Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.10 no.2 Montevideo 2021 Epub Dec 01, 2021
https://doi.org/10.22235/ech.v10i2.2546
Original Articles
Users of Alcohol and other Drugs in the Psychosocial Care Network: Nursing Care
1 Universidade do Estado da Bahia, Brazil
2 Universidade do Estado da Bahia, Brazil
3 Universidade do Estado da Bahia, Brazil
4 Universidade de São Paulo, Brazil
5 Universidade Federal da Bahia, Brazil
6 Universidade do Estado da Bahia, Brazil, rudvalsousa@yahoo.com.br
Keywords: mental health services; health care; access to health services; reception; nursing.
Palavras-chave: serviços de saúde mental; atenção à saúde; acesso aos serviços de saúde; acolhimento; enfermagem.
Palabras clave: servicios de salud mental; cuidados de la salud; acceso a servicios de salud; recepción; enfermería.
Introduction
According to a report by the World Health Organization, the issue of alcohol consumption and other drugs has been characterized as one of the main public health problems in the world, in fact school age children have already used some type of illicit drug.1 The World Drug Report, published in 2018, reveals an expansion of the world market in the use of illicit psychoactive substances, with opium, cocaine and cannabis occupying a prominent place among the most consumed drugs in 2016, this includes the Brazilian situation. 2
According to the 3rd National Survey on drug use by the Brazilian population, 3.2% of individuals used illegal substances in the 12 months prior to the survey, which corresponds to 4.9 million people. In this scenario, it is noteworthy that the most alarming data relates to the abuse of alcohol. This is undoubtedly seen as a public health problem, which requires the reformulation of care practices aimed at these users with a focus on mental health. 3
Historically, the mental health care model focused only on the disease, in a hospital-centric perspective, and excluded issues outside of the disease model. However later discussions about the chronicity of users, the biomedical model, the violation of human and citizenship rights, led to political, scientific, and social initiatives. This brought about a new way of thinking about the health-disease process which was based on valuing individual care. 4
From this perspective, the Psychosocial Care Network (Portuguese acronym: RAPS) emerged, (established by Ordinance No. 3.088/2011 of the Ministry of Health of Brazil) as a strategy for coping with vulnerabilities, injuries and diseases that affect the population. The Network proposes the reorganization of mental health services in an integrated manner, diversifying and expanding health actions and equipment, aiming to ensure universal access and comprehensive care for people in psychological distress. 5
RAPS' action is directly formed within primary care services, with a Family Health Strategy, Basic Health Units and street offices; hospital care services, with psychiatric beds in general, urgent and emergency hospitals; specialized services, such as the Psychosocial Care Centers (Portuguese acronym: CAPS); in addition to the services of therapeutic residences. 6
Regarding specialized services, it is worth mentioning the CAPS modalities. These are the Adult CAPS, CAPSi (children and adolescents), and the AD CAPS (Alcohol and drugs). Their purpose is centered on the performance of a strategic role in the articulation of the network within the area, and thus creating an important advance in mental health care, with an open and community-based model, and guaranteeing the free movement of people through health services and other places in the community. (7
From this perspective, caps in line with the principle of comprehensive care, it is recognized that the problem of drug addiction is multifactorial and requires a variety of interventions. These are the expansion of coverage with the participatory performance of health professionals to meet individual needs of users, focusing on the harm caused by the misuse of alcohol and other drugs, psychosocial rehabilitation, and a harm reduction policy.8-9
In this situation Psychiatric Nursing at the national and international level is recognized as a significant professional specialty, as it improves access and quality in the services of the mental health network as a part of public health demands, with a good capacity for inclusion in multidisciplinary teams. The nursing team professionals are a fundamental base for the care of network users, since in all the strategies that make up RAPS, this team is a continual presence. 9
The nursing team, from the perspective of interdisciplinary work, has the commitment and responsibility to develop a psychosocial care model that is capable of establishing participatory relationships with users, as well as building those therapeutic proposals committed within the guidelines of the Brazilian Psychiatric Reform. These seek to exercise a humanized care that recognizes the subject as the protagonist and considers their individuality, with a focus on multidimensionality as a biopsychosocial-spiritual being.5,8-9
Thus, professional nursing care for alcohol abusers and other drugs in RAPS should be based on an expanded clinical perspective, where professionals can break barriers with hospitalization and isolation, and consolidate care that includes intersectoral and interdisciplinary actions, that are capable of promoting continuous monitoring and linking users to the services that make up strategic, primary and hospital care. 5
To understand the strategy and work of the expanded clinic, it is important to return to the concept of care production as a new paradigm emerging from the proposition of breaking with the traditional care practice, which is centered on medical knowledge and on a clinic based exclusively on the biological dimension. The expanded clinic care system assumes the user as the core of the process, and it is important to note that in the context of mental health, this is represented by alcohol abusers/other drug abusers and their families. Thus, care is produced from collective and related moments between users, family, and health workers. 10
In this study, it is proposed to analyze the interrelationship between users of alcohol and other drugs, accompanied by RAPS, and the workers of the nursing team, to enable identification and understanding as how care may be given in these scenarios.
