Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.23 no.38 Montevideo 2021 Epub Sep 30, 2021
https://doi.org/10.22592/ode2021n37e304
Update
Oral manifestations associated with SARS-COV-2: A literature review
1Facultad de Odontología Universidad de Concepción, Chile. n475sg@gmail.com
2Departamento de patología y diagnóstico, Facultad de Odontología, Universidad de Concepción, Chile.
Objective:
Identify the main oral manifestations associated with COVID19 and describe their location in the oral cavity.
Methods:
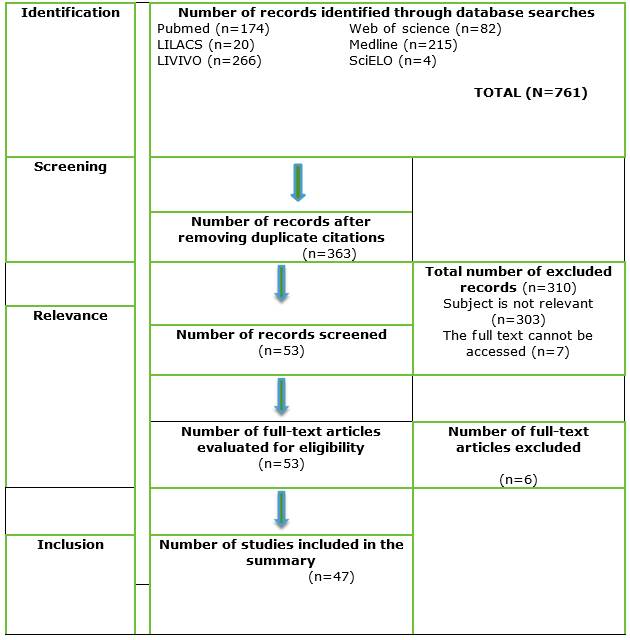
The literature search was conducted in PubMed, Medline, LILACS, LIVIVO, Web of Science, and SciELO. The following words were searched for: oral mucosa, oral mucosa lesion, oral manifestations, COVID-19, and SARS-CoV-2. Duplicate articles were eliminated, and the pieces were shortlisted. Finally, inclusion and exclusion criteria were applied.
Results:
This study included 47 articles. The main oral manifestations in patients with COVID-19 are taste disorders, xerostomia, ulcers, vesicles, and others located in different areas of the oral mucosa.
Conclusions
More studies are needed to determine the potential oral etiopathogenesis of SARS-CoV-2. Moreover, dentists play a significant role in the multidisciplinary and telemedicine team.
Keywords: COVID-19; oral manifestation; oral mucosa
Objetivo:
Identificar las principales manifestaciones y describir su ubicación en la cavidad oral en pacientes COVID-19.
Métodos:
Se utilizaron las bases de datos PubMed, Medline, LILACS, LIVIVO, Web of Science y SciELO; utilizando los términos de búsqueda oral mucosa, oral mucosa lesion, oral manifestations, COVID-19 y SARS-CoV-2. Se eliminaron duplicados, luego se realizó preselección de artículos, y finalmente se aplicaron los criterios de inclusión y exclusión.
Resultados:
Se seleccionaron 47 publicaciones, encontrando manifestaciones orales en pacientes COVID-19 tales como alteración en gusto, xerostomía, úlceras, vesículas, entre otras; ubicándose en diferentes áreas de la mucosa oral.
Conclusiones:
Se necesitan más estudios para vislumbrar la posible etiopatogenia a nivel oral del SARS-CoV-2. Además, se destaca el rol del odontólogo en el equipo multidisciplinario y en la teleconsulta.
Palabras clave: COVID-19; manifestación oral; mucosa oral
Objetivo:
Identificar as principais manifestações e descobrir sua ubiquação na cavidade oral em pacientes com COVID-19.
Método:
Foram utilizadas as bases de dados PubMed, Medline, LILACS, LIVIVO, Web of Science e SciELO; utilizando os termos de pesquisa oral mucosa, oral mucosa lesion, oral manifestations, COVID-19 e SARS-CoV-2. Duplicadas foram removidas, depois uma pré-seleção de artigos foi feita, e finalmente os critérios de inclusão e exclusão foram aplicados.
