Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.24 no.39 Montevideo jun. 2022 Epub 01-Jun-2022
https://doi.org/10.22592/ode2022n39e407
Case report
Diagnosis and conservative treatment of odontogenic keratocyst: a case presentation
1 Departamento de Odontología. Facultad de Ciencias de la Salud. Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú. lida.velazque@unsaac.edu.pe
2 Departamento de Farmacia y Bioquímica. Facultad de Ciencias de la Salud. Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú.
3 Departamento de Medicina Humana. Facultad de Ciencias de la Salud. Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú.
Odontogenic keratocysts are potentially aggressive and have high recurrence rates. Their clinical and radiographic features are not clearly defined. They can occur at any stage of life. Seventy to 80% are located in the mandible, commonly in the area between the third molar and the mandibular angle, from where they grow towards the ramus and body. They are generally asymptomatic lesions that can grow considerably. They are often found on routine radiographs. This paper reports the case of a 40-year-old woman with a parakeratinized odontogenic keratocyst. After assessing the cyst's clinical, radiographic and histopathological features, we managed and treated the condition timely, conservatively, and with satisfactory results. We concluded that preparing the patient's dental history carefully and based on clinical, radiographic, and histopathological findings allowed us to make the correct diagnosis and develop the necessary treatment plan.
Keywords: Parakeratinized odontogenic keratocyst; keratocystic odontogenic tumor; diagnosis
El queratoquiste odontogénico es una entidad potencialmente agresiva y de alta recurrencia, con características clínicas y radiográficas no definidas claramente. Se presenta en cualquier etapa de la vida. El 70 a 80% se ubican en la mandíbula, comúnmente en la región de tercer molar y ángulo mandibular desde donde progresan hacia la rama y cuerpo. Son lesiones en general asintomáticas que pueden alcanzar dimensiones notables. A menudo se encuentran en el examen radiográfico de rutina. El objetivo del presente artículo es reportar el caso de una mujer de 40 años de edad, con un queratoquiste odontogénico paraqueratinizado, evaluando sus características clínicas, radiográficas e histopatológicas que llevaron a un manejo y tratamiento conservador oportuno y adecuado con resultados satisfactorios. Concluyendo que la minuciosa elaboración de la historia clínica basado en hallazgos clínicos, radiográficos e histopatológicos conduce a un diagnóstico correcto, que permite la elaboración de un plan de tratamiento adecuado.
Palabras Claves: Queratoquiste Odontogénico Paraqueratinizado; Tumor Odontogénico Queratoquístico; diagnóstico
O Queratocisto odontogênico potencialmente agressivo e de alta recorrência, com características clínicas e radiográficas não claramente definidas. Ocorre em qualquer estágio da vida. 70 a 80% estão localizados na mandíbula, geralmente na região do terceiro molar e no ângulo mandibular de onde progridem para o ramo e o corpo. São lesões geralmente assintomáticas que podem atingir dimensões notáveis. Eles são freqüentemente encontrados no exame radiográfico de rotina. O objetivo deste artigo é relatar o caso de uma mulher de 40 anos com um queratocisto odontogênico paraqueratinizado, avaliando suas características clínicas, radiográficas e histopatológicas que conducem ao manejo e tratamento conservador oportuno e adequado, com resultados satisfatórios. Concluindo que o cuidadoso preparo da história médica com base em achados clínicos, radiográficos e histopatológicos leva a um diagnóstico correto, o que permite o desenvolvimento de um plano de tratamento adequado.
