Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.24 no.40 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22592/ode2022n40e318
Update
Regenerative treatment of intrabony defects using minimally invasive flaps: Scoping Review
1Facultad de Odontología, Universidad Andres Bello, Viña del Mar, Chile. mariajose.ossh@gmail.com
2Facultad de Odontología, Universidad Andres Bello, Viña del Mar, Chile. rodrigo.arayc@gmail.com
3Facultad de Odontología, Universidad de Valparaíso, Chile. jaime.segovia@uv.cl
Objective:
To analyze the clinical results of the regenerative treatment of intrabony defects using minimally invasive flaps in patients with periodontitis.
Methods
: A scoping review was conducted. Pubmed, Scopus, Ebsco Complete, and OpenGrey were searched for relevant articles and several clinical (probing depth, clinical insertion level, gingival margin recession) and radiographic indicators were evaluated. We also evaluated the flap design used, with a follow-up of at least six months.
Results:
Thirteen articles were included. We observed an average probing depth reduction of 4.69 mm, clinical attachment gain of 4.23 mm, and a recession of −0.44 mm. The groups treated with modified papilla preservation technique and entire papilla preservation technique presented better clinical results. The single-flap approach presented the largest recession.
Conclusion:
Minimally invasive flaps have excellent clinical results, without additional benefits with the adjunctive application of biomaterials.
Keywords: periodontal pocket; alveolar bone loss; intrabony defect; reconstructive surgical procedures; guided tissue regeneration; periodontal
Objetivo:
Analizar los resultados clínicos del tratamiento regenerativo de defectos intraóseos mediante colgajos mínimamente invasivos en pacientes con periodontitis.
Métodos:
Se realizó una revisión sistemática exploratoria o scoping review. Se buscaron artículos en las bases de datos Pubmed, Scopus, Ebsco Complete y OpenGrey, evaluándose indicadores clínicos (profundidad de sondaje, nivel de inserción clínica, recesión del margen gingival), radiográficos y el diseño de colgajo utilizado, con un seguimiento de al menos 6 meses.
Resultados:
13 artículos fueron incluidos, observando en promedio una reducción de profundidad de sondaje de 4,69 mm, ganancia de inserción de 4,23 mm, y una variación de la recesión de −0,44 mm. Los grupos intervenidos con Modified Papilla Preservation Technique y Entire Papilla Preservation Technique presentan mejores resultados clínicos. Single Flap Approach es el que presenta mayor recesión.
Conclusión:
Los colgajos mínimamente invasivos tienen excelentes resultados clínicos, sin beneficios adicionales con la aplicación conjunta de biomateriales.
Palabras clave: Cirugía Periodontal; Pérdida Ósea Alveolar; Defecto Intraóseo; Cirugía Reconstructiva; Regeneración Ósea Guiada
Objetivo:
Analisar os resultados clínicos do tratamento regenerativo de defeitos intraósseos por meio de retalhos minimamente invasivos em pacientes com periodontite.
Métodos:
Foi realizada uma revisão exploratória sistemática, onde se buscaram artigos nas bases de dados Pub Med, Scopus, Ebsco Complete e OpenGret, e se avaliaram vários indicadores clínicos (profundidade de sondagem, nivel de inserção clínica, ressecção da margem cervical), radiografias e o desenho do retalho utilizado, com um segmento de pelo menos 6 meses.
Resultados:
Foram incluídos 13 artigos, observando em promedio uma redução de profundidade de sondagem de 4,69 mm; aumento de inserção de 4,23 mm e uma variação de resseção de -0,44mm. Os grupos tratados com Modified Papila Preservation Technique e Entire Papila Preservation Technique foram os que apresentaram melhores resultados clínicos. O que apresentou maior resseção foi o Single Flap Approach.
Conclusão:
Os retalhos minimamente invasivos apresentam excelentes resultados clínicos, sem benefícios adicionais com a aplicação conjunta de biomateriais.
Palavras-chave: Cirurgia Periodontal; Perda Óssea Alveolar; Defeito Intraósseo; Cirurgia Reconstrutiva; Regeneração Óssea Guiada
Introduction and background
Periodontitis is a multifactorial chronic inflammatory disease associated with subgingival biofilm dysbiosis and the progressive destruction of the supporting tissues.1 Intrabony defects (IBD), also called “vertical defects,” are one of the sequelae of periodontitis, where the base of the periodontal pocket appears apical to the alveolar crest.2 These defects can be classified according to the morphology of the residual bone walls, defect width, and their topographic extension around the tooth, with one, two, or three residual walls surrounding the bone defect. Intrabony defects can be self-contained or not self-contained. Clinically, these IBD appear in relation to the associated loss of tooth support, in the specific site of periodontal destruction. Also, they act as ecological niches for periodontal pockets.3 The goal of periodontal treatment is to stop this progressive destruction by controlling infection, thus preventing tooth loss.4,5 However, periodontal pockets associated with IBD often remain, even after nonsurgical periodontal treatment (NSPT), thus increasing the risk of disease progression and worsening the prognosis. Therefore, surgical intervention is often considered a valid option.4
Current evidence shows the potential for tissue formation in IBD treated with guided tissue regeneration (GTR) using biological membranes placed in the affected site. This acts as a guide for the healing process.6-8 This results in the formation of new periodontal tissue, attachment, and alveolar bone, which can be measured clinically, radiographically, and histologically.2 Currently, GTR has become a clinically viable and more economical alternative to extraction and subsequent replacement of severely periodontally compromised teeth, even in complex cases, such as when the tooth apex is affected.9
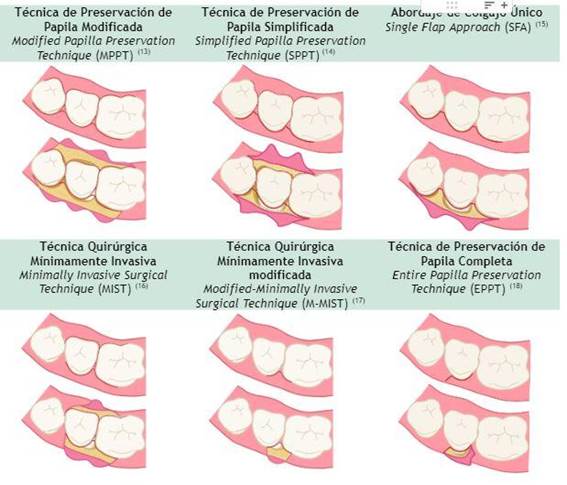
Minimally invasive treatment techniques have been developed with incisions that seek to maintain the integrity of the papilla by elevating more conservative flaps to access the IBD.10 This promotes healing, including minimal tissue trauma, low vascular impairment, healing by first intention, and clot stability.11,12 Papilla preservation flap (PPF) designs improve clinical outcomes compared to conventional access flaps and should be considered a surgical prerequisite in any regenerative procedure.2
Currently, the following flap designs are described within minimally invasive periodontal surgery (MIPS): modified papilla preservation technique (MPPT),13 simplified papilla preservation flap (SPPF),14 single-flap approach (SFA),15 minimally invasive surgical technique (MIST),16 modified minimally invasive surgical technique (M-MIST),17 and entire papilla preservation technique (EPPT).18
Current evidence cites MIPS’ clinical benefits and patient acceptance.2 However, despite multiple studies and reviews supporting the effectiveness of minimally invasive flaps over conventional access flaps, it is unknown which of these techniques provides better clinical results and whether the use of biomaterials favors their effectiveness.19,20 This study aims to analyze the clinical outcomes of intrabony defect regeneration using various minimally invasive flap designs.