Resultados:
Foram selecionadas 47 publicações, encontrando manifestações orais em pacientes com COVID-19, tais como alterações no paladar, xerostomia, ulcerações, vesículas, entre outros; localizando-as em diferentes áreas da mucosa oral.
Conclusão:
São precisos mais estudos pra vislumbrar a possível etiopatogenia a nível oral do SARS-CoV-2. Ademais, destaca-se o role do odontólogo na equipe multidisciplinar e na tele consulta.
Palavras-chave: COVID-19; Manifestação oral; mucosa oral
Introduction
The new infectious disease Coronavirus 2019 (COVID-19), whose etiology is Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCoV2), has had a massive impact worldwide given its transmission rate, the resulting severe respiratory disorders, and the number of deaths globally. All this significantly compromises people’s quality of life.1 Since it originated in Wuhan, China, the disease has reached a high infectivity rate. Projections estimate 47 million cases worldwide and a mortality rate ranging from 3% to 12%. Over one million people have died.1-3
The specific origin of the pandemic is not fully understood. Although it is unclear how humans acquired the disease, it is estimated that it involved an animal. Bats are the main wild beings that are reservoirs for this type of virus. A viral jump occurred between this animal and a human being in Wuhan, China, in November 2019.2,4
The main infection routes of SARSCoV2 in humans are saliva droplets expelled when talking1,2,5-9 or sneezing within a distance of two meters or when in contact with exposed surfaces.2,6-9 Fifty percent of transmissions occur through exposure to asymptomatic people.2 It is important to note that patients can transmit the infection up to two weeks after recovering from the disease.4
Current research shows that the SARSCoV2 virus invades human cells through the angiotensin-converting enzyme 2 (ACE2) receptor.1,7,9-23 In this way, cells with ACE2 receptor distribution can become hosts to the virus and cause an inflammatory response in adjacent organs and tissues, including the oral cavity.1,7,8,10,12,14,16-19,21-28
This literature review aims to identify the main oral manifestations in patients with COVID19 and to describe their location in the oral cavity.
Materials and methods
This literature review included the following stages: selecting the topic, defining the objectives, stating the inclusion and exclusion criteria, developing a work plan for the literature search, selecting, and retrieving the studies that meet the criteria, collecting data to analyze and summarize the results, and finally, drawing conclusions.
The search was conducted from 9 October to 30 December 2020 in PubMed, Medline, LILACS, LIVIVO, Web of Science, and SciELO.
The search terms defined for the database search were: oral mucosa, oral mucosa lesion, oral manifestations, COVID-19, and SARS-CoV-2, with boolean operators OR and AND. Results: ((COVID-19) OR (SARS-CoV-2)) AND (mucosa oral)), ((COVID-19) OR (SARS-CoV-2)) AND (oral mucosa lesion)) and ((COVID-19) OR (SARS-CoV-2)) AND (oral manifestations)). The title and abstract were read to determine relevance. Then, the full texts were read to determine if they met the inclusion and exclusion criteria.
The inclusion criteria covered articles published within the last two years that contain the search terms in Spanish and English (Fig. 1).
The following articles were excluded: studies conducted on animals, focused on treating patients infected with the SARSCoV2 virus, COVID19 patients without oral manifestations, and those related to prevention and/or biosafety measures that did not meet our objectives.
Development
Duplicate articles were discarded and studies that met the inclusion and exclusion criteria were selected. The final selection included 47 articles: 9 case reports, 1 case report with narrative literature review, 2 systematic reviews, 3 critical reviews, 9 narrative reviews, 4 observational studies, and 19 letters to the editor. In addition, information from one article and two websites was included in the introduction.
