Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.24 no.40 Montevideo dic. 2022 Epub 01-Dic-2022
https://doi.org/10.22592/ode2022n40e220
Research
Morphological distribution of Class II malocclusions according to skeletal pattern in an adult sample of the Faculty of Dentistry of the Universidad de Chile
1Cirujano-Dentista Práctica Privada, Santiago, Chile. f.vidaurre9@gmail.com
2Cirujano-Dentista, Ortodoncista Práctica Privada. Chile
3Instituto de Investigación en Ciencias Odontológicas (ICOD), Centro de Análisis Cuantitativo en Antropología Dental (CA2), Facultad de Odontología y Departamento de Antropología, Facultad de Ciencias, Universidad de Chile. gmanriquezss@odontologia.uchile.cl
4Servicio de Cirugía Máxilo Facial, Hospital San Borja Arriarán. Facultad de Odontología, Universidad de Chile, Santiago, Chile.
Objective:
To determine the morphological distribution of Class II malocclusions according to their skeletal pattern in an adult sample of the Faculty of Dentistry of the Universidad de Chile.
Materials and methods:
The sample consisted of 220 teleradiographies of individuals over 18 years old with an ANB angle greater than 4°. SNA and SNB angles were measured to assign the Class II skeletal pattern.
Results:
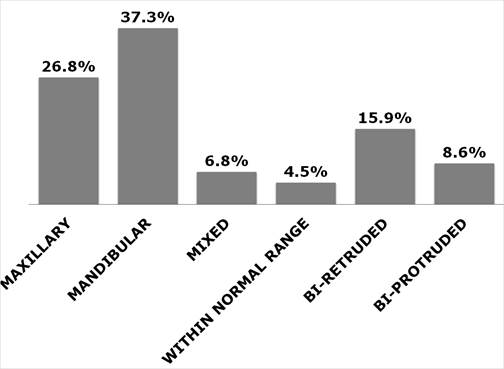
The mandibular was the most frequent skeletal pattern followed by the maxillary. In addition, three new skeletal patterns that had not been explicitly described in the relevant literature were found (Bi-Protruded, Bi-Retruded and Within Normal Range).
Conclusions:
The most frequent Class II malocclusion skeletal pattern in our study was the mandibular. The Bi-Retruded and Bi-Protruded variants should be incorporated into the skeletal diagnosis, particularly the Bi-Retrudeddue to its significant high frequency and clinical relevance.
Keywords: cephalometrics; Class II malocclusion
Objetivo:
Determinar la distribución morfológica de las Clases II según su naturaleza esqueletal en una muestra de población adulta de la Facultad de Odontología de la Universidad de Chile.
Materiales y métodos:
La muestra experimental estuvo compuesta por 220 telerradiografías laterales de cráneo de individuos mayores de 18 años con ángulos ANB mayores a 4°. Para asignar la naturaleza esqueletal se midieron los ángulos SNA y SNB.
Resultados:
Se obtuvo que la naturaleza esqueletal más frecuente fue la mandibular seguido por la maxilar. Además, se obtuvieron tres nuevas naturalezas esqueletales las cuales, según el análisis de la literatura pertinente, no habían sido descritas explícitamente con anterioridad (bi-protruida, bi-retruida y en norma).
Conclusiones:
La naturaleza esqueletal de las maloclusiones Clase II más frecuente en nuestro estudio fue la naturaleza mandibular. Las variantes bi-retruida y bi-protruida deberían ser incorporadas en el diagnóstico esqueletal, especialmente la variante bi-retruida, debido a su significativa alta frecuencia y relevancia clínica.
Palabras clave: Cefalometría; maloclusión Clase II
Objetivo:
Determinar a distribuição morfológica da má oclusão de Classe II de acordo ao padrão esquelético, em uma amostra da população adulta da Faculdade de Odontologia da Universidade do Chile.
