Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.8 no.2 Montevideo Dec. 2019 Epub Dec 01, 2019
https://doi.org/10.22235/ech.v8i2.1848
Artículos Originales
Food Addiction: Another determinant associated with the adhesion of nutritional treatment
1 Universidad Católica del Uruguay, Uruguay. luciabentancoruy@hotmail.com
2Fondo Nacional de Recursos, Uruguay
Keywords: Food Addiction; Nutritional Evaluation; Nutrition Surveys.
Palabras Clave: Adicción a la Comida; Evaluación Nutricional; Encuestas Nutricionales
Palavras-chave: Dependência de Alimentos; Avaliação Nutricional; Inquéritos Nutricionais.
Introduction
Obesity is a multi-factorial disease: it is linked not only to genetic factors such as sex and age, but also the educational, economic, social and cultural aspects of each individual. There is also another factor of great relevance, often ignored: the psychological aspects of the disease. An important point within this factor is the self perception of body image (BI). In a study of patients who attend the Secondary Cardiovascular Prevention Program of the National Resource Fund (SCPP of the NRF) it was observed that most patients have a severe underestimation of their BI: they perceived themselves with a lower weight than they actually had. The obese perceived themselves as overweight, and the overweight as having a normal weight1. If the person does not perceive him/herself having a problem of malnutrition by excess, he/she will not change aspects of their habits leading to modify their situation and thus reducing the risks of developing chronic diseases.
Within the psychological factor, Food Addiction (FA) is a key factor. The word addiction comes from the Latin addictio: debtor, for lack of payment, who was given out as a slave to his creditor.2 According to the World Health Organization (WHO), an addiction is a physical and psycho-emotional disease; it is a dependency or a need towards a substance, activity or relationship (codependence) 2. Repeated consumption of foods rich in sugars and fats results in a decreased regulation of dopamine (DA) receptors and a decrease in the sensitivity of the symbolic meso-reward circuit; these changes occur in response to abuse in addictive behaviors to substance such as alcohol, marijuana, cocaine and heroin. The decrease in DA activity in the ventral tegmental area (VTA) leads to a significant increase in food consumption3. In 1956 Randolph4 described the existence of individuals presenting symptoms related to certain foods with a pattern similar to that observed in addiction. Repeated exposure to certain foods, particularly foods of high energy density, in vulnerable individuals can trigger compulsive consumption and low control over their intake4; the term food addiction (FA) therefore comes up.
There are several researches and studies worldwide that evaluate FA in certain populations, highlighting that the prevalence of FA in students and the community in general ranges from 5-10%, increasing in obese populations up to 15-25%. This number increases even more in morbidly obese populations5. In Latin America there is a study conducted in Mexico and another one in Chile. The first one is a validation of the Yale Food Addiction Scale (YFAS) and its translation into Spanish. The second one assesses the presence of FA in Chilean students and relates it directly to their nutritional status. This study shows that this condition is more prevalent in women than in men and that it is related to obesity 4,6.
The Secondary Cardiovascular Prevention Program (SCPP) has been developed to improve the care process of patients with ischemic heart disease and/or high cardiovascular risk. The objective of the Program is to optimize the treatment of patients with coronary heart disease, promote healthy lifestyles, control cardiovascular risk factors and facilitate access to cardio-protective medication to improve survival rates, quality of life and decrease the need for new revascularization procedures7.
The present study seeks to study the prevalence of FA in patients attending the SCPP in order to optimize the tools already in use for their treatment and to generate the possibility of creating new ones, thus favoring the integral care of the patient in the cardiovascular consultation. The objectives are I) to study the prevalence of food addiction in patients attending the SCPP of the National Resources Fund in the period October-December 2016 in Montevideo, Uruguay; II) to characterize the study population according to age, sex and nutritional status; and III) to know the prevalence of food addiction in patients.
Methodology
A descriptive, observational and cross-sectional study was conducted. The sample was not probabilistic, convenient, of 153 patients attending the SCPP who had a consultation between October and December 2016, whose necessary data to evaluate the proposed variables was available and who could answer the required questionnaire. For the characterization of the study population, the data found in the “María” computer system of the NRF was used.