Palavras-Chave: Ceratocisto odontogênico paraqueratinizado; Ceratocisto de tumor odontogênico; diagnóstico
Introduction
The term "odontogenic keratocyst" (OK) was initially defined by the World Health Organization (WHO) in 2005 as a benign intraosseous tumor with a characteristic lining of parakeratinized stratified squamous epithelium and potentially aggressive, infiltrative behavior. (1,2 In 2017, the WHO reclassified the condition as a cyst.3 The OK presents microscopically, with an aggressive clinical growth, and biological behavior of high recurrence: between 25 and 60%. 2,4,5 Its etiology is still debated: it could arise from the proliferation of the epithelial dental lamina of the jaws,2 from the basal cells of the oral epithelium,6,7 or the enamel organ by degeneration of the stellate reticulum, before the start of enamel apposition. 7
It is quite usual to find an OK clinically or radiographically: it amounts to approximately 10 to 20% of all odontogenic cysts. It is the third most common cyst of the mandible. (3 However, it amounts to 28.7% of cases detected in a radiograph.8) They occur at any age, from ages 7 to 885), but they are most commonly diagnosed between the second and third decades of life. 2 The most frequent location is the mandible (70-80%), mainly in the lower third molar and mandibular angle area (50-75%), from where the cyst projects towards the mandibular ramus and body,9,10 with a higher prevalence among males. 5,11
It generally presents as an asymptomatic, non-destructive, slow, and expansive growth of long evolution where the skin and oral mucosa appear normal, but sometimes there is palpable crepitus. In most cases, it is associated with impacted teeth. 12 Only advanced cases present an increase in volume that involves the bone plate (lingual in the mandible and buccal in the maxilla). They can grow significantly, so they also present tumorization and pain. 2,10
Radiographically it has various presentations: sometimes with an oval or rounded cavity appearance,5,10 mostly unilocular and with multilocularity in extensive lesions. In over 40% of cases it is associated with the crown of a retained tooth.4 It rarely presents as an interradicular or periradicular radiolucent image and is associated with vital teeth.12 The OK appears as a radiolucent image, with well-defined and thin borders, with or without a peripheral sclerotic halo.12,13
In some cases, they resemble dentigerous cysts on radiographs when associated with tooth retention. Multilocular lesions resemble ameloblastoma, and smaller lesions resemble residual cysts, lateral periodontal cysts, and radicular cysts. 2
Most are single lesions, but multiple lesions may occur exceptionally. This is known as the Gorlin-Goltz syndrome or "nevoid basal cell carcinoma syndrome." 5
Histologically, the OK presents two widespread variants. The first is the parakeratinized OK, with thin stratified pavement epithelium, usually 8-10 layers thick, and a parakeratinized and corrugated surface. It also features a flat epithelium-connective tissue interface, i.e., without dermal-epithelial invaginations, where the basal cells have polarized, hyperchromatic nuclei arranged in rows. The second variant, the orthokeratinized cyst, is less frequent and has a thin, granular epithelial lining and a thicker, non-corrugated orthokeratin lining, with a keratinized lumen and basal cells difficult to detect. 1,14 Some lesions present both parakeratotic and orthokeratotic areas. 2,6,10
Both histologic variants show different clinical behaviors. Orthokeratinized cysts have a lower growth potential and recurrence rate and are frequently associated with a retained tooth. Radiographically, they are most often unilocular and located in the maxilla or anterior area of the mandible. 15
The most widely accepted OK treatment in the literature is simple lesion enucleation followed by curettage to reduce the high recurrence rates: the lesion might reappear up to ten years post-surgery. The various treatment options include simple enucleation, which is not recommended due to the high recurrence rates: 17-56%. Chemical adjuncts can be used, such as Carnoy's solution after enucleation (absolute alcohol, chloroform, 98% acetic acid, and ferric chloride)15,16 or cryotherapy, which reduces recurrence from 1 to 8.7%. Another treatment option is pre-surgical decompression by marsupialization to reduce the lesion size and intraluminal pressure, making surgery less aggressive. En bloc mandibular resection is usually indicated in extensive lesions. 2,11,15,16
This paper describes the clinical and histopathological management and the planning of conservative surgical treatment of a large right mandibular odontogenic keratocyst in a 40-year-old woman involving an adjacent tooth and its postoperative follow-up.
Case description
A 32-year-old female patient from Cusco, Peru, married, an accountant, seeking care at the Centro de Radiodiagnóstico Estomatológico y Maxilofacial (CERES), referred by the local dental clinic. She reported slight pain on contact on the right hemiface and a sensation of liquid oozing from the lower right second molar with a foul odor, with approximately four months of evolution. The patient reports that her lower right third molar was removed due to intense pain around one year ago, with no documentary evidence of radiographic diagnosis.