Materiais e Métodos:
A amostra experimental foi composta de 220 indivíduos acima de 18 anos de idade, com ângulo ANB maior que 4°. Os ângulos SNA e SNB foram medidos para determinar o padrão esquelético da Classe II.
Resultados:
Foi observado que o padrão esquelético mais frequente foi o mandibular e depois maxilar. Além disso, foram obtidos três novos tipos de padrões esqueléticos que, de acordo com a análise da literatura relevante, não haviam sido explicitamente descritos anteriormente: bi-protrusão, bi-retrusão e em norma.
Conclusões:
O padrão esquelético mais frequente das más oclusões de Classe II do nosso estudo foi mandibular. As variantes bi-protrusão e bi-retrusão deveriam ser incorporadas no diagnóstico esquelético, especialmente a variante de bi-retrusão, devido à sua significativa frequência elevada e relevância clínica.
Palavras-chave: Cefalometria; má oclusão de Classe II
Introduction
Dental malocclusion is one of the most prevalent disorders affecting the oral cavity after dental caries and periodontal disease. It ranks third among the priorities of dental conditions in public health relevance worldwide.1,2 Dental malocclusion is defined as a variation from the typical occlusal pattern or a variation from the normal range of growth and morphology, which may affect the teeth, the bone skeleton, or both.1,2 Malocclusion is not a pathology itself but a variation that may or may not be associated with pathological conditions.1
In 1899, Angle classified malocclusions. This classification is so straightforward that it remains one of the leading classification systems in orthodontics. Angle uses the term “Class” to refer to the sagittal relationships between the dental arches, and its indicators are I, II, and III. This system is widely accepted and allows orthodontists from different countries to communicate fluently.3,4 Having said that, this classification only describes dental relationships. It took some time in the history of orthodontics for lateral skull teleradiography and, concomitantly, conventional cephalometric analysis to be adopted to determine the skeletal component of malocclusion.5 Thus, with the advent of cephalometry it was clear that malocclusions are not only dental in nature but that the position or size of the maxilla and mandible might affect the relationship between the upper and lower teeth too.
Specifically, Class II malocclusions would result from a sagittal disproportion, both in size and in the position of the jaws. The concomitant literature shows that Class II malocclusions could be due to three well-determined skeletal situations: a) a protruded maxilla; b) a smaller size or retruded mandible; and c) a combination of both.6-11
Studies on the prevalence of malocclusions have been based mainly on the sagittal relationship of the dental arches1,12-14 where Class II represents between 5% and 29% of the population.6,15 Studies on this subject are scarce and include discrepant data, particularly in Chile. Thus, while Burgos determined that Class II prevalence in a sample of 185 cases (children and adolescents) was 21.7%,16 Aguirre showed a higher frequency of skeletal Class II in a sample of 92 individuals: 44.6%.17 In another study, Iturriaga and Whittle determined that Class II prevalence in a sample of 1000 cases was 31% in men and 25% in women.18 However, none of these studies have determined the skeletal pattern, especially for Class II malocclusions. Thus, the main aim of the present study is to determine the morphological distribution of Class II malocclusion according to its skeletal component, or what we will refer hereafter as “skeletal pattern”, in an adult sample from the Faculty of Dentistry of the Universidad de Chile.
We used an anonymized database of lateral teleradiographies housed at the Center for Quantitative Analysis in Dental Anthropology (CA2), Faculty of Dentistry, Universidad de Chile. A total of 1,011 lateral teleradiographies belonging to individuals over 18 years old attending the Dental Clinic of the Faculty of Dentistry with no history of orthopedic or orthodontic treatment were analyzed. ANB angle greater than 4° with normal or increased proclination of the upper incisors indicated the presence of a Class II malocclusion. Retruded upper incisors were excluded from the sample. The final sample included 220 teleradiographies (161 women and 59 men).
