Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Enfermería: Cuidados Humanizados
versão impressa ISSN 1688-8375versão On-line ISSN 2393-6606
Enfermería (Montevideo) vol.8 no.2 Montevideo dez. 2019 Epub 01-Dez-2019
https://doi.org/10.22235/ech.v8i2.1847
Original Articles
Comprehensive nursing care in an infant with hypoxic ischemical encephalopathy related to perinatal asphyxia
1 Universidad Federal de São Carlos (UFSCar). dsanchescouto@gmail.com
2 Universidad Juárez del Estado de Durango (UJED)
3Universidad Federal de Mato Grosso (UFMT)
Keywords: Nursing diagnosis; Nursing; Pediatric Nursing; Nursing process.
Palabras clave: Diagnóstico de enfermería; Enfermería; Enfermería Pediátrica; Proceso de enfermería.
Palabras-chave: Diagnóstico de enfermagem; Enfermagem; Enfermagem Pediátrica; Processo de enfermagem.
Introduction
Ischemic hypoxic encephalopathy (IHE) is a consequence of suffocation at childbirth, and responsible for generating neurological disabilities1. The IHE syndrome is a neurological disorder that consists of a dynamic process that affects term and preterm infants. This brain injury occurs in two stages: first, suffocation causes the reduction of blood flow to the brain causing primary damage. Blood and oxygen containment at birth can cause damage to the cells of the central nervous system, including cell death. Second, when the blood flow is restored in an injured brain, various side effects are triggered, which can damage the neural cells or even lead to brain death(2, 4).
According to the World Health Organization (WHO), perinatal asphyxia (PA) is among the three leading causes of death among neonates5. Up to 25% of newborns and 8% of deaths of children under 5 are directly associated with PA2. Each year, out of every 1,000 live births, three to five will present AP at birth, increasing the risks of neurological sequel3. Of the live newborns who suffered asphyxiation at the time of delivery, 15% to 20% die even in the neonatal period; and 25% of the survivors show permanent neurological disability. The most serious neurological damages occur as cerebral palsy, epilepsy and hyperactivity, among other aggravations. The risk conditions associated with IHE can develop during pregnancy, at the time of delivery or after birth, associated with low birth weight and prematurity5,7.
Nursing assistance focused on ensuring the recovery of infant health is developed in a systematic and individualized manner. With a humanized look, assistance should be extended to parents and family members, who have high levels of stress and anxiety as a result of the child's hospitalization. Nursing care is able to meet needs that go beyond direct assistance to pathology, strengthening the relationship and providing the bond with parents trying to reassure them8. The nursing team has a fundamental role in the care of infants with sequels of PA; they are responsible for ensuring that the treatment will be carried out correctly, contributing to the positive evolution of the infant. In the daily nursing care, aimed at pediatric patients, the Nursing Process shows the best ways to enable quality assistance, since there is a plan of actions that prioritize the patient. In this way, this study is aimed to present the Nursing Process in the clinical case of an infant hospitalized in a public institution with brain injury caused by perinatal asphyxiation
Methodology: Clinical Case
This is a clinical case report developed during the Social Nursing Service in the pediatric intensive care unit in a children's hospital in the city of Durango, Mexico, in November and December 2017. It is a descriptive work presenting the history, evolution, nursing diagnosis, planning of the interventions and the results obtained.
Identification and medical diagnosis data: MRJ is a 3 month and 28 day male baby on November 6, 2017, admitted to the Pediatric Intensive Care Unit. The medical diagnosis is: Global cerebral hypoxia. Moderate pulmonary hypertension (61 mmHg). Right ventricle hypertrophy. Total right pulmonary atelectasis remitted. Chemosis Cardiorespiratory arrest (two episodes). Secondary epileptic state. Secondary ischemic hypoxic encephalopathy.
Prenatal history: The mother, an 18-year-old first timer, student, B+ blood, with incomplete prenatal control, has consumed folic acid, ferrous sulfate, vaccinated against tetanus and influenza. No history of gestational complication. At 37 weeks gestation, a cesarean section is performed due to a restriction of intrauterine growth.
