Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.10 no.2 Montevideo 2021 Epub Dec 01, 2021
https://doi.org/10.22235/ech.v10i2.2603
Original Articles
Influence of Self-efficacy on Uncertainty and Quality of Life of Women with Breast Cancer. Integrative Review
1 Universidad Central del Ecuador
2 Universidad de Concepción, Chile, osanhue@udec.cl
Keywords: self-efficacy; uncertainty; quality of life; breast cancer.
Palabras clave: autoeficacia; incertidumbre; calidad de vida; cáncer de mama.
Palavras-chave: autoeficácia; incerteza; qualidade de vida; câncer de mama.
Introduction
The demographic, epidemiological, and environmental transformations that society has been experimenting have brought about significant changes, mainly in the health-disease process of the populations. (1) Aging, population growth, and adopting harmful habits have increased the incidence of malignant, non-transmissible chronic diseases. 2,3 In this scenario, cancer constitutes one of the main challenges for healthcare systems around the world, given its high mortality rate and the impact it has on individual, family, and social levels. 4
Among the different types of cancer, breast cancer is of special concern due to its high prevalence and incidence in the world’s female population.5 The latest estimates published in 2020 by the International Agency for Research on Cancer reported 2,261,419 new cases and 684,996 deaths caused by this disease.6 In Latin America and the Caribbean there has been an increase in breast cancer with 462,000 new cases and close to 100,000 deaths. 7
In this context, breast cancer constitutes a global public health problem that has a major impact on women, their families and healthcare systems, given that it is a silent, complex, and extremely harmful disease.8 As a consequence, screening methods for early diagnosis and treatment are decisive in reducing this disease’s mortality, achieving a higher survival rate,8 promoting early psychosocial adaptation and improving the quality of life of affected women.9
Nowadays, a wide range of simple and combined cancer treatments are available that offer higher chances of recovery. However, these treatments cause multiple side effects that deteriorate body image, functional capacity, psychological state and social relationships, affecting the well-being of women and their families. 10
Although the prognosis and survival rate of women with breast cancer has dramatically improved in recent years, affected women experience problems in multiple aspects of their lives. 11 The psychological impact generated by the diagnosis, treatment, and survival stages negatively impact women’s lives, given that they create uncertainty, anxiety, fear of death, loneliness, depression, pain, suffering throughout the disease process, feelings of loss of control over their lives, and gradual loss of self-esteem and their personal coping resources. 10-12
These feelings and perceptions are associated with diagnosis, the lack of knowledge of the disease process, treatments and uncertainty about the future. 12) Uncertainty has been identified as a factor that causes high levels of psychological stress, and it is regarded as the most influential variable during the process of adaptation to the disease, 14 generating ambiguities that hinder the understanding of the disease and its treatment, which can have an impact on the timely initiation of treatment, the degree of adherence to treatment and the patient’s adaptation to their new health condition. 3
Health-related quality of life (HRQoL) is regarded by multiple authors as a multidimensional and dynamic concept. (15, 16) Shumaker and Naughton (1995) defined HRQoL as “the subjective assessment of the influence of current health status, and health care on the individual´s ability to maintain a level of functioning and their general well-being. Where social, physical and cognitive functioning; mobility and self-care; and emotional well-being converge”. 15 It is thus deduced that the quality of life of women with breast cancer is greatly affected not only in physical aspects, but also in psychological, social, and spiritual factors due to the changes in their physical image which deteriorate their self-esteem, self-management skills, feelings, attitudes, mood and social relationships, 17 all of which affect their psyche. 18
Quality of life has become a necessary criterion within oncological care for breast cancer, as it should lead to an improvement in the overall well-being of affected women. In this regard, one of the variables that has shown a positive influence on the well-being of people with chronic diseases is self-efficacy, 19 which plays a mediating role between personal skills and human behavior, which determines their motivation and well-being. 20
The construct of self-efficacy was introduced by Bandura (1977) as a key point of the Social Cognitive Theory, acknowledging that individuals possess a self-system that allows them to control their thoughts, feelings, emotions and regulate their behavior in potentially stressful situations. 21 Among women with breast cancer, self-efficacy is regarded as an essential abilityin order to cope with the difficulties, high levels of stress, anxiety, uncertainty, and depression associated with the disease process and its treatments, 22 enhancing a series of strategies such as having a positive mindset and a fighting spirit, which in turn, lead to a better quality of life.23
Consequently, to inquire about the possible intervention of self-efficacy to improve quality of life and reduce uncertainty, would allow to explore in greater depth the impact of these variables on the experience of women with breast cancer, which could contribute with various orientations to the health team, for the design of future care interventions with a holistic approach, focused on the development of coping strategies that facilitate the process of adaptation to the disease. 24 In addition to contributing evidence to healthcare practice in the field of nursing care.
Therefore, the objective of this study is to determine the influence self-efficacy has on uncertainty and quality of life of women with breast cancer through the review of published scientific literature, which will identify the care needs of affected women. Moreover, this study aims to be a contribution to clinical practice and to disciplinary knowledge in the area, allowing healthcare and nursing professionals to apply the existing knowledge and evidence to promote the implementation of interventions that help to improve the quality of life of the women affected by this disease and their families.