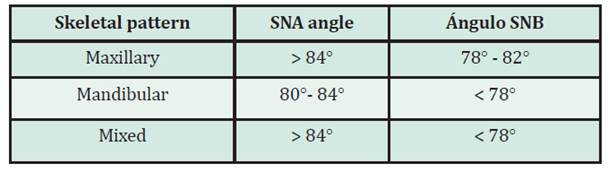
The SNA and SNB angles were measured to assign each teleradiograph to a skeletal pattern. The skeletal pattern was considered as maxillary when the SNA angle was greater than 84° and, at the same time, the SNB angle fell within the cephalometric range, i.e., between 78° and 82°. The skeletal nature was considered mandibular when the SNB angle was lower than 78°, and the SNA angle was within the normal range, i.e., between 80° and 84°. Finally, individuals were classified as having a mixed skeletal pattern when the SNA angle was above the normal range, and the SNB angle was below the normal range (Table 1, Figure 2). The angles were measured using TpsDig2 (V. 2.31, 2017) software. The selection of the teleradiographies and the measurement of the angles were carried out by the same operator (FV).
To estimate the intraobserver error, we tested the null hypothesis 1 (H01), which states H01: µ1 = µ2, where µ is the parametric mean of the angle values (1) and their respective repeated measures (2). In this case, an Anova test on repeated measures, considering male and female samples separately for each angle was applied.
To determine the effect of the sex variable, in this study we tested the null hypothesis 2 (H02). This hypothesis states that H02: µ1 = µ2, where µ is the parametric mean of the number of skeletal classes, 1 corresponding to males and 2 to females. H02 was tested after a non-parametric Chi-square test (Chi2). Statistical analyses were performed with PAST (V. 4.03) software (Paleontological Statistical Software Package for Education and Data Analysis).
Results
Regarding the intra-observer error, no statistically significant differences were observed between the original and the repeated measures performed by the same observer (FV). SNAmen: F(1,18)=0.71442, p=0.1268; SNAwomen: F(1,18)=1.513, p=0.2499; SNBmen: F(1,18)=3.309, p=0.1023; SNBwomen: F(1,18)=3.799, p=0.08308; ANBmen: F(1,18)=0.0016, p=0.9687; ANBwomen: F(1,18)= 0.6723, p=0.4334). Given that the differences in the ratio of skeletal patterns according to sex were statistically non-significant (Chi2 (g.l.5)=7.8021, p=0.16748, p Monte Carlo=0.1667, N permutations=9999), the effect of sex was not considered in the analysis..
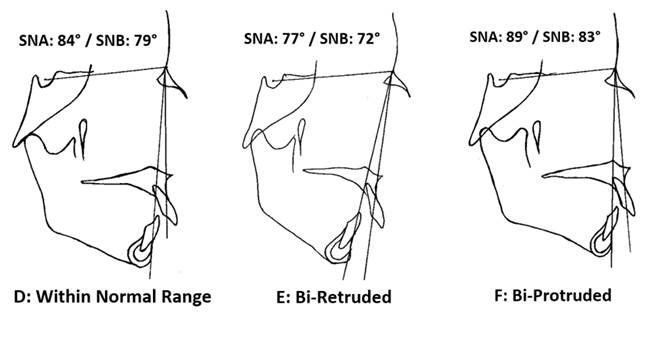
After measuring the SNA and SNB angles and having assigned each teleradiograph to any of the previously established patterns in the literature (i.e. maxillary, mandibular, or mixed), a significant number of cases could not be assigned to any of the above mentioned patterns. When the SNA and SNB angular measurements of this subsample were analyzed, three additional skeletal patterns were found. The first pattern was defined as “Within Normal Range” when the SNA and SNB angular values were within the first standard deviation of the sample distribution. The second pattern, named “Bi-Retruded”, corresponds to SNA values lower than 80° and the SNB values lower than 78°. Finally, the third skeletal pattern, defined as “Bi-Protruded,” considers individuals having SNA and SNB angles greater than 84° and 82°, respectively (Table 2, Fig. 1, Fig. 3).