Pathological history: the baby was already hospitalized in a pediatric intensive care unit due to various conditions, the main diagnosis being an IHE. The newborn weighs 1600 grams, length of 40 cm, blood O + and APGAR score of 7 at 1 minute and 8 at 5 minutes.
He is transferred to the Neonatal Intensive Care Unit where oxygen is supplied by nasal tips and kept in an incubator. Two weeks after birth, he was diagnosed with gastroesophageal reflux disease and delayed gastric emptying with unknown etiology. A week later, the short lingual frenulum is corrected. He goes to the Growth and Development area when improvement and weight gain is shown. Totaling 57 days hospitalized, at 57 days of age, voluntary discharge is requested, weighing 2170 grams, with anemia, in-hospital pneumonia and a probable diagnosis of Silver-Russell syndrome. Silver Russell syndrome, where most cases are sporadic, has a genetic relationship. It is a disease characterized by intrauterine and postnatal growth retardation and abnormal cranial perimeter9. The discharge note shows that the patient is hypoactive, hypo-reactive, pale, hydrated, with no head support, tolerating feeding by an orogastric tube, still requiring oxygen supply by nasal tips, respiratory wheezing, peristalsis present and hypotrophic.
CLINICAL REPORT
At 3 months and 19 days of age he enters the emergency department due to bronchoaspiration while being fed with an orogastric tube, with the presence of a seizure. He suffers from cardiorespiratory arrest, and cardiopulmonary resuscitation maneuvers are performed. Mechanical ventilation begins when an orotracheal tube is placed, and at the dawn of the following day a central peripheral insertion catheter is placed in the right lower limb. He is admitted to the Intensive Care Unit, where he is diagnosed with global cerebral hypoxia resulting in hypoxic-ischemic encephalopathy, total right pulmonary atelectasis, and moderate pulmonary hypertension, which presumably caused a right ventricular hypertrophy detected later. Upon admission it has a weight of 3800 grams and length of 50 cm. At home he was being fed a breast milk substitute through an orogastric tube. Treatment starts with analgesics (acetaminophen), antibiotics (cefotaxime and clindamycin), anticonvulsants (levetiracetam, phenobarbital and phenytoin), calcium gluconate, phosphodiesterase inhibitor (sildenafil), antiemetics (metoclopramide), diuretics (furosemide). Then ophthalmic medications were added as a treatment for the conjunctivitis acquired in the hospital (hypromellose and prednisolone). A bladder catheter is placed to maintain strict fluid control. Five solutions are indicated: a) 3 ml of valproic acid titrated in 24 milliliters of physiological solution to pass 1 ml / h, b) 115 ml of 10% glucose solution plus 115 milliliters of physiological solution with 9 mEq of KCl for 24 h , c) 2 ml of dobutamine plus 10 ml of physiological solution to pass 0.8 ml / h, d) 0.6 ml of norepinephrine volumetric to 24 ml of 5% glucose solution to pass 0.6 ml / h, and e) 3.6 ml of volumetric midazolam to 24 ml of physiological solution to pass 1 ml / h. During the first week of intensive care he suffers another cardiac arrest and survives. Valuation is done eight days after being admitted.
ASSESSMENT BY FUNCTIONAL HEALTH PATTERNS
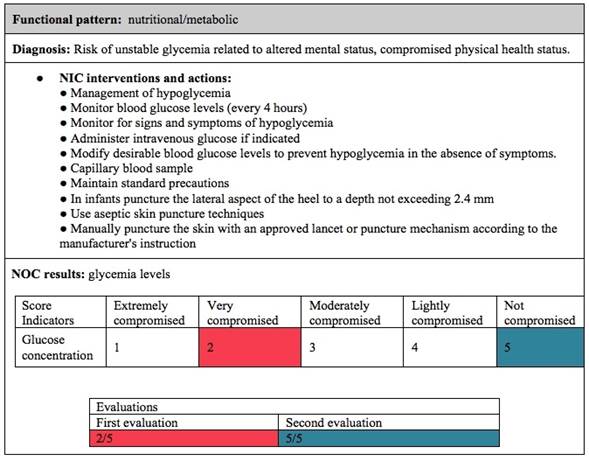
Nutritional/metabolic: He has dropped from 3800 grams to 3350 grams. According to the weight table for age in children, his weight is less than adequate for him. The abdominal perimeter is 32 centimeters. He is fasting because he is expected to have a tracheostomy, which has been postponed due to his delicate state. It has a glycemia value of 60 mg / dl, so the glucose solution constantly changes to achieve euglycemia. From the above, the Risk of unstable glycemia related to altered mental status, compromised physical health status was diagnosed7.