Materials and methods
This systematic exploratory review or scoping review was written following the PRISMA-ScR statement (Preferred Reporting Items Systematic Review and Meta-Analyses extension for Scoping Reviews) protocol. We did not consider the possibility of registering the protocol in any database.
The following inclusion criteria were considered to include the articles in this review: randomized clinical trials (RCTs), controlled clinical trials (CCTs) and case series (CS), studies with humans treated with MIPS in IBD resulting from periodontal disease, at least six months postoperative follow-up, studies specifying clinical and/or radiographic outcomes, studies in English or Spanish.
The following exclusion criteria were also considered: studies that do not specify the flap design used, case reports or articles without detailed methodology and narrative reviews, publications that report data from previous studies by the same authors, studies that only report treatment in smokers, treatment of furcation lesions, or IBD of second molars due to impacted third molars.
The following literature databases were selected to identify potentially relevant articles: PubMed, Scopus, and Ebsco Complete. In addition, a grey literature search was performed through OpenGrey by authors MOS and RAC independently between 20 April and 3 June 2021. The final search results were exported into a reference manager and listed in a spreadsheet; duplicates were removed and confirmed manually. Any disagreement was resolved by a third-party reviewer (JSC).
Search strategy
An electronic search was performed according to the selected databases and the described protocol. The PubMed search was performed with the following combination of MeSH terms and free terms: ((“Periodontal Pocket/surgery” OR “Periodontal Pocket/therapy”) OR (“Alveolar Bone Loss/surgery” OR “Alveolar Bone Loss/therapy” ) OR (“intrabony defect”) OR (“infrabony defect”) OR (“intraosseous”) OR (“intra-osseous”) OR (“intra-bony”)) AND (“Reconstructive Surgical Procedures”) AND (“Guided Tissue Regeneration, Periodontal”) NOT “Dental Implants, Single-Tooth” NOT “Furcation Defects” NOT “Peri-Implantitis”.
The search strategy in the Scopus, EBSCO, and OpenGrey databases was performed using a combination of free terms: ((“Periodontal Pocket” AND (“Alveolar Bone Loss” OR “intrabony defect” OR “infrabony defect” OR “intraosseous” OR “intra-osseous” OR “intra-bony”)) AND (“Reconstructive Surgical Procedures” OR “Guided Tissue Regeneration” OR “entire papilla preservation” OR “papilla preservation” OR “simplified papilla preservation” OR “modified papilla preservation” OR “minimally invasive surgical” OR “modified minimally invasive surgical” OR “single flap approach”) NOT “furcation defect” NOT “implant” NOT “peri-implantitis” NOT “suprabony”).
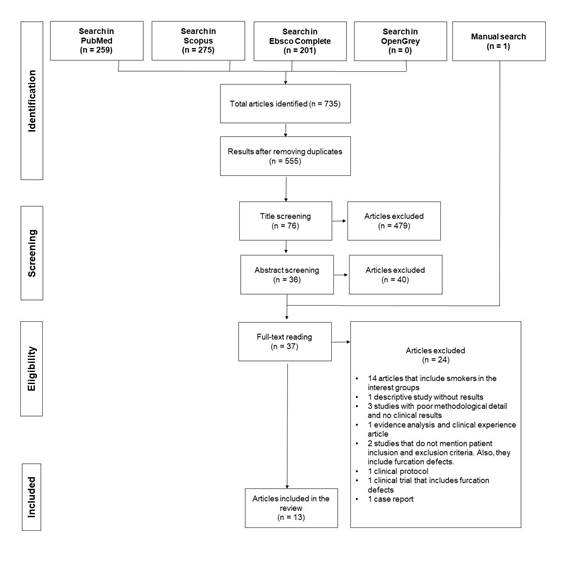
The search was limited to studies on humans, written in English or Spanish, and of the type defined in the inclusion criteria. A total of 735 articles were obtained from these four databases; duplicates were eliminated, leaving 555 documents.
Evidence selection was conducted independently by two reviewers (MOS and RAC) following these steps:
1. The articles initially identified after excluding duplicates (n=555) were listed in a data sheet. The documents were then selected after reading the titles (n=76).
2. After that, the reviewers screened the abstracts (n=36) to determine if they met the inclusion and exclusion criteria.
3. The eligibility of the potentially relevant full texts was decided by grouping them in a reference manager. The reviewers evaluated each full article for data extraction and final inclusion.
Disagreements were resolved under consensus and discussion with a third-party reviewer (JSC).
Data extraction and analysis
Data were extracted from all the selected studies that met the inclusion criteria and analyzed using a table with the characteristics of each article according to the variables to analyze.
We considered the following features when collecting and extracting the data: author, title and year, study design, number of patients and their characteristics (gender, age), type of intervention (details about the technique applied), follow-up, comparison (if any), clinical results according to variations in probing depth (PD), clinical attachment level (CAL), gingival margin recession (GMR), radiographic angle (RA), and radiographic bone level (RBL).
The two reviewers extracted data independently using a jointly designed table. The studies included in the table were then organized according to the flap design. The table includes the clinical results. The studies’ bias assessment was not considered.
Results
The complete search of the databases resulted in 735 articles. After title and abstract screening, 699 were excluded because they were off-topic. After reading the 36 articles fully, 24 were excluded because of their study design and methodology based on the inclusion criteria. Finally, one article was manually added, resulting in a total of 13 articles that were processed in data extraction and included in this paper.
Characteristics of information sources
Table 1 presents the characteristics of the selected articles.16,21-31 The groups that included smokers were not considered in the analysis of results. All included articles were published between 2007 and 2021; 244 patients were considered for this paper. Of the 13 studies, 4 reported a total follow-up of six months, 6 of 12 months, 1 of 15 months, 1 of 24 months, and the remaining 1 of 36 months.