Thus, this study aims to analyze the production of care provided by the nursing team to users of alcohol and other drugs in the Psychosocial Care Network.
Methodology
This is an exploratory and descriptive research with a qualitative approach that is based on the idiosyncrasies related to the constructivist paradigm, (11) and based on social research, 12 considering its approach to the theme of care production in RAPS as a phenomenon, in its assumption to the inherent complexity within psychosocial care. The survey met the steps recommended by the Consolidated Criteria for Reporting a Qualitative Survey (COREQ). 13
The study was carried out in three health units, namely: Psychosocial Care Centre in the specialty alcohol and drugs (AD CAPS); Psychosocial Care Centre mod I (CAPS I), and a Family Health Strategy team (Portuguese acronym: ESF). These are all located in a municipality in the interior of Bahia - Brazil.
These units are part of the Health Care Network of the municipality where the study took place. The Family Health Strategy (ESF) unit is a complementary service to the primary care model, which is based on multidisciplinary teamwork in the territory. The other two units (CAPS I and CAPS AD) are specialized mental health units that compose the RAPS, and carry out monitoring, treatment, and social reintegration of people with severe and persistent mental disorders. They also act in a perspective of interdisciplinary care, with a multidisciplinary team, in which the nursing team is has a role.
This study is an integral part of a Master’s Research developed in the Graduate Program in Public Health at the Universidade Estadual de Feira de Santana (UEFS).
Six nurses and five nursing technicians (members of the teams of the services) participated in the study. They responded to a semi-structured interview with the following guiding question: “How is nursing care produced with users of alcohol and other drugs followed up in RAPS?” There were other questions related to the sociodemographic and labor characterization of the participants and validated by researchers from the research group with experience in the relevant area.
An inclusion criterion was that the team member had to be working in the service for more than six months, and exclusion criteria were those employees on vacation, leave or assuming a management position. All participants voluntarily agreed to collaborate with the study and signed the Informed Consent Form.
Of the 13 professionals from the nursing teams working in the three scenarios and who met the inclusion criteria, only two nursing technicians refused to participate in the study.
Data collection took place between December 2017 and February 2018, through interviews conducted in privacy, with an average duration of 30 minutes, using a voice recorder. Statements were transcribed and organized for analysis according to Bardin's Content Analysis Technique. 14
The Thematic Content Analysis 14 followed three steps: 1) pre-analysis, in which data from the empirical material were organized; floating reading of the interviewees' statements were performed, leading to the identification of registration units; 2) exploration of the material allowed the researchers to proceed with the excerpts of the interviewees' statements, transforming them into record units, which were classified, coded and finally grouped into units which could be based on convergences and divergences, from these the thematic categories emerged ; 3) treatment of the results led to the prioritisation of the most relevant categories, as based on the object of study, and interpretation and discussion followed, according to the theoretical framework and based on the literature.
To ensure anonymity, the participants were identified with codes based on the service modality (ESF for the Family Health Strategy; CAPS I for Psychosocial Care Centre I and CAPS AD for Psychosocial Care Centre Alcohol and Drugs).
The design and conduct of the research complied with all the recommendations and ethical precepts as determined by Resolution No. 466/12 of the National Health Council and was approved by the Research Ethics Committee under opinion No. 2,420,638.
Results
Eleven professionals from the nursing team working in the three RAPS services participated in the study. Nine were female and two male; eight were over 30 years old, and working in the service between six months and 24 years, with nine working for over 2 years in the service.
