Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.24 no.40 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22592/ode2022n40e227
Research
Self-report of awake bruxism and related factors amongst physical education university students
Abstract Bruxism is an activity of the masticatory muscles with high prevalence in the general population. It has also been described as a frequent phenomenon in university students of some disciplines. Based on this idea, the present work analyzes the self-perception and some factors associated with the awake bruxism in university students of physical education (ISEF-UdelaR). This is an observational, descriptive and cross-sectional study in a sample of 178 university students. Data were collected through a self-report questionnaire. The 67.9% of the participants were daytime bruxism and 33% reported it (21% women and 13% men). Yet likewise, six out of ten volunteers who reported bruxism also reported anxiety, and three out of ten volunteers with bruxism reported stress. In conclusion, “probable” awake bruxism is highly prevalent in physical education students and the factor most associated with daytime bruxism is anxiety.
1 Núcleo de Investigación Educación Física, Deporte y Salud (NIEFDS) Instituto Superior de Educación Física, Universidad de la República, Uruguay; luciastefanelli@hotmail.fr
2Instituto Superior de Educación Física. Centro Universitario del Este. Universidad de la Republica, Uruguay. Centro de Biofísica y Neurociencias. Facultad de Ciencias de la Salud. Universidad de Carabobo, Venezuela
3Catedra de Fisiología General y Bucodental; Facultad de Odontología, Universidad de la República, Uruguay
4Núcleo de Investigación Educación Física, Deporte y Salud (NIEFDS) ISEF, Universidad de la República, Uruguay
Keywords: bruxism; anxiety; stress; orofacial pain; temporomandibular disorders
El bruxismo es una actividad parafuncional de los músculos masticatorios con alta prevalencia en la población general. Asimismo, se ha descrito como un fenómeno frecuente en estudiantes universitarios de algunas disciplinas. En este sentido, el presente trabajo analizó la autopercepción y algunos factores asociados al bruxismo de la vigilia en estudiantes universitarios de educación física (ISEF-UdelaR). Se presenta un estudio observacional, descriptivo, transversal, en una muestra de 178 jóvenes universitarios. Para la recolección de los datos se utilizó un cuestionario de autoreporte. El 67,9% de los participantes conocían el bruxismo y el 33% lo reportaron (el 21% y 13%, representado por mujeres y hombres respectivamente). Asimismo, seis de cada diez voluntarios que reportaron bruxismo también reportaron ansiedad y tres de cada diez voluntarios con reporte de bruxismo reportan estrés. En suma, el bruxismo “probable” de vigilia es altamente prevalente en estudiantes de educación física y el factor más asociado al bruxismo de la vigilia es la ansiedad.
Palabras clave: Bruxismo; Ansiedad; Estrés; Dolor orofacial; Trastornos témporomandibulares
O bruxismo é uma atividade parafuncional dos músculos mastigatórios com alta prevalencia na população em geral. Assim mesmo, vem sendo descrito como um fenômemo frequente em estudantes universitários de algumas disciplinas. Neste sentido, o trabalho atual analisou a autopercepção e alguns fatores associados ao bruxismo da vigília em estudantes universitários de educação física (ISEF-UdelaR). Trata-se de um estudo observacional, descritivo, transversal, com uma amostra de 178 jovens universitários. Os dados foram coletados através de um questionário de auto-relato. Os 67,9% dos participantes conheciam o bruxismo e 33% lhe relataram (21% e 13% representado por mulheres e homens, respectivamente). Assim mesmo, seis de cada dez voluntários que relataram bruxismo, também relataram ansiedade e três dos dez voluntários que relataram bruxismo, relataram estresse. Então, o bruxismo “provável” da vigília é altamente prevalente em estudantes de educação física e o principal fator associado ao bruxismo da vigília seria a ansiedade.