The variables used to characterize the study population were age (over or under 60 years), sex and nutritional status. For the latter, the categories were differentiated according to the age of the patient since BMI index criteria are different. If under 60 years of age: underweight (BMI ‹18.5), normal weight (BMI between18.5-24.9), overweight (BMI between 25-29.9), obesity (BMI ≥30). For adults over 60 years of age, underweight (BMI ‹23), normal weight (BMI 23-27.9), overweight (BMI 28-31.9), obesity (≥32). OPS 2002. The YFAS scale was used to measure the FA. Questions were asked by telephone to almost the entire population and staff (3% of the study population) to the selected sample.
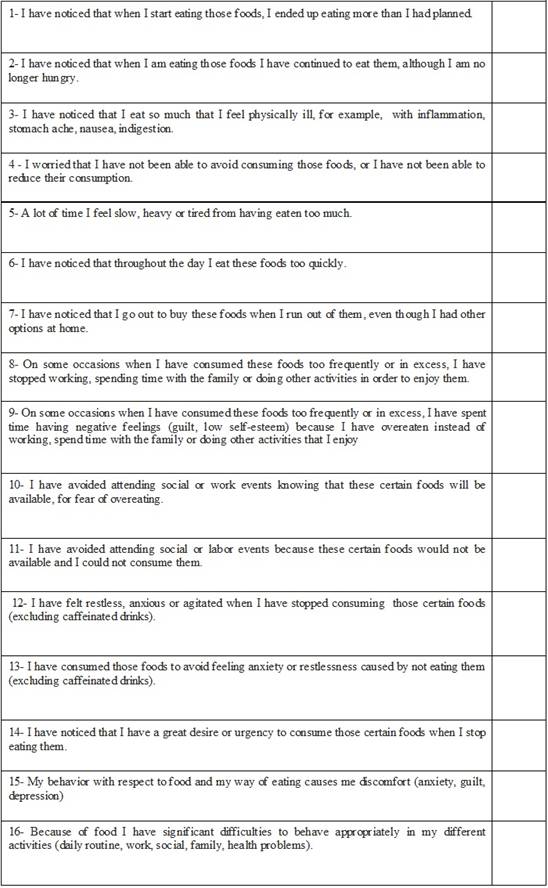
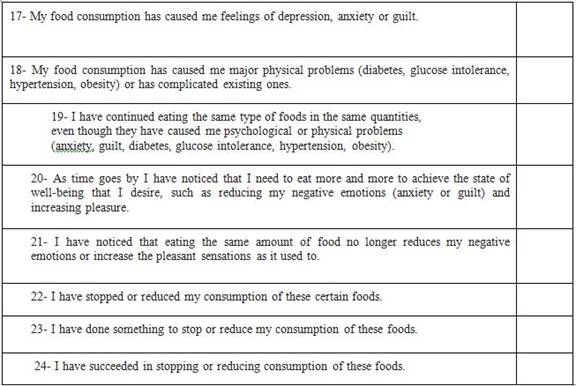
Gearhardt and others developed a tool based on the DSM-IV-TR to determine which individuals are at a high risk of food addiction, regardless of their weight4, a questionnaire of 25 questions in dichotomous format and Likert scale where subjects are asked to refer to their behaviors related to food in the last twelve months. This questionnaire allows differentiating individuals with FA from those who do not have it, as well as observing those who have symptoms. The use of this instrument shows that higher food addiction scores correlate with greater activation of regions involved in substance dependence, in response to certain foods. The Spanish translation of the scale by Valdés et al6 was used. For the analysis of the results, an Excel matrix was extracted from the web page of the Laboratory of Science and Treatment of Foods and Addictions.
A pilot test was carried out to apply the survey to a group of patients attending the Obesity Care Program in order to verify their understanding of the same. Although the sample was small (10 participants), it appears that 10% of the respondents presented food addiction, indicated by the presence of three or more symptoms and the presence of clinical significance. Of the remaining ones, although they did not present addiction because they did not meet the criteria established for it, it is remarkable that 44% have three or more symptoms of addiction, a fact to be taken into account in the care given to them, since it can interfere with the success of the treatment.