Materials and method
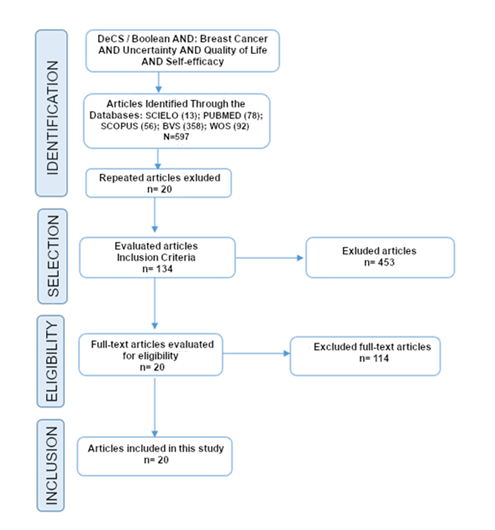
This review is carried out in the context of Evidence-Based Nursing, which promotes the application of research findings in clinical nursing practice as a key element to achieve a higher quality of care. 25 This research followed the methodology for integrative reviews proposed by Mendes et al., 26 which allows to gather the best evidence in the selected field of study, whose stages are: definition of the problem and formulation of the review question, establishment of inclusion and exclusion criteria for the studies, search identification of the relevant studies in the scientific databases, selection and categorization of studies, evaluation of the studies included in the review, interpretation of results and synthesis of knowledge. In addition, PRISMA quality criteria for integrative reviews were considered.27
The PIO strategy 25 was used to formulate the question guiding this study, which was defined as follows: What influence does self-efficacy have on uncertainty and quality of life of women with breast cancer?
A review of the scientific literature was conducted to answer the question posed using the databases: Scielo, Pubmed, Scopus, Bvs and Medline and Web of Science. The following DeCS and MeSH descriptors were considered: “breast cancer”, “uncertainty”, “quality of life” and “self-efficacy” in Spanish, English, and Portuguese. Finally, the research was carried out using a combination of the descriptors “cáncer de mama AND incertidumbre”, “cáncer de mama AND calidad de vida” and “cáncer de mama AND autoeficacia”, in Spanish; “breast cancer and uncertainty”, “breast cancer and quality of life”, “breast cancer and self-efficacy”, in English, conjugated using the Boolean Operator AND due to the characteristics of this research study.
The inclusion criteria allowed for public access primary quantitative research studies published in English, Spanish and Portuguese between 2015 and 2020 who preferably had a nurse as first or corresponding author, to enhance the development of Nursing care; and whose sample included women with a breast cancer diagnosis. The exclusion criteria included secondary studies such as meta-analyses, systematic reviews, integrative reviews, and studies whose full texts were not available online.
Initially, 134 articles were identified, 20 of which met the inclusion criteria. Quality assessment was carried out using the Effective Public Health Practice Project (EPHPP) tool, which assesses the risk of bias and classifies the methodological quality of the studies into low, moderate, and strong. 28
Finally, a critical reading was carried out to assess the validity, reliability, relevance, and pertinence of the selected articles. The review complied with the ethical principles by respecting copyrights, using proper citation, and crediting the reviewed authors. Figure 1
Results
With a baseline of 20 articles that addressed the subject and met the proposed criteria, we proceeded to synthesize and analyze them. The articles that make up the corpus of analysis are presented in Table 1 and are arranged according to the relationship between the studied variables.
Table 1: Results of the influence of self-efficacy on uncertainty and quality of life of women with breast cancer according to the selected articles
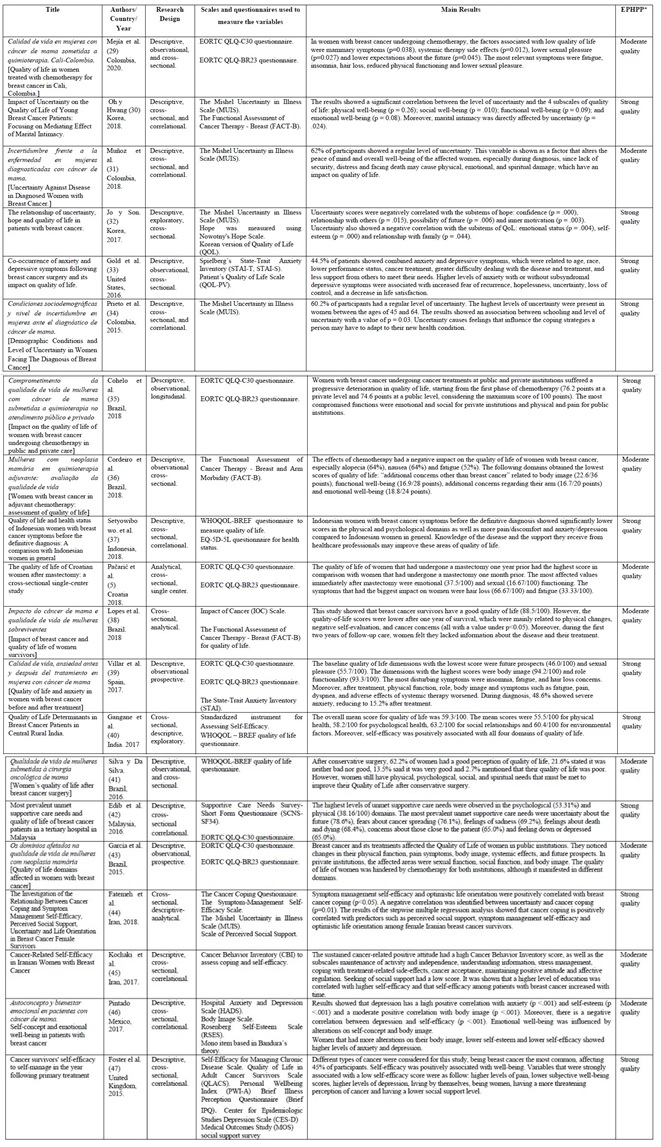
Source: Own elaboration (2021).
