Services on Demand
Journal
Article
Related links
Share
Enfermería: Cuidados Humanizados
Print version ISSN 1688-8375On-line version ISSN 2393-6606
Enfermería (Montevideo) vol.8 no.2 Montevideo Dec. 2019 Epub Dec 01, 2019
https://doi.org/10.22235/ech.v8i2.1846
Original Articles
Nursing Models and Theories: Support for Palliative Care
13Universidad Católica del Uruguay
Keywords: Nursing model; Nursing theory; Palliative Care.
Palabras clave: Modelo de Enfermería; Teoría de la Enfermería; Cuidados Paliativos.
Palavras chave: Modelo de Enfermagem; Teoria de Enfermagem; Cuidados Paliativos.
Introduction
The World Health Organization (WHO) defines Palliative Care as an approach that improves the quality of life of patients and their families facing the problems associated with fatal diseases, through the prevention and relief of suffering through early identification and impeccable evaluation; the treatment of pain and other physical, psychosocial and spiritual problems1. It emphasizes teamwork as a pillar of palliative service programs, helping, among other things, for the patient to live as actively as possible until their death2.
On the other hand, the International Nursing Council considers in its definition of Nursing that it encompasses the autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or not and in all settings. Nursing includes health promotion, disease prevention and care for sick, disabled and dying people. Defense, promotion of a safe environment, research, and participation in the configuration of health policy and in the management of patients and health systems, and education are also key nursing functions3.
The purpose of Nursing is care, which is framed in actions and interventions with a solid scientific and humanistic foundation, based on theoretical models that guide discipline and professional practice. These models allow the development of the profession as they involve the interaction of a body of knowledge that improves the practice of nurses in all areas4. The evidence-based clinical practice places nurses within a professional discipline that provides the foundation for the interventions to be original, innovative and individualized5. In the same way, the conceptual models of Nursing constitute a series of conceptions that attribute a general interpretation in relation to the topic of interest for nurses: the care of the other.
Nursing in Palliative Care is considered a specialty within the discipline, so it is required to be in possession of a specialization or a master's degree in the area. The nurse should also have tools for critical thinking and evidence-based practice, communication training, patient and family education, spiritual and psychosocial care6. In addition, a professional must have training in the five basic roles of Nursing; clinical role, clinical consulting, administration, education and research as it constitutes the first link between the patient, family and members of the interdisciplinary team of Palliative Care7. On the other hand, according to Hagan, all nurses should be competent for Palliative Care, regardless of their environment or work area, making it possible through adaptive, undergraduate and postgraduate Palliative Care training programs that include communication skills, objectives of attention, and decision making. As well as creating an environment that supports nurses from the moral point of view, enhancing their capacity and work scope8.
Another important aspect of the nurse's role is related to the function of protecting the dignity of the person at the end of their life. According to Johnston, people want to be treated with dignity and must also have the right to die with dignity. Care with dignity is an intervention that guides nurses to identify and provide adequate care, from a physical, spiritual, emotional and social point of view9. The preservation of dignity can be instrumentalized through specific actions focused on care, in an integral way that facilitates the work of health personnel10.
This type of care is highly demanding for the nurse, both emotionally and physically. Inevitably, history itself, self-knowledge and sensibilities intersect with the suffering and experience of the patient and their family. Hence the importance of personal and institutional strategies that focuses on the nurse's self-care. However, the situation of the emotional stress of the nurse is exacerbated when she feels the opposite of what she was taught in her professional training, in which the educational model insists that there should be an emotional distance with the user and not involve your feelings9.
Based on a search for academic papers published between 2012 and 2018, it was possible to focus and base the use of nursing models for the practice of Palliative Care. However, it is important to mention that despite the recognized importance of the use of disciplinary fundamentals in care, there are still few publications that account for this.
Methodology
The objective of this research was to determine the use of nursing theories and models in Palliative Care. Such research and experiences could serve as a link between the theory and practice of Palliative Care nursing. An integrative review was carried out, which is understood as a method whose objective is the summary of published research, in order to obtain new conclusions on a topic of interest11.