Results
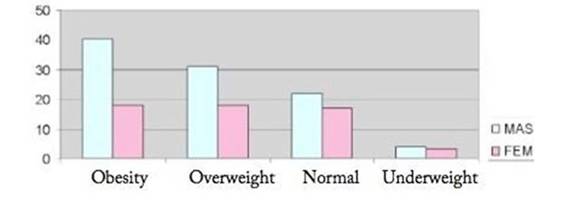
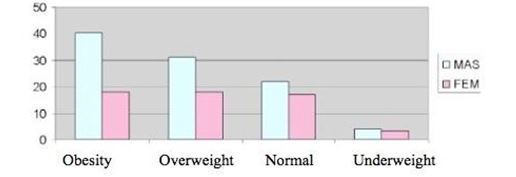
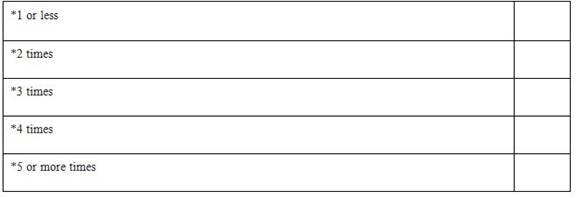
The study population consisted of a total of 153 patients, 63% of them male. 81% of the population was over 60 years of age, being classified as older adults. Analyzing the nutritional status of these patients, it appears that 70% of the population presented malnutrition due to excess, 32% were overweight and 38% were obese. (Table 1) (Graph 1)
Table 1: Distribution of respondents according to nutritional status and age
Source: Personal Collection (2019)
Table 2: Distribution of respondents according to sex and nutritional status
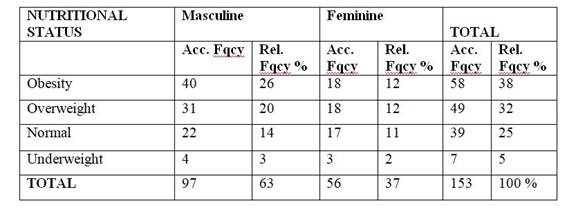
Source: Personal Collection (2019)
If nutritional status and sex are also taken into account, it is observed that half of the respondents who are overweight or obese are men (Table 2). Most of the surveys were by telephone (97%). Regarding the prevalence of FA in this population, 5.9% (95% CI = 2.7-10.9) of the sample meets the YFAS criteria. This means that it has three or more symptoms of the pathology and that also associates clinical significance (questions 15 and 16 of the scale greater than 1 (Graph 2).
Table 3: Distribution of respondents according to sex and food addiction
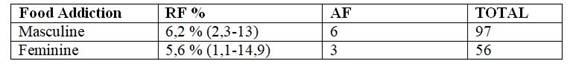
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
No relationship between addiction and sex was observed. There are similar figures of addiction prevalence in both sexes (Table 3)
Table 4: Distribution of patients according to age and food addiction
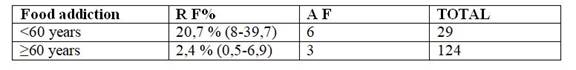
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
There is a higher prevalence of addiction in the age range under 60 (Table 4)
Table 5: Distribution of patients according to nutritional status and food addiction
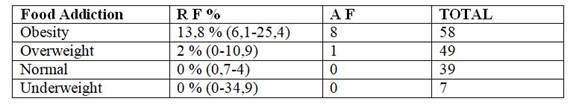
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
Obesity is most prevalent at 13.8% followed by overweight (Table 5, Table 6, Table 7, Table 8, Table 9)
Table 6: Distribution of patients with no food addiction according to the quantity of symptoms present
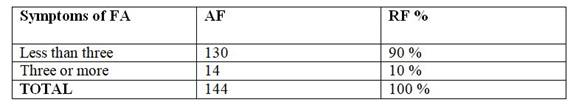
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
Table 7: Distribution of patients with more than three symptoms by sex
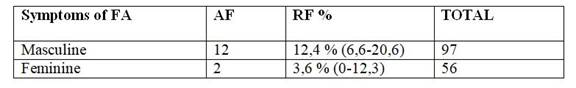
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
Table 8: Distribution of patients with more than three symptoms by age
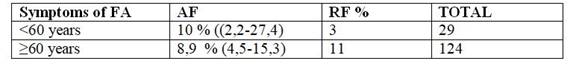
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
Table 9: Distribution of patients with more than 3 symptoms according to nutritional status
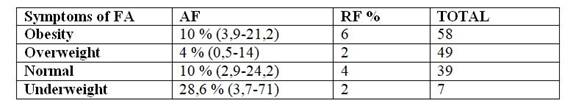
Source: Fondo Nacional de Recursos, Oct-Dec (2016)
There is a 10% of the population presenting three or more symptoms for FA without even having the clinical significance that determines the presence of the pathology, predominantly in the male population (12.4%) and under 60 years (10%). Taking into account the association of the presence of FA symptoms and nutritional status, there are 10% of obese people who have three or more symptoms for FA and 4% of overweight patients, while in the population with Normal status there are 10% who have these symptoms. These values were exceeded by underweight patients, but these results are affected by the low sample size (95% CI = 3.7-71). A point that is of the utmost importance to highlight is that all the patients that integrated the sample present at least one symptom of FA.
