that mothers who received this support showed greater satisfaction, lower incidence of stress and depression; and children showed better weight gain at each check-up, reduced morbidity and limited further deterioration of health, which reduced infant hospitalization, contributing to the reduction of infant mortality. 11,12,18,27
This form of interaction could help overcome emotional difficulties, and increase mothers' peace of mind, confidence in breastfeeding and sharing of knowledge and experiences, improving communication between professionals and mothers, making support more effective and humanized. 15,17,18
For support to have positive results, the evidence recommends initiating it in the first few days after discharge and maintaining it continuously for at least 6 months. In addition, to achieve greater adherence to this form of professional support, it was described as necessary to generate intervention strategies developed in a pedagogical and participatory manner by health professionals. In this way they stimulate dialogue and interaction between the subjects, requiring that the generation of instances of support comes mostly from the professionals; notwithstanding always having the capacity to respond to the urgent needs of the mothers. 11,14,15,18,27
Conclusion
Considering the objective of this research, eHealth was found to be an effective tool to provide professional support to women in the process of breastfeeding, as well as to promote breastfeeding.
This new way of providing support is characterized by continuity of care, convenience associated with the absence of travel, greater satisfaction with the time spent, and improved accessibility.
eHealth can be used successfully in low-, middle- and high-income settings, as the use of mobile devices is almost universal. However, professionals need to be trained to better manage resources and acquire the skills to provide quality, safe and proactive care that is meaningful to the people receiving it.
The positive effects of this type of accompaniment and the increased acceptance of these interventions make eHealth a powerful and efficient tool that contributes to the maintenance and improvement of breastfeeding, as well as comprehensive maternal and child health.
This study seeks to contribute to the strengthening of the tenth step for happy and natural breastfeeding, which is "To coordinate hospital discharge so that parents and their new-borns continue to have access to care and support services when needed".
REFERENCES
1. Organización Mundial de la Salud. Breastfeeding and COVID-19: scientific brief, 23 June 2020 (Internet). 2020 (citado 10 de junio de 2020). Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/332639/WHO-2019-nCoV-Sci_Brief-Breastfeeding-2020.1-eng.pdf?sequence=1&isAllowed=y [ Links ]
2. Organización Mundial de la Salud. Nutrición de la madre, el lactante y el niño pequeño: plan integral de aplicación sobre nutrición de la madre, el lactante y el niño pequeño: informe bienal: informe del Director General (Internet). 2018 (citado 10 de junio de 2020). Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/276443/A71_22-sp.pdf?sequence=1&isAllowed=y&ua=1 [ Links ]
3. Organización Mundial de la Salud. Promoting proper feeding for infants and young children. Nutrition (Internet). 2015 (citado 4 de julio 2020);7-9. Disponible en: Disponible en: http://www.who.int/nutrition/topics/infantfeeding/en/ [ Links ]
4. Organización Mundial de la Salud. Guideline: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services (Internet). 2017 (citado 4 de julio 2020);1-136. Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/259386/9789241550086-eng.pdf [ Links ]
5. Organización Mundial de la Salud y el Fondo para las Naciones Unidas (UNICEF). Guía para la aplicación: proteger, promover y apoyar la lactancia materna en los establecimientos que prestan servicios de maternidad y neonatología - Revisión de la Iniciativa Hospitales Amigos del Niño 2018 (Internet). 2019 (citado 4 de julio 2020). Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/326162/9789243513805-spa.pdf?ua=1 [ Links ]