Clinical results
MIST and M-MIST
MIST was used in six articles16,21,17,29,31 and 79 patients underwent surgery. The initial PD values recorded ranged from 7.07 to 8.00 mm, with an average reduction of 4.31 mm (3.51—5.00 mm). The initial CAL values ranged from 8.70 to 12.15 mm, with an average gain of 3.99 mm (2.85—4.80 mm). The initial GMR values ranged from 1.00 to 5.00 mm, with an average variation of −0.34 mm (−0.94 — 0.10 mm). One article included M-MIST and MIST, reporting statistically significant changes in baseline and postoperative values in each group. However, it concludes that another study design is required to compare both techniques.17
EPPT
EPPT was used in two articles 22,24 and 42 patients underwent surgery. The initial PD values recorded ranged from 9.26 a to 9.75 mm, with an average reduction of 6.57 mm (6.20 — 7.00 mm). The initial CAL values ranged from 11.40 to 12.25 mm, with an average gain of 6.32 mm (5.83—6.83 mm). The initial GMR values ranged from 2.13 to 2.50 mm, with an average variation of −0.24 mm (−0.36— −0.16 mm).
Table 1 Characteristics of the articles included
| Authors | Year | Design | Study group (male/female, average age, age range) | Treatment | Follow-up | Clinical and radiographic findings |
|---|---|---|---|---|---|---|
| Cortellini et al. 16 | 2007 | CSC | 13 (4/9; 43,10 ± 9,80 years; 34 - 63) | MIST + EMD | 12 months | PD, CAL, GMR, RA. |
| Ribeiro et al.21 | 2011 | RCTs | 14 (8/6; 45,43 ± 6,79 years; 35 - 57) | MIST | 3 months y 6 months | PD, CAL, GMR, RA. |
| 13 (4/9; 45,31 ± 7,57 years; 35 - 57) | MINST | |||||
| Aslan et al. 22 | 2020 | RCTs | 15 (8/7; 43,93 ± 12,85 years; 21 - 63) | EPP | 12 months | PD, CAL, GMR, RA, RBL. |
| 15 (10/5; 44,93 ± 13,06 years; 22 - 60) | EPPT + EMD + DBBM | |||||
| Corbella et al. 23 | 2019 | CCTs | 10 (3/2; 45,0 ± 11,4 years; #) | MPPT/SPPF + EMD | 12 months | PD, CAL, GMR, RBL. |
| 10 (1/5; 53,90 ± 14,1 years; #) | MPPT/SPPF + EMD + DBBM | |||||
| Aslan et al. 24 | 2017 | CSC | 12 (9/3; 42,60 ± 13,10 years; 22 - 60) | EPPT | 12 months | PD, CAL, GMR, RA, RBL. |
| Pilloni et al. 25 | 2021 | RCTs | 16 (8/8; 41,19 ± 8,49 years). | SFA + AH | 12, 18, and 24 months | PD, CAL, GMR. |
| 16 (7/9; 41,75 ± 10,22 years). | SFA + EMD | |||||
| Cortellini et al. 17 | 2009 | CCTs | 15 (6/9; 46,10 ± 10,30 years; 31 - 65) | M-MIST + EMD | 12 months | PD, CAL, GMR, RA, RBL. |
| 5 (2/3; 54 ± 9,00 years; 44 - 64) | MIST + EMD | |||||
| Miliauskaite et al. 26 | 2008 | CSC | 25 (11/14; #, 28 - 68) | MPPT/SPPF | 36 months | PD, CAL, GMR. |
| Trombelli et al. 27 | 2018 | ReCT | 11 (6/5; 56,80 ± 9,10; #) | SFA + EMD + DBBM | 6 months | PD, CAL, GMR, RBL. |
| 11 (8/3; 43,60 ± 9,80; #) | ||||||
| Trombelli et al. 28 | 2010 | RCTs | 12 (8/4; 56,30 ± 5; #) | SFA | 6 months | PD, CAL, GMR, RBL. |
| 12 (9/3; 45,60± 8,5; #) | SFA + AH/GTR | |||||
| Cortellini et al. 29 | 2008 | CSC | 20 (6/14; 49,7 ± 8,3; 35 - 63) | MIST + EMD | 12 months | PD, CAL, GMR, RA, RBL. |
| Oh et al. 30 | 2020 | CSC | 11 (6/5; 56 ± 17; 27 - 84) | SFA + DFDBA + Collagen | 15 months | PD, CAL, GMR, RBL. |
| Ribeiro et al. 31 | 2010 | CSC | 12 (5/7; 47.4 ± 7.0,#) | MIST + EMD | 6 months | PD, CAL, GMR, RBL. |
Abbreviations: RA, radiographic angle; DBBM, deproteinized bovine bone material; DFDBA, demineralized freeze-dried bone allograft; RCT, randomized clinical trial; CCT, controlled clinical trial; ReCT, retrospective clinical trial; EMD, enamel matrix derivative; EPPT, entire papilla preservation technique; GTR, guided tissue regeneration; HA, hyaluronic acid; MINST, minimally invasive nonsurgical approach; MIST, minimally invasive surgical approach; MPPT, modified papilla preservation technique; CAL, clinical attachment level; RBL, radiographic bone level; PD, probing depth; GMR, gingival margin recession; CSC, case series cohort; SFA, single flap approach; SPPF, simplified papilla preservation flap.
MPPT and SPPF
These flaps were included in two articles.23,26 Forty-five patients underwent surgery. The initial PD values recorded ranged from 5.90 to 8.60 mm, with an average reduction of 4.6 mm (3.20 — 5.90 mm). The initial CAL values ranged from 6.60 to 11.40 mm, with an average gain of 4.03 mm (3.20 — 4.50 mm). The initial GMR values ranged from 0.71 to 2.80 mm, with a mean variation of −0.41 mm (−0.70 — 0.07 mm). Corbella et al.23 had positive clinical results for each group and found no significant differences between the two groups. Miliauskaite et al.26 conclude that there is a statistically significant reduction in PD (p<0.001) and CAL (p<0.001).
SFA
It was included in four articles.25,27,28,30 Sixty-six patients underwent surgery. In two studies,27,28) the groups that included smokers were not considered in the results. The initial PD values recorded ranged from 7.25 to 8.50 mm, with an average reduction of 4.60 mm (3.12 — 5.30 mm). The initial CAL values ranged from 7.37 to 10.10 mm, with an average gain of 3.29 mm (2.43 — 4.40 mm). The initial GMR values ranged from 0.06 to 2.40 mm, with a mean variation of −0.74 mm (−1.13 — −1.50 mm).