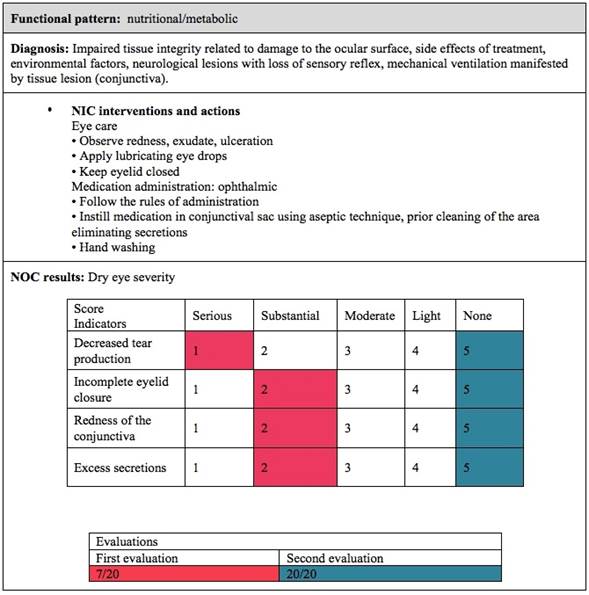
His hair is thin and sparse with good implantation. The eyes are brown, with isocoric, miotic and light-reactive pupils. There is eyelid edema, flushed sclera, presence of meatiness in the left eye and abundant secretions. Thus, the deterioration of tissue integrity related to damage to the ocular surface, side effects of the treatment, environmental factors, neurological lesions with loss of sensory reflex, mechanical ventilation manifested by tissue injury (conjunctiva) was diagnosed7.
The mucosa of the nose is hydrated, pink, and there is abundant secretion. In the mouth the mucous membranes are hydrated, there is little bleeding due to the orotracheal tube and the orogastric tube, and there is a presence of sialorrhea. There is peripheral edema, he is multipunched, there is erythema and peeling in the neck and perineum, injury due to the pulse oximeter on the dorsum of the right foot. The peripheral insertion venous catheter area is protected with a dressing, the area is healed daily.
A gasometry is performed and among the important data is the carbon dioxide pressure with a value of 45 mmHg and the pH at 7.58. Platelets have a value of 136x (10)3 , hematocrit is 30.9% and hemoglobin is 10.2 g / dl. TP is 15.2 seconds, in the TPT there is no coagulation, and the fibrinogen has a value of 197.7 mg / dl.
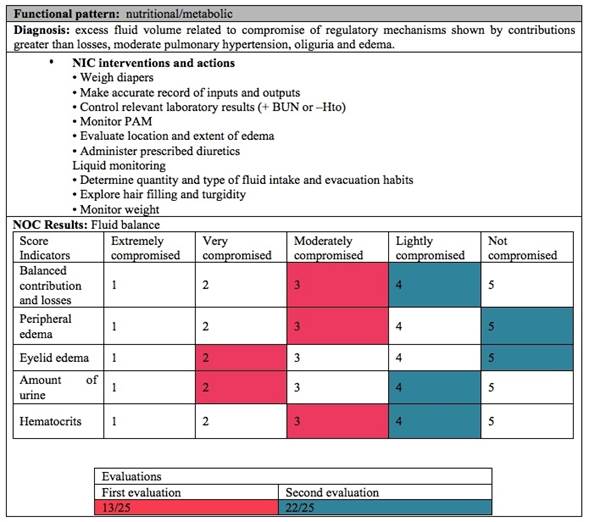
Elimination: Intestinal elimination is not present. He has a bladder catheter put in place at the time of admission in intensive care, diuresis is scarce (10 ml), and increases considerably after diuretic administration (55 ml), it is light yellow. In one day he has a loss of liquid of 467 ml and a total income of 582 ml. Therefore Excess of volume of fluid was diagnosed, related to compromise of the regulatory mechanisms manifested by contributions greater than losses, moderate pulmonary hypertension, oliguria and edema 7. There is a positive water balance.