6. Organización Mundial de la Salud. Executive Board. mHealth Use of appropriate digital technologies for public health: report by the Director-General (Internet). 2017 (citado 10 de junio de 2020). Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/274134/B142_20-en.pdf?sequence=1&isAllowed=y [ Links ]
7. Organización Mundial de La Salud. WHO Guideline: Recommendations on digital interventions for health system strengthening (Internet). 2019 (citado 10 de junio de 2020). Disponible en: Disponible en: https://apps.who.int/iris/bitstream/handle/10665/274134/B142_20-en.pdf?sequence=1&isAllowed=y [ Links ]
8. Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci (Internet). 2016 (citado 10 de junio de 2020);30(4):662-9. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/27074869/ [ Links ]
9. Giglia R, Cox K, Zhao Y, Binns CW. Exclusive breastfeeding increased by an internet intervention. Breastfeed Med (Internet). 2015 (citado 11 de junio de 2020);10(1):20-5. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/25358119/ [ Links ]
10. Cervantes Guijarro CM, Sanchez Luna M, Bazan Fernandez P. Uso de las nuevas tecnologías y telemedicine en el seguimiento del recién nacido sano. Pediatr Aten Primaria. (Internet). 2014 (citado 10 de junio de 2020);16(64):305-10. Disponible en: Disponible en: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1139-76322014000500005 [ Links ]
11. Patel A, Kuhite P, Puranik A, Khan SS, Borkar J, Dhande L. Effectiveness of weekly cell phone counselling calls and daily text messages to improve breastfeeding indicators. BMC Pediatr (Internet). 2018 (citado 11 de junio de 2020);18(1):337. Disponible en: Disponible en: https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-018-1308-3 [ Links ]
12. Maslowsky J, Frost S, Hendrick CE, Trujillo Cruz FO, Merajver SD. Effects of postpartum mobile phone-based education on maternal and infant health in Ecuador. Int J Gynecol Obstet (Internet). 2016 (citado 11 de junio de 2020);134(1):93-8. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/27126905/ [ Links ]
13. Demirci J, Kotzias V, Bogen DL, Ray KN, Uscher-Pines L. Telelactation via Mobile App: Perspectives of Rural Mothers, Their Care Providers, and Lactation Consultants. Telemed e-Health (Internet). 2019 (citado 11 de junio de 2020);25(9):853-8. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6748400/pdf/tmj.2018.0113.pdf [ Links ]
14. Kapinos K, Kotzias V, Bogen D, Ray K, Demirci J, Rigas MA, et al. The use of and experiences with telelactation among rural breastfeeding mothers: Secondary analysis of a randomized controlled trial. J Med Internet Res (Internet). 2019 (citado 11 de junio de 2020);21(9). Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/31482848/ [ Links ]
15. Silva Cavalcanti D, Sousa Cabral C, Pinheiro de Toledo Vianna R, Maria Osório M. Online Participatory Intervention to Promote and Support Exclusive Breastfeeding: Randomized Clinical Trial. MCN Am J Matern Nurs (Internet). 2019 (citado 10 de junio de 2020);44(6):366. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/30825414/ [ Links ]
16. Wu Q, Huang Y, Van Velthoven MH, Wang W, Chang S, Zhang Y. The effectiveness of using a WeChat account to improve exclusive breastfeeding in huzhu county qinghai province, China: Protocol for a randomized control trial. BMC Public Health (Internet). 2019 (citado 10 de junio de 2020);19(1):1603. Disponible en: Disponible en: https://www.researchgate.net/publication/337688471_The_effectiveness_of_using_a_WeChat_account_to_improve_exclusive_breastfeeding_in_Huzhu_County_Qinghai_Province_China_protocol_for_a_randomized_control_trial [ Links ]
17. Ahmed AH, Roumani AM, Szucs K, Zhang L, King D. The Effect of Interactive Web-Based Monitoring on Breastfeeding Exclusivity, Intensity, and Duration in Healthy, Term Infants After Hospital Discharge. JOGNN - J Obstet Gynecol Neonatal Nurs (Internet). 2016 (citado 10 de junio de 2020);45(2):143-54. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/26779838/ [ Links ]