The general clinical examination revealed mild facial asymmetry with increased volume of the right posteroinferior hemiface, with effacement of the right nasolabial line, pain on deep palpation, and presence of crepitus, with no signs of inflammation or palpable lymph nodes (Fig. 1A).
The intraoral clinical examination revealed a slight increase in the volume of the vestibular mucosa of the lower right molar region without color alterations. We detected prominent superficial blood vessels, a slight expansion of the external cortex, crepitus, moderate pain on palpation, absence of tooth 4.8, increased sensitivity of tooth 4.7 to thermal tests, and a tingling sensation on vertical percussion. There was evidence of increased crepitus and pain radiating in a caudal direction on deep palpation of the right mandibular ramus on its inner side. (Fig. 1B).
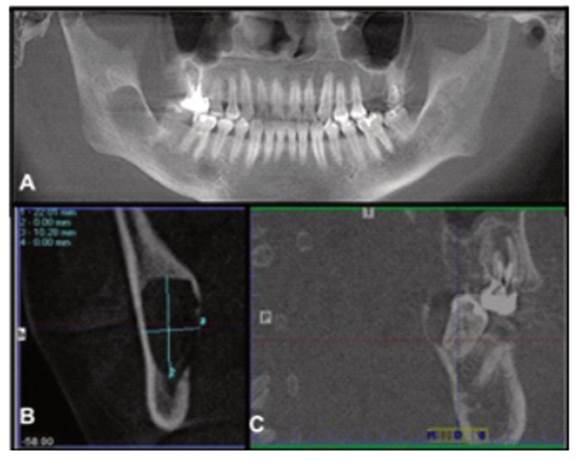
The panoramic radiograph shows a large unilocular and radiolucent lesion measuring approximately 5x4 cm, with defined borders, corticated edges, projecting distally from the root of tooth 4.7, extending in the cephalic direction until roughly the middle of the mandibular ramus. Its growth compromises tooth 4.7, the posterior region of the mandibular body, and right mandibular ramus and angle. Tooth 4.8 is absent, and there is a slight caudal displacement of the mandibular canal.
The CBCT, in its panoramic reconstruction (Fig. 2A), confirms an extensive hypodense lesion with defined and corticated borders involving the root of tooth 4.7. The transverse reconstruction shows a 22.01x10.28 mm oval lesion, with cortical expansion and severe thinning with perforation of the lingual cortex (Fig. 2B). The sagittal reconstruction shows exposure of the distal and palatal region of tooth 4.7 with complete alveolar bone resorption. We also detected a slight displacement of the mandibular canal in the caudal direction (Fig. 2C).
After a thorough clinical and radiological examination, a presumptive diagnosis of parakeratinized odontogenic keratocyst and ameloblastoma was made. The patient was referred to the specialized dental clinic of the National University of San Antonio Abad del Cusco (Universidad Nacional de San Antonio Abad del Cusco) for treatment and follow-up.
After preparing the treatment plan, the patient was asked to sign the informed consent form, and preoperative laboratory tests were ordered. As typical values were found, we decided to perform the aspiration test and subsequent excisional biopsy
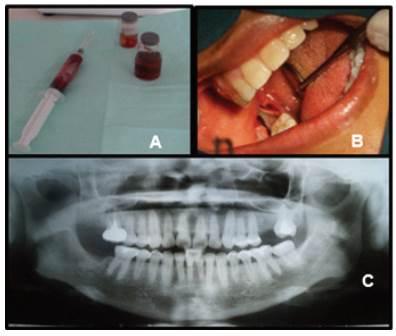
Aspiration was performed before the excisional biopsy. Abundant bloody fluid and traces of tiny granules of apparent necrotic tissue were found (Fig. 3A). Total enucleation was performed. A single retromolar incision was made under local lower truncal anesthesia to open the vestibular and lingual flaps. The lesion was isolated entirely for subsequent enucleation (Fig. 3B), followed by thorough curettage and lavage of the bone cavity with abundant sterile saline solution. Tooth 4.7 was extracted and sutured with polypropylene to prevent recurrence. Painkillers, intramuscular anti-inflammatories and antibiotics, and alcohol-free mouthwash were prescribed.