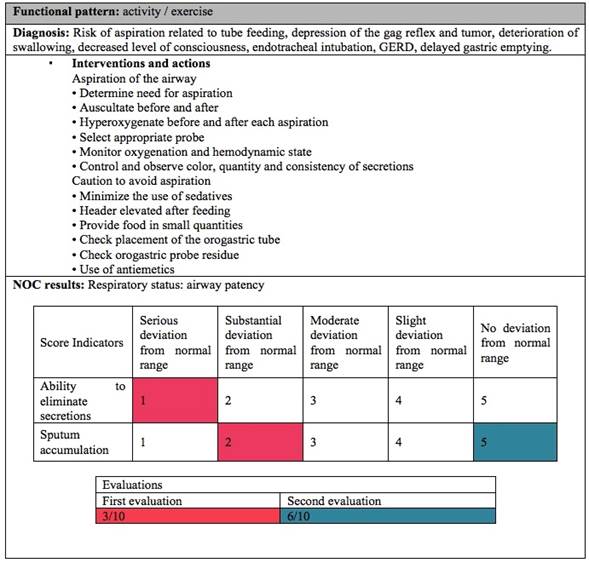
Activity / exercise: In the cardiovascular state, he has a heart rate of 90 beats per minute, blood pressure of 102/64 mmHg, capillary filling is less than 3 seconds. Raising the diagnosis of risk of bleeding related to essential coagulopathies 7. As for the respiratory status, he has mechanical ventilation with a respiratory rate of 19 breaths per minute, a FiO2 of 35% and oxygen saturation that is maintained above 90%. It has a good skin color, there are no signs of respiratory distress. There are abundant secretions from nose and mouth, and bronchial lavage produces thick hyaline and whitish secretions. There is risk of aspiration related to tube feeding, depression of the gag reflex and tumor, deterioration of swallowing, decreased level of consciousness, endotracheal intubation, GERD, delayed gastric emptying 7. Mobility is absent due to sedation, he is hypotonic. When trying to suspend sedation for the first time, presents a seizure of the tonic type; however, the dose of the sedative is lowered and begins to show repetitive movements in the extremities. There is marked spasticity. Impairment of physical mobility is diagnosed, related to cognitive, neuromuscular and sensory-perceptual impairment, decreased muscle control, decreased resistance to medications manifested by slowing of movement, limitation of range of movement, jerky movements 7.
Rest / sleep: It is not possible to assess due to sedation, there is no distinction between states of consciousness.
Cognitive / perceptual: There is reaction to light, but not tactile stimuli. The pupils are miotic, isocoric, there is no crying and he is prone to seizures, presenting repetitive movements. Global ischemia is observed in brain tomography, so parents are informed that neurological damage is important and permanent. Presents a great risk of developmental delay related to seizure, brain injury 7.
Coping / stress tolerance: For the assessment of pain, the patient's behavior was observed in response to physical contact or when performing nursing procedures. It is recommended to use a Pain Scale capable of assessing facial expression, crying, breathing, body movement and alertness. In that case, leading to a diagnosis of acute pain related to harmful agents (punctures, bronchial lavage, aspiration) manifested by changes in heart rate, defensive behavior and protective gestures 7.
Self-perception / self-concept: Parents remain positive regarding patient recovery. However they recognize feeling tired, worried and anxious.
Role / relationship: He lives with his parents, grandparents and uncles, is the only infant in his family. His parents receive constant support from relatives.
Sexuality / reproduction: The testicles are lowered, the foreskin is retractable, urinary meatus with normal location and permeable anus. There are erythema and characteristics of a fungal infection in the perineal area, as well as diaper rash. Raising the diagnosis of impairment of skin integrity related to age extremes, mechanical factors, humidity, physical immobilization, impaired sensation and bony prominences manifested by the alteration of the skin surface7.
Coping / stress: The behavior of the parents before the hospitalization of the baby is positive, but they constantly feel anxiety, as well as fear of touching and moving the infant due to ignorance of its handling.