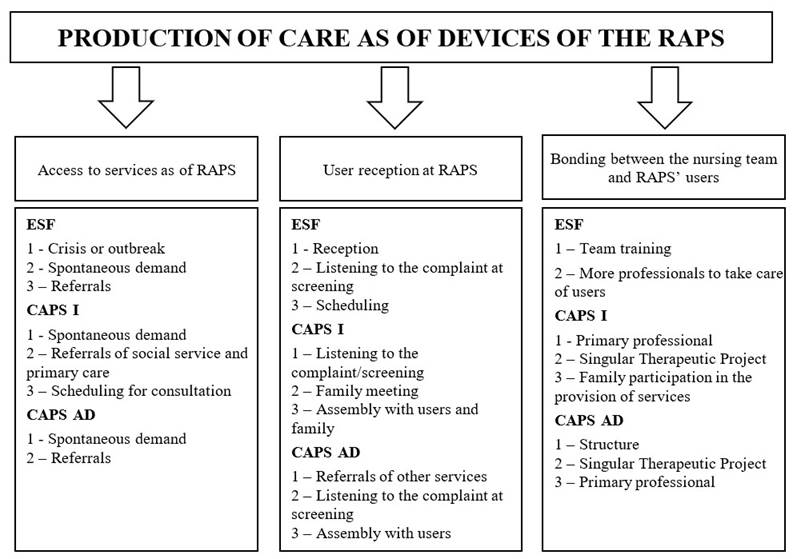
Data analysis allowed the emergence of three thematic categories seeking to represent how care is produced by the nursing team in RAPS, namely: 1) Access to services as of RAPS; 2) User reception in RAPS and 3) Bonding between the nursing team and users in RAPS, which characterize the care produced by professionals, as shown in Figure 1.
The figure represents the three thematic categories from the care production devices (access, welcoming and bonding) from the perspective of workers in the field of nursing in the three scenarios that constitute the RAPS and the path of users with severe and persistent mental disorder, in search of specific care manifested by monitoring, treatment or social reinsertion.
The categories with their respective definitions and record units are presented below, based on how care for users with mental disorders is decided, from the perspective of the nursing team.
Category 1: Access to services as of RAPS
This category includes the nursing team's understanding of how users of alcohol and other drugs access RAPS services in search of care. In the registration units presented below, it is possible to observe that the participants show access occurs by spontaneous demand, referrals made by the ESF team, or the Social Assistance Reference Centre (Portuguese acronym: CREAS).
They have access here when they are in crisis, it is very rare to schedule an appointment, we forward them to the CAPS, which monitors the patients there (ESF).
It comes referenced from CREAS and the ESF, or spontaneous demand, then we look for CAPS AD partnerships (CAPS I).
If there is a spontaneous or forwarded demand, the user will be received and attended (CAPS AD).
Access is often made by scheduling the appointment, which is carried out by professionals from each service to which the user is linked, as follows:
In some cases of urgent need, high pressure, high temperature, all of this we sort and it's scheduled right here (ESF).
Appointments with the psychiatrist are made on Tuesdays and Wednesdays in the morning, screening is done on Monday, Tuesday and Wednesday afternoon. It is important to remember that these appointments are for our demand, not for outpatients (CAPS I).
We work with an appointment, if he arrives here and the family says he is not well, that the medication is not having the expected effect, he is attended (CAPS AD).
Crisis cases, a characteristic condition that make users seek RAPS, occur punctually, as can be seen in the registration units highlighted below:
When they arrive here in crisis, they are medicated and later released and instructed to seek the CAPS (ESF).
If they are not our patients, we provide the first service, medicate and request the Mobile Emergency Care Service (SAMU) to take them to the hospital (CAPS I).
Category 2 - User reception at RAPS
The reception, for those study participants who do not work at CAPS AD, is configured from a unidirectional flow and guided by spontaneous demand. The registration units provide a description of these professionals’ understanding regarding care in directing the reception of users of alcohol and other drugs.
When they need this service, they will be directed to the reception, where they will be listened to and then to screening and to the service (ESF).
We listen and try to know what he wants, if he needs something, what he needs at the moment, in the screening, and then we forward it (CAPS I).
The first contact is at the reception, they make the form, I receive them and then I refer them (ESF).
A notable difference occurs in the way workers at CAPS AD communicate with the patient at reception, this involves active listening and interdisciplinary actions:
He arrives, the reception receives him and forwards him to me (nurse), I reception him, listen to his problem and triage the patient, I then forward it to the doctor, if he needs to be seen on the same day I forward it to her, otherwise we'll make an appointment (CAPS AD).
The patient will arrive, be received, we will sit down with him and the family and listen to what led him to seek the service (CAPS AD).
It is observed that the strategies used for reception users in the context of the ESF, do not present user reception in an integrative perspective within the guidelines of the mental health policy and the RAPS itself. As for the CAPS AD professionals, despite recognizing the possibility of reception strategies, such as family meetings and assemblies, it is observed that these are not put into practice.