All flap designs
In 17 study groups, the mean PD reduction was 4.69 mm, the mean CAL gain was 4.23 mm, and the mean recorded GMR variation was −0.44 mm. Regarding PD and CAL values, the groups treated with MPPT and EPPT showed an average above the mean of all groups. Regarding GMR, SFA was the flap technique that presented the greatest recession. Table 2 presents the individual clinical outcomes of the articles included.
Radiographic findings
Only two articles23,30 included their results on the final bone level and the resulting difference compared to the initial level. These results are shown in Table 3. One article describes a significant association between CAL gain and the distance between the cementoenamel junction (CEJ) and the bottom of the defect (BD) (p < 0.0001) and with the initial defect angle (p = 0.0038).29 Corbella et al.23 reported no significant radiographic difference between the bone substitute (BS) group and the control group. In contrast, Oh et al.30 reported a statistically significant reduction of ID radiographically (CEJ-BD) (p = 0.0015).
Use of biomaterials and biological agents
The application of enamel-derived matrix (EMD) in the bone defect was recorded in ten articles. For the flaps, they used MIST, M-MIST, EPPT, MPPT, SPPF, and SFA. Hyaluronic acid (HA) was used in one of the cohort groups in conjunction with SFA.25 Regarding BS, deproteinized inorganic bovine bone (DBBM) was used in conjunction with EMD in four studies.22-24,27 In one study, demineralized freeze-dried bone (DFDBA) was used in conjunction with collagen to treat ID.30 The studies that assessed the results of EMD and BS concluded that applying different biomaterials and biological agents did not result in a statistically significant improvement in clinical and radiographic outcomes compared to the control group.
Table 2 Clinical results of the studies included
| Study | Design | Treatment | Number of patients | Follow-up | Clinical results | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PD (mm) | CAL (mm) | GMR (mm) | |||||||||||
| initial | final | delta | initial | final | delta | initial | final | delta | |||||
| Ribeiro et al. 21 | RCTs | MIST | 14 | 6 m | 7.07 ± 1.13 | 3.56 ± 0.84 | 3.51 ± 0.90 | 10.73 ± 1.56 | 7.88 ± 1.46 | 2.85 ± 1.19 | 3.74 ± 1.09 | 4.22 ± 1.06 | 0.48 ± 0.51 |
| Cortellini et al. 16 | CSC | MIST + EMD | 13 | 12 m | 7.70 ± 1.80 | 2.90 ± 0.80 | 4.80 ± 1.80 | 8.70 ± 2.70 | 3.80 ± 2.20 | 4.80 ± 1.90 (3-8) | 1.00 ± 1.50 | 0.90 ± 2.10 | 0.10 ± 0.90 |
| Ribeiro et al. 31 | CSC | MIST + EMD | 12 | 6 m | 7.21 ± 1.67 | 3.58 ± 1.11 | 3.63 ± 2.23 | 12.15 ± 2.19 | 9.04 ± 2.49 | 3.10 ± 2.02 | 5.0 ± 1.89 | 5.94 ± 2.45 | 0.94 ± 1.59 |
| Cortellini et al. 29 | CSC | MIST + EMD | 20 | 12 m | 7.10 ± 1.40 | 2.50 ± 0.60 | 4.60 ± 1.30 | 8.70 ± 1.70 | 4.30 ± 1.10 | 4.40 ± 1.40 | 1.60 ± 1.00 | 1.80 ± 1.00 | - 0.20 ± 0.60 |
| Cortellini et al. 17 | CCTs | M-MIST + EMD | 15 | 12 m | 7.70 ± 1.50 | 3.07 ± 0.60 | 4.60 ± 1.50 | 9.70 ± 1.80 | 5.13 ± 1.00 | 4.50 ± 1.40 | 2.00 ± 1.30 | 2.07 ± 1.30 | 0.07 ± 0.30 |
| MIST + EMD | 5 | 8.00 ± 1.90 | 3.00 ± 0.70 | 5.00 ± 2.40 | 10.00 ± 2.90 | 5.20 ± 0.80 | 4.80 ± 2.40 | 2.00 ± 1.20 | 2.20 ± 1.10 | 0.20 ± 0.50 | |||
| Aslan et al. 22 | RCTs | EPP | 15 | 12 m | 9.26 ± 1.65 | 3.06 ± 0.79 | 6.20 ± 1.33 | 11.40 ± 2.17 | 5.56 ± 1.74 | 5.83 ± 1.12 | 2.13 ± 1.12 | 2.50 ± 1.40 | -0.20 ± 0.25 |
| EPP + EMD + DBBM | 15 | 9.33 ± 2.87 | 2.83 ± 0.74 | 6.5 ± 2.65 | 11.66 ± 3.45 | 5.36 ± 1.85 | 6.3 ± 2.5 | 2.33 ± 1.23 | 2.53 ± 1.36 | -0.36 ± 0.54 | |||
| Aslan et al. 24 | CSC | EPP + EMD + DPBM | 12 | 12 m | 9.75 ± 3.07 | 2.75 ± 0.75 | 7.00 ± 2.80 | 12.25 ± 3.64 | 5.41 ± 2.02 | 6.83 ± 2.51 | 2.50 ± 1.31 | 2.66 ± 1.55 | -0.16 ± 0.38 |
| Corbella et al. 23 | CCTs | MPPT/SPPF + EMD | 10 | 12 m | 7.70 ± 2.30 | 6 m: 3.30 ± 1.80 12 m: 2.80 ± 0.80 | 12 m: 4.90 ± 3.00 | 9.40 ± 3.10 | 6 m: 5.90 ± 2.60 12 m: 5.00 ± 2.80 | 4.40 | 1.70 ± 2.10 | 6 m: 260 ± 2.30 12 m: 2.30 ± 2.40 | 12 m: 0.60 ± 1.10 |
| MPPT/SPPF + EMD + DBBM | 10 | 8.60 ± 1.60 | 6 m: 3.00 ± 0.90 12 m: 3.0 ± 0.70 | 12 m: 5.90 ± 1.60 | 11.40 ± 3.50 | 6 m: 7.10 ± 1.20 12 m: 6.90 ± 1.10 | 4.50 | 2.80 ± 2.40 | 6 m: 4.10 ± 1.30 12 m: 3.90 ± 1.50 | 12 m: 0.70 ± 2.30 | |||