The time frame considered for the article search was 5 years, finding one article published in 2020; 29 nine in 2018;5,30,31,35-37,38,44 four in 2017; 32,39,40,45,46 and three in 2016 (33,41,42 and 2015. 34,43,47 Regarding the research design, 100% of the studies had a quantitative approach, 84.2% were cross-sectional and 15.3% were longitudinal. Eight were correlational studies;30,31,34,37,42,45-47 seven were observational;29,33,35,36,39,41,43 three were analytical 5,38,44 and two were exploratory. 32,40 Considering the EPHPP scores,28 nine articles had moderate quality5,29,31,36,38,41,43,45,46 and eleven reached a strong quality. 30,32-35,37,39,40,42,44,47
Regarding the geographical area of the selected studies, seven took place in Asia; 30,32,37,40,42,44,45 ten in the Americas 29,31,33-36,38,41,43,46) and three in Europe, 5,39,47 evidencing that the majority were carried out in the Americas. 25% of them took place in Brazil, 35,36,38,41,43 15% in Colombia, 29,31,34 10% in Iran 44,45 and Korea 30,32 and 5% were carried out in the United States, 33 Croatia, 5 Indonesia, 37 Spain, (39) Malaysia, 42 Mexico 46 and the United Kingdom. 47 The studies were published in English (10= 52.6%), Portuguese (5= 26.3%) and Spanish (4= 21%).
The articles made use of a wide variety of scales and questionnaires to collect data in accordance with the objectives of each study, as shown in Table 2.
Table 2: Main Self-Efficacy, Uncertainty and Quality of Life Scales used in the reviewed studies
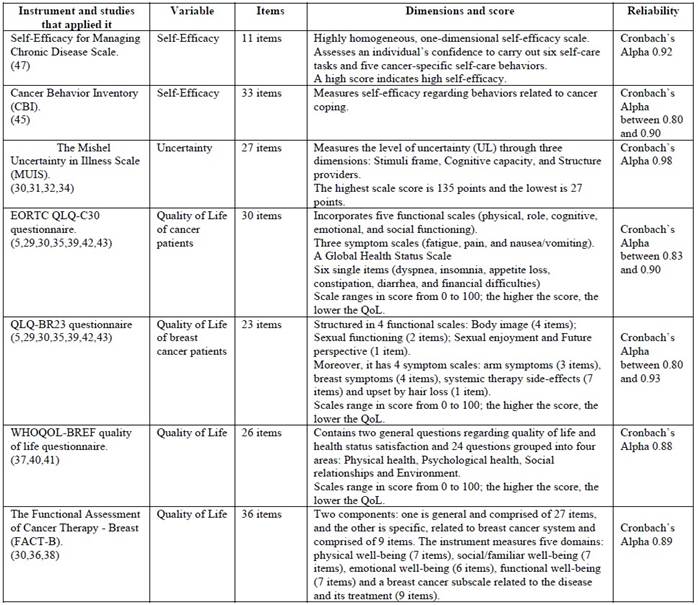
Source: Own elaboration (2021).