There is no, as there were groups from the programs before, these activities should be done at CAPS here, there is no (ESF).
Meeting with the family that takes place once a week and the meeting that takes place every 15 days with users and with the family, but it is not taking place at this frequency (CAPS I).
In meetings and assemblies, we also listen to the family, then we sit down with the team to take better care of them, but now it hasn't happened (family meetings: although these meetings with family should happen, they are not actually occurring) (CAPS AD).
Category 3 -Bonding between the Nursing Team and RAPS’ users
This category points to the main characteristics regarding creating bonding between the nursing team and users of alcohol and other drugs in RAPS. It should be considered that this bonding makes the provision of care possible.
It is a relationship of trust between us and the users, they are at ease when they trust (ESF).
Being closer to them, creating bonds of affection, attention, care (CAPS I).
Listen carefully and try to understand your need so that he trusts you (professional) always more, gives attention (CAPS AD).
Therefore, the link can be created from a primary professional in the team with whom the user can better identify and establish a relationship.
All are primary professional, but there is always a specific one (CAPS I).
Everyone is someone's primary professional, that patient who is closer, so we will look for the professional that the patient is more open to (CAPS AD).
However, for some participants in this study, the service nurse is considered to be the primary professional. This characterizes transfer of responsibility and denies the possibility of other team members taking on the role of primary professional, as can be seen in the registration units presented below:
Here at the unit, there is no (primary professional), there is a psychiatrist, nurse, psychologist at the CAPS, a whole team (ESF).
Yes, the primary professional in this case are the nurses, mainly the coordinator (CAPS I).
There is no primary professional, we are few here, there is no way (ESF).
When asked about bond establishment and how this is made, it would appear there is a development of the Singular Therapeutic Project, (Portuguese acronym: PTS) and this has been the most used strategy by CAPS workers.
The team talks and evaluates a therapeutic plan according to the needs of each one, but we have not been able to do it yet (CAPS AD).
With the family, with the user and with the professional, we bring together the nurses, psychologists, social workers and schedule a day and the family comes with the user and on top of his diagnosis we build the therapeutic project (CAPS I).
After receiving the user, the reception and screening are carried out, then the professionals sit down and then a therapeutic plan is made (CAPS AD).
This strategy is unknown to those who work outside and beyond the CAPS, these workers claim they do not know about the PTS. These are comments from the ESF worker registration units:
Therapeutic project? I don't know, I think whoever could tell you is the coordinator. I don't know (ESF).
We don't have it. I don't know how it's done (ESF).
We do not work with PTS, there is no way, it must be done in CAPS (ESF).
Discussion
Brazilian Psychiatric Reform commenced in the 1960s, and strategies have been sought to produce care for people with mental disorders that go beyond the asylum and an oppressive dimension. There has been a rethinking of mental care into a more dynamic system that involves teaching, meeting, and discussion with patients, and understanding and respect for the subjective creation of the social reality of the person, so that 15 individual characteristics can be considered and be fundamental in the direction of care. Therefore, it is vital to understand the patient as being important, and to respect their autonomy, and thus enabling their health needs from a perspective of completeness and complexity. 16
To meet these needs (in the scenario of Brazilian public policies), Presidential Decree No. 7508/11 regulates the Organic Law of the Unified Health System (Portuguese acronym: SUS) (Law No. 8080/90). This law officially recognizes primary care as a gateway for services, and bringing improvements related to resoluteness which are based on the needs of the population, qualifying access, and the creation of efficient care. 17 The ESF and CAPS are services that do not require referrals but must ensure comprehensive care regardless of the level of complexity of the service.
However, it should be noted that the users' itinerary does not lead to the production of care that respects the principles of universality, equity and integrality.
The first category, which deals with access to RAPS services, already demonstrates difficulty in the direction of care since it involves problems in accessing the health service, this condition is exacerbated in non-specialized services such as the ESF. A study carried out on the practices of the ESF as a gateway and access for users to specialized service shows that, despite promoting the expansion of care at the basic level, the strategy does not ensure complex and comprehensive access, thus interrupting the continuity of care and the connection between the different services. 18
As shown in the results of the present study carried out directly with professionals from the nursing team, another study carried out with managers 19 shows, (from another perspective), that the nursing team, when referring the user, understands such action as a way of ensuring access to RAPS and considers its role as part of the network to be achieved. However, this care does not reach its comprehensive goal and is fragmented. Therefore, it is understood there is a need for better articulation between the ESF and specialized psychosocial care services, seeking a new structure for the CAPS and its participatory integration with primary care services.