| Miliauskaite et al. 26 | CSC | MPPT/SPPF + EMD | 25 | 36 m | 5.90 ± 1.00 | 2.70 ± 0.80 | 3.20 | 6.60 ± 1.20 | 3.40 ± 1.30 | 3.20 | 0.71 ± 1.20 | 0.64 ± 1.10 | 0.07 |
| Pilloni et al. 25 | RCTs | SFA + HA | 16 | 12, 18, and 24 m | 7.31 ± 0.27 | 12 m: 4.18 ± 0.81 18 m: 4.12 ± 1.14 24 m: 4.00 ± 1.09 | # 3.12 | 7.37 ± 0.88 | 12 m: 4.94 ± 1.06 18 m: 5.19 ± 1.28 24 m: 5.19 ± 1.42 | # 2.43 | 0.06 ± 0.68 | 12 m: 0.75 ± 0.58 18 m: 1.06 ± 0.57 24 m: 1.19 ± 0.75 | # -0.69 |
| SFA + EMD | 16 | 7.25 ± 0.93 | 12 m: 3.00 ± 1.22 18 m: 2.87 ± 0.80 24 m: 2.75 ± 0.57 | # 4.25 | 7.37 ± 0.96 | 12 m: 4.25 ± 1.29 18 m: 4.31 ± 1.08 24 m: 4.44 ± 1.03 | # 3.12 | 0.12 ± 0.62 | 12 m: 1.25 ± 0.69 18 m: 1.44 ± 0.63 24 m: 1.69 ± 0.70 | # -1.13 | |||
| Trombelli et al. 27 | ReCT | SFA + EMD + DBBM | 11 | 6 m | 7.7 ± 1.2 | 3.6 ± 0.9 | 4.1 ± 1.1 | 10.10 ± 2.50 | 6.50 ± 2.00 | 3.50 ± 0.90 | 2.40 ± 2.20 | 2.90 ± 1.60 | - 0.50 ± 1.00 |
| Trombelli et al. 28 | RCTs | SFA + HA | 12 | 6 m | 8.5 ± 1.8 | 3.3 ± 0.6 | 5.3 ± 1.5 | 9.20 ± 2.40 | 4.8 ± 1.5 | 4.4 ± 1.5 | 0.7 ± 0.9 | 1.5 ± 1.1 | -0.8 ± 0.8 |
| SFA + HA/GTR | 12 | 6 m | 9.1 ± 2.6 | 3.8 ± 1.3 | 5.3 ± 2.4 | 11.4 ± 2.4 | 6.4 ± 1.7 | 4.7 ± 2.5 | 2.1 ± 1.7 | 2.5 ± 1.3 | -0.4 ± 1.4 | ||
| Oh et al. 30 | CSC | SFA + DFDBA + Collagen | 11 | 15 m | 7.3 ± 2.0 | 4.1 ± 1.0 | # 3.2 | 8.80 ± 2.00 | 5.80 ± 2.00 | 3.00 | 1.30 ± 1.80 | 1.90 ± 1.50 | -0.6 |
Abbreviations: DBBM, deproteinized bovine bone material; DFDBA, demineralized freeze-dried bone allograft; RCT, randomized clinical trial; CCT, controlled clinical trial; EMD, enamel-derived matrix; EPPT, entire papilla preservation technique; HA, hyaluronic acid; MINST, minimally invasive nonsurgical technique; MIST, minimally invasive surgical approach; MPPT, modified papilla preservation technique; CAL, clinical attachment level; PD, probing depth; GMR, gingival margin recession; CSC, case series cohort; SFA, single flap approach; SPPF, simplified papilla preservation technique.
Table 3 Radiographic results of the studies included
| Study | Design | Treatment | Number of patients | Follow-up | Radiographic findings | |||
|---|---|---|---|---|---|---|---|---|
| Rx angle | Radiographic bone level | |||||||
| initial | final | difference | ||||||
| Ribeiro et al. 31 | CSC | MIST + EMD | 12 | 6 m | # | CEJ-BD: 7.88 ± 1.57 IBD: 5.25 ± 1.76 | # | # |
| Cortellini et al. 29 | CSC | MIST + EMD | 20 | 12 m | 33.70 ± 6.40 | INFRA: 5.50 ± 1.80 CEJ-BD: 9.90 ± 2.10 | # | # |
| Cortellini et al. 17 | CCTs | M-MIST + EMD | 15 | 12 m | 32.10 ± 4.10 | INFRA: 6.00 ± 1.50 CEJ-BD: 11.10 ± 2.30 | # | # |
| MIST + EMD | 5 | 33.20 ± 11.10 | INFRA: 6.00 ± 1.90 CEJ-BD: 11.20 ± 2.80 | # | # | |||
| Aslan et al. 22 | RCTs | EPP | 15 | 12 m | 29.33 ± 9.48 º | INFRA: 6.7 ± 1.62 CEJ-BD: 12.48 ± 2.12 | # | # |
| EPP + EMD + DBBM | 15 | 28.8 ± 8.76 º | INFRA: 6.63 ± 2.74 CEJ-BD: 12.8 ± 3.50 | # | # | |||
| Aslan et al. 24 | CSC | EPP + EMD + DPBM | 12 | 12 m | 28.20 ± 9.60º | INFRA: 7.08 ± 2.87 CEJ-BD: 13.30 ± 3.60 | # | # |
| Corbella et al. 23 | CCTs | MPPT/SPPF + EMD | 10 | 12 m | # | INFRA: 4.40 ± 1.50 CEJ-BD: 8.80 ± 2.40 | 6 m INFRA: 2.80 ± 1.20 CEJ-BD: 7.20 ± 2.30 12 m INFRA: 1.80 ± 1.10 CEJ-BD: 6.10 ± 2.30 | 12 m CEJ-BD: 3.90 ± 3.20 12 m INFRA: 3.00 ± 1.70 |
| MPPT/SPPF + EMD + DBBM | 10 | # | INFRA: 5.40 ± 2.10 CEJ-BD: 12.20 ± 2.70 | 6 m INFRA: 1.50 ± 1.70 CEJ-BD: 7.10 ± 2.60 12 m INFRA: 1.60 ± 1.00 CEJ-BD: 6.10 ± 2.40 | 12 m CEJ-BD: 5.50 ± 3.10 12 m INFRA: 3.40 ± 2.50 | |||
| Oh et al. 30 | CSC | SFA + DFDBA + Collagen | 11 | 15 m | # | CEJ-BD: 8.2 ± 3.0 | CEJ-BD: 6.3 ± 3.0 | 1.9 ± 1.8 |
Abbreviations: CEJ-BD, cementoenamel junction and bottom of the defect; DBBM, deproteinized bovine bone material; DFDBA, demineralized freeze-dried bone allograft; RCT, randomized clinical trial; CCT, controlled clinical trial; EMB, enamel-derived matrix; EPPT, entire papilla preservation technique; HA, hyaluronic acid; IBD, intrabony defect; INFRA, intrabony component depth; MINST, minimally invasive nonsurgical technique; MIST, minimally invasive surgical approach; MPPT, modified papilla preservation technique; CS, case series; SFA, single-flap approach; SPPF, simplified papilla preservation technique.