Palavras-chave: Bruxismo; Ansiedade; Estresse; Dor orofacial; Transtornos temporomandibulares
Introduction
The term “bruxism” has undergone a drastic evolution in recent years. The condition has been associated with dental clenching and parasomnias and has even been considered a predisposing or protective against certain conditions. More recently, it has been linked to muscle contraction events. Functionally, it is also defined as a collective term for parafunctional movements outside the physiological range of chewing movements.1,2) It can also cause various signs and symptoms, including masseter muscle hypertrophy, tooth wear, fracture or failure of restorations and dental implants, tooth sensitivity or pain, muscle or joint involvement, and temporomandibular joint (TMJ) disc displacements.3 Tooth clenching is of great concern, given its multiple clinical implications.4) In recent years, the definition of “bruxism” has been modified mainly to unify the diffuse and heterogeneous criteria prevailing in the professional and research communities. Therefore, a recent international consensus of experts defined bruxism as “repetitive masticatory muscle activity characterised by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible.”5 For this reason, most of the works published in the last five years base their research designs on this definition.6,7
For several decades, studies on bruxism focused on what happened during sleep. However, this changed as a result of international expert consensus. Experts recommended that single definition of bruxism should no longer be used in favor of two separate definitions considering the circadian manifestations of the phenomenon: sleep and wakefulness.8) Awake bruxism (AB) is a masticatory muscle activity occurring during wakefulness that is characterized by repetitive or sustained tooth contact and/or by bracing or thrusting the mandible, and sleep bruxism (SB) is a masticatory muscle activity during sleep characterized as rhythmic (phasic) or non-rhythmic (tonic).5,9)
Some authors state that bruxism prevalence is between 22% and 31%.10,11 According to Manfredini et al.,10 bruxism is not related to gender, and it tends to decrease with age. In Uruguay, a study including 2,800 people on the prevalence of temporomandibular disorders (TMD) and bruxism revealed that 30% of the participants reported feeling they had slept clenching their teeth. Additionally, approximately 72% had parafunctional tooth wear facets.12
Some studies have shown a potential association between bruxism, anxiety, and stress in college students.13-15 According to Carvallo and Mouthéz,16 there is a positive correlation between bruxism and anxiety. Thus, one of the manifestations of stress is bruxism, the gnashing and clenching of teeth without a functional purpose with variable frequency in the general population.17 In this regard, a study showed that 68% of university students are stressed and that awake bruxism was detected in over half the sample (52.1%).18) In addition, moderate to severe bruxism is a warning sign regarding oral health, since tooth wear, loss of restorations/teeth, and muscle and/or joint pain may occur, affecting health and quality of life.19-22)
Several studies agree that university students suffer high levels of stress and anxiety daily, confirming the association between stress and bruxism. There has been increased incidence of bruxism in the last decades.21-23) A study conducted in Finland on a sample of 4,403 students at the University of Applied Sciences also showed that bruxism and TMDs are prevalent in university students.24) However, no studies have yet analyzed the problem of bruxism among physical education students. This degree may include very specific strength, power, and resistance training activities. This could lead us to think that this student population may behave differently from other university students regarding psychological stress, anxiety, or bruxism, among other factors.
In this context, this study aimed to use self-reporting to explore teeth clenching and factors associated with AB, such as stress and anxiety in undergraduate physical education students at Universidad de la República, Uruguay.
Materials and methods
Participants
A total of 178 volunteers of both sexes participated in this study. They were students of the Higher Institute of Physical Education (ISEF) of Universidad de la República (UdelaR), aged between 18 and 34. Volunteers were recruited consecutively based on a call for volunteers made by ISEF to complete an online and email questionnaire.