A study carried out on the experiences of crack users and their dialogue with the clinic reaffirms the difficulty that users must access services, thus preventing them from gaining adequate care. 3 The practice of the health teams is still historically based on the logic of productivity and guided by the performance of procedures and access criteria which are based on actions created for a specific population or user’s crisis. These actions create a productivist practice, which is contrary to the principles of comprehensiveness and complexity inherent to care.
There is a greater vulnerability in the lives of those who become or are users of alcohol and other drugs, but important social determinants are often disregarded. A study carried out with students from a Public University in Colombia concluded that most of its participants had social inequalities, making them vulnerable and exposed to stressful situations, which are common starting points for the abuse of substances such as alcohol and other drugs. 19
Thus, public policies that consider the social determinants for discussions about the production of care for users of psychosocial care services are very important. In the territories in Brazil, the Primary Health Care is responsible for monitoring cases and actions to reduce drug and alcohol abuse and its consequent damage. However, there is still a flaw in the care process when health workers say they do not know what to do with these users, and their intervention is limited to referring them to the CAPS-AD. 3) Such ignorance is also evidenced in the understanding of the participants in this study.
The second category of the study deals with the reception of users in RAPS. Here the results show that the professionals of the nursing team do not know how to conduct monitoring of the user and focus on the act of referring. However, it was observed in this research that this nursing team has concerns about letting the user leave the service without listening to them. This allows us to infer that from the perspective of reception, there is an attempt to produce some care of sorts.
Studies 16 recognize that the creation of care through support is important. This concerns the attitude in which the user is approached, considering their social role as a citizen with rights and duties, and treating them as the protagonist of their care process and not as a passive being.
The act of listening contributes to the creation of care, it is based on the individual, and forms understanding and communication between users and health workers. In this there is the possibility that the user can play an active role in improving their health. 20
With further regard to user support, a survey 18 evaluated the way in which reception is conducted in specialized services, and how it was made possible to verify a practice based on an ethical and humanistic behavior, one in favor of a relationship of trust, listening, and commitment to users, their family members and other health professionals. This was guided by a culture of harmony and legitimized by the structuring principles of the SUS.
It is noteworthy that the results of this study show that participants working in CAPS use the reception environment because it is a tool that produces comprehensive and resolute care, however those who work in the ESF understand that despite the importance of reception, users must be referred to specialized services, thus demonstrating that there is a lack of qualification to perform extramural care in specialized units. Thus, it is worth considering the need for qualification of ESF’ professionals with knowledge about psychosocial care, so that they can resolve the health needs of users of alcohol and other drugs.
It is important to emphasize that access crosses over different health care practices, in an itinerary that goes from the “entrance door of Brazil's National Health System (SUS)”, to the different types of care inherent within RAPS. Thus, professionals working in the network should not simply focus upon receiving the user and referring him to another service, but also seek to listen, guide and plan assistance that meets their real needs in any RAPS service. 2
This situation should prevail throughout the network and not just at some areas. This is evidenced in the results that when it comes to a specialized unit such as CAPS AD, it is clear the direction of care should entail active listening, this takes care of the needs and (attempts to meet) the user’s demands, although at times they must resort to secondary care devices, such as the hospital.
Shared care between the ESF and the CAPS still presents a challenge. A study 16 that sought to analyze the bond-responsibility of the ESF teams, points out that the bond is often not established, due to teams' lack of interest and theoretical appropriation in discussing those cases that require mental health care within the territory.
A systematic review study 21 indicates that the ESF goes beyond being the entrance door to RAPS but represents the user's first contact with the health system, since it is the most appropriate environment for instituting educational and preventive measures.
Thus, as an intervention strategy we can highlight the use of succinct and short-term therapeutic techniques, such as the "Short Intervention". This is a therapeutic technique aimed at changing conduct, seeking harm reduction, and helping users to realize they are at risk, potentially becoming a motivation for them to reduce or stop consuming such substances. 22
It is then essential to guarantee such strategies are in place to welcome users, into an environment where they feel safe and confident. Thus, links can be established with health professionals and services, so that the right care is enabled to meet the user’s needs as well as their families. As for other strategies for the provision of care, we highlight the importance of the reception, the PTS, the technical reference, home visits and team meetings as tools for the creation of care for users, but these practices require a commitment from the entire team.23
We emphasize the results of this study bring as modalities of care offered in CAPS. The assemblies are a form of therapeutic resource that enable autonomy for the patient, in the search for greater participation and accountability for users in their treatment; assemblies also represent an important institutional instrument. However, in this study, some professionals reported that they knew about this type of tool, but did not put it into practice, thus neglecting a care strategy that could be used in the services.