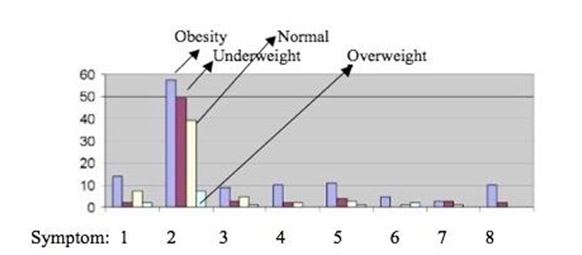
Through the previous graph it can be observed which symptoms of food addiction predominated by nutritional status.
Symptom:
1- Substance taken in greater quantity and for a longer period than expected.
2- Persistent desire or repeated failed attempts to stop eating. 3- A lot of time/activity to obtain, use, recover. 4- Important social, occupational or recreational activities given or reduced.
5 - The use continues despite the knowledge of the adverse consequences (for example, the breach of the obligation of the paper, the use when it is physically dangerous).
6- Tolerance (marked increase in quantity, marked decrease in effect).
7- Characteristic withdrawal symptoms, substance taken to relieve withdrawal.
8- The use causes deterioration or clinically significant distress.
In obesity, symptoms 2, 1 and 5 stand out. For all patients, regardless of their nutritional status, symptom 2 is the most prevalent, and has to do with the desires and attempts to stop or reduce the consumption of certain foods (Graph 3).
Discussion
In Uruguay almost 65% of the population is overweight or obese. The data shown in this study does not deviate from reality and exceeds the national average. The characteristics of age, sex and nutritional status are directly correlated with the study conducted in the NRF (2004-2007), where the majority of the population admitted was male, between 30 and 70 years, with obesity predominant.
Malnutrition by excess, more specifically obesity, results from a change in the form of diet and physical activity, including the so-called “nutritional transition” 8. This excessive increase in the percentage of obese people in the world forced to deepen their study and look for new causes that were the initial kick for developing public policies that would attack the problem, tending to reduce it.
Although new causes have been sought and continued to be sought, in recent years much emphasis has been placed on working on the psychological aspects that influence the development and maintenance of obesity. In this line, the perception of body image was studied, and in several studies worldwide a distortion in its perception was found, where most of the people who integrated the studies underestimated their weight 9,10. A similar study was carried out in patients attending the SCPP, having been measured through the Stunkard silhouettes, with similar results as the worldwide standard, with a very high percentage of patients underestimating their body weight 1.
The normalization and social acceptance of obesity, and the persistence of altered para-clinical values in these patients despite all the material and human resources used in their treatment forced to find other causes that could be interfering with the adherence to the treatment. The prevalence of FA was almost 6%, value similar to that found in student populations and the general community (5-10%). In 2015, in Chile, the YFAS questionnaire was applied to a population of university students, showing as a result that FA was more prevalent in women and was related to obesity. A prevalence of FA of 25% was found in a sample of obese adults. In obese people who wish to lose weight, the rates increase even more, meeting the FA criteria by 41.7% and 53.7% in patients requesting bariatric surgery. In the present study, FA can also be associated with excess weight since 13.8% of the obese presented FA symptoms, while 2% were overweight. It is not possible to relate the results of the aforementioned research regarding the prevalence according to sex. In this investigation the prevalence of FA was similar in both sexes.