Data collection and self-reporting instrument
The data collected are based on the participants’ surveyed selfperception and not on a clinical study. The data were collected through a selfreport questionnaire answered in person or by email. The questionnaire was developed following previously published parameters that explore variables such as self-perceived awake tooth clenching, facial muscle tension, and stiffness, facial muscle fatigue on awakening, head and jaw pain, etc. We used the classifications and parameters14 from the validated criteria for determining bruxism15) according to the international consensus on bruxism diagnosis.1
Statistical data analysis and processing
The statistical processing of signs/symptoms associated with bruxism was based on reporting frequency. Statistical analysis was performed using PAST statistical software. The X2 test (Pearson distribution) was applied to associate the different variables, assuming a significant value p<0.05 (95% CI). The analysis included associations based on the frequency of bruxism reporting (reported bruxism, no reported bruxism) with reported age, sex, stress, and anxiety.
Results
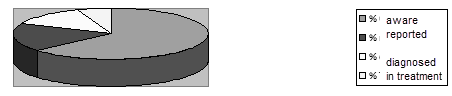
The sample included 178 students, with a mean age of 24 (minimum 18 and maximum 34). A total of 68% of students said they knew what bruxism was. Thirty-three percent reported having bruxism, of which 14% claimed to have been clinically diagnosed. Of the volunteers, 6% were undergoing treatment with an oral device (Figure 1).
Age and perceived bruxism
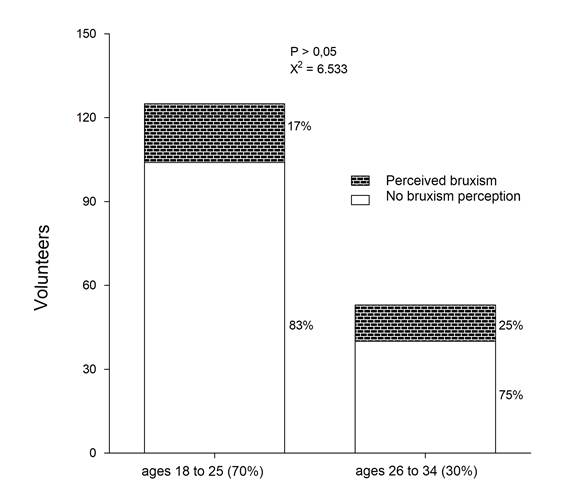
Seventeen percent of the volunteers aged between 18 and 25 (70% of the sample) self-reported bruxism. Of the remaining 30% (26 and 34 years), 25% self-reported bruxism (Figure 2).
Sex and perceived bruxism
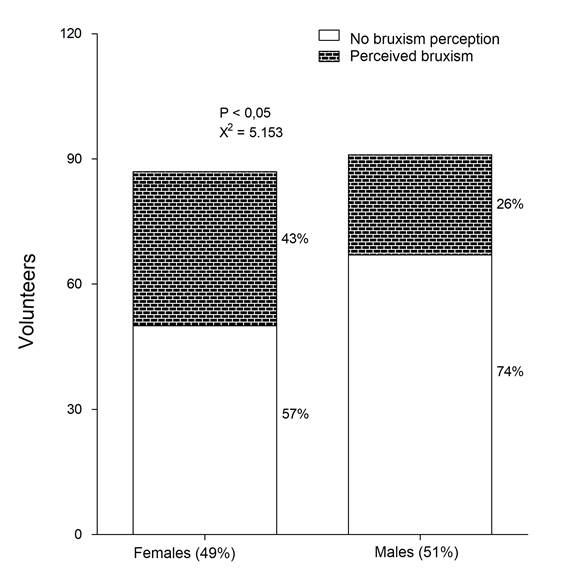
Forty-nine percent of the sample was female, and the remaining 51% was male. Additionally, 43% of the female participants reported bruxism, and only 26% of the male participants reported it (Figure 3).