A study 24 of theoretical reflection on therapeutic interventions using meetings as group devices (and marked in the constitution of Brazilian public policies and the CAPS), demonstrated that with the use of this device, users began to better face their imposed limits by their illness/addiction. Therefore, by emphasizing healthy aspects within the demands of daily life, the illness/addiction takes a secondary role, giving rise to the experience of empowerment, which can be therapeutic.
The use of group meetings (assemblies) can become a strategy for building bonds, if the professionals of the nursing team recognize the concept of bonding and seek to exercise it, but there is still a lack of understanding for the necessity to develop strategies for building bonds.
The third category deals with the bond between the nursing staff and RAPS users. However, professionals working in specialized services state there is little articulation between the ESF and the CAPS for the construction of shared and integral care which presents difficulties in the creation of care. CAPS professionals point out the lack of interest and theoretical appropriation of the ESF team to discuss cases that require mental health care in primary health care. Unfortunately, this favors an attitude of non-responsibility and a bond between users and staff cannot be generated. This situation was also observed in two other studies with nursing professionals on the creation of care. 25-26
Thus, for bonding to occur, it is important to have professionals trained to deal with users of alcohol and other drugs throughout RAPS, not just in specialized services. There is an assumption that this was to be initiated by the reference professional, which was not perceived in the studied scenario, either because they did not understand its relevance or because of a mistaken understanding that this role belongs only to the nurse. In effect the primary reference technician must be the one responsible for monitoring the user from a PTS (Single Therapeutic Plan). 3
Research 26 developed in a city in Northeast Brazil discussed how social subjects understand the management practices of nurses' care in the ESF and included the bonding device. The research showed the importance of actions based on a reference professional within the RAPS services and built upon the matrix support of the teams, whether at the basic or specialized level. The primary role of the reference technician is based on the preparation and practical application of the PTS, which implies a situational diagnosis, the approximation between user, family, and professionals, and resulting in individual or collective therapeutic practices, forming a generation of a bond between the team and users. This should be a common practice not only for professionals working at CAPS, but for everyone in the network.
In this scenario, the production of care by the nursing team with the user and their families can be conducted in a multidisciplinary team, which allows for the expansion of a dialogue between different social actions, and enhancing bonds, in addition to establishing responsibilities between health services and the user's network of relationships.
Thus, the PTS needs to be built together with the user as a strategy for their co-responsibility and encouragement of their autonomy, with a view to recovering citizenship, self-esteem, and contractual power, and where the life project of each user is a pillar of support.
As evidenced in the results of this study, another study 27 showed that ESF professionals are also unaware of the PTS. This is a device that needs to be disseminated beyond the psychosocial care network, considering its relevance in the care offered by the ESF, as it enables assistance in the management of care, valuing an individual’s uniqueness, considering their way of being, thinking and behavior, and thus enabling the demonstration of a scenario in which professionals can and should develop interdisciplinary care.
A systematic review in Australia developed by experts in the field, sought to synthesize the evidence regarding the strategies for comprehensive care for users of alcohol and other drugs and concluded that although health workers recognize the benefits of comprehensive care, they are still using incipient strategies to produce a biopsychosocial-spiritual care in the context of assistance to users of alcohol and other drugs. 28
Conclusion
The study showed that the production of professional care provided by the nursing staff to for users of alcohol and other drugs in the investigated RAPS takes place through access, reception and emotional bonding between the nursing team and users in RAPS, however this only occurs in specialized units and not across the entire network.
Care practices need to be better articulated between the different RAPS scenarios so that effective and quality care is produced for users and their families, and this should happen in the network as a whole and not just in specialized units. It is necessary to recognize the ESF as the gateway, in which the entire team needs to be prepared to take care of users in view of their needs, to recognize their individualities and vulnerabilities in the face of inequalities and social determinants.
This study is limited since it involved the participation of only one group of individuals, those is the nursing field. If there had been a greater interdisciplinary participation, a wider discussion from different perspectives would have been made available.
It is expected that the discussions envisioned in this research will be expanded into new studies concerning the care practices offered by professionals of the nursing staff to users of alcohol and other drugs; and further the possibilities of building new practices as well as reflect upon those that have been developed.