Table 2: Distribution of the skeletal patterns of Class II malocclusions observed in this study, considering the conventional and the additional classification proposed in this study
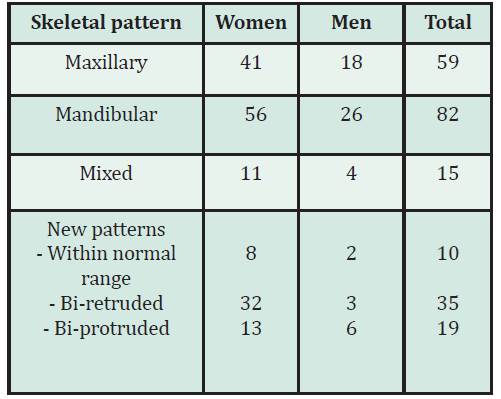
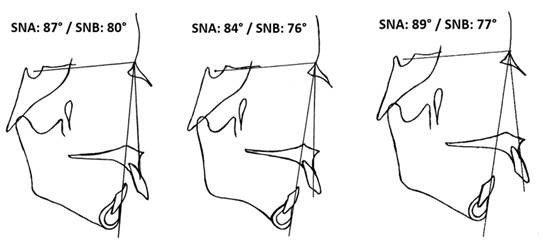
Figure 2: Simplified diagrams of SNA and SNB measurements (from left to right: Maxillary, Mandibular and Mixed skeletal patterns).
Discussion
To determine the morphological distribution of Class II malocclusions in adult patients according to their skeletal pattern in a sample from the Faculty of Dentistry, Universidad de Chile, an analytical, cross-sectional, and quantitative study was carried out using lateral teleradiographies obtained from an anonymized database housed at the Center for Quantitative Analysis in Dental Anthropology, Faculty of Dentistry, Universidad de Chile.
Regarding Class II malocclusions, there is no agreement in the literature about their origin or etiology. Some authors state that this sagittal disproportion would be caused mainly by a retruded mandible.8,9,11 Some attribute it to a protruded position of the maxilla with respect to the skull,6,7 and others to a combination of alterations that may affect both structures.10 The prevalence of each of these patterns has not been clearly established. In this respect, our results indicate that Class II malocclusion is mainly attributed to altered mandibular position or size. These results agree with Ardani et al., who studied an Indonesian adult population and concluded that the mandibular pattern is the most frequent one.15 Helder and Buschang studied French-Canadian adolescents finding that the increase in the ANB angle observed in Class II individuals is mainly due to a decrease in the SNB angle.11
In contrast, Hassan studied a Saudi population (85 children aged 10-13 years old), and found that the maxilla was significantly more prognathic in the Class II group due to an increased SNA angle.6 Rosenblum found that 56.6% of individuals with Class II malocclusion had maxillary protrusion, and only 26.7% had mandibular retrusion.7
These discrepancies can be attributed to different factors, such as the use of an imprecise criterion, as Class selection based on dental rather than on skeletal relationships. In addition, studying children and adolescents may introduce a confusion factor, 6 as the final size and position of the mandible is established towards the end of the individual’s growth and development process. Given that the mandible is the last structure to mature, studying an adult sample may yield more reliable results when determining the skeletal component of Class II malocclusions.19 Based on all this evidence, the mandible would be the primary determinant of malocclusions since it would be under the environmental and epigenetic influence for more time11.