The cases reported in the literature describe heterogeneous lesions between patients and even in the same patient.10-13 What varies is the presentation, location, and size.5,10,12,29 Oral manifestations have appeared in healthy COVID-19 patients with no relevant medical history,1,5,12,13,18,30-33 and in patients with underlying conditions.1,7,10,12,13,16,18,23,27-30,33-41
The manifestations that are mentioned more frequently are taste disorders and ulcers, while the least mentioned are pustules, glossitis, and geographic tongue. The main manifestations found are described below (Table 1):
Table 1: Oral manifestations reported in patients with COVID-19
| Oral manifestation | Type of publication | References |
|---|---|---|
| Taste disorders | 5 case reports 2 systematic reviews 7 narrative reviews 2 critical reviews 10 letters to the editor 3 observational studies 1 case report with narrative literature review | 30 references (1,6-12,14,16-19,21-24,26,29,30,33,36,38,40-46) |
| Burning sensation | 1 case report 3 narrative reviews 3 letters to the editor 2 observational studies 1 case report with narrative literature review | 10 references (6,8,12,18,27,36,39,41,44,47) |
| Xerostomia | 2 case reports 5 narrative reviews 1 critical review 2 letters to the editor 2 observational studies | 12 references (5,6,8-10,16-18,24,29,36,47) |
| Halitosis | 3 narrative reviews 2 letters to the editor | 5 references (16,17,25,27,48) |
| Erythema | 4 case reports 1 narrative review 1 systematic review 3 critical reviews 4 letters to the editor 1 observational study 1 clinical case with narrative literature review | 15 references (1,9-13,19,20,27,28,30,31,41,46,49) |
| Petechias | 2 case reports 4 narrative reviews 1 systematic review 2 critical reviews 3 letters to the editor 1 clinical case with narrative literature review | 13 references (1,5,9,11,13,15,17,18,20,26,27,31,41) |
| Macules | 2 case reports 1 narrative review 1 systematic review 2 critical reviews 3 letters to the editor 1 observational study 1 clinical case with narrative literature review | 11 references (10-13,17,19,20,26,29,41,47) |
| Bulla/blisters | 3 case reports 5 narrative reviews 1 systematic review 3 critical reviews 3 letters to the editor 1 observational study 1 clinical case with narrative literature review | 17 references (8,9,11,12,15-20,23,26,28,30,37,41,49) |
| Pustules | 1 case report 1 narrative review 2 letters to the editor | 4 references (13,27,31,32) |
| Ulcers | 6 case reports 6 narrative reviews 1 systematic review 3 critical reviews 11 letters to the editor 2 observational studies 1 clinical case with narrative literature review | 30 references (1,5,6,8-13,15-20,23,25-30,33-35,38,41,44-46) |
| Desquamative gingivitis | 2 case reports 3 narrative reviews 1 systematic review 2 critical reviews 1 letter to the editor | 9 references (9,11,12,15,18,19,25,27,30) |
| Salivary gland infection | 3 narrative reviews 2 critical reviews 2 letters to the editor 1 clinical case with narrative literature review | 8 references (8,19-21,24,28,41,45) |
| Geographic tongue | 2 letters to the editor | 2 references (6,44) |
| Glossitis | 3 narrative reviews 1 critical review 2 letters to the editor | 6 references (9,16,17,27,39.44) |
| Candida coinfection | 2 case reports 1 narrative review 1 systematic review 2 letters to the editor 1 observational study 1 clinical case with narrative literature review | 8 references (5,6,10,11,17,39,41,46) |
| Herpetiform lesions | 4 case reports 3 narrative reviews 1 systematic review 1 critical review 3 letters to the editor 1 observational study 1 clinical case with narrative literature review | 14 references (1,9-11,14,17,18,26,27,30,33,41,42,46) |
The location of lesions is unspecific, but they appear mainly on the palate, tongue (mainly on the dorsum), and also lip (inners side and semi mucosa). Lesions are also reported in the oral mucosa, gingiva, and oropharynx (Table 2).