REFERENCES
1. Brasil. Ministério da Saúde. A Política para Atenção Integral a Usuários de Álcool e outras Drogas. Brasília: Ministério da Saúde; 2003. [ Links ]
2. Bastos FI, Vasconcellos MT, Boni RB, Reis NB, Coutinho CF. (Org). III Levantamento Nacional sobre o uso de drogas pela população brasileira. Rio de Janeiro: Fiocruz/Icict; 2017. Disponível em: https://www.arca.fiocruz.br/handle/icict/34614 [ Links ]
3. Souza MC, Afonso ML. Saberes e práticas de enfermeiros na saúde mental: desafios diante da reforma psiquiátrica. Rev. Interinst. Psicol. 2015;8(2):332-347. Disponível em: http://pepsic.bvsalud.org/pdf/gerais/v8n2/v8n2a04.pdf [ Links ]
4. Ortiz SE, Domingues EA, Prado KL, Barbosa PL. Prática de enfermagem o centro de atenção psicossocial. Rev. Bras. Enferm. 2020;73(1). Disponível em: DOI: 10.1590/0034-7167-2018-0175 [ Links ]
5. Portaria nº 3.088 de 23 de dezembro de 2011. Institui a Rede de Atenção Psicossocial para pessoas com sofrimento ou transtorno mental e com necessidades decorrentes do uso de crack, álcool e outras drogas, no âmbito do Sistema Único de Saúde (SUS). Diário Oficial da União. Brasília; 2011. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt3088_23_12_2011_rep.html. [ Links ]
6. Fernandes HN, Eslabão AD, Mauch LM, Franchini B, Coimbra VC. A práxis do cuidado em saúde mental na atenção ao uso e abuso de álcool. Cienc cuid. saúde. 2012;11(4):827-831. DOI: 10.4025/cienccuidsaude.v11i4.15407 [ Links ]
7. Sousa FD, Sousa AL. Uma revisão sobre as redes de atenção à saúde no Brasil. Revista Científica Multidisciplinar Núcleo do Conhecimento. 2018;1(11):57-75. DOI: 10.32749/nucleodoconhecimento.com.br/saude/saude-no-brasil [ Links ]
8. Terezinha ZM, Fontoura CM, Bradt FM, Ziegler HM, Godinho BK. Percepção dos trabalhadores de saúde sobre o cuidado as pessoas com crise a rede de atenção psicossocial. Esc. Ana Nery. 2016;20(3):e20160059. DOI: 10.5935/1414-8145.20160059 [ Links ]
9. Varela DS, Sales IM, Dantas FM, Monteiro CF. Rede de saúde no atendimento ao usuário de álcool, crack e outras drogas. Esc Ana Nery. 2016;20(2):296-302. DOI: 10.5935/1414-8145.20160040 [ Links ]
10. Franco TE, Merhy EE. Trabalho, produção do cuidado e subjetividade em saúde. São Paulo: Hucitec; 2013. [ Links ]
11. Feuerwerker LCM. Micropolítica e saúde: produção do cuidado, gestão e formação. Porto Alegre: Rede UNIDA; 2014. [ Links ]
12. Minayo MC. O desafio do conhecimento: pesquisa qualitativa em Saúde. 12. ed. São Paulo: Hucitec ; 2014. [ Links ]
13. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32- item checklist for interviews and focus group. Int J Qual Heal Care. 2007;19(6):349-57. Disponível em: https://academic.oup.com/intqhc/article/19/6/349/1791966 [ Links ]
14. Bardin L. Análise de conteúdo. São Paulo: Edições 70; 2016. [ Links ]
15. Amorim RG, Lavrador MCC. A Perspectiva da Produção de Cuidado pelos Trabalhadores de Saúde Mental. Psicologia Ciência e Profissão. 2017;37(2):273-288. Disponível em: https://www.scielo.br/pdf/pcp/v37n2/1982-3703-pcp-37-2-0273.pdf [ Links ]
16. Subrinho LQ, Sena EL, Santos VT, Carvalho PA. Cuidado ao consumidor de drogas: percepção de enfermeiros da estratégia de saúde da família. Saúde Soc. 2018;27(3):834-844. DOI: 10.1590/s0104-12902018180079 [ Links ]
17. Decreto nº 7.508 de 28/2011. Dispõe sobre a organização do Sistema Único de Saúde, o planejamento da saúde, a assistência à saúde e a articulação Inter federativa e dá outras providências (Internet) Diário Oficial da União. Brasília; 2011. Disponível em: http://www.planalto.gov.br/ccivil_03/_ato2011-2014/2011/decreto/d7508.htm [ Links ]
