Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.23 no.38 Montevideo 2021 Epub 01-Dic-2021
https://doi.org/10.22592/ode2021n37e214
Research
Oral health care beliefs among caregivers of the institutionalized elderly in Antofagasta, Chile, 2019
1Escuela de Odontología, Universidad Pedro de Valdivia, Chile
2Departamento de Odontología, Universidad de Antofagasta, Chile. constanza.garrido@uantof.cl
Objective:
to analyze oral health care related beliefs among caregivers of the institutionalized elderly in Antofagasta, Chile, 2019.
Material and methods:
A quantitative, observational, descriptive, cross-sectional study was conducted. Forty-nine caregivers were interviewed with the DCBS-sp questionnaire to determine their oral health care beliefs. STATA 14® was used to conduct the statistical analysis.
Results:
Of the caregivers interviewed, 36.73% have oral health training, and 97.96% feel they need training. Trained caregivers have significantly better average oral health scores on internal locus of control and self -efficacy.
Conclusions
Caregivers have insufficient oral health training, and there are unfavorable beliefs about the oral health care of the institutionalized elderly. It is necessary to design oral health educational interventions to allow this group of professionals to improve their oral health care related beliefs.
Key words: oral health beliefs; caregivers; oral care
Objetivo:
analizar las creencias relacionadas al cuidado de la salud oral en cuidadores de adultos mayores institucionalizados de la ciudad de Antofagasta, Chile, 2019.
Material y Métodos:
Estudio cuantitativo, observacional, descriptivo, transversal. Se entrevistó a 49 cuidadores con el cuestionario DCBS-sp, para determinar sus creencias relacionadas al cuidado de la salud oral. Para análisis estadístico se utilizó STATA 14 ®.
Resultados:
El 36,73% tiene capacitación en salud oral y el 97,96%, percibe la necesidad de capacitarse. Cuidadores con capacitación tienen significativamente más puntajes promedio favorables a la salud bucal en las dimensiones locus control interno y autoeficacia.
Conclusiones:
Cuidadores tienen baja capacitación para el cuidado de la salud bucal, existiendo creencias desfavorables al cuidado de la salud bucal de las personas mayores institucionalizados. Es necesario diseñar intervenciones de educación para la salud bucal en este grupo que permitan mejorar las creencias relacionadas al cuidado de la salud oral.
Palabras clave: creencias en salud oral; cuidadores; cuidado bucal
Objetivo:
analisar as crenças relacionadas à atenção à saúde bucal em cuidadores de idosos institucionalizados na cidade de Antofagasta, Chile, 2019.
Materiais e Métodos:
Estudo quantitativo, observacional, descritivo, transversal. 49 cuidadores foram entrevistados com o questionário DCBS-sp para determinar suas crenças relacionadas aos cuidados com a saúde bucal. Para análise estatística, foi utilizado o STATA 14 ®.
Resultados:
36,73% possuem treinamento em saúde bucal e 97,96% percebem a necessidade de treinamento. Cuidadores treinados apresentam escores médios significativamente mais elevados favoráveis à saúde bucal nas dimensões de controle do locus interno e autoeficácia.
Conclusões:
Os cuidadores apresentam baixa formação para os cuidados com a saúde bucal, há crenças desfavoráveis em relação aos cuidados com a saúde bucal de idosos institucionalizados. É necessário desenhar intervenções de educação em saúde bucal nesse grupo para melhorar as crenças relacionadas aos cuidados com a saúde bucal.
Palavras-chave: crenças em saúde bucal; cuidadores; cuidados bucais
Introduction and background
According to the literature, the institutionalized elderly are older adults in a state of frailty or dependence, whose ability to maintain their oral health is reduced because of cognitive impairment, loss of functionality, and/or loss of autonomy.1 Therefore, they require support or help from another person to perform basic daily activities such as brushing their teeth, a practice the caregiver is partially or totally responsible for.2 This impacts the oral health of institutionalized people, and there is evidence that oral health deterioration is significantly higher in institutionalized and dependent elderly people than in their autonomous peers.3
The role of formal caregivers in the oral care of the institutionalized elderly is essential to maintain their oral health. However, barriers have been reported in oral hygiene procedures, for example, as older adults may not want another person to perform oral hygiene or do not follow the instructions given by caregivers, among other things.4 Additionally, some of the barriers caregivers face when performing oral hygiene tasks for a third party depend on the value they place on their oral health and that of the people under their care.5
This shows the need to implement oral health education programs focused on caregivers and addressing the existing barriers to oral care. In fact, these interventions for caregivers have proven to be effective as they improve oral hygiene indicators in the elderly under their care.1,2 Therefore, the relevant community or group should be diagnosed when designing oral health education programs to identify their needs and understand the experience of those who will benefit from the program.6
Evidence on this subject in Chile is scarce: it is mainly available from the center and south of the country, there being no studies in the north of the country. However, the published studies are consistent with international findings, reporting a high prevalence of oral diseases in dependent older adults living at home, poor denture conditions, and poor oral hygiene and oral health.7-9 A study on dependent home caregivers showed that the more dependent an older adult is, the more critical the caregiver's role in the home patient's oral hygiene, as the older person is unable to perform oral hygiene activities on their own. This study also detected a low frequency of oral care training, where 73.3% of caregivers had not been trained.4 This has also been observed in caregivers of institutionalized elderly patients: over 70% have not been trained to perform daily oral hygiene,10,11 and 92% of the institutionalized elderly need help with their oral hygiene.11 Therefore, the challenge of this research project was to analyze the oral health care beliefs of caregivers of the institutionalized elderly in Antofagasta, in northern Chile. This evidence will be helpful to design and implement interventions to support and train these caregivers.