Discussion
This review analyzes the clinical results of the different flap designs in MIPS on IBD. The articles that included smokers in any of their study groups were discarded because the literature shows the effects of tobacco smoking on healing.32-35) The results studied from each flap design proved effective in treating IBD. While each flap design offers similar CAL gain and PD reduction results, the EPPT flap shows the best results with averages of 6.06 mm CAL gain and a 6.35 mm PD reduction. A case series published by the same author reports results similar to those in this review.36 EPPT is a new technique proposed in 2017 by Aslan to treat deep IBD. Its design includes a single vertical incision contralateral to the bone defect ensuring adequate access to fully preserve the interdental papilla, thus ensuring optimal healing conditions.18,36 In addition, we posit that applying this design could favor healing stability: recent studies and those included in this review report a 100% rate of primary closure.22,24,36 This improves the stability of the biomaterial and the clot formed inside the defect.18 The good clinical results might result from the strict indications for this procedure and the characteristics that the defect must have in terms of extension and depth.18,37 Still, the evidence for EPPT is scarce; to our knowledge, only one randomized clinical trial,22three case series 18,24,36 and one narrative review37 have been published, and no published clinical trials compare it with other designs.
A slight GMR increase was recorded, which is consistent with other articles.10,38 Also, various studies show that the sites treated with MIPS show comparable results to those treated with nonsurgical procedures.21,39 A long-term study shows that papillary recession in sites treated with PPF shows no significant changes compared to baseline values and remains stable over 15 and 20 years,40 probably due to the inherent characteristics of flap designs. Conversely, studies evaluating the position of the gingival margin in sites treated with traditional flaps report increased recession, up to a maximum of 2 mm, resulting in higher values than those of NSPT.41,42
Therefore, traditional surgical therapies show higher recession rates when compared to MIPS or NSPT. This increased recession could be explained by the reduction in pocket depth and the contraction of the periodontal tissues after periodontal therapy. This promotes adaptation, the reconstruction of the supracrestal attachment apparatus, and the formation of the long junctional epithelium, so gingival recession can be considered part of the healing response.42,43 The effectiveness in the clinical results associated with GMR in MIPS is attributed to the stability and intimate adaptation of the flap and to the blood flow of the papilla adjacent to the defect. Several authors propose the latter.17,40,44,45 Retzepi et al. compared gingival blood flow during SPPF and modified Widman flap healing using laser Doppler flowmetry in patients with periodontal disease. In the SPPF flap, a more favorable vascular flow response and a hyperemic resolution was observed, both in the peripheral mucosal sites of the flap and in the papillary mucosa. The authors conclude that this design positively affects the recovery of gingival blood flow.46
Regarding the use of biomaterials and biological agents, our results concluded that adding EMD in CPMI does not improve clinical or radiographic outcomes significantly. EMD is the most widely used biological agent in studies reviewed, and its application as proteins for regenerating bone defects has been studied extensively.47-50 Sculean et al. detail the effects of EMD application on periodontal regeneration and healing. They conclude that applying EMD with traditional flaps significantly improves defect filling compared to conventional flap debridement alone.51 This is strongly supported in several articles.52-54 In contrast, and in agreement with our results, other studies conclude that there is no significant difference in the additional application of biomaterials in CPMI.55-56 Similar findings are reported by Liu et al. They assessed the clinical differences of EMD application in IBD through minimally invasive access.57 They found no significant difference in clinical and radiographic outcomes after one year of follow-up. This could be caused by structuring the flap with minimal soft tissue extension and elevation. This minimizes vascular damage and makes the clot more stable, providing an ideal environment for the healing process.45,57 The same authors report a primary closure close to 100% after one week, which, jointly with the extraordinary clinical healing capacity observed in PPF, would explain the statistically non-significant results regarding the application of minimally invasive surgery with and without biomaterial.57
One of the main limitations of this scoping review may be that the search was limited to homogeneous groups of studies when the evidence for CPMI is new, and the current publications are scarce and heterogeneous. For instance, only EPPT articles published to date were analyzed and written by the same professional, who also proposed this flap design. This limits the reproducibility and generalized interpretation of the results.
The results analyzed call for future studies to assess the number of IBD walls and their implication in the results. In addition, trials including smokers should report individualized results in order to make comparisons and assess the effectiveness of MIPS under these conditions. We also suggest that the gingival phenotype be evaluated before the intervention to observe GMR variations and their implication.
Regarding the current limited evidence, no RCTs compare the clinical performance of various minimally invasive flap designs, nor is there a classification system for IBD that considers the variables of the defect itself to help determine the most appropriate minimally invasive surgical strategy for each case.
Conclusions
Minimally invasive flap designs applied in MIPS are effective for treating IBD as they offer additional clinical advantages to traditional flaps in terms of decreased PD, CAL gain, and a slight increase in GMR. Furthermore, it is clear that applying biomaterials in MIPS procedures provides no additional benefits, which translates into a decrease in surgical intervention costs. Therefore, MIPS should be considered as the first line of treatment for multiple and isolated periodontal IBD in the area of periodontal regeneration.