Five different phases were considered; the first was the elaboration of the research question, in which the topic to be investigated was defined according to a guiding question, which was formulated according to the PICo strategy; the "P" corresponding to the Problem, "I" Phenomenon of interest, and "Co" to the context, thus achieving a delimitation of the problem12. In this integrative review, the question asked was: What research evidences the use of models and / or theories of Nursing in Palliative Care between 2012 and 2018?
In the second phase the literature search was carried out. Articles of inclusion in English, Spanish and Portuguese were considered as inclusion criteria, in which the application in Palliative Care of a nursing model or theory, published between 2012 and 2018, in journals indexed in Scopus, Scielo and Web of Science, full text and incorporated the keywords "Nursing model" AND "Palliative Care" and "Nursing theory" AND "Palliative Care", in the title, summary or text. The selected databases were included because they had access through the agreements of the participating universities. 18 articles emerged from this search that met the aforementioned criteria.
In the third phase the data was collected. The information was collected according to the methodology indicated in the previous phase, with relevant memos and field notes for the answer to the research question. On the other hand, title, author, country, year of publication, research methodology, objective and results were also registered.
The fourth phase considered data analysis. The analysis of the articles was carried out, emphasizing the inclusion criteria mentioned. Finally, the last phase was carried out with the presentation and interpretation of the results, which are presented in the following section.
Results and Discussion
Karlsson and his team observed that the patients in the terminal phase presented spring nursing problems, such as self-care deficit, affected physical mobility, risk of impaired skin integrity, risk of infection, unbalanced nutrition, fatigue, altered oral mucosa and pain. They also determined that the orientation of a Nursing model more accurately supports the identification of the main problems that people and their families present in the area of Palliative Care. In this way, the nursing model would demonstrate the necessary resources for timely care, being essential for the organization, planning and for the provision of priorities by Nursing13.
Contreras and collaborators investigated the reasons and meanings it has for the nurse to work with people in a Palliative Care program in Chile. A sociodemographic questionnaire and open questions were applied in a sample of 32 participants. It was then analyzed, using the Delphi method. The results indicate that nurses suggest that, in order to work in the area of Palliative Care, it is necessary to have commitment, knowledge and vocation. They say that they require more training since it is a complex area, especially in the area of mental health, where the emotional support that can be granted to this patient and their family becomes relevant14.
It has been observed that the suffering at the end of the life of institutionalized people in residences generates a strong impact on nurses, since it produces feelings of helplessness and inability to intervene in these situations. Therefore, care aimed at relieving suffering should involve not only the management of symptoms, but also the emotional response associated with the institutionalization of sick people15.
The results described above coincide with the findings of Pérez and Cibanal. In a qualitative research carried out in Mexico, the nurses' narratives realize that their personal self must be separated from their professional self, which generates great existential anguish. In their speeches, nurses also state that the importance of comprehensive patient support, which involves the family, health personnel and the institution. Therefore, the nurse's feelings and emotions must be linked or socialized with the rest of the actors, in other words, fear, anguish and despair are shared16.
Although nurses are the members of the health team that have the greatest contact with patients in the face of a life-limiting illness, they have few competencies in Palliative Care, which is the reason that is likely to affect the quality of care and quality life of people with such diseases17.