Values / beliefs: Both parents are Catholics, in the cradle there are religious and scapular images. They consider the preservation of life as something important.
Care Plan And Results
Given the identified diagnoses, it was possible to establish the best interventions and monitor the patient's development and improvement. The interventions follow the ones established by the Nursing Interventions Classification (NIC) as a reference and for the contribution of the expected results the Nursing Outcomes Classification (NOC)(8, 9). Thus it was possible to present the construction of the care plan and the results obtained with the nursing intervention.
The first diagnosis was Risk of unstable glycemia related to altered mental state, compromised physical health status, which was managed to carry out a rigorous risk control, and in a few days the glycemia is normalized, values> 70 mg / dl, (best exposed in Table 1).
Table 1: Diagnostic care plan: Risk of unstable glycemia related to altered mental status, compromised physical health status.
Source: Personal Collection (2018)
In the diagnosis of deterioration of tissue integrity related to damage to the ocular surface, side effects of the treatment, environmental factors, neurological lesions with loss of sensory reflex, mechanical ventilation manifested by tissue lesion (conjunctiva), treatment with chloramphenicol was started. Not obtaining results, it goes through an evaluation by an ophthalmologist, who diagnoses chemosis. The treatment was changed to prednisolone and hypromellose ophthalmic was changed. The problem disappears within a few days after starting the new treatment (interventions in Table 2).
Table 2: Diagnostic care plan: Impaired tissue integrity related to damage to the ocular surface.
Source: Personal Collection
For excess fluid volume related to compromise of regulatory mechanisms shown by contributions greater than losses, moderate pulmonary hypertension, oliguria and edema, a better balance is achieved. As a result after the intervention it was possible to improve the edema presented above, as shown in Table 3.
The patient presented a high risk of bleeding related to essential coagulopathies. With the interventions it was possible to hardly notice a little difference, as Table 4 shows.
In the development route, the patient was subjected to a transfusion of 57 milliliters of fresh frozen plasma and two globular packages of 57 milliliters each.
Table 4: Care plan for the diagnosis of bleeding risk related to essential coagulopathies
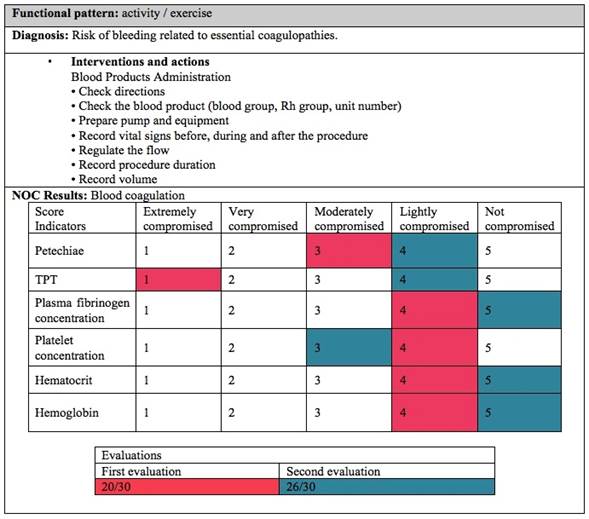
Source: Personal Collection (2018)
For the risk of aspiration related to tube feeding, depression of the gag reflex and tumor, deterioration of swallowing, decreased level of consciousness, endotracheal intubation, GERD, delay in gastric emptying, the intervention plan presented in Table 5. It was possible to present a good evolution, and to partially decrease the risk of aspiration. It is important to highlight that at the time of the second evaluation, the fast was suspended and the baby was begun to be fed with 40 milliliters of formula for infants by orogastric tube.
For the diagnosis of deterioration of physical mobility, it was possible to improve his joint and urinary performance and to reduce the risk of pressure ulcers. The evolution of this care can be observed in Table 6.