18. Adib-Hajbaghery M, Hashemi-Demneh T. Effect of telephone follow-up on postdelivery breastfeeding and maternal attachment. J Nurs Midwifery Sci. 2017;4(4):117. [ Links ]
19. Martinez-Brockman JL, Harari N, Pérez-Escamilla R. Lactation Advice through Texting Can Help: An Analysis of Intensity of Engagement via Two-Way Text Messaging. J Health Commun (Internet). 2018 (citado 10 de junio de 2020); 23(1):40-51. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/29236569/ [ Links ]
20. Gallegos D, Cromack C, Thorpe KJ. Can a phone call make a difference? Breastfeeding self-efficacy and nurse responses to mother’s calls for help. J Child Heal Care (Internet). 2018 (citado 10 de junio de 2020);22(3):433-46. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/29514511/ [ Links ]
21. Burkhart S. Using Telemedicine to Improve Breastfeeding Outcomes in the Primary Care Setting Sarah Burkhart University of Missouri-Kansas City (Internet). 2017 (citado 10 de junio de 2020). Disponible en: Disponible en: https://mospace.umsystem.edu/xmlui/handle/10355/63241 [ Links ]
22. Friesen CA, Hormuth LJ, Petersen D, Babbitt T. Using videoconferencing technology to provide breastfeeding support to low-income women: Connecting hospital-based lactation consultants with clients receiving care at a community health center. J Hum Lact (Internet). 2015 (citado 10 de junio de 2020);31(4):595-9. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/26297347/ [ Links ]
23. Mullen SM, Marshall A, Warren MD. Statewide Breastfeeding Hotline Use Among Tennessee WIC Participants. J Nutr Educ Behav. (Internet) 2017 (citado 12 de junio de 2020);49(7):S192-S196.e1. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/28689557/ [ Links ]
24. Hmone MP, Dibley MJ, Li M, Alam A. A formative study to inform mHealth based randomized controlled trial intervention to promote exclusive breastfeeding practices in Myanmar: Incorporating qualitative study findings. BMC Med Inform Decis Mak (Internet). 2016 (citado 12 de junio de 2020);16(1):60. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/27260252/ [ Links ]
25. Asiodu I V., Waters CM, Dailey DE, Lee KA, Lyndon A. Breastfeeding and Use of Social Media Among First-Time African American Mothers. JOGNN - J Obstet Gynecol Neonatal Nurs (Internet). 2015 (citado 10 de junio de 2020);44(2):268-78. Disponible en: Disponible en: https://translate.google.com/translate?hl=es-419&sl=en&u=https://pubmed.ncbi.nlm.nih.gov/25712127/&prev=search&pto=aue [ Links ]
26. Demirci JR, Suffoletto B, Doman J, Glasser M, Chang JC, Sereika SM, et al. The development and evaluation of a text message program to prevent perceived insufficient milk among first-time mothers: Retrospective analysis of a randomized controlled trial. J Med Internet Res (Internet). 2020 (citado 10 de junio de 2020);22(4):e17328. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32347815/ [ Links ]
27. Ericson J, Eriksson M, Hellström-Westas L, Hoddinott P, Flacking R. Proactive telephone support provided to breastfeeding mothers of preterm infants after discharge: a randomised controlled trial. Acta Paediatr Int J Paediatr (Internet). 2018 (citado 10 de junio de 2020);107(5):791-8. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/29405368/ [ Links ]
How to cite: Carrasco Salazar P, Márquez-Doren F, Lucchini-Raies C. Accompanying Breastfeeding with eHealth: Integrative Review. Enfermería: Cuidados Humanizados. 2022;11(1), e2552. DOI: 10.22235/ech.v11i1.2552
Contribution of the authors: a) Study conception and design, b) Data acquisition, c) Data analysis and interpretation, d) Writing of the manuscript, e) Critical review of the manuscript. P. C. S. has contributed in a, b, c, d; F. M. D. in e; C. L. R. in e.
Received: April 20, 2021; Accepted: April 18, 2022











 texto em
texto em