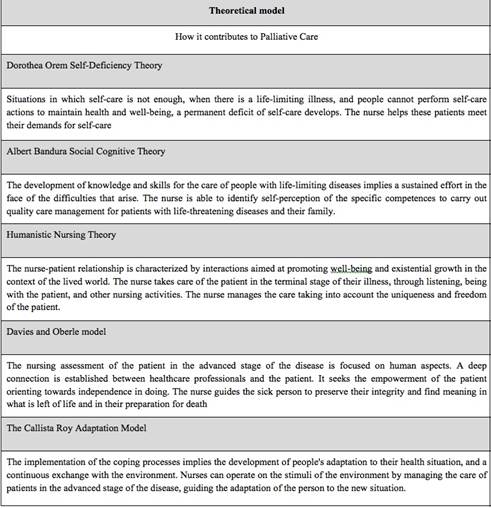
Among the theoretical works that have been explored, one of the most used has been the Dorothea Orem Self-Deficiency Theory, which can be applied to different contexts and in particular to Palliative Care. Orem proposes a classification of nursing care situations that includes seven groups, and in the final group represents the life-limiting disease. In this case, care focuses on the quality of life that is severely affected, until reaching the final stage of life. The central care becomes the maintenance of the comfort of the person in said stage18.
Along these lines, Orem's conceptual model is not only oriented towards end-of-life situations, but can also provide care for people with serious and long-term illnesses. Taking into account the deficit of self-care and the needs of sick people there are different types of nursing systems: fully compensatory, partially compensatory and educational-support system18. This type of system provides an indication of the degree of participation of the person in their personal care, to implement, regulate or refuse therapeutic care. The person or group can go through the different systems or activate several at the same time19.
In the partially compensatory system, partial support of nursing care is required, for reasons of limitation or disability. In this system, the nurse and the patient interact to meet the self-care needs of the latter. The patient can perform some basic personal care activities, such as hygiene and limited movement4. On the other hand, in the fully compensatory system, the person cannot perform any self-care activity, which translates into a total nursing unit. A final system is the so-called support education system. In this system, the individual needs guidance and instruction to carry out the self-care, so that the nurse advises, supports and educates the patient about the necessary measures so that the person can perform their self-care4.
Another theory used is the Humanistic Theory of Nursing, which highlights the link that is established between the nurse and the person receiving care. It is a nurse-patient meeting where both actors feel affected20. The philosophical perspectives of the Humanistic Theory of Nursing, according to Wu & Volker, are applicable to the practice of nursing in Palliative Care. The use of the basic concepts of the Humanistic Theory of Nursing can provide a common nomenclature for the different stages of the Nursing Process in Palliative Care21. The bond of trust and support of nurses with the person in the final stage of life is essential to promote the comfort of the person, encourage them in decision-making and promote the maintenance of dignity and quality of life in this last phase. Humanistic nursing is oriented towards the values and purposes of Palliative Care, and in this context, both the nurse and the people who receive care contribute their own perspectives in the nurse-patient encounter. In this way, the Humanistic Theory of Nursing orients the importance of caring, of developing empathy and the nurse-person encounter22.
Palliative Care favors the holism, dignity and quality of life of people who are at an advanced stage of the disease and their families. Figueiredo argues that the basic principles of the Humanist Theory of Nursing are appropriate for all professionals who care for people at the end of life, since they can provide a vision for nurses to empathize and respond to people who are close to their death22.
The Davies and Oberle model was developed with the purpose of describing the clinical component of the nurse's role in Palliative Care, the attributes of palliative nursing for practice and for training programs. The role of Nursing is oriented towards a supportive being with multiple dimensions: to be able to value, to be able to achieve connection, to be able to train and do, to be able to find the meaning and the preservation of one's integrity. This model considers that the nurse should not be separated from her self as a person23. Newton & McVicar investigated whether the nursing attributes described in the original model were still applied, but found no evidence to prove their application in current Palliative Care contexts24.
Another of the models that have been used in Palliative Care is the Callista Roy Model. Roy's Adaptation model argues that the person is an open and adaptive system that uses an input, processing and output sequence; that people adapt in relation to the internal and external stimuli that surround it and that respond to the factors that cause them stress individually, due to their changing characteristics25.
The coping processes involved in the course and development of adaptation that people carry out, include the use of a large amount of energy, which according to Roy could be used towards the recovery of the disease. In his theory, Roy considers people in a holistic way and argues that they are constantly interacting with the environment. The concept of adaptation implies that the person is an open system and responds to internal and external stimuli. The nurse's role in care translates into the manipulation of stimuli from the environment, with the aim of bringing them closer to the person's positive coping field. Adaptation is considered as the effective response to a stimulus26.