Table 6: Care plan for the diagnosis of impairment of physical mobility
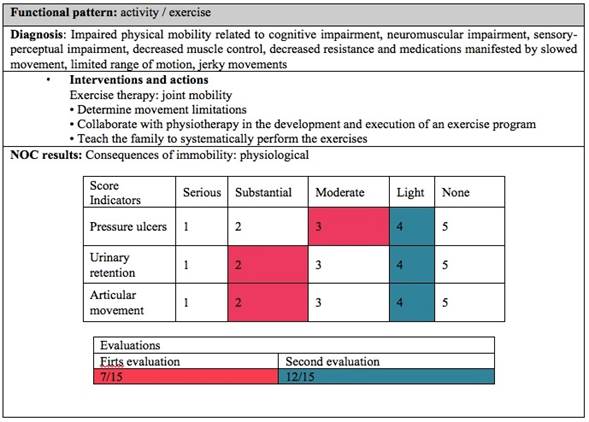
Source: Personal Collection (2018)
For the diagnosis of risk of developmental delay related to seizures and brain injury, it was possible to plan how to prevent and manage seizures, as shown in Table 7.
Table 7: Care plan for the diagnosis of risk of developmental delay
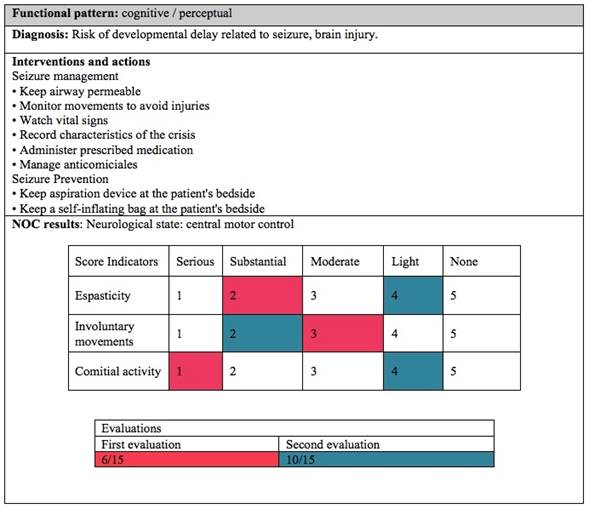
Source: Personal Collection (2018)
For the diagnosis of deterioration of skin integrity, a care intervention was planned focused on avoiding pressure injuries, as shown in Table 8. There was a highly positive evolution after the application of topical panthenol and miconazole in the genital area.
Table 8: Care plan for the diagnosis of deterioration of skin integrity
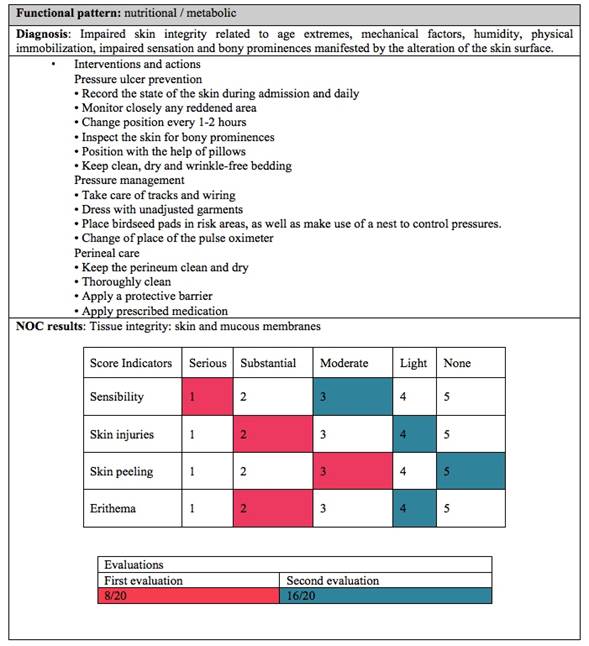
Source: Personal Collection (2018)
In the diagnosis of acute pain related to harmful agents (punctures, bronchial lavage, aspiration) manifested by changes in heart rate, defensive behavior and protective gestures, it is possible to visualize the interventions performed, in Table 9. The interventions achieve a satisfactory evolution presenting a reduction of defensive behaviors and gestures of protection.