Thus, the genetic ancestry of the sample seems to play key role in skeletal class pattern. Ardani et al. compared their own results obtained in a Javanese population with studies conducted in populations from Canada, China, Nepal, Italy, Iraq, and Saudi Arabia, concluding that facial pattern variation in Class II skeletal pattern may be affected by the ancestry of the patients.15
Although our results show that Class II is caused mainly by a retruded mandible, it could also be explained by a protruded maxilla or by a combination of alterations in the position and size of both maxilla and mandible. After Ardani et al., the most frequent skeletal pattern is the mandibular, followed by excessive maxilla, then a mixed pattern, and finally by normal maxillary and mandibular length.15
Conversely, some authors categorically attribute Class II malocclusions only to a retruded mandible9,11 or only to a prognathic maxilla,6 excluding other potential etiologies. This could be explained by the use of averages instead of the specific values of each measurement. It is essential to consider all the skeletal patterns, even if they are rare, due to the fact that they are a crucial factor when diagnosing and planning a personalized treatment.
One of the main findings of this work is the description of three new skeletal patterns, which according to the analysis of the relevant literature, had not been explicitly described before. While orthodontists may have already detected these Class II presentations, they do not appear in the literature as clearly as the others do. Nevertheless, some studies may potentially be indirectly comparable to ours. Thus, Sidlauskas et al. evaluated 86 patients aged between 9 and 12 finding that 8% of Class II individuals presented maxillary retrognathia, defined when the SNA angles were under 77°. However, this percentage would have been considerably higher if these authors had considered angles lower than 80° as maxillary retrognathia, like in our study. All the patients in the Sidlauskas et al. study had ANB angles greater than 4°, so we could deduce that this same percentage of patients had a Bi-Retruded Class II malocclusion.20 In a sample of 277 patients aged 8 to 11, McNamara studied the nature and frequency of specific components that may contribute to a Class II occlusal relationship, finding a high frequency of cases with maxillary retrusion (48.9%).21 However, the inclusion criteria used by McNamara21 were based on a dental rather than a skeletal diagnosis without distinguishing between Class II division 1 and Class II division 2, being both morphologically different entities that should be considered as two extreme patterns of a retruded mandible variation.22 Finally, Pancherz10 compared Class II division 1 and Class II division 2 malocclusions in children aged 8 to 10 and 11 to 13 years old. He observed that 15% of the first group, and 13% of the second, had a retruded maxilla.10
The literature does not support the existence of sexual dimorphism in cephalometric studies.9,10,23,24 However, the high expression of Bi-Retruded Class II in women compared to men in our results is striking. Although this result would reflect the proportion of both sexes in the total sample regardless of skeletal pattern, future studies should be considered for understanding the relevance of this finding.
The Bi-Retruded group arouses particular interest regarding the impact of mandibular and maxillary retrusion on the upper airway. It is essential to study the upper airway and its relationship with mandibular position and size in orthodontic diagnosis due to its association with obstructive respiratory disorders, especially sleep apnea.25 Severe mandibular deficiency has been associated with narrowed pharyngeal airway, which increases the likelihood of impaired respiratory function and possibly causes disorders such as rhoncopathy, increased upper airway resistance syndrome and obstructive sleep apnea-hypopnea syndrome.26 Nadja e Silva et al. evaluated airway dimensions in patients with Class II skeletal malocclusion with cephalometry in 80 individuals aged 10 to 17 years old. They found that the size of the oropharynx and nasopharynx, as well as the mandibular position and length, were smaller in Class II individuals, and that there was a positive correlation between the size of the oro-nasopharynx and different cephalometric measurements characteristic of Class II, including the SNB angle.25 If a patient with a retrognathic mandible also presents a retruded maxilla, a greater involvement of signs and symptoms of upper airway obstructive problems may appear. This is fundamental in the therapeutic indication of orthopedic and surgical bimaxillary advancement.25 Bimaxillary advancement surgery has proven to be beneficial in terms of increased upper airway size, improved oximetric indicators, and better quality of life as measured with the Epworth Sleepiness Scale.27,28
Thus, the Bi-Retruded skeletal variant of Class II is relevant for orthodontic practice because it enriches the diagnosis and guides the treatment, where bimaxillary sagittal modifications are required to achieve the right dento-skeletal balance.