Table 2: Localization of oral manifestations reported in patients with COVID-19
| Localization | Type of publication | References |
|---|---|---|
| Palate | 3 case reports 4 narrative reviews 1 systematic review 2 critical reviews 10 letters to the editor 1 observational study 1 clinical case with narrative literature review | 22 references (1,6,9,11-13,15,17,18,20,23,26-31,35,38,39,41,43) |
| Tongue | 5 case reports 2 narrative reviews 1 systematic review 2 critical reviews 11 letters to the editor 2 observational studies 1 clinical case with narrative literature review | 24 references (1,5,6,9-12,17,20,23,26-29,32,33,35,38,39,41,44-46,49) |
| Lip | 6 case reports 4 narrative reviews 1 systematic review 2 critical reviews 7 letters to the editor 2 observational studies 1 clinical case with narrative literature review | 23 references (1,5,6,9,11,13,15,17,18,20,23,26-30,34,37,38,41,42,46,49) |
| Oral mucosa | 2 case reports 2 narrative reviews 1 systematic review 1 critical review 3 letters to the editor 1 observational study | 10 references (1,9,11,15,27,28,29,37,46.49) |
| Gum | 1 case report 3 narrative reviews 1 systematic review 1 critical review 5 letters to the editor 1 clinical case with narrative literature review | 12 references (5,6,9,11,13,15,18,26-28,41,48) |
| Oropharynx | 2 case reports 2 narrative reviews 1 systematic review 2 letters to the editor 1 observational study | 8 references (5,10,11,13,18,23,27,31) |
Discussion
Although oral mucosa lesions have been reported in patients infected with SARS-COV-2 virus, it is believed that the cause is not the virus itself, but that the lesions would be secondary to the drugs5,7,9-11,15,17,18,21,26,28,30,32,36,39,41,43,50 administered for the treatment, or due to the compromise and deterioration of the immune system,1,6,9-12,15-17,26,27,33,34,36,38,41,45,50 which also enables opportunistic infections.5,6,9-11,15-18,25-28,33,36,39,41,42,45,48,50 The most commonly reported conditions are Candida albicans coinfections5,6,10,11,17,39,41 and/or other viruses.1,9,10,16,17,27,33,41-43,45,46,50 Despite these assumptions, some of the studies reviewed theorize about SARS-CoV-2’s vascular and thrombotic effect on the oral mucosa.6,9,12,15,17,23,27,29,34 Similarly, oral mucosa lesions could be triggered by factors such as stress.5,8,18,22,25,26,32,37
We must emphasize the importance of the ACE2 receptor, which is distributed in the cell membrane of various organs and tissues, such as the respiratory tract, the nervous system, the digestive system, and the skeletal muscle.1,9,13,23,24,27 In the oral cavity, they appear in the oral1,7,8,12,16-19,21-27 and gingival (7,14,21,23,24 mucosa epithelial cells. There is a strong presence in tongue epithelial cells (1,7-11,14,15,17,18,21,24,25,27,33,36 and salivary glands.1,9-12,16-20,24,27,36 Due to this high expression,8,9,11,14,15,18,19,21,22,24,25,27,33, the tongue is described as a susceptible organ.14,19,25,33 Some authors say that salivary glands6,8,10,21,24,36 and periodontal pockets9,18,25,36,44 could act as virus reservoirs.
These ACE2 receptor would be the main SARSCoV2 receptors, causing cells that distribute this receptor to trigger inflammatory reactions in the associated organs and tissues.1,9,10,13 Therefore, several authors state that this interaction in the tongue could explain taste disorders in patients with COVID19.1,8-11,15-19,22,24 It has also been said that the interaction between the virus and this receptor alters the function of oral keratinocytes and the epithelial lining of the salivary gland ducts after infection.1 Additionally, saliva and nasal secretion could have high viral loads involved in these oral alterations.9,12
Multiple authors agree on the need for additional studies and thorough research1,5,9-16,23,24,26,28-31,34-36,42,43,50 to determine the pathogenic mechanisms of SARS-CoV-2 on oral tissues and thus determine whether oral mucosal lesions are directly or indirectly related to COVID19 progression.1
Conclusion
Oral manifestations in COVID-19 patients have been reported in multiple sites of the oral cavity and are highly heterogeneous. The subject is so new that the prevalence of these manifestations is still unknown since the cases reported are few compared to the number of infected patients. Additionally, most cases lack complementary tests, such as biopsies or hematology tests, which help identify the real etiological agent. All this leaves unanswered questions about the possible etiopathogenesis or factors that might influence the development of these lesions. Therefore, it is necessary to conduct further research.