The most significant contribution of these studies is the description of each variable in relation to breast cancer and the influence that may exist between them, which shows the priorities that need to be addressed in healthcare, an example of this are the deterioration in Quality of life of women due to breast cancer and its treatments 5,32,35,36,39, uncertainty as a psychological stressor that affects quality of life30,31,34,40) and Self-efficacy as a facilitating factor for well-being and coping. 45-47
Deterioration of women’s quality of life due to breast cancer and its treatments
Regarding quality of life and well-being in breast cancer patients, it has been shown that women experience physical and psychological alterations to a greater extent; 39,32 overall quality of life deteriorates due to cancer treatments, 5,35,36,39 changes in body image and degree of functionality, (33, 36) and uncertainty regarding the therapeutic approach, fear of death and future expectations. 31,32,37
Studies show that overall quality of life of women with breast cancer obtained low scores,38,40 as women experience multiple changes that may lead to a loss of balance between the physical, emotional, and social functions.(32, 36, 37, 39) Moreover, the domains of quality of life that are most affected by the disease are the psychological, 37,39 social 32 and functional, especially sexual, dimensions. 5,29,38 It has also been shown that certain psychological determinants may affect the quality of life and well-being of affected women 33,37 such as anxiety, self-esteem, positive thoughts, and uncertainty30,31 as well as socioeconomic factors such as level of education, age, income, marital status, and perceived social support. 34
Women’s physical domain is affected by prolonged treatments that are exhausting, which cause countless side-effects such as nausea, vomiting, dizziness, fatigue, alopecia, insomnia,29,36 changes in body image and significant functional limitations.5,35,39 Negative changes should be highlighted regarding sexuality, mainly in young women, as a result of the impact of cancer treatments and specially chemotherapy, which cause exhaustion, low self-esteem due to altered body image, fear of rejection by their partner due to loss of femininity, low levels of sexual hormones and decrease in sexual desire. 36,40
Studies show that most of the unmet needs that alter the quality of life of women with breast cancer are psychosocial, which could aggravate their physical symptoms, 42 and affect their family life. Moreover, women with this diagnosis have higher levels of anxiety with or without depressive symptoms, which are associated with a higher fear of recurrence of the disease, hopelessness toward the future, uncertainty due to the disease, loss of control over their lives and a decrease in life satisfaction. 33 Furthermore, the physical, emotional, and spiritual effects of the disease alter the well-being and peace of mind of women due to lack of security, distress, and fear of facing death, which may accelerate the development of the disease or create different pathologies, compromising their quality of life 30,31
Another key aspect of living with breast cancer that is worth mentioning, is the personal and family burden caused by this disease. 32,33 Relevant concerns for women are family unbalance and restructuring due to the disease, requiring care or support from their spouse or close relative in moments of crisis, and fear of the family future due to the constant threat of death and loss of functionality.31 Fear of damaging their marital relationship or estrangement from their partner, 35,40) due to the lack or decrease in sexual activity are relevant factors to consider, especially in patients who have undergone total or partial mastectomies. 30
Uncertainty as a psychological stressor that affects quality of life
Uncertainty in the face of the disease has proved to be a psychological stressor that deteriorates peace of mind (31,42 and affects the four domains of quality of life, mainly the psychological domain, directly related to depression.30-32 The uncertainty that develops after being faced with a diagnosis may lead to significant emotional alterations for affected women and their families, given that it creates high levels of stress, distress, anxiety, depression, and hopelessness. 31 Moreover, uncertainty negatively affects quality of life, healthcare satisfaction and self-care. 30
Uncertainty also proved to be a cognitive factor that accompanies women and their families throughout the development of the disease, as living with a chronic disease such as breast cancer means living with a constant feeling of lack of security and worry in some women.31) After a diagnosis confirmation, women experience fear of death, feelings of doubt toward the future, anxiety, confusion, desperation, hopelessness, and worry regarding the disease and their own and their family’s future. 31,32 From the moment of diagnosis, women’s lives change and are restructured, which leads to a deep emotional crisis that damages their psychological well-being.
Furthermore, uncertainty is regarded as a stressor that damages the peace of mind and overall well-being of the affected women, given that they perceive the disease to be an obstacle to beat in order to continue with their life project, being influenced by low level of education, age, low financial resources, and cultural factors. 31 Women have higher uncertainty when faced with the disease prognosis and complexity of the treatment if they have a low education level and lack information. 34
At the same time, uncertainty increases in patients with a low socioeconomic level, because this condition can be a determinant factor in the access to healthcare services and delays in treatment initiation, which contributes to the increase of uncertainty in the disease and generates a discomfort derived from the inability to determine the meaning of the facts that damages the well-being of the sick women. 30,34,40)
Self-efficacy as a facilitating factor for well-being and coping
During the breast cancer process, women suffer from high levels of stress, anxiety, uncertainty, and distress, 34 in addition to physical pain, functional limitations, and lower self-esteem, which alter their well-being and lower their self-efficacy. 47 Similarly, women who experience changes in body image because of cancer treatments have higher levels of anxiety and depression, which lower self-efficacy and self-concept. 46 Ongoing uncertainty, prolonged medical treatments, and constant fear of death, 31) make it difficult for women to maintain a high level of self-efficacy. 19
However, studies show that self-efficacy is positively related to quality of life of people with chronic diseases; social support and optimism are also linked with a higher level of self-efficacy and psychological well-being. 44,45 There is a positive correlation between self-efficacy and quality of life 40 well-being and coping,44,45,47 given that self-efficacy would condition the personal mechanisms that ease the adaptation to their new health condition. (44
Self-efficacy in managing symptoms and optimism toward life are positively correlated with coping in breast cancer patients, 44 and a maintained positive attitude is related to a high level of behavior against cancer.47 Furthermore, research showed that a high level of education is related to higher self-efficacy and that self-efficacy in patients grows over time. 45
Moreover, there is a negative correlation between uncertainty and the 7 subscales of the Cancer Behavior Inventory (CBI): maintaining activity and independence, seeking and understanding medical information, stress management, coping with treatment-related side-effects, accepting cancer and maintaining a positive attitude, affective regulation and seeking support. 45 Low socioeconomic levels,45,47 lack of knowledge of the disease, 38 being a woman and having less social support 46,47) were among the determinant factors of low self-efficacy levels.