In a study evaluating the Yale food addiction scale, the presence of symptoms to develop FA was negatively correlated with weight loss, suggesting that this symptomatology could affect the success of treatment in obese people 5. In the present study it was observed that the entire population presented at least one symptom for FA, and 10% had three or more symptoms, being more prevalent within the male sex and in persons under 60 years of age. If the nutritional status where these symptoms prevail is also considered, there is 10% in obesity and 4% in overweight. It is important to note that in the population with normal nutritional status there are 10% who have these symptoms. These values were exceeded by patients with low weight, but these results are affected by the low sample size (95% CI = 3.7-71), recommending for a future study the increase in size and the possibility of conduct a similar investigation only with low weight patients.
One of the key symptoms of this pathology is craving, the urgent or irrepressible desire which in most cases results in a loss of control. This contributes to the development, maintenance and relapse of addictive behavior. When analyzing the symptoms related to nutritional status, the persistent or repeated desire to be able to stop eating certain foods is present regardless of the status. In obesity the symptom that alludes to the consumption of food in excess and for longer periods than expected is the one that predominates, and in almost the same proportion the patients declared to keep on eating despite knowing the adverse consequences. In a study of obese people in the United States and Australia in 2014, it was observed that 86% of the population had a persistent desire or unsuccessful attempts to reduce consumption of certain foods, and 29% reported continuing to consume them despite psychological or physical problems derived from such abuse 12. Intervention when these symptoms are present can prevent the development of FA in patients who do not yet have it. It is of great importance to know the treatments that are currently being used in order to select those that are the most appropriate and applicable in this group of patients.
The first choice treatments to address addictions, and in particular craving, are based on the use of drugs and/or psychotherapeutic treatments. Interventions can be performed to prevent the development of pathology in patients attending the SCPP. Among these psychological and/or behavioral treatments is the Cognitive Behavioral Therapy (CBT) that has shown satisfactory results in the reduction of symptoms of FA and food psychopathology. This allows the patient to observe their behavior, thoughts and emotions and their relationship with their inadequate eating habits to find better alternatives. Nutritional interventions allow patients to maintain healthy eating habits through psycho-education and the establishment of regular eating patterns such as risk management.
On the other hand, the Interpersonal Therapy has been used with good results in overweight and obese patients who report loss of control when eating. It focuses on interpersonal problems, improves mood and increases the patients' feelings of self-efficacy. The Behavioral Dialectic Therapy (BDT) was adapted for application in eating disorders, and it focuses on emotional regulation. New technologies have also begun to be used, such as virtual reality, which simulates a three-dimensional computer generated environment and allows the user to interact in real time with an interface that facilitates a sense of presence in that environment and the judgment of their experience.
Pharmacological treatments are similar to those applied in patients with substance dependence. First, non-selective opioid receptor antagonists, such as Naltrexone, may decrease the desire and consumption of foods high in sugar and fat in people with normal weight and in obese patients diagnosed with bulimia nervosa or another eating disorder. On the other hand, selective serotonin reuptake inhibitor drugs decrease binge-eating episodes. Glutamate-based treatments, both Acamprosate and Topiramate have shown positive results, decreasing craving for food and controlling weight gain in alcohol-dependent patients. It is suggested that neuro-modulation techniques to treat food addiction and more specifically craving could be useful 13.
Conclussion
The SCPP treats the patient in an integral way, trying to cover all the aspects that make up his pathology in order to contribute to a better quality of life. In the latest data obtained from a study conducted on this population, it was observed that approximately 3 out of 10 patients are obese and do not meet the recommendation for consumption of fruits, vegetables, fish or lean meat. In turn, fat consumption is inappropriate (presence of fried foods, butter, margarine). Despite the efforts made, there are a significant number of patients who do not adhere to any aspect of the treatment. The present study looked for another factor that could be negatively influencing the adhesion of these patients, and it was observed that almost 6% of the population presented FA. A fact to highlight is that there is a 10% that although they do not have FA have three or more symptoms of the pathology, which could trigger an addiction if it is not treated in time. It is noteworthy that all the members of the sample have at least one of the symptoms. It was also observed that among patients who are obese, 1 in 10 has FA. Being a topic that has taking relevance in the last few years, and having access to the test that allows to evaluate the presence of this pathology, it would be convenient to consider it a tool in the care of patients in the SCPP, being able to refer them to the psychology team of the institution when needed.