Materials and methods
The Ethics Committee of Universidad Pedro de Valdivia and the technical directors of the long-stay facilities of the city of Antofagasta in the second region of Chile authorized this study. A quantitative, observational, descriptive, and cross-sectional study was conducted. The target population was caregivers of elderly people working at long-stay facilities in Antofagasta in 2019. The entire population of caregivers was considered, excluding those who refused to participate in the study or who had been working as caregivers for less than two months. Of the total number of caregivers, all of them agreed to participate, and only one was excluded because he had been working for two days at the time. This resulted in a sample of 49 subjects who agreed to participate and signed an informed consent.
A single researcher interviewed the participants to collect their information: age, sex, educational level, how long they had cared for the elderly, whether or not they had oral care training, and their self-perceived need for training to perform oral care for an elderly person. In addition, the researcher asked the questions included in the DCBS-sp questionnaire, translated and validated in Chile by Garrido-Urrutia et al.12 This questionnaire seeks to determine the oral health beliefs of people who must perform oral care for others. The questionnaire includes 28 randomly ordered questions and 4 dimensions, each including 7 questions. The answers include a 5-point scale, where 1 represents positive beliefs and 5, negative beliefs.12 The multiple dimensions of this instrument make it possible to distinguish various psychological variables that influence health behaviors. The internal locus of control dimension refers to beliefs that an outcome depends on one's abilities, behaviors, or responsibilities; the external locus of control dimension refers to beliefs that an outcome depends on external factors that the individual cannot control; the self-efficacy dimension is the individual's self-perception of ability; and finally, the oral health beliefs dimension refers to beliefs around oral health.13
The data collected was analyzed with STATA 14® statistical software. A descriptive analysis of the variables studied was performed, summarizing them through percentages, average values, and standard deviation (SD). The Student's t-test was used, with a 95% confidence level and a p<0.05., to analyze the difference in means by dimension between caregivers who reported oral health training and those who did not.
Results
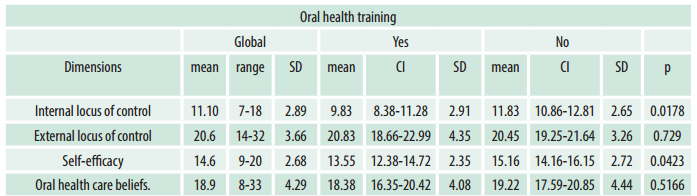
Table 1 shows the following sociodemographic characteristics: age, educational level, length of time as a caregiver, oral health training, and self-perceived need for training to perform oral care for an elderly patient. All the formal caregivers who participated in the study were women. Most caregivers felt the need for training to perform oral care for an older adult, as only one caregiver said she did not feel that need. Only 18 caregivers (36.73%) had received oral health training.
Table 1: Sociodemographic characteristics of caregivers at long-stay facilities in Antofagasta, Chile, 2019 (n=49)
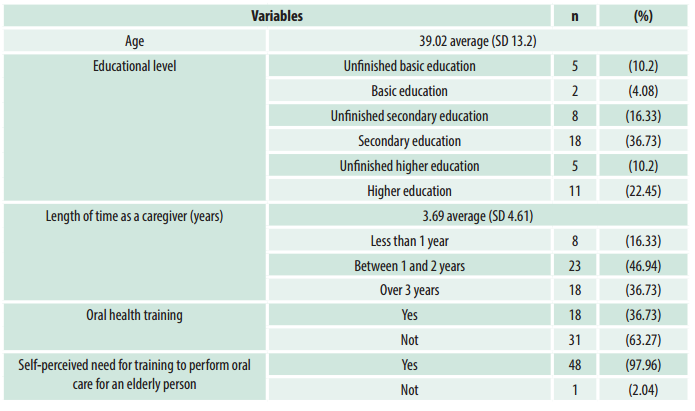
Table 2 shows the response percentages and average score per question of the questionnaire on oral health beliefs in caregivers (DCBS-sp).