Discussion
The study of health-related quality of life of women with breast cancer continues to be a challenge for healthcare professionals, especially in nursing, due to its high complexity and that, in fact, the quality of life is a result of the interaction of women and their families with the disease, its evolution, cancer treatments and their side-effects, as well as the changes produced in their physical, psychological, and social domains due to the disease. Even so, studying the quality of life of patients with breast cancer has enabled a shift from the traditional concept of health and purely physical well-being into a more comprehensive concept of well-being. 49
The analysis of the obtained results clearly evidences that women with a breast cancer diagnosis undergo multiple changes in their clinical, psychological, family, social, functional, sexual, and work spheres that negatively impact their quality of life. 5,29,37,39) The affected women have low levels of overall quality of life, 40 due to the alterations arising from the disease and its treatments, which cause a loss of balance between the physical, emotional, and social functions. As a result, the study of psychological, social, and spiritual aspects has become more relevant in recent years, as they offer a more comprehensive approach, which is necessary in the field of nursing in relation to quality of life. 50
Women and their families who must coexist with breast cancer feel lack of security, fear and uncertainty regarding future prospects and require the influence of a constant positive attitude as a predictor of a better understanding of the disease and managing stress, anxiety, and depression; this motivational support and assistance to maintain a positive attitude may be given and stimulated by the healthcare team, especially by nurses caring for patients in oncology units supported by the interdisciplinary team that treats women, facilitating the development of coping strategies that allow affected women to adapt to their new health condition. 45 As a consequence, self-efficacy is regarded as an important predictor that influences women’s behavior against breast cancer and constitutes a facilitating factor for well-being, as shown by the obtained results.
The reviewed studies placed uncertainty as a variable that generated high levels of stress, distress, anxiety, depression, and hopelessness, all of which negatively affect the quality of life of women with breast cancer and their families, their level of satisfaction with healthcare services and self-efficacy. 30 These situations make women feel unable to confront the disease and its challenges. Therefore, care strategies targeted toward women with breast cancer should incorporate clinical and psychological elements and the perspective of the affected patients, thus having a more meaningful impact on their well-being and quality of life.
Uncertainty is a cognitive factor that accompanies women and their families throughout the development of the disease, as living with a chronic disease such as breast cancer means living with a constant feeling of worry and lack of security. 31 Lack of information may lead to uncertainty 38 and it may also create a feeling of discomfort due to the patient’s inability to determine the meaning of the facts; a subjective interpretation of their disease puts them in an unfavorable position that may alter their psychological well-being and responsiveness.
A revealing fact is that uncertainty increases in patients with a low socioeconomic level,34 which could be a determinant factor derived from difficult access to healthcare services, delays in the initiation of treatment and needing to fulfill a great number of requirements.
Women’s self-esteem is damaged during the course of the disease, altering their well-being and damaging their self-efficacy.46 After suffering changes in their body image due to cancer treatments, women show higher levels of anxiety and depression, which could lead to lower self-efficacy and self-concept. Studies show a negative linear relationship between self-efficacy and uncertainty in the face of the disease, given that uncertainty may create emotional discomfort, increase difficulty to predict symptoms, a gradual loss of motivation and a lower coping capacity, 51 which negatively relate to quality of life and well-being.
Although scientific literature shows little evidence regarding the influence of self-efficacy on quality of life and uncertainty in women with breast cancer, it was determined that self-efficacy regarding symptom management and an optimistic outlook on life were positively correlated with coping with breast cancer. Furthermore, there is a significant negative correlation between uncertainty and maintenance of activity and independence, seeking and understanding medical information, stress management, coping with treatment-related side-effects, accepting cancer and maintaining a positive attitude, affective regulation and seeking support. Maintaining a positive attitude is related to higher levels of behavior against cancer and a high level of education is related to higher levels of self-efficacy.
In view of this, it is deeply important in nursing to achieve a holistic approach regarding oncological care, as it highlights the need to design care interventions that incorporate biological, psychological, emotional, spiritual, and social factors, also to identify the sociocultural determinants of each context due to the nature of the recipient of nursing care: the human being. This should be done so that the diverse care, help and support needs of women with breast cancer can be met.
Conclusions
As an answer for the objective, it was determined that self-efficacy is a predictor of a better quality of life in women with breast cancer, given that self-efficacy has a positive relationship with well-being and the development of disease coping strategies. Uncertainty proved to be a psychological stressor that damages the overall well-being of affected women, and it negatively influences the psychological, functional, social, and physical domains. However, this variable may be mediated by enhancing self-efficacy as a powerful cognitive factor that has an effect on behavior and responsiveness to existential crisis created by the disease and its treatments.
The quality of the information provided by the healthcare team, especially by nurses, represents a key point in the care of sick women and their families. Uncertainty rises if the information is ambiguous, so nursing care calls for the development of relevant, empathetic, sensitive, and humane educational programs. In this regard, it is recommended that nurses carry out care interventions starting from the moment of diagnosis and throughout the course of the disease in order to reduce doubts and possible emotional effects.
Education is a useful tool to lower uncertainty toward the disease during care interventions if it is reliable and concise, provided by a credible source and given through clear and assertive communication means. This would help people to understand the disease process, allowing for the development of coping strategies that ease the adaptation to the new health condition. Uncertainty toward the disease should be addressed during the different stages of the disease: moment of diagnosis, treatment, and care. Reliable information and nursing care will reduce uncertainty in each phase of the disease.
Based on the results, self-efficacy is a determinant of well-being when faced with different health conditions. Moreover, applying this psychological tool during nursing interventions may help improve self-perception, increase the patient’s self-confidence, and give them a positive attitude to effectively manage crisis.