In this scenario, nurses act as external regulators, and detect inconsistent behaviors and their stimuli, from which they carry out the appropriate Nursing Process to eliminate or relieve the stimulus and thus guide towards adaptation27. There is evidence that the application of Roy's model has been used successfully in improving the quality of life of people with chronic diseases28. Research in the field of oncology in Western countries revealed various obstacles to the effective management of pain, such as: fear of addiction, fear of tolerance development, fear of side effects, and fatalistic beliefs, which could be explained through Roy's Adaptation Model29.
Taking up the Orem model, the authors Desbiens, Gagnon & Fillion, consider that this model seems to provide an adequate framework to guide the use of Albert Bandura's Social Cognitive Theory in the area of Palliative Care for nursing. According to the authors, who propose this shared theory, it defines the therapeutic relationship between nurses and people with advanced disease, in addition to providing a scenario for the development of nursing competencies in Palliative Care and improving the quality of care. Along the same lines, Desbiens argues that a shared theory could be useful as a framework in the evaluation of Palliative Care training programs for Nursing. This theory provides an approach to guide nurses in the development of competencies to give quality care to patients with diseases in terminal stages of the disease. It involves concepts of nursing competencies, self-competence, nursing interventions, self-care, physical and emotional symptoms and quality of life. All of them define the type of therapeutic relationship that will occur between the Palliative Care granted by the nurse and the patient at the end of their life28.
Sedillo explored the self-competence of Palliative Care in clinical aspects, interaction with the patient and their family and priorities in education, in 25 workers of a hospital service. The data were analyzed using the Kruskal-Wallis non-parametric statistical test. Most of the selected participants mentioned pediatric training in Palliative Care as their main priority for future education.
On the other hand, the results support the hypothesis that Palliative Care providers have different levels of self-competence. The clinical staff did not show greater self-competence in the use of parenteral opioid analgesics; use of adjuvant analgesics; evaluation of pain in the patient who is not responding or confused; or the evaluation and management of pediatric pain, when compared to other staff. All the clinical skills mentioned above are crucial for the management of symptoms and end-of-life care. Another important aspect to note is that the support health personnel: social workers, physical therapists and community workers, have greater self-competence when performing the basic pain assessment and also a better ability to explain the prognosis of end of life With family members. This result can be expected, as support staff reported more years of formal training in this area29. Table 1
Conclusions
The nurse discipline has models and theories applicable to the different care areas. However, an underutilization of these is evidenced through the publications. It is necessary to acquire knowledge in the application of theoretical frameworks that guide the Nursing Process and that are supported by the evidence, so that the Nursing discipline can optimize the care experience, improve the health of populations and reduce the cost per capita of care4.
It is also important to note that continuity of care is linked to the satisfaction of people who receive care and their quality of life. The appropriate follow-up of the care of people and the response to complex health problems in changing scenarios constitute a challenge that tests the adaptability of care and its professionals.
The currents that have contributed to the progress of nursing practice have been mainly oriented to the techniques of treatment of the disease, following the satisfaction of the needs of sick people and finally oriented towards health and its link with social and economic aspects.
Through the conceptual models of Nursing, a frame of reference for nursing practice is provided, focusing on the conceptual network of nursing formed by the categories: person, environment, health and nursing. The theoretical development of nurses has been undervalued and some of the aspects that have contributed to this reality are given because many nurses continue to cement their practice in the biomedical model, as was done at the beginning of the profession. This position is an obstacle to develop critical thinking and the advancement of nursing knowledge.
Some nurses do not recognize the relationship between theories and care practice; therefore there is a dissociation between both worlds. Apparently this starts from undergraduate training, since teachers other than those who supervise or teach clinical aspects of Nursing teach the models and theories. On the other hand, students consider that theories are only learned from academic professors and literature, while aspects of direct attention are acquired and developed together with clinical nurses.