The sample obtained was placed in 10% formalin and sent for histopathological study (Fig. 3A). The sections studied showed flat stratified epithelium with inflamed stroma and a corrugated parakeratinized surface, with basal cells with hyperchromatic nuclei. In some areas, the epithelium was separated from the cystic capsule, which confirmed the diagnosis of parakeratinized odontogenic keratocyst.
The sutures were removed, and the first postoperative control was performed ten days later. Three months later, the patient was seen for a clinical check-up and an evaluation with a panoramic radiograph. The radiograph showed excellent healing, no recurrence, and bone neoformation in the region of the lesion (Fig. 3C). Tooth 4.6 tested positive for pulp vitality.
Discussion
The odontogenic keratocyst is one of the most studied cysts in oral pathology due to its aggressive behavior, high recurrence, and histopathological features. It is one of the most frequent odontogenic cystic lesions (approximately 10 to 15%).2 Histologically, they can be of primordial origin (60% of cases) when they arise from the remains of dental lamina and are not associated with teeth; and of dentigerous origin in 40% of cases, derived from a reduced enamel organ and associated with retained teeth.16
Most OKs reported in the literature show a preference for males at a 1:1.4 ratio.5,16 They can appear at any age, but more frequently in the third decade of life. They generally involve the posterior region of the mandible at the level of the third molars.1,2,4,5,11 On the contrary, our case reports a lesion in a female patient in her forties. The lesion is unlikely to be associated with a retained tooth, so it must be a primordial cyst, which tend to go unnoticed. What is consistent with the literature is its frequent location.
The lesion generally presents increased volume, pain, and marked bone expansion on clinical examination. However, most lesions are asymptomatic, which does not coincide with our case. Although there is no significant volume increase, there is pain at the slightest contact or superficial palpation, signs, and symptoms that point to a pathology whose magnitude cannot be predicted. Therefore, this type of lesion with clinical features that may mask the severity of the clinical picture is known as "casual findings."
Radiographically, the lesions' multilocular aspect and defined and corticated borders point to a parakeratinized OK, while the unilocular aspect is more associated with the orthokeratinized type.2 This was not found in our case because the lesion was parakeratinized and unilocular.
The treatments proposed in the literature are manifold. However, the one with the lowest percentage of recurrence is total lesion enucleation, followed by curettage, abundant washing with saline solution, and extraction of compromised parts. All these essential procedures were performed on our patient. These procedures should have a postoperative follow-up of up to ten years to report the success and healing of the lesion and avoid recurrence caused by multiple factors, including incomplete enucleation and curettage due to a weak cyst wall or invasion of adjacent soft tissues, as well as satellite cysts given the high mitotic activity.2,4,11
The case reported supports most of the clinical manifestations published in the literature. However, this lesion does not present fully defined clinical features that would make its recognition and diagnosis accurate. Therefore, we aim to emphasize the importance of a complete and well-developed clinical history, which will allow for an accurate and timely diagnosis so the patient can be referred to a specialist and, if necessary, other medical specialists can be consulted.
Although most lesions are benign, they can create significant asymmetries and facial deformities in the long term, leading to esthetic and psychological problems.
The literature reports an increasingly high number of new cases and types of OKs, generally associated with asymptomatic patients and routine radiographic examinations. Therefore we conclude that proper knowledge and use of complementary examinations is essential, as well as clinical and radiographic follow-ups up to 10 years after the procedure. The recurrence rate of this pathology could be the cause of new clinical presentations.