Anxiety, stress, and perceived bruxism
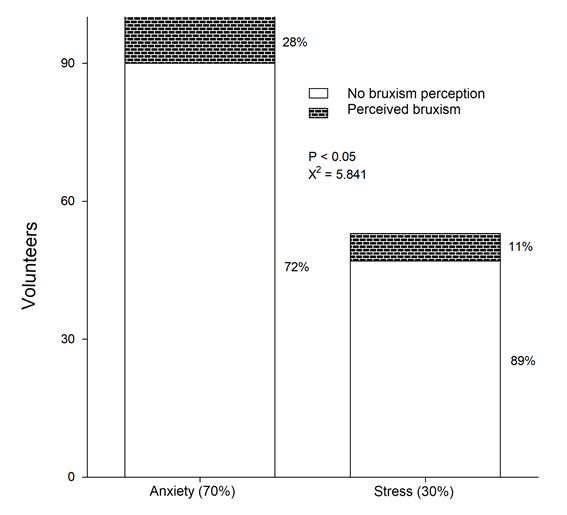
Regarding anxiety and stress, 28% of the volunteers who reported anxiety also reported bruxism. As for the volunteers who reported suffering from stress, 11% also reported bruxism (Figure 4).
Associated factors and perceived bruxism
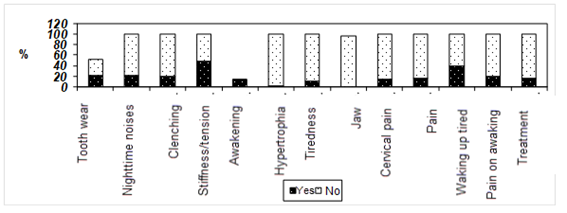
As for factors associated with bruxism, 21% reported tooth wear, 20.2% reported clenching their teeth during the day, and 6% described suffering from stiffness and tension in the jaw. Twenty-one percent reported their teeth made noises at night and 15 % had orofacial pain. Additionally, 4% reported having a locked jaw upon awakening, and 40% woke up feeling tired (Figure 5).
Discussion
This study found no associations between age and bruxism in university physical education students. This result agrees with previous studies conducted on a young population,18,25,26 but does not coincide with the study by Emodi Perlman et al.,27 who observed a correlation between awake bruxism and age. These differences probably occured because the studies have heterogeneous methodological designs.
Women presented a higher percentage of self-reported bruxism than men. This agrees with previous studies stating that bruxism is higher in women than in men.12 In addition, disorders related to the function of the masticatory system, as well as TMDs, tend to be more frequent in women.28) However, this association has not been verified for awake bruxism.18,25,27) The findings of this work regarding the coexistence of bruxism and anxiety in university students agree with other studies that demonstrate the significant association between self-reported waking bruxism and anxiety.26,29,31) Likewise, another study observed that students with bruxism are more predisposed to anxiety.18,30 These findings support modern changes in diagnostic and therapeutic paradigms as we migrate from a purely mechanistic model to a bio-psycho-social model that considers emotional factors.
Regarding stress and bruxism, some studies indicate that people who self-report bruxism are more likely to develop this parafunction when stress is a risk factor.29,32 These findings are consistent with our own: there is a significant correlation between waking bruxism and stress. Another factor frequently associated with bruxism is tiredness. 33-35 We observed that 39.8% of university students reported waking up tired. All these factors could cause neuromuscular alterations and an increased likelihood of TMDs.22 Similarly, tooth clenching increases with stress experienced mainly during the day and exam periods.16 As a result, students are affected and suffer from anxiety and stress.13
A study conducted among engineering students, in which moderate stress predominated, found evidence of tooth wear.19 These data agree with our study that reported 21.3% dental attrition. However, tooth wear may not be considered a determinant of bruxism, as it may be caused by diet, age, and other factors.13,36,37 In addition, patients suffering from clenching bruxism tend not to wear down their teeth. According to Machado et al.,38 bruxism sufferers are those with dental wear in at least one tooth, associated with teeth clenching/grinding, since bruxism can increase tooth enamel wear. However, at first, the teeth may not show signs of wear.39) This makes it challenging to diagnose bruxism in young people. Also, on clinical examination, wear facets may indicate a previous history of bruxism, and the condition may no longer exist at the time of examination.13)