Acknowledgments
To our moms, dads, and family for being our emotional support throughout our degree studies. To our “La Fístula” followers for making this journey more enjoyable
REFERENCES
1. Sanz M, Tonetti M. Introduction : classifying periodontitis. Eur Fed Periodontol. 2019;(March):1-9. [ Links ]
2. Nibali L, Koidou VP, Nieri M, Barbato L, Pagliaro U, Cairo F. Regenerative surgery versus access flap for the treatment of intra-bony periodontal defects: A systematic review and meta-analysis. J Clin Periodontol. 2020;47(S22):320-51. [ Links ]
3. Papapanou PN, Tonetti MS. Diagnosis and epidemiology of periodontal osseous lesions. Periodontol 2000. 2000;22(1):8-21. [ Links ]
4. Mancini L, Adriano F, Marchetti E. Periodontal Regeneration. Encyclopedia MDPI 2021 ;1:87-98. [ Links ]
5. Ryder MI, Armitage GC. Minimally invasive periodontal therapy for general practitioners. Periodontol 2000. 2016;71(1):7-9. [ Links ]
6. Reynolds MA, Kao RT, Nares S, Camargo PM, Caton JG, Clem DS, et al. Periodontal Regeneration - Intrabony Defects: Practical Applications From the AAP Regeneration Workshop. Clin Adv Periodontics. 2015;5(1):21-9. [ Links ]
7. Nibali L, Sultan D, Arena C, Pelekos G, Lin GH, Tonetti M. Periodontal infrabony defects: Systematic review of healing by defect morphology following regenerative surgery. J Clin Periodontol. 2021;48(1):100-13. [ Links ]
8. Stavropoulos A, Bertl K, Spineli LM, Sculean A, Cortellini P, Tonetti M. Medium- and long-term clinical benefits of periodontal regenerative/reconstructive procedures in intrabony defects: Systematic review and network meta-analysis of randomized controlled clinical studies. J Clin Periodontol. 2021;48(3):410-30. [ Links ]
9. Cortellini P, Buti J, Pini Prato G, Tonetti MS. Periodontal regeneration compared with access flap surgery in human intra-bony defects 20-year follow-up of a randomized clinical trial: tooth retention, periodontitis recurrence and costs. J Clin Periodontol. 2017;44(1):58-66. [ Links ]
10. Clementini M, Ambrosi A, Cicciarelli V, De Risi V, de Sanctis M. Clinical performance of minimally invasive periodontal surgery in the treatment of infrabony defects: Systematic review and meta-analysis. J Clin Periodontol. 2019;46(12):1236-53. [ Links ]
11. Trombelli L, Simonelli A, Quaranta A, Tu YK, Li H, Agusto M, et al. Effect of Flap Design for Enamel Matrix Derivative Application in Intraosseous Defects. JDR Clin Transl Res. ahead of print 2020:1-11. [ Links ]
12. Sultan N, Jafri Z, Sawai M, Bhardwaj A. Minimally invasive periodontal therapy. J Oral Biol Craniofacial Res. 2020;10(2):161-5. Available from: https://doi.org/10.1016/j.jobcr.2020.04.014 [ Links ]
13. Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J. Periodontol. 1995; 66: 261-266. [ Links ]
14. Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restor Dent. 1999; 19:589-599. [ Links ]
15. Trombelli L, Farina R, Franceschetti G. Use of the single flap approach in periodontal reconstructive surgery. Dent. Cadmos. 2007; 8:15-25. [ Links ]
16. Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intrabony defects: A novel approach to limit morbidity. J Clin Periodontol. 2007;34(1):87-93. [ Links ]
17. Cortellini P, Tonetti MS. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol. 2009;36(2):157-63. [ Links ]
18. Aslan S, Buduneli N, Cortellini P. Entire Papilla Preservation Technique: A Novel Surgical Approach for Regenerative Treatment of Deep and Wide Intrabony Defects. Int J Periodontics Restorative Dent. 2017;37(2):227-33. [ Links ]
19. Wu YC, Lin LK, Song CJ, Su YX, Tu YK. Comparisons of periodontal regenerative therapies: A meta-analysis on the long-term efficacy. J Clin Periodontol. 2017;44(5):511-9. [ Links ]
20. Graziani F, Gennai S, Cei S, Cairo F, Baggiani A, Miccoli M, et al. Clinical performance of access flap surgery in the treatment of the intrabony defect. A systematic review and meta-analysis of randomized clinical trials. J Clin Periodontol. 2012;39(2):145-56. [ Links ]
21. Ribeiro FV, Casarin RCV, Palma MAG, Júnior FHN, Sallum EA, Casati MZ. Clinical and Patient-Centered Outcomes After Minimally Invasive Non-Surgical or Surgical Approaches for the Treatment of Intrabony Defects: A Randomized Clinical Trial. J Periodontol. 2011;82(9):1256-66. [ Links ]
22. Aslan S, Buduneli N, Cortellini P. Clinical outcomes of the entire papilla preservation technique with and without biomaterials in the treatment of isolated intrabony defects: A randomized controlled clinical trial. J Clin Periodontol. 2020;47(4):470-8. [ Links ]
23. Corbella S, Alberti A, Calciolari E, Taschieri S, Francetti L. Enamel matrix derivative for the treatment of partially contained intrabony defects: 12-month results. Aust Dent J. 2019;64(1):27-34. [ Links ]
24. Aslan S, Buduneli N, Cortellini P. Entire papilla preservation technique in the regenerative treatment of deep intrabony defects: 1-Year results. J Clin Periodontol. 2017;44(9):926-32. [ Links ]
25. Pilloni A, Rojas MA, Marini L, Russo P, Shirakata Y, Sculean A, et al. Healing of intrabony defects following regenerative surgery by means of single-flap approach in conjunction with either hyaluronic acid or an enamel matrix derivative: a 24-month randomized controlled clinical trial. Clin Oral Investig. 2021; 25(8):5095-5107. [ Links ]
26. Miliauskaite A, Selimovic D, Hassan M, Nagano F, Soell M, Sano H, et al. Papilla preservation technique combined with Emdogain in the treatment of intrabony defects: a novel treatment regimen for chronic periodontitis. Stomatologija. 2008;10(1):22-6. [ Links ]
27. Trombelli L, Farina R, Minenna L, Toselli L, Simonelli A. Regenerative periodontal treatment with the single flap approach in smokers and nonsmokers. Int J Periodontics Restor Dent. 2018;38(4):e59-67. [ Links ]
28. Trombelli L, Simonelli A, Pramstraller M, Wikesjö UME, Farina R. Single Flap Approach With and Without Guided Tissue Regeneration and a Hydroxyapatite Biomaterial in the Management of Intraosseous Periodontal Defects. J Periodontol. 2010;81(9):1256-63. [ Links ]
29. Cortellini P, Nieri M, Pini Prato G, Tonetti MS. Single minimally invasive surgical technique with an enamel matrix derivative to treat multiple adjacent intra-bony defects: Clinical outcomes and patient morbidity. J Clin Periodontol. 2008;35(7):605-13. [ Links ]
30. Oh SL, Joshi S. Single-Flap Approach in Periodontal Regeneration for Intraosseous Defects: Case Series. Clin Adv Periodontics. 2020 Jun 1;10(2):69-74. [ Links ]