This analysis found that breast cancer creates high levels of stress, suffering, uncertainty, and distress from the moment of diagnosis and throughout the disease and treatments processes, as well as during recovery, up until remission. This drastically damages the quality of life of affected women. This study showed that self-efficacy is a cognitive-behavioral factor of self-protection, allowing women with breast cancer to accept and/or handle difficulties and threats that may hinder their biopsychosocial well-being.
Future research should consider using a qualitative approach to analyze the relationship between self-efficacy and uncertainty in women with breast cancer.
One of the limitations of the present study was the difficulty finding studies that analyzed the influence of self-efficacy on uncertainty and quality of life in breast cancer patients.
REFERENCES
1. Vea H, Cabrera A, Barros M, Rivera L, Seco A, Martín A. Enfoques, evolución y afrontamiento del envejecimiento demográfico en Cuba. Rev Panam Salud Pública. 2018;42:e21. [ Links ]
2. Serra Valdés M, Serra Ruíz M, García M. Las enfermedades crónicas no transmisibles: magnitud actual y tendencias futuras. Rev Finlay. 2018;8(2):140-8. [ Links ]
3. Ramírez-Perdomo CA, Rodríguez-Velez ME, Perdomo-Romero AY. Incertidumbre frente al Diagnostico de Cáncer. Texto Contexto - Enferm (Internet). 2018 (citado 15 de abril de 2019);27(4). Disponible en: Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-07072018000400319&lng=es&tlng=es [ Links ]
4. Barrios E, Garau M. Cáncer: magnitud del problema en el mundo y en Uruguay, aspectos epidemiológicos. An Fac Med. 2017;4(1):7-161. [ Links ]
5. Pačarić S, Kristek J, Mirat J, Kondža G, Turk T, Farčić N, et al. The quality of life of Croatian women after mastectomy: a cross-sectional single-center study. BMC Public Health. 2018;18(1):999. [ Links ]
6. Global Cancer Observatory, International Agency for Research on Cancer, Organización Mundial de la Salud . Cancer today (Internet). Ginebra: OMS; 2020 (citado 17 de marzo de 2019). Report No.: Data visualization tools for exploring the global cancer burden in 2020. Disponible en: Disponible en: http://gco.iarc.fr/today/home [ Links ]
7. Organización Mundial de la Salud, Organización Panamericana de la Salud, Global Cancer Observatory. Cáncer de mama en las Américas (Internet). Ginebra: OMS; 2018 (citado 18 de marzo de 2019) Disponible en: Disponible en: https://www.paho.org/hq/index.php?option=com_docman&view=download&category_slug=estadisticas-mapas-4868&alias=46503-epidemiologia-cancer-de-mama-en-las-americas-2018&Itemid=270&lang=es [ Links ]
8. Knaul FM, López Carrillo L, Lazcano Ponce E, Gómez Dantés H, Romieu I, Torres G. Cáncer de mama: un reto para la sociedad y los sistemas de salud. Salud Pública México. 2009;51:s138-40. [ Links ]
9. Hajian sepideh, Mehrabi E, Simbar M, Houshyari M. Coping Strategies and Experiences in Women with a Primary Breast Cancer Diagnosis. Asian Pac J Cancer Prev (Internet). 2017 (citado 25 de febrero de 2020);18(1). Disponible en: Disponible en: http://doi.org/10.22034/APJCP.2017.18.1.215 [ Links ]
10. Finck C, Barradas S, Zenger M, Hinz A. Quality of life in breast cancer patients: Associations with optimism and social support. Int J Clin Health Psychol IJCHP. 2018;18(1):27-34. [ Links ]
11. López Z, González J, Amador R, Lorenzo O, Herrera L, Bello L. Cáncer de mama en mujeres jóvenes. Presentación de dos casos. Rev Médica Electrónica. 2018;40(4):1186-96. [ Links ]
12. Valderrama MC, Sánchez R. Anxiety and depression disorders in relation to the quality of life of breast cancer patients with locally advanced or disseminated stage. Rev Colomb Psiquiatr Engl Ed. 2018;47(4):211-20. [ Links ]
13. Lopes JV, Bergerot CD, Barbosa LR, Calux NM de CT, Elias S, Ashing KT, et al. Impact of breast cancer and quality of life of women survivors. Rev Bras Enferm. 2018;71:2916-21. [ Links ]
14. Yeong K, Seon Y. Los efectos de la incertidumbre sobre la calidad de vida en pacientes jóvenes con cáncer de mama: centrados en el efecto mediador de la intimidad matrimonial. J Korean Acad Nurs. 2018;48(1):50-8. [ Links ]
15. Rajmil L, Estrada MD, Herdman M, Serra-Sutton V, Alonso J. Calidad de vida relacionada con la salud (CVRS) en la infancia y la adolescencia: revisión de la bibliografía y de los instrumentos adaptados en España. Gac Sanit. 2001;15:34-43. [ Links ]