Finally, it is essential to recognize that dentists are crucial members of the health and telemedicine teams. Dentists should perform a careful oral examination to diagnose, treat, and control the pain caused by the lesions described.
REFERENCES
1. Brandão TB, Gueiros LA, Melo TS, et al. Oral lesions in patients with SARS-CoV-2 infection: could the oral cavity be a target organ? Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;S2212-4403(20)31119-6. [ Links ]
2. World Health Organization. Coronavirus disease (COVID-19) pandemic. Situations Reports. EPI-WIN Updates (nº 28 What we know about COVID-19). 2020 Citado: 5 noviembre de 2020. Disponible en: Disponible en: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [ Links ]
3. Worldmeter. COVID-19 Coronavirus Pandemic. 2020. Citado: 20 de noviembre 2020. Disponible en: Disponible en: https://www.worldometers.info/coronavirus/ [ Links ]
4. Ortiz-Prado E, Simbaña-Rivera K, Gómez-Barreno L, et al. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn Microbiol Infect Dis. 2020;98(1):115094. [ Links ]
5. Corchuelo J, Ulloa FC. Oral manifestations in a patient with a history of asymptomatic COVID-19: Case report. Int J Infect Dis. 2020;100:154-157. [ Links ]
6. Díaz Rodríguez M, Jimenez Romera A, Villarroel M. Oral manifestations associated with COVID-19. Oral Dis. 2020; doi: 10.1111/odi.13555. [ Links ]
7. Orellana-Centeno JE, Morales-Castillo V, Guerrero SRN. Generalidades, manejos, cuidados y manifestaciones clínicas del SARS-CoV-2. Rev ADM. 2020;77(3):153-155. [ Links ]
8. Pant, B. COVID-19: Oral manifestations, impact and lessons for the future. Orthodontic Journal of Nepal. 2020; 10(2), 52-54. [ Links ]
9. Parra-Sanabria EA, Bermúdez-Bermúdez M, Peña-Vega CP, Rueda-Jiménez A. Manifestaciones orales y maxilofaciales asociadas a la COVID-19. Revisión de la literatura. Acta Odont Col. 2020; 10(Supl. COVID-19): 60-80. [ Links ]
10. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, De Paula RM, Cembranel AC, Santos-Silva AR, Guerra ENS. Oral mucosal lesions in a COVID-19 patient: New signs or secondary manifestations? Int J Infect Dis. 2020;97:326-328. [ Links ]
11. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca Canto G, Sugaya N, Santos-Silva AR, Guerra ENS. Oral Manifestations in Patients with COVID-19: A Living Systematic Review. J Dent Res. 2020;11:22034520957289. [ Links ]
12. Cruz Tapia RO, Peraza Labrador AJ, Guimaraes DM, Matos Valdez LH. Oral mucosal lesions in patients with SARS-CoV-2 infection. Report of four cases. Are they a true sign of COVID-19 disease? Spec Care Dentist. 2020;1-6. [ Links ]
13. Ciccarese G, Drago F, Boatti M, Porro A, Muzic SI, Parodi A. Oral erosions and petechiae during SARS-CoV-2 infection. J Med Virol. 2020;10.1002/jmv.26221. [ Links ]
14. Cornejo-Ovalle Marco, Espinoza-Santander Iris. COVID-19 y manifestaciones orales. Int. J. Odontostomat. 2020;14( 4 ):538-539. [ Links ]
15. Maciel PP, Martelli Ju´nior H, Martelli DRB, Machado RA, Andrade PV, Perez DEC, et al. COVID-19 pandemic: oral repercussions and its possible impact on oral health. Pesqui Bras Odontopediatria Cli´n Integr. 2020; 20(supp1):e0138. [ Links ]