Conclusion
The most frequent Class II malocclusion skeletal pattern in our study was the mandibular, followed by the maxillary. Due to their clinical relevance, the Bi-Retruded and Bi-Protruded patterns should be included in the description of the Class II skeletal patterns, especially the Bi-Retruded. Since optimal treatment and correction of sagittal skeletal discrepancies must be based on the individualized diagnosis, we recommend that the different Class II skeletal patterns morphologies described in the present study be considered by clinicians.
REFERENCES
1. Mishra P, Mote N, Mishra S, Mishra R, Rajbhar J, Neil-Pravara O. Prevalence of different types of malocclusion in young adults. Ahmednagar District, Maharashtra (According to Angle's classification) Pravara Med Rev. 2018;10(1):4-9. [ Links ]
2. Narayanan RK, Jeseem M, Kumar TA. Prevalence of malocclusion among 10-12-year-old schoolchildren in Kozhikode District, Kerala: An epidemiological study. Int J Clin Pediatr Dent. 2016;9(1):50. [ Links ]
3. Angle EH. Classification of malocclusion. Dent Cosmos. 1899;41:350-75. [ Links ]
4. Massler M, Frankel JM. Prevalence of malocclusion in children aged 14 to 18 years. Am J Orthod 1951;37(10):751-68. [ Links ]
5. Rojas Valenzuela R, Carvajal R, Bustamante S, Silva AL, Rojas R. Estudio Cefalométrico de Harvold de los Tamaños Maxilares y de la Altura Facial Antero Inferior en Niños de 9 Años de Edad, con Clase I Esqueletal, del Area Norte de la Región Metropolitana. Rev Dental Chile. 2001;92(3):15-9. [ Links ]
6. Hassan AH. Cephalometric characteristics of Class II division 1 malocclusion in a Saudi population living in the western region. Saudi Dental J 2011;23(1):23-7. [ Links ]
7. Rosenblum RE. Class II malocclusion: mandibular retrusion or maxillary protrusion? Angle Orthod 1995;65(1):49-62. [ Links ]
8. Craig CE. The skeletal patterns characteristic of Class I and Class II, Division I malocclusions in norma lateralis. Angle Orthod 1951;21(1):44-56. [ Links ]
9. Freitas MR, Santos MAC, Freitas KMS, Janson G, Freitas DS, Henriques JFC. Cephalometric characterization of skeletal Class II, division 1 malocclusion in white Brazilian subjects. J Appl Oral Sci. 2005;13(2):198-203 [ Links ]
10. Pancherz H, Zieber K, Hoyer B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: a comparative study in children. Angle Orthod 1997;67(2):111- 20. [ Links ]
11. Jacob HB, Buschang PH. Mandibular growth comparisons of Class I and Class II division 1 skeletofacial patterns. Angle Orthod 2014;84(5):755-61. [ Links ]
12. Soh J, Sandham A, Chan YH. Occlusal status in Asian male adults: prevalence and ethnic variation. Angle Orthod 2005;75(5):814-20. [ Links ]
13. Burgersdijk R, Truin GJ, Frankenmolen F, Kalsbeek H, van't Hot M, Mulder J. Malocclusion and orthodontic treatment need of 15-74-year-old Dutch adults.Community Dent Oral Epidemiol 1991;19(2):64-7. [ Links ]
14. Tang EL. Occlusal features of Chinese adults in Hong Kong. Aust Orthod J 1994;13(3):159. [ Links ]
15. Ardani IGAW, Sanjaya ML, Sjamsudin J. Cephalometric characteristic of skeletal class II malocclusion in Javanese population at Universitas Airlangga Dental Hospital. Contemp Clin Dent 2018;9(Suppl 2):S342. [ Links ]
16. Burgos D. Prevalencia de maloclusiones en niños y adolescentes de 6 a 15 años en Frutillar, Chile. Int J Odontostomat 2014;8(1):13-9. [ Links ]