18. Souza AC, Amarante PD, Abrahão AL. Inclusão da saúde mental na atenção básica à saúde: estratégia de cuidado no território. Rev Bras Enferm. 2019;72(6):1677-1683. DOI: 10.1590/0034-7167-2018-0806 [ Links ]
19. Narváez NEB, Rivero MO, Guerra EH. Social determinants in the consumption of psychoactive substances in university students in 2016. Enfermería (Montevideo). 2018;7(2):12-35. Disponível em:http://www.scielo.edu.uy/pdf/ech/v7n2/en_2393-6606-ech-7-02-12.pdf [ Links ]
20. Agonigi RC, Carvalho SM, Freire MAM, Gonçalves LF. The production of care in the routine of Family Health Teams. Rev. Bras. Enferm. 2018;71(Suppl 6):2659-2665. Disponível em: https://www.scielo.br/pdf/reben/v71s6/0034-7167-reben-71-s6-2659.pdf [ Links ]
21. Pereira MO, Anginoni BM, Ferreira NC, Oliveira MAF, Vargas D, Colvero LA. Efetividade da intervenção breve para o uso abusivo de álcool na atenção primária: revisão sistemática. Rev. Bras. Enferm. 2013; 66(3):420-428. Disponível em: https://www.scielo.br/pdf/reben/v66n3/a18v66n3.pdf [ Links ]
22. Abreu AMM, Jomar RT, Taets GGC, Souza MHN, Fernandes DB. Screening and Brief Intervention for the use of alcohol and other drugs. Rev. Bras. Enferm. 2018;71(Suppl 5):2258-2263. Disponível em: https://www.scielo.br/pdf/reben/v71s5/0034-7167-reben-71-s5-2258.pdf [ Links ]
23. Amorim AC, Assis MM, Santos AM. Vínculo e responsabilização como dispositivos para produção do cuidado na estratégia de saúde da família. Rev. baiana saúde pública. 2014;38(3):539-554. DOI: 10.5327/Z0100-0233-2014380300004 [ Links ]
24. Junqueira AM, Carniel IC, Montovani A. As assembleias como possibilidade de cuidado em saúde mental em um CAPS. Rev. Nesme 2015;12(1):31-40. Disponível em: http://pepsic.bvsalud.org/pdf/vinculo/v12n1/v12n1a06.pdf [ Links ]
25. Ferreira TP, Sampaio J, Souza AC, Oliveira DL, Gomes LB. Produção do cuidado em Saúde Mental: desafios para além dos muros institucionais. Interface. 2017;21(61):373-84. DOI: 10.1590/1807-57622016.0139. [ Links ]
26. Silva SS, Assis MM, Santos AM. Enfermeira como protagonista do gerenciamento do cuidado na estratégia saúde da família: diferentes olhares analisadores. Texto Contexto Enferm. 2017;26(3):e1090016. DOI: 10.1590/0104-07072017001090016. [ Links ]
27. Silva AI, Loccioni MF, Orlandini RF, Rodrigues J, Peres GM, Maftum MA. Projeto Terapêutico Singular para profissionais da estratégia de saúde da família. Cogitare Enferm. 2016;21(3):01-08. DOI: 10.5380/ce.v21i3.45437 [ Links ]
28. Savic M, Best D, Manning V, Lubman DI. Strategies to facilitate integrated care for people with alcohol and other drug problems: a systematic review. Subst Abuse Treat Prev Policy. 2017;12(19):1-12. DOI: 10.1186/s13011-017-0104-7 [ Links ]
How to cite: De Brito PMC, Alves MB, Oliveira VM, Nóbrega MdPSdS, Baptista SCO, Da Silva RS. Users of Alcohol and other Drugs in the Psychosocial Care Network: Nursing Care. Enfermería: Cuidados Humanizados. 2021;10(2):175-190. DOI: 10.22235/ech.v10i2.2546
Contribution of the authors: a) Study conception and design, b) Data acquisition, c) Data analysis and interpretation, d) Writing of the manuscript, e) Critical review of the manuscript. P. M. C. d. B. has contributed in a, b, c, d, e; M. B. A. in c, d, e; V. M. O. in d, e; M. d. P. S. d. S. N. in d, e; S. C. O. P. in d, e; R. S. D. S. in c, d, e.
Received: April 17, 2021; Accepted: October 29, 2021










 text in
text in