16. Pedrosa MS, Sipert CR, Nogueira FN. Salivary glands, saliva and oral findings in COVID-19 infection. Pesqui Bras Odontopediatria Cli´n Integr. 2020; 20(supp1):e0104. [ Links ]
17. Nemeth-Kohanszky María Eugenia, Matus-Abásolo Carolina Paz, Carrasco-Soto Rolando Rafael. Manifestaciones Orales de la Infección por COVID-19. Int. J. Odontostomat. 2020; 14(4):555-560. [ Links ]
18. Gutiérrez Flores R, Zambrano Rodríguez G. Implicaciones bucales por COVID-19. Revisión de tema. Odontol Sanmarquina.2020;23(4):419-23. [ Links ]
19. Capocasale G, Nocini R, Faccioni P, Donadello D, Bertossi D, Albanese M, Zotti F. How to deal with coronavirus disease 2019: A comprehensive narrative review about oral involvement of the disease. Clin Exp Dent Res. 2020;10.1002/cre2.332. [ Links ]
20. Halboub E, Al-Maweri SA, Alanazi RH, Qaid NM, Abdulrab S. Orofacial manifestations of COVID-19: a brief review of the published literature. Braz Oral Res 2020;34:e124. [ Links ]
21. Odeh ND, Babkair H, Abu-Hammad S, Borzangy S, Abu-Hammad A, Abu-Hammad O. COVID-19: Present and Future Challenges for Dental Practice. Int J Environ Res Public Health. 2020;17(9):3151. [ Links ]
22. Abalo-Lojo JM, Pouso-Diz JM, Gonzalez F. Taste and Smell Dysfunction in COVID-19 Patients. Annals of Otology, Rhinology & Laryngology. 2020; 129(10):1041-1042. [ Links ]
23. Katz J,Yue S. Increased odds ratio for COVID 19 in patients with recurrent aphthous stomatitis. J Oral Pathol Med 2020;00:1-4. [ Links ]
24. Pastrian G. Presencia y expresio´n del receptor ACE2 (Target de SARS-CoV-2) en tejidos humanos y cavidad oral.Posibles rutas de infeccio´n en o´rganos orales. Int. J. Odontostomat. 2020;14(4):501-507. [ Links ]
25. Riad A, Kassem I, Hockova B, Badrah M, Klugar M. Halitosis in COVID-19 patients. Spec Care Dentist. 2020;1-3. [ Links ]
26. de Sousa FACG, Paradella TC. Considerations on oral manifestations of COVID-19. J Med Virol. 2021;93:667-668. [ Links ]
27. Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M. Oral manifestations of COVID -19 disease: A review article. Dermatologic Therapy. 2020;e14578. [ Links ]
28. Riad A, Klugar M, Krsek M. COVID-19-Related Oral Manifestations: Early Disease Features? Oral Dis. 2020;00:1-3. [ Links ]
29. Soares CD, Carvalho RA, Carvalho KA, Carvalho MG, Almeida OP. Letter to Editor: Oral lesions in a patient with COVID-19. Med Oral Patol Oral Cir Bucal. 2020;25(4):e563-e564. [ Links ]
30. Martín Carreras-Presas C, Amaro Sánchez J, López-Sánchez AF, Jané-Salas E, Somacarrera Pérez ML. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 2020;00:1-3. [ Links ]
31. Cebeci Kahraman F, Çaskurlu H. Mucosal involvement in a COVID-19-positive patient: A case report. Dermatol Ther. 2020;33(4):e13797. [ Links ]
32. Alzahrani MJ, Moussa MM, Alfaraj D. Acute Generalized Exanthematous Pustulosis After COVID-19 Infection: A Case Report From Saudi Arabia. Cureus. 2020;12(11):e11609. [ Links ]
33. Riad A, Kassem I, Hockova B, Badrah M, Klugar M. Tongue ulcers associated with SARS-CoV-2 infection: A case series. Oral Dis. 2020;00:1-3. [ Links ]
34. Cebeci Kahraman F, Özen T, Elibol T. Lip necrosis in a patient with paroxysmal nocturnal hemoglobinuria: Can it be triggered by COVID-19? J Cosmet Dermatol. 2020;19:3168-3170. [ Links ]