16. Schwartzman L. Calidad de vida Relacionada con la Salud: Aspectos Conceptuales. Enferm Glob (Internet). 2003 (citado 22 de abril de 2019);21. Disponible en: Disponible en: https://scielo.conicyt.cl/pdf/cienf/v9n2/art02.pdf [ Links ]
17. Joaquín-Mingorance M, Arbinaga F, Carmona-Márquez J, Bayo-Calero J, Joaquín-Mingorance M, Arbinaga F, et al. Estrategias de afrontamiento y autoestima en mujeres con cáncer de mama. An Psicol. 2019;35(2):188-94. [ Links ]
18. Molano-Tobar NJ, Varela PEV. Percepción Acerca Del Cáncer De Mama En Un Grupo De Mujeres De Un Hospital En Popayán, Colombia. MHSalud. 2017;13(2):1-14. [ Links ]
19. Guerrero Alcedo JM, Parra Soteldo LR, Mendoza Oropeza JC. Autoeficacia y calidad de vida en pacientes con diabetes mellitus tipo 2 sometidos a hemodiálisis. Rev Cuba Salud Pública. 2016;42(2):193-203. [ Links ]
20. Olaz F, Pérez E. Creencias de Autoeficacia: desarrollo de escalas y líneas de investigación. Rev Tesis. 2012;1:157-70. [ Links ]
21. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191-215. [ Links ]
22. Pereyra Girardi CI, Ronchieri Pardo C d V, Rivas A, Trueba DA, Mur JA, Páez Vargas N. Autoeficacia: Una Revisión Aplicada A Diversas Áreas De La Psicología. Ajayu Órgano Difus Científica Dep Psicol UCBSP. 2018;16(2):299-325. [ Links ]
23. Doria SCR, Jimenez NNV, Montes JEO. Condiciones de vida y estrategias de afrontamiento de las mujeres con cáncer de mama en Córdoba, Colombia. An Psicol Ann Psychol. 2020;36(1):46-55. [ Links ]
24. Molano-Tobar NJ, Varela PEV. Percepción acerca del cáncer de mama en un grupo de mujeres de un hospital en Popayán, Colombia. MHSalud Rev En Cienc Mov Hum Salud (Internet). 2017 (citado 20 de marzo de 2020);13(2). Disponible en: Disponible en: https://www.revistas.una.ac.cr/index.php/mhsalud/article/view/9014 [ Links ]
25. Coello P, Ezquerro O, Fargues I, García J, Marzo M, Navarra M, et al. Enfermería basada en la evidencia. Hacia la excelencia en los cuidados. (Internet). primera edición. Vol. 7. Barcelona - España: Avances de Enfermería; 2004. 130 p. Disponible en: https://ebevidencia.com/wp-content/uploads/2013/08/EBE.-Hacia-la-excelencia-en-cuidados.pdf [ Links ]
26. Mendes KDS, Silveira RC de CP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto - Enferm. 2008;17:758-64. [ Links ]
27. Barrios Serna KV, Orozco Núñez DM, Pérez Navas EC, Conde Cardona G. Nuevas recomendaciones de la versión PRISMA 2020 para revisiones sistemáticas y metaanálisis. Acta Neurológica Colomb. 2021;37(2):105-6. [ Links ]
28. Higgins J, Green S. Manual Cochrane de revisiones sistemáticas de intervenciones (Internet). Centro Cochrane Iberoamericano. Barcelona - España: John Wiley & Sons; 2011. 639 p. (versión 5.1.0). Disponible en: https://es.cochrane.org/sites/es.cochrane.org/files/public/uploads/Manual_Cochrane_510_reduit.pdf [ Links ]
29. Mejía-Rojas ME, Contreras-Rengifo A, Hernández-Carrillo M. Calidad de vida en mujeres con cáncer de mama sometidas a quimioterapia en Cali, Colombia. Biomédica. 2020;40(2):349-61. [ Links ]
30. Oh YK, Hwang SY. Impact of Uncertainty on the Quality of Life of Young Breast Cancer Patients: Focusing on Mediating Effect of Marital Intimacy. J Korean Acad Nurs. 2018;48(1):50. [ Links ]
31. Muñoz D, Cogollo R, Arteaga A, Hernandez S. Incertidumbre Frente A La Enfermedad En Mujeres Diagnosticadas Con Cáncer De Seno. Investig Andina. 2018;20(36):11-22. [ Links ]
32. Jo K-H, Son B-K. (The relationship of uncertainty, hope and quality of life in patients with breast cancer). Taehan Kanho Hakhoe Chi. 2004;34(7):1184-93. [ Links ]
33. Gold M, Dunn LB, Phoenix B, Paul SM, Hamolsky D, Levine JD, et al. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97-105. [ Links ]
34. Prieto A, Rocha H, Yepes T, Navas D, Monterroza R, Torres Y. Condiciones Sociodemográficas y Nivel de Incertidumbre en Mujeres ante el Diagnóstico de Cáncer de Mama. Hacia Promoc Salud. 2015;13. [ Links ]
35. Coelho RCFP, Garcia SN, Marcondes L, da Silva FAJ, de Paula A, Kalinke LP. Impact on the quality of life of women with breast cancer undergoing chemotherapy in public and private care. Investig Educ En Enfermeria. 2018;36(1). [ Links ]