Another critical sign of bruxism is teeth grinding,39 considered a major contributing factor in TMDs.40) In this study, 20.2% of the volunteers had perceived teeth clenching during the day in the previous two months and 21% upon awakening (or that they were awakened) by teeth noises (grinding) while sleeping. Both teeth grinding and clenching are related to muscle hyperactivity.17) This may be due to the overexertion of the masticatory muscles. This effort leads to other symptoms associated with bruxism that include jaw pain and pain in the facial muscles due to the effort made by these muscles.41) During hyperfunction, the muscles may present painful symptoms40 or even radiated pain, such as pain in the head.13,20,42 This agrees with our results: 15.1% reported orofacial pain (Figure 5). In addition, 61% reported daily stiffness and strains (Figure 5). Regarding students’ perception, 33% reported bruxism (Figure 1), which agrees with a study that determined the prevalence (33.9%) of awake bruxism through self-reporting.25) It is also consistent with a systematic review of self-reported studies which presents a 22.1-31% AB prevalence in people who reported having suffered this parafunction frequently in the last six months.10
Conclusions
This study analyzes the situation of university physical education students regarding awake bruxism for the first time. It has found a high prevalence and a significant association between self-reported bruxism and females. These preliminary results suggest the need for more extensive studies to explore potential causal factors specific to this university degree. They might be linked to strength or resistance physical activity, stress, and anxiety.
REFERENCES
1. Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne G et al. Bruxism defined and graded: An international consensus. J Oral Rehabil. 2013; 40 (1): 2-4. [ Links ]
2. Sierwald I, John M, Schierz O, Hirsch C, Sagheri D, Jost-Brinkmann P. Association of temporomandibular disorder pain with awake and sleep bruxism in adults. J Orofac Orthoped 2015; 76 (4): 305-317. [ Links ]
3. Falisi G, Rastelli C, Panti F, Maglione H, Quezada-Arcega R. (2014). Psychotropic drugs and bruxism. Expert Opinion on DrugSafety. 2014; 13 (10): 1319-1326. [ Links ]
4. Fuentes A, Martínez K, Miralles R, Gutiérrez M, Santander H, Fresno M. Electromyographic activity during awake too thgrindin gtasksat different jaw posture in the sagittal plane. Acta Odontologica Scandinavica. 2013; 71 (3-4): 917-922. [ Links ]
5. Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018; 45 (11): 837-44. [ Links ]
6. Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F. The bruxism construct: Fromcut-off points to a continuum spectrum . J Oral Rehab 2019; (46): 991-997. [ Links ]
7. Saito-Murakami K, Sato M, Otsuka H, Miura H, Terada N, Fujisawa M. Day time masticatory muscle electromyography biofeed back regulates the phasic componente of sleep bruxism. J Oral Rehab. 2020; 47(7): 827-833. [ Links ]
8. Nakayama R, Nishiyama A, Shimada M. Bruxism-Related Signsand Periodontal Disease: A Preliminary Study. Open Dentistry J 2018; 12 (1): 400-405. [ Links ]
9. Melo G, Duarte J, Pauletto P, Porporatti A, Stuginski-Barbosa J, Winocur E et al. Bruxism: Anumbrella review of systematic reviews. J Oral Rehab 2019; 46 (7): 666-690. [ Links ]
10. Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F. Epidemiology of bruxism en adults: a systematic review of the literature. J Orofac Pain. 2013; (30): 49-55. [ Links ]
11. Hermesh H, Schapir L, Marom S, Skopski R, Barnea E, Weizman A et al. Bruxism and oral parafunctional hyperactivity in social phobia outpatients. J Oral Rehabil. 2015; 42 (2): 90-7. [ Links ]
12. Riva R, Sanguinetti M, Rodríguez A, Guzzetti LL, Lorenzo S, Álvarez R et al. Prevalencia de trastornos témporomandibulares y bruxismo en Uruguay: Parte I. Rev Odontoestomatología. 2011; 13 (17): 54-71. [ Links ]
13. Orlandi Costa A, Silveira de Oliveira E, Douglas de Oliveira D, Aguiar Tavano K, Gomes A. Prevalence and factors associated with bruxism in university. Rev. Bras. Odontol. 2017; 74 (2): 120-5. [ Links ]
14. Tarco A, Plinio E. Prevalencia de bruxismo en los deportistas del grupo de alto rendimiento de las disciplinas de atletismo, halterofilia y boxeo de la Concentración Deportiva de Pichincha, Quito 2017.Universidad Central Ecuador. 2018; 10-11. Disponible en: http://www.dspace.uce.edu.ec/handle/25000/13817 [ Links ]
15. Molina OF, dos Santos J, Mazzetto M, Nelson S, Nowlin T. Oral jaw behaviors in TMD and bruxism: a comparison study by severity of bruxism. Cranio. 2001 Apr; 19(2): 114-22.doi:10.1080/08869634.2001.11746160. Disponible en: https://pubmed.ncbi.nlm.nih.gov/1184 [ Links ]
16. Carvalho C, Mourthé G. O Bruxismo na visão da Psicologia. Arq Bras Odontol. 2005; 18-25. [ Links ]
17. Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. Sleep Med Rev. 2000; (4): 27-43. [ Links ]
18. Ordoñez-Plaza MP, Villavicencio-Caparó E, Alvarado-Jimenez OR, Vanegas-Avecillas M. Prevalencia de bruxismo de vigilia evaluado por auto-reporte en relación con estrés, ansiedad y depresión. Rev Estomatol Herediana. 2016; 26 (3): 147-55. [ Links ]
19. Capetillo-Hernández G, Torres-Capetillo E, Moreno-Marín F, Montejo-Arroyo D, Arroyo-Flores M, Flores-Aguilar S. Bruxism in Engineering students. Rev Mex Med Forense. 2019; 4(suppl1): 70-72. [ Links ]
20. Von Bischhoffshausen K, Wallem AH, Allendes AA, Rodrigo DM. Prevalencia de Bruxismo y estrés en Estudiantes de Odontología de la Pontificia Universidad Católica de Chile. Int. J. Odontostomat.2019; 13 (1): 97-102. [ Links ]
21. Sánchez S. Interacciones sobre la salud bucodental y el Rendimiento deportivo anaeróbico. Universidad de Barcelona. Barcelona. 2014 [ Links ]
22. Cavallo P, Carpinelli L, Savarese G. Perceived stress and bruxism in university students. BMC Res. Notes. 2016 ; 9 (1): 514. [ Links ]
23. Quadri MF, Mahnashi A, Al-Almutahhir A. Association of awake bruxism with khat, coffee, tobacco, and stress among Jazan university students. Int J Dent. 2015: 1-5. [ Links ]
24. Huhtela OS, Näpänkangas R, Joensuu T, Raustia A, Kunttu K, Sipilä K. Self-Reported Bruxism and Symptoms of Temporomandibular Disorders in Finnish University Students. J Oral Fac Pain Headache. 2016; 30 (4): 311-17. [ Links ]
25. Sener, S., Karabekiroglu, S., Ünlü, N. Genç yetiskin bireylerde bruksizm farkindaligi ve iliskili degisik faktörlerin degerlendirilmesi. Cumhur Dent J. 2014; 17 (4), 361. [ Links ]
26. Winocur E, Uziel NLT, Lisha T, Goldsmith C, Eli I. Self-reported Bruxism associations with perceived stress, motivation for control, dental anxiety and gagging. J Oral Rehabil. 2011; 38 (1), 3-11. [ Links ]