35. Ansari R, Gheitani M, Heidari F, Heidari F. Oral cavity lesions as a manifestation of the novel virus (COVID-19). Oral Dis. 2020. [ Links ]
36. Sinjari B, D'Ardes D, Santilli M, Rexhepi I, D'Addazio G, Di Carlo P, Chiacchiaretta P, Caputi S, Cipollone F. SARS-CoV-2 and Oral Manifestation: An Observational, Human Study. J Clin Med. 2020;9(10):3218. [ Links ]
37. Bakar Dertli?oglu S . Skin rashes in COVID-19: A report of three cases. J Health Sci Med 2020; 3(4): 490-492. [ Links ]
38. Bemquerer LM, de Arruda JAA, Soares MPD, Mesquita RA, Silva TA. The oral cavity cannot be forgotten in the COVID-19 era: is there a connection between dermatological and oral manifestations?, J American Academy Dermatol 2020; S0190-9622(20)33073-5. [ Links ]
39. Riad A, Gad A, Hockova B, Klugar M. Oral Candidiasis in Non-Severe COVID-19 Patients: Call for Antibiotic Stewardship. Oral Surg. 2020; doi: 10.1111/ors.12561. [ Links ]
40. Passarelli PC, Lopez MA, Mastandrea Bonaviri GN, Garcia-Godoy F, D'Addona A. Taste and smell as chemosensory dysfunctions in COVID-19 infection. Am J Dent. 2020;33(3):135-137. [ Links ]
41. Eghbali Zarch R, Hosseinzadeh P.COVID-19 from the perspective of dentists: A case report and brief review of more than 170 cases. Dermatologic Therapy.2021;e14717. [ Links ]
42. Kitakawa D, Oliveira FE, Neves de Castro P, Carvalho LFCS. Short report - Herpes simplex lesion in the lip semimucosa in a COVID-19 patient. Eur Rev Med Pharmacol Sci. 2020;24(17):9151-9153. [ Links ]
43. de Carvalho L, Kitakawa D, Cabral LAG. Oral lesions of herpes zoster in COVID-19 patients or truly associated to the disease? Oral Dis. 2020;00:1-2. [ Links ]
44. Nuno-Gonzalez A, Martin-Carrillo P, Magaletsky K, Martin Rios MD, Herranz Mañas C, Artigas et al. Prevalence of mucocutaneous manifestations in 666 patients with COVID-19 in a field hospital in Spain: oral and palmoplantar findings. Br J Dermatol. 2020;184:158-185. [ Links ]
45. Abu-Hammad S, Dar-Odeh N, Abu-Hammad O. SARS-CoV-2 and oral ulcers: A causative agent or a predisposing factor? Oral Dis. 2020;00:1-2. [ Links ]
46. Mascitti H, Bonsang B, Dinh A, Assan F, Perronne V, Leblanc T, Duran C, Bouchand F, Matt M, Le Gal A, N'guyen Van Thanh J, Lanore A, Jacob L, Kiavue N, Siméon S, Bessis S, de Truchis P, Landowski S, Davido B, Moreau F, Rameix-Welti MA, Gault E, Gaillard JL, Roux AL, Sivadon-Tardy V, Salomon E, El Sayed F, Carlier R, Emile JF, Perronne C, Bourgault-Villada I. Clinical Cutaneous Features of Patients Infected With SARS-CoV-2 Hospitalized for Pneumonia: A Cross-sectional Study. Open Forum Infect Dis. 2020;7(11):ofaa394. [ Links ]
48. Patel J, Woolley J. Necrotizing periodontal disease: Oral manifestation of COVID-19. Oral Dis. 2020;00:1-2. [ Links ]
50. Ponce JB, Tjioe KC. Overlapping findings or oral manifestations in new SARS-CoV-2 infection. Oral Dis. 2020;00:1-2. [ Links ]
Authorship contribution: 1. Conception and design of study 2. Acquisition of data 3. Data analysis 4. Discussion of results 5. Drafting of the manuscript 6. Approval of the final version of the manuscript NSG has contributed in 1, 2, 3, 4, 5, 6. TNT has contributed in 3, 4, 5, 6. GVC has contributed in 2, 3, 4, 5, 6. AMSR has contributed in 3, 4, 5, 6.
Received: January 15, 2021; Accepted: March 22, 2021











 text in
text in