31. Ribeiro FV, Nociti Júnior FH, Sallum EA, Sallum AW, Casati MZ. Use of enamel matrix protein derivative with minimally invasive surgical approach in intra-bony periodontal defects: Clinical and patient-centered outcomes. Braz Dent J. 2010;21(1):60-7. [ Links ]
32. Trombelli L, Farina R, Minenna L, Toselli L, Simonelli A. Regenerative Periodontal Treatment with the Single Flap Approach in Smokers and Nonsmokers. Int J Periodontics Restorative Dent. 2018 Jul;38(4):e59-67. [ Links ]
33. Tatsumi M, Yanagita M, Yamashita M, Hasegawa S, Ikegami K, Kitamura M, et al. Long-term exposure to cigarette smoke influences characteristics in human gingival fibroblasts. J Periodontal Res. 2021;56(5):951-63. [ Links ]
34. Alanazi H, Park HJ, Chakir J, Semlali A, Rouabhia M. Comparative study of the effects of cigarette smoke and electronic cigarettes on human gingival fibroblast proliferation, migration and apoptosis. Food Chem Toxicol . 2018;118(May):390-8. https://doi.org/10.1016/j.fct.2018.05.049 [ Links ]
35. Chaffee BW, Couch ET, Ryder MI. The tobacco-using periodontal patient: The role of the dental practitioner in tobacco cessation and periodontal diseases management Benjamin. HHS Public Heal. 2017;71(1):52-64. [ Links ]
36. Aslan S, Buduneli N, Cortellini P. Reconstructive surgical treatment of isolated deep intrabony defects with guided tissue regeneration using entire papilla preservation technique: A prospective case series. J Periodontol. 2020;(May):1-8. [ Links ]
37. Pei X. New surgery approaches preserving entire papilla to treat isolated interdental intrabony defects: A narrative review. Clin Exp Dent Res. 2021;(November 2020):1-7. [ Links ]
38. Windisch P, Iorio-Siciliano V, Palkovics D, Ramaglia L, Blasi A, Sculean A. The role of surgical flap design (minimally invasive flap vs. extended flap with papilla preservation) on the healing of intrabony defects treated with an enamel matrix derivative: a 12-month two-center randomized controlled clinical trial. Clin Oral Investig 2021;(0123456789). https://doi.org/10.1007/s00784-021-04155-5 [ Links ]
39. Aimetti M, Ferrarotti F, Mariani GM, Romano F. A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: a 24-month randomized controlled clinical trial. Clin Oral Investig. 2017;21(1):327-37. [ Links ]
40. Isidor F, Karring T. Long-term effect of surgical and non-surgical periodontal treatment. A 5-year clinical study. J Periodontal Res. 1986;21(5):462-72. [ Links ]
41. Froum SJ, Weinberg MA, Rosenberg E, Tarnow D. A Comparative Study Utilizing Open Flap Debridement with and Without Enamel Matrix Derivative in the Treatment of Periodontal Intrabony Defects: A 12-Month Re-Entry Study. J Periodontol. 2001;72(1):25-34. [ Links ]
42. Tugnait A, Clerehugh V. Gingival recession its significance and management. J Dent 2001;29 (6): 381-394 [ Links ]
43. Trombelli L, Simonelli A, Minenna L, Vecchiatini R, Farina R. Simplified procedures to treat periodontal intraosseous defects in esthetic areas. Periodontol 2000. 2018 Jun 1;77(16):93-110. [ Links ]
44. Cortellini P, Tonetti MS. Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: A randomized-controlled trial in intra-bony defects. J Clin Periodontol. 2011;38(4):365-73. [ Links ]
45. Cortellini P. Minimally invasive surgical techniques in periodontal regeneration. J Evid Based Dent Pract 2012;12(3 SUPPL.):89-100. http://dx.doi.org/10.1016/S1532-3382(12)70021-0 [ Links ]
46. Retzepi M, Tonetti M, Donos N. Comparison of gingival blood flow during healing of simplified papilla preservation and modified Widman flap surgery: A clinical trial using laser Doppler flowmetry. J Clin Periodontol. 2007;34(10):903-11. [ Links ]
47. Graziani F, Peric M, Marhl U, Petrini M, Bettini L, Tonetti M, et al. Local application of enamel matrix derivative prevents acute systemic inflammation after periodontal regenerative surgery: A randomized controlled clinical trial. J Clin Periodontol. 2020 Jun;47(6):747-55. [ Links ]
48. Miron RJ, Sculean A, Cochran DL, Froum S, Zucchelli G, Nemcovsky C, et al. Twenty years of enamel matrix derivative: the past, the present and the future. J Clin Periodontol. 2016;43(8):668-83. [ Links ]
49. Lee JH, Park YS, Kim YT, Kim DH, Jeong SN. Assessment of early discomfort and wound healing outcomes after periodontal surgery with and without enamel matrix derivative: an observational retrospective case-control study. Clin Oral Investig. 2020;24(1):229-37. [ Links ]
50. Zhou S, Sun C, Huang S, Wu X, Zhao Y, Pan C, et al. Efficacy of Adjunctive Bioactive Materials in the Treatment of Periodontal Intrabony Defects: A Systematic Review and Meta-Analysis. Biomed Res Int. 2018;2018. [ Links ]
51. Sculean A, Alessandri R, Miron R, Salvi GE, Bosshardt DD. Enamel Matrix Proteins and Periodontal Wound Healing and Regeneration. Clin Adv Periodontics. 2011;1(2):101-17. [ Links ]
52. Esposito M, Grusovin MG, Papanikolaou N, Coulthard P, Worthington H V. Enamel matrix derivative (Emdogain(r)) for periodontal tissue regeneration in intrabony defects. A Cochrane systematic review. Eur J Oral Implantol. 2009;2(4):247-66. [ Links ]
53. Kao RT, Nares S, Reynolds MA. Periodontal Regeneration - Intrabony Defects: A Systematic Review from the AAP Regeneration Workshop. J Periodontol. 2015;86(2-s):S77-104. [ Links ]
54. Rojas MA, Marini L, Pilloni A, Sahrmann P. Early wound healing outcomes after regenerative periodontal surgery with enamel matrix derivatives or guided tissue regeneration: A systematic review. BMC Oral Health. 2019;19(1):1-16. [ Links ]
55. Liu S, Hu B, Zhang Y, Li W, Song J. Minimally invasive surgery combined with regenerative biomaterials in treating intra- bony defects: A meta-analysis. PLoS One. 2016;11(1):1-13. [ Links ]
56. Aimetti M, Fratini A, Manavella V, Giraudi M, Citterio F, Ferrarotti F, et al. Pocket resolution in regenerative treatment of intrabony defects with papilla preservation techniques: A systematic review and meta-analysis of randomized clinical trials. J Clin Periodontol. 2021;48(6):843-58. [ Links ]
57. Liu B, Ouyang X, Kang J, Zhou S, Suo C, Xu L, et al. Efficacy of periodontal minimally invasive surgery with and without regenerative materials for treatment of intrabony defect: a randomized clinical trial. Clin Oral Investig 2021;(0123456789). https://doi.org/10.1007/s00784-021-04134-w [ Links ]
Received: January 20, 2022; Accepted: May 30, 2022











 texto en
texto en