REFERENCES
1.Riccetto P, Calvo S, Gambogi R, Nigro S, Sánchez F. Percepción de imagen corporal, factor clave en el cuidado del estado nutricional. Fondo Nacional de Recursos. Montevideo, Uruguay; 2015. [ Links ]
2. Facchini, M, Zonis Zukefeld, R. Adicción alimentaria: teoría, clínica y abordaje terapéutico. Universidad Austral; 2016 [ Links ]
3.Stoeckel LE, Weller RE, Cook EW 3rd, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods.Neuroimage 2008; 41: 636-647. [ Links ]
4.Obregón A, Fuentes J, Pettinell P. Asociación entre adicción a la comida y estado nutricional en universitarios chilenos. Revista médica de Chile (Revista en línea) 2015 (acceso 9 Sept 2019 ); 143(5). Disponible en: http://dx.doi.org/10.4067/S0034-98872015000500006 [ Links ]
5.Meule, A. & Gearhardt, A.N. Five years of the Yale Food Addiction Scale: Taking stock and moving forward Curr Addict Rep (Revista en línea) 2014 (acceso 9 Sept 2019) 1: 193. https://doi.org/10.1007/s40429-014-0021-z [ Links ]
6.Valdés M, Rodríguez M, Cervantes J, Camarena B, de Gortar P. Traducción al español de la escala de adicción a los alimentos de Yale (Yale Food Addiction Scale) y su evaluación en una muestra de población mexicana-Análisis factorial. Salud Mental 2016; 39(6): 295-302. Disponible en: http://www.medigraphic.com/pdfs/salmen/sam-2016/sam166c.pdf [ Links ]
7.Fondo Nacional de Recursos (En línea). Montevideo. 2017. Programa de Prevención Secundaria Cardiovascular. (acceso 9 Sept 2019) Disponible en: Disponible en: http://www.fnr.gub.uy/descripcion_cardio [ Links ]
8.Organización de las Naciones Unidas para la alimentación y la agricultura (En línea). The nutrition transition and obesity. (acceso 9 Sept 2019) Disponible en: Disponible en: http://www.fao.org/focus/S/obesity/obes2.htm [ Links ]
9.Zaragoza A, Ortiz R. Estado nutricional y nivel de actividad física según percepción de los estudiantes de la Universidad de Alicante. Rev Esp Nutr Comunitaria (Revista en línea) 2012 (acceso 9 Sept 2019) 18 (3): 149-153. Disponible en: Disponible en: https://fcsalud.ua.es/es/alinua/documentos/investigacion/articulo-nutricion-y-activida-fisica.pdf [ Links ]
10.Squiers L, Renaud J, Mc Comack L, Tzenq J, Bann C, Williams P. How accurate are Americans’ perceptions of their own weight? J Health Commun (Revista en línea) 2014 (acceso 9 Sept 2019) (19)7: 795-812. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/24580374 [ Links ]
11.Quintero J, Félix Alcántara M, Banzo-Arguis C, Martínez de Velasco Soriano R, Barbudo E, Silveria B, Pérez-Templado Ladrón de Guevara . Psicopatología en el paciente con obesidad. Salud Mental (revista en internet) 2016 (acceso 9 Sept 2019) 39(3): 123-130 Disponible en: http:doi.org/10.17711/SM.0185-3325.2016.010 [ Links ]
12.Agüera Z, Wolz I, Sánchez I, Sauvaget A, Hilker I, Granero R, Jiménez-Murcia S, Fernández-Aranda F. Adicción a la comida un constructo controvertido. C. Med. Psicosom (Revista en línea) 2016 (acceso 9 Sept 2019) 117. Disponible en: Disponible en: http://www.editorialmedica.com/download.php?idart=727 [ Links ]
Authors' participation: The authors claim to have participated in: the design and design of the work; data acquisition; data analysis and interpretation; the writing of the manuscript; and the critical revision of the manuscript.
In the last 12 months: YES - NO
25- How many times in the last year have I tried to stop or decrease the consumption of these certain foods?
Received: February 14, 2019; Accepted: July 04, 2019











 text in
text in