REFERENCES
1. Philipsen HP. Keratocystic odontogenic tumour. In: Barnes L, Evenson JW, Reichart P, Sidransky D. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. p. 306-307. [ Links ]
2. Pazdera J, Kolar Z, Zboril V, Tvrdy P, Pink R. Odontogenic keratocysts/ keratocystic odontogenic tumours: biological characteristics, clinical manifestation and treatment. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014; 158(2):170-174. [ Links ]
3. Wright JM, Vered M. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol. 2017;11(1):68-77. [ Links ]
4. Kebede B, Dejene D, Teka A, Girma B, Aguirre EP, Guerra NEP. Big Keratocystic Odontogenic Tumor of the Mandible: A Case Report. Ethiop J Health Sci. 2016; 26(5):491-496. [ Links ]
5. Kahraman D, Gunhan O, Celasun B. A series of 240 odontogenic keratocysts: Should we continue to use the terminology of 'keratocystic odontogenic tumour' for the solid variant of odontogenic keratocyst? J Craniomaxillofac Surg. 2018; 46(6):942-946. [ Links ]
6. Wright JM, Vered M. Update from the 4th edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck Pathol. 2017; 11(1):68-77. [ Links ]
7. Quezada M, Delgado W, Calderón V. Características radiográficas de los queratoquistes odontogénicos paraqueratinizados del maxilar inferior. Rev Estomatol Herediana 2005; 15(2):112-118. [ Links ]
8. Hashmi AA, Edhi MM, Faridi N, Hosein M, Khan M. Mutiple keratocystic odontogenic tumors (KCOT) in a patient with Gorlin syndrome: a case report with late presentation and absence of skin manifestations. BMC Res Notes. 2016; 22(9):357. [ Links ]
9. Naruse T, Yamashita K, Yanamoto S, Rokutanda S, Matsushita Y, Sakamoto Y, et al. Histopathological and immunohistochemical study in keratocystic odontogenic tumors: Predictive factors of recurrence. Oncol Lett. 2017; 13(5):3487-3493. [ Links ]
10. Menon S. Keratocystic Odontogenic Tumours: Etiology, Pathogenesi and Treatment Revisited. J Maxillofac Oral Surg. 2015; 14(3):541-7. [ Links ]
11. Robles P, Roa I. Keratocystic odontogenic tumor: Clinicopathological aspects and treatment. J Oral Res. 2014; 3(4):249-256. [ Links ]
12. Kodali R, Guttikondaleela N, Chintada K. Conservative Management of A Massive Keratocystic Odontogenic Tumour of Mandible: A Case Report and Review. J Res Adv Dent. 2014; 1:96-101. [ Links ]
13. Bello IO. Keratocystic odontogenic tumor: A biopsy service's experience with 104 solitary, multiple and recurrent lesions. Med Oral Patol Oral Cir Bucal. 2016; 21(5):538-546. [ Links ]
14. Deyhimi P, Hashemzadeh Z. Study of the biologic behavior of odontogenic keratocyst and orthokeratinaized odontogenic cyst using TGF-alpha and P53 markers. Pathol Res Pract. 2014; 210(4):201-214. [ Links ]
15. de Molon RS, Verzola MH, Pires LC, Mascarenhas VI, da Silva RB, Cirelli JA, et al. Five years follow-up of a keratocyst odontogenic tumor treated by marsupialization and enucleation: A case report and literature review. Contemp Clin Dent. 2015; 6(1):106-110. [ Links ]
16. Alchalabi NJ, Merza AM, Issa SA. Using Carnoy's Solution in Treatment of Keratocystic Odontogenic Tumor. Ann Maxillofac Surg. 2017; 7(1):51-56. [ Links ]
Conflict of interest declaration: The authors have no conflict of interest regarding the publication of this paper.
Authorship contribution: 1. Conception and design of study 2. Acquisition of data 3. Data analysis 4. Discussion of results 5. Drafting of the manuscript 6. Approval of the final version of the manuscript. LVR has contributed in 1, 2, 3, 4, 5, 6. CAC has contributed in 2, 4, 5. CJVH has contributed in 3, 4, 5. GVR has contributed in 2, 3, 5.
Received: April 23, 2020; Accepted: November 23, 2021











 texto em
texto em