Another aspect that has influenced the low use of nursing models and theories is that, in many contexts, the direct care of certain people has been delegated to auxiliary staff, while nurses have focused on administrative activities, the execution of the processes of standardization and standardization of quality, and ensuring the performance of indications of other professionals, which has been at the expense of disciplinary development.
Nurses, as integral professionals, who take care from a holistic perspective must possess competences in conceptual and technical aspects of their profession and discipline, in addition to the knowledge, skills, abilities and attitudes necessary to face the situations that arise and that help Improve the quality of care. Nursing is in a search for self-government, demonstrating to the world that it is a science, and that care constitutes a contribution to society. On the other hand, the democratization of knowledge through the Internet, the legislative changes that involve Nursing in the different countries of the world, protecting the exercise, defining roles and recognizing their role in improving the quality of life of people, promote the scientific development of the discipline through its own models and theories.
REFERENCES
1.World Health Organization. Global Atlas on Palliative Care At the End of Life (Internet) 2014 Available from: http://www.thewhpca.org/resources/global-atlas-on-end-of-life-care (Accessed: 2016-07-17) [ Links ]
2.Word Health Organization. Key facts (Internet) 2018 Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care (Accessed: 2019-06-22) [ Links ]
3.International Council of Nursing. Definition of Nursing. (Internet) 2002 Avalaible from: https://www.icn.ch/nursing-policy/nursing-definitions (Accessed: 2019-06-22) [ Links ]
4.Raile M. Nursing Theorists and Their Work. 8ª ed. Madrid: Elsevier Mosby; 2015. 829p. DOI: 10.1080/15524256.20 11.593152 [ Links ]
5.Hain,D. & Haras S. Changing Nephrology Nurses' Beliefs about the Value of Evidence-Based Practice and Their Ability to Implement in Clinical Practice. Nephrology Nursing Journal 2015; 42: 563-566. ISSN: 1526744X [ Links ]
6.Bornem T. Palliative Care Nursing. Current problems in cancer . 2011; 35: 351-356. DOI: 10.1016/j.currproblcancer.2011.10.009 [ Links ]
7.De Arco-Canoles OdelC, Suarez-Calle ZK. Rol de los profesionales de enfermería en el sistema de salud colombiano. Univ. Salud.2018;20(2):171-182. DOI: http://dx.doi.org/10.22267/rus.182002.121 [ Links ]
8.Hagan TL. Nursing's role in leading palliative care: A call to action. Nurs Educ Today. 2018; 61: 216-19. DOI: 10.1016/j.nedt.2017.11.037. [ Links ]
9.Johnston B. Dignity-conserving care in palliative care setting: An integrative review. Journal of Clinical Nursing.2015; 24:1743-1772. DOI: 10.1111/jocn.12791 [ Links ]
10.Östlund U. How to conserve dignity in palliative care: suggestions from older patients, significant others, and healthcare professionals in Swedish municipal care. BMC Palliative Care. 2019; 18:10. Available from: https://doi.org/10.1186/s12904-019-0393-x (Accessed 2019-06-23). [ Links ]
11.Crossetti MGO. Revisão integrativa de pesquisa na enfermagem o rigor cientifico que lhe é exigido (editorial). Rev Gaúcha Enferm., Porto Alegre (RS) 2012 jun;33(2):10-11. [ Links ]
12.Mamédio C, Andrucioli C, Cuce M. Estrategia PICO para la construcción de la pregunta de Investigación y la búsqueda de evidencia. Rev Latino-am Enfermagem. 2007; 15(3): 508-511. [ Links ]