Table 9: Care plan for the diagnosis of acute pain related to harmful agents
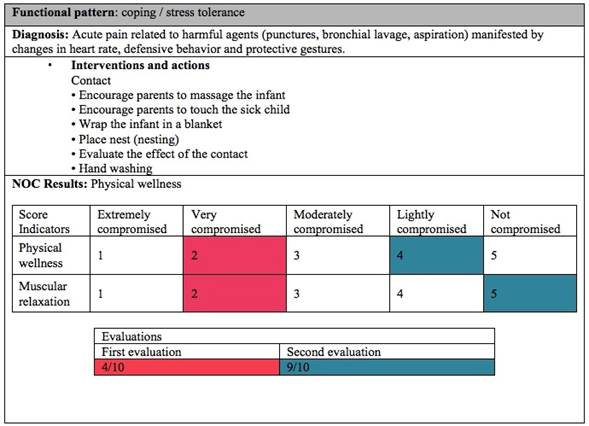
Source: Personal Collection (2018)
The treatment of patients with AP and IHE needs comprehensive care for the services provided, which begins in the delivery room and continues in the intensive care unit. Safely controlled hypothermia is the best strategy to reduce mortality related to IHE; the creation of protocols allows the introduction of patient care10. The treatment through hypothermia associated with the nursing interventions presented in this study, which obtained positive results, composes a relevant protocol for comprehensive patient care.
Final Consideration
The application of the nursing process during the social service enabled the development of evidence-based assistance under the use of NANDA, NIC and NOC tools, collaborating to train professionals capable of implementing quality assistance. What happened here is considered a sporadic case, due to a request for voluntary discharge in the middle of the clinical improvement process, generating complications and aggravating the clinical situation. The report of this case shows the importance of nursing in interventions early, together with a multidisciplinary team, adapting care and enabling a quality of life for the patient and family members.
REFERENCES
1. Blasina, F. Protección del recién nacido frente a la asfixia perinatal : perspectivas de un largo camino. Arch Pediatr Urug. 2016;87(3):195-7. [ Links ]
2. Lemus-Varela, M., Sola, A., Golombek, S., Baquero, H., Dávila-Aliaga, C., Fariña, D., et al. Recomendaciones terapeuticas del VII Consenso Clinico de SIBEN para la encefalopatia hipoxico-isquemica neonatal. Neoreviews . 2016; 17 (9): 554-67. Disponible en: http://neoreviews.aappublications.org/cgi/doi/10.1542/neo.17-9-e554 [ Links ]
3. Balushi, A., López, M., Wintermark, P. Impacto de la ventilación en el desarrollo de daño cerebral en recién nacidos con asfixia, tratados con hipotermia. Anest en México. 2017;29(1): 30-40. [ Links ]
4. Grupo de Trabajo Hipotermia Terapéutica C de EF-N (CEFEN). Recomendación para el tratamiento con hipotermia en recién nacidos con encefalopatía hipóxico- isquémica. Arch Argent Pediatr. 2017;115 (3:s):38-52. Disponible en: http://www.sap.org.ar/docs/publicaciones/archivosarg/2017/v115n3a26s.pdf [ Links ]
5. Rivera, M., Lara, N., Baró, T. Asfixia al nacer: factores de riesgo materno y su repercusión en la mortalidad neonatal. Rev Ide Inf Científica. 2017; 96 (6): 1143-52. [ Links ]
7. Riesgo-prendes, L., Salamanca Matta, A., Monterrey Gutiérrez, P., Bermúdez Hernández, P., Vélez, J. Hipoxia perinatal en el Hospital Mederi de Bogotá: comportamiento en los años 2007 a 2011. Rev Salud Pública. 2017; 19 (3): 332-9. [ Links ]
8. Segur, P., Morero, J., Oliveira, C. Assistência de Enfermagem ao recém-nascido com Sindrome do Desconforto Respiratório. Rev UNINGÁ. 2019;56 (S2): 141-59. [ Links ]
9. Hernández, EES. Síndrome Rusell Silver. Presentación de caso. Rev Méd Electrón (Internet). 2018 ;40(3): 784-9. [ Links ]
10. Silvera, F., Gesuele, JP., Oca, RM., Vidal, G., Martínez, V., Lucas, L., et al. Neuroprotección en pacientes con asfixia perinatal. Arch Pediatr Urug. 2016 ;87(3): 221-33. [ Links ]
Received: August 20, 2018; Accepted: May 15, 2019











 texto em
texto em