27. Emodi Perlman A, Lobbezoo F, Zar A, Rubin FR, van Selms M, Winocur E. Self-Reported bruxism and associated factors in Israeli adolescents. J Oral Rehabil. 2016; 43, 443-50. [ Links ]
28. Okeson P. Tratamiento de Oclusión y afecciones temporomandibulares. (8 ed.). (C. b. Mosby, Ed.) Barcelona, España: Elsevier Inc. 2019. [ Links ]
29. Ahlberg J, Lobbezoo F, Ahlberg Ke. Self-reported bruxism mirrors anxiety and stress in adults. Med Oral Patol Oral Cir Bucal. 2013; 18 (1), 7-11. [ Links ]
30. Kampe T, Tagdae T, Bader G, Edman G. Reported symptoms and clinical findings in a group of subjects with longstanding bruxing behaviour . J. Oral Rehabil. 1997; 24 (8), 581-7. [ Links ]
31. Tavares L, da-Silva Parente Macedo L, Duarte C, de Goffredo Filho G, de Souza Tesch R Cross-sectional study of anxiety symptoms and self-report of awake and sleep bruxism in female TMD patients. Cranio. 2016; 34 (6), 378-81. [ Links ]
32. Van-Selms M, Visscher C, Naeije M, Lobbezoo F. Bruxism and associated factors among Dutch adolescents. Community Dent Oral Epidemiol. 2013; 41 (4), 353-63. [ Links ]
33. Alfaya T, Tannure P, Barcelos R, Dip E, Uemoto L, Gouvêa C. Clinical management of childhood bruxism. Rev Gaúch Odontol. 2015; (63), 207-12. [ Links ]
34. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxisme physiology and pathology: an overview for clinicians. J Oral Rehabil. (J. O. Rehabil, Ed.).2008; 35 (7), 476-94. [ Links ]
35. Carvalho A, Cury A, Garcia R. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res. 2008; (22), 31-5. [ Links ]
36. Matsumoto H, Tsukiyama Y, Kuwatsuru R, Koyano K. The effect of intermit¬tent use of occlusal splint devices on sleep bruxism: a 4-week observation with a portable electromyographic recording device. J Oral Rehabil. 2015; (42), 251-8. [ Links ]
37. Palinkas M, De Luca Canto G, Rodrigues L, Bataglion C, Siéssere S, Semprini M. e. Comparative capabilities of clinical assessment, ciagnostic Criteria, and polysomnography in detecting bleep Bruxism. J Clin Sleep Med 2015. [ Links ]
38. Machado N, Fonseca R, Branco C, Barbosa G, Fernandes Neto A, Soares C, et al. Dental wear caused by association between Bruxism and gastro¬esophageal reflux disease: a rehabilitation report. J Appl Oral Sci. 2007; 15: 327-33. [ Links ]
39. Murali R, Rangarajan P, Mounissamy A. Bruxism: Conceptual discussion and review. J Pharm Bioallied Sci. 2015; (7), S265-70. [ Links ]
40. Koyano K, Tsukiyama Y, Ichiki R,Kuwata T Assessment of bruxism in the clinic. J Oral Rehabil. 2008; 35, 495-508. [ Links ]
41. Tuz H, Onder E, Kisnisci R. Prevalence of otologic complaints in patients with temporomandibular disorder. Am J Orthod Dentofacial Orthop. 2003; 23, 620-3. [ Links ]
42. Pergamalian A, Rudy T, Zaki HG. The association between wear facets, bruxism, and severity of facial pain in patients with temporomandibular disorders. J Prosthet Dent. 2003; 90, 194-200. [ Links ]
Declaration of interests: The authors certify that they have no commercial interests that represents a conflict of interests in connection with the manuscript
Authors' contribution note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript. MLS has contributted in 1, 2, 3, 4 y 6 JMG ha contributted in 2, 3, 4 y 6 MKF ha contributted in 3, 4 y 6 LIFR ha contributted in 3, 4 y 6 DLSP ha contributted in 1, 2 SB ha contributted in 1, 2
Received: July 06, 2022; Accepted: December 13, 2022











 texto en
texto en