17. Aguirre Cortez P. Frecuencia de clases esqueletales segun el analisis de Steiner en pacientes entre 15 y 25 anos de edad del Programa de Especialización en Ortodoncia y Ortopedia Dentofacial de la Universidad de Talca entre los anos 2005-2009: Universidad de Talca (Chile). Tesis de grado. Escuela de Odontologia. Facultad de Ciencias de la Salud, Universidad de Talca, 2011. [ Links ]
18. Iturriaga R, Whittle M. Analysis of 1000 cases of dentomaxillaty anomalies. Rev Dent Chile. 1990;81(3):116-23. [ Links ]
19. Baccetti T, Stahl F, McNamara Jr JA. Dentofacial growth changes in subjects with untreated Class II malocclusion from late puberty through young adulthood. Am J Orthod Dentofacial Orthop 2009;135(2):148-54. [ Links ]
20. Sidlauskas A, Svalkauskiene V, Sidlauskas M. Assessment of skeletal and dental pattern of Class II division 1 malocclusion with relevance to clinical practice. Stomatologija. 2006;8(1):3-8. [ Links ]
21. McNamara JA. Components of Class II malocclusion in children 8-10 years of age. Angle Orthodon 1981;51(3):177-202. [ Links ]
22. Mizoguchi I, Toriya N, Nakao Y. Growth of the mandible and biological characteristics of the mandibular condylar cartilage. Japanese Dental Sci Rev. 2013;49(4):139-50. ´ [ Links ]
23. Rothstein T, Yoon-Tarlie C. Dental and facial skeletal characteristics and growth of males and females with Class II, Division 1 malocclusion between the ages of 10 and 14 (revisited)-Part I: Characteristics of size, form, and position.Am J Orthod Dentofacial Orthop 2000;117(3):320-32. [ Links ]
24. Sharma BP, Xin C. Comparative cephalometric analysis of angle class II division 1 malocclusion between Chinese male and female subjects. Orthodont J Nepal. 2014;4(2):21-3. [ Links ]
25. Lacerda RHW, Silva AWC, Ramos TB. Assessment of upper airways measurements in patients with mandibular skeletal Class II malocclusion. Dental Press J Orthod 2015;20(5):86- 93. [ Links ]
26. Kannan A, Sathyanarayana HP, Padmanabhan S. Effect of functional appliances on the airway dimensions in patients with skeletal class II malocclusion: A systematic review. J Orthod Sci 2017;6(2):54. [ Links ]
27. Zaghi S, Holty J-EC, Certal V, Abdullatif J, Guilleminault C, Powell NB, Riley RW, Camacho M. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngology-Head & Neck Surgery. 2016;142(1):58-66. [ Links ]
28. Rojo-Sanchis C, Almerich-Silla JM, Paredes-Gallardo V, Montiel-Company JM, Bellot-Arcís C. Impact of bimaxillary advancement surgery on the upper airway and on obstructive sleep apnea syndrome: A meta-analysis. Sci Rep 2018;8(1):1-8. [ Links ]
29. Ellis III E, McNamara Jr JA, Lawrence TM. Components of adult Class II open-bite malocclusion. J Oral Maxillofac Surg 1985;43(2):92-105. [ Links ]
Conflict of interest declaration: The authors have no conflict of interest regarding the publication of this paper.
Authorship contribution 1. Conception and design of study 2. Acquisition of data 3. Data analysis 4. Discussion of results 5. Drafting of the manuscript 6. Approval of the final version of the manuscript FV has contributed in 2, 3, 4, 5, 6. CB has contributed in 2, 3, 4. RC has contributed in 2, 3, 4. AD has contributed in 1, 3, 4, 5, 6. GM has contributed in 1, 3, 4, 5, 6.
Received: April 27, 2021; Accepted: May 10, 2022











 texto en
texto en