13.Karlsson M. Community nurses' experiences of ethical problems in end-of-life care in the patient's own home. Scandinavian Journal of Caring Sciences.2013; 27:831-838. DOI: 10.1111/j.1471-6712.2012.01087 [ Links ]
14.Contreras S. Los pacientes del programa alivio del dolor y cuidados paliativos: razones y significados para enfermeras/os. (Patients of the pain relief and palliative care programme: reasons and meaning for nurses) Cienc. Enferm. 2016; 22: 47-63. DOI: 10.4067/S0717-95532016000100005. [ Links ]
15.Dobrina R. An overview of hospice and palliative care nursing models and theories. International Journal of Palliative Care, 2014; 20: 75-81. DOI: 10.12968/ijpn.2014.20.2.75 [ Links ]
16.Perez M.E. Perspectiva de la enfermera ante el paciente oncológico en fase terminal en Tampico, Tamaulipas, México. (Perspective from the nurse to the terminal cancer patient in Tampico, Tamaulipas, Mexico) Cultura de los Cuidados. 2011; 30: 52-59 DOI: 10.7184/cuid.2011.30.08 [ Links ]
17.Adams J. Nursing Roles and Strategies in End-of-Life Decision Making in Acute Care: A Systematic Review of the Literature. Research and Practice 2011; Article ID 527834, 15 pages. DOI: 10.1155/2011/527834 [ Links ]
18.Pina P. Self-care: Orem’s theoretical contribution to the Nursing discipline and profession Revista de Enfermagem Referência. 2014. 4:157-163 DOI: 10.12707/RIV14081 [ Links ]
19Johnston et al. .An exploration of self-management support in the context of palliative nursing: a modified concept analysis BMC Nursing 2014; 13:13:21. DOI: 10.1186/1472-6955-13-21 [ Links ]
20.Figueiredo de Sá França R. The importance of communication in pediatric oncology palliative care: focus on Humanistic Nursing Theory Rev. Latino-Am. Enfermagem. 2013; 21 :780-6. DOI: 10.1590/S0104-11692013000300018 [ Links ]
21.Wu H. L. & Volker D. L. Humanistic Nursing Theory: application to hospice and palliative care. Journal of advanced nursing.2012; 68: 471-479. DOI: 10.1111/j.1365-2648.2011.05770. [ Links ]
22.Figueiredo de Sá França R. Importance of Palliative Care in Pediatric Oncology. International Archives of Medicine.2016; 9: 1-10. DOI: 10.1590/S0104-11692013000300018. [ Links ]
23.Oberle K & Davies B. Support and caring: exploring the concepts. Oncology Nursing Forum.1992; 19: 763-767 [ Links ]
24.Newton J. Evaluation of the currency of the Davies and Oberle (1990) model of supportive care in specialist and specialised palliative care settings in England. Journal of Clinical Nursing. 2014. 23: 1662-1676 DOI: 10.1111/jocn.12301. [ Links ]
25.Badr Naga B. Roy Adaptation Model: Application of Theoretical Framework. Middle east journal of family medicine, Middle East Journal of Family Medicine.2014; 12: 48-51 [ Links ]
26.Fazel Asgarpoor, A. The effect of a care plan based on the Roy Adaptation Model on level of Fatigue in hemodialysis patients. Evidence Based Care.2011. 1: 77-90. DOI: 10.22038/ebcj.2011.3766 [ Links ]
27.Shahed S. Effect of an Educational-Supportive Program Based on Roy Adaptation Model on Marital Satisfaction in Mastectomy Patients Receiving Chemotherapy Journal of Evidence-based Care. 2016; 6: 71-78 DOI: 10.22038/ebcj.2016.6744 [ Links ]
28.Desbiens, J. Gagnon. Development of a shared theory in palliative care to enhance nursing competence. Journal of Advanced Nursing.2012; 68: 2113-2124. DOI: 10.1111/j.1365-2648.2011.05917 [ Links ]
29.Sedillo R A pilot study of palliative care provider self-competence and priorities for education in Kenya. /Journal of Hospice & Palliative Nursing. 2015 ; 17 : 356-363. DOI: 10.1097/NJH.0000000000000176 . [ Links ]
Received: February 05, 2019; Accepted: August 04, 2019











 text in
text in