36. Cordeiro L de AM, Nogueira DA, Gradim CVC. Mulheres com neoplasia mamária em quimioterapia adjuvante: avaliação da qualidade de vida (Women with breast cancer in adjuvant chemotherapy: assessment of quality of life) (Mujeres con neoplasia mamaria en la quimioterapia adyuvante: evaluación de la calidad de vida). Rev Enferm UERJ. 2018;26(0):17948. [ Links ]
37. Setyowibowo H, Purba FD, Hunfeld JAM, Iskandarsyah A, Sadarjoen SS, Passchier J, et al. Quality of life and health status of Indonesian women with breast cancer symptoms before the definitive diagnosis: A comparison with Indonesian women in general. PloS One. 2018;13(7):e0200966. [ Links ]
38. Lopes JV, Bergerot CD, Barbosa LR, Calux NM de CT, Elias S, Ashing KT, et al. Impact of breast cancer and quality of life of women survivors. Rev Bras Enferm. 2018;71:2916-21. [ Links ]
39. Villar R, Fernández P, Garea C, Pillado MT, Barreiro V, Martín CG, et al. Quality of life and anxiety in women with breast cancer before and after treatment. Rev Lat Am Enfermagem (Internet). 2017 (citado 5 de mayo de 2019);25. Disponible en: Disponible en: http://www.scielo.br/scielo.php?script=sci_abstract&pid=S0104-11692017000100404&lng=en&nrm=iso&tlng=en [ Links ]
40. Gangane N, Khairkar P, Hurtig A-K, Sebastián MS. Quality of Life Determinants in Breast Cancer Patients in Central Rural India. Asian Pac J Cancer Prev APJCP. 2017;18(12):3325-32. [ Links ]
41. Silva N, Da Silva SR. Qualidade de vida de mulheres submetidas à cirurgia oncológica de mama. Rev Enferm UERJ. 2016;24(3):7634. [ Links ]
42. Edib Z, Kumarasamy V, Abdullah N binti, Rizal A, Al-Dubai S. Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health Qual Life Outcomes. 2016;14(26). DOI: 10.1186/s12955-016-0428-4 [ Links ]
43. Garcia S, Jacowski M, Castro G, Galdino C, Guimarães P, Kalinke LP, et al. Quality of life domains affected in women with breast cancer. Rev Gaúcha Enferm. 2015;36(2):89-96. [ Links ]
44. Fatemeh MT, Saeedeh A, Samira B. The Investigation of the Relationship Between Cancer Coping and Symptom Management Self-Efficacy, Perceived Social Support, Uncertainty and Life Orientation in Breast Cancer Female Survivors. 2018;26(1):1-10. [ Links ]
45. Kochaki Z, Mohajjel A, Hassankhani H, Asghari M, Sanaat Z. Cancer-Related Self-Efficacy in Iranian Women With Breast Cancer. Womens Health Bull (Internet). 2015 (citado 30 de marzo de 2020);2(2). Disponible en: Disponible en: http://womenshealthbulletin.neoscriber.org/en/articles/21251.html [ Links ]
46. Pintado S. Self-concept and emotional well-being in patients with breast cancer. Rev Iberoam Psicol Salud (Internet). 2017 (citado 20 de marzo de 2020);8(2). Disponible en: Disponible en: http://www.rips.cop.es/pii?pii=7 [ Links ]
47. Foster C, Breckons M, Cotterell P, Barbosa D, Calman L, Corner J, et al. Cancer survivors’ self-efficacy to self-manage in the year following primary treatment. J Cancer Surviv Res Pract. 2015;9(1):11-9. [ Links ]
48. Muñoz DIM, Jiménez RC, Noriega AA, Pérez SH. Incertidumbre Frente a La Enfermedad En Mujeres Diagnosticadas Con Cáncer De Seno. Investig Andina. 2018;20(36):11-22. [ Links ]
49. Pérez-Hernández S, Okino-Sawada N, Díaz-Oviedo A, Lordelo-Marinho PM, Ruiz-Paloalto ML, Pérez-Hernández S, et al. Espiritualidad y calidad de vida en mujeres con cáncer de mama: una revisión integrativa. Enferm Univ. 2019;16(2):185-95. [ Links ]
50. Kim YH, Choi KS, Han K, Kim HW. A psychological intervention programme for patients with breast cancer under chemotherapy and at a high risk of depression: A randomised clinical trial. J Clin Nurs. 2018;27(3-4):572-81. [ Links ]
51. Sánchez LA, Rodríguez MCM, Luis M de la LB, Sotomayor MMS y, Hernández RMTT, Badillo VP. Incertidumbre y calidad de vida en mujeres y hombres afectados por cáncer. Enferm Cuid Humaniz. 2012;1(2):77-83. [ Links ]
How to cite: Pastuña-Doicela R, Sanhueza-Alvarado O. Influence of Self-efficacy on Uncertainty and Quality of Life of Women with Breast Cancer. Integrative Review. Enfermería: Cuidados Humanizados. 2021;10(2):124-144. DOI: 10.22235/ech.v10i2.2603
Contribution of the authors: a) Study conception and design, b) Data acquisition, c) Data analysis and interpretation, d) Writing of the manuscript, e) Critical review of the manuscript. R. P. D. has contributed in a, b, c, d; O. S. A. in d, e.
Received: June 14, 2021; Accepted: October 14, 2021










 text in
text in