Finally, Table 3 shows the average score per dimension of the DCBS-sp questionnaire and if the caregiver had received oral health training. Trained caregivers had significantly lower average values, i.e., favorable to oral health, in the internal locus of control and self-efficacy dimensions (p < 0.05).
Table 2: Percentage of responses and average score per question in the DCBS-sp questionnaire (n=49)
| Questions | Dimension | Strongly agree (%) | Agree (%) | Don't know (%) | Disagree (%) | Strongly disagree (%) | Average score (SD) |
|---|---|---|---|---|---|---|---|
| 1. I believe that the patients themselves report when oral health care assistance is needed. | OHCB | 40.82 | 14.29 | 6.12 | 26.53 | 12.24 | 3.44 (1.54) |
| 2. If I brush and floss their teeth correctly, I expect fewer dental problems. | SE | 55.1 | 24.49 | 10.2 | 8.16 | 2.04 | 1.77 (1.06) |
| 3. I believe that I know how different oral mucosal disorders can be treated. | SE | 4.08 | 8.16 | 71.43 | 14.29 | 2.04 | 3.02 (0.69) |
| 4. I believe that fluoride products are most suitable for children. | OHCB | 20.41 | 20.41 | 36.73 | 14.29 | 8.16 | 3.3 (1.19) |
| 5. I believe teeth should last a lifetime. | IL | 48.98 | 30.61 | 4.08 | 8.16 | 8.16 | 1.95 (1.27) |
| 6. Only the dentist can prevent cavities and gum disease. | EL | 14.29 | 18.37 | 4.08 | 48.98 | 14.29 | 2.69 (1.32) |
| 7. I believe cavities can be prevented. | IL | 71.43 | 22.45 | 6.12 | 0 | 0 | 1.34 (0.59) |
| 8. If I had been given oral health care training, I would be able to provide better oral health care. | SE | 81.63 | 18.37 | 0 | 0 | 0 | 1.18 (0.39) |
| 9. If both parents have had bad teeth, brushing and flossing will not help. | EL | 8.16 | 12.24 | 14.29 | 38.78 | 26.53 | 2.36 (1.23) |
| 10. I believe that prostheses don't have to be removed. | EL | 4.08 | 2.04 | 12.24 | 51.02 | 30.61 | 1.97 (0.94) |
| 11. I believe I know how to floss correctly. | SE | 22.45 | 28.57 | 46.94 | 2.04 | 0 | 2.28 (0.84) |
| 12. It is not possible to prevent sickness and medicines from destroying teeth. | EL | 20.41 | 16.33 | 24.49 | 38.78 | 0 | 3.18 (1.16) |
| 13. I believe flossing teeth can help prevent gum disease. | IL | 34.69 | 36.73 | 20.41 | 8.16 | 0 | 2.02 (0.94) |
| 14. Once gum disease has started, it is almost impossible to stop it. | OHCB | 2.04 | 20.41 | 26.53 | 36.73 | 14.29 | 2.59 (1.03) |
| 15. I believe I know how to prevent oral candidiasis. | SE | 20.41 | 16.33 | 57.14 | 6.12 | 0 | 2.48 (0.89) |
| 16. If the gums bleed when you floss, this usually means that you should stop flossing. | OHCB | 14.29 | 34.69 | 18.37 | 24.49 | 8.16 | 3.22 (1.21) |
| 17. I believe tooth loss is a normal part of growing old. | EL | 28.57 | 40.82 | 10.2 | 12.24 | 8.16 | 3.69 (1.24) |
| 18. Even if you take good care of your teeth, they are only going to fall out as you get older. | EL | 22.45 | 28.57 | 6.12 | 38.78 | 4.08 | 3.26 (1.30) |
| 19. I believe that our patients want me to offer help with oral care. | IL | 67.35 | 30.61 | 0 | 2.04 | 0 | 1.36 (0.60) |
| 20. I believe visiting the dentist is only necessary when experiencing pain. | OHCB | 2.04 | 0 | 2.04 | 36.73 | 59.18 | 1.48 (0.73) |
| 21. If I knew the facts about dental disease, I would be able to practice better oral care. | SE | 69.39 | 28.57 | 2.04 | 0 | 0 | 1.32 (0.51) |
| 22. I believe dentures are less trouble than taking care of natural teeth. | OHCB | 12.24 | 22.45 | 20.41 | 28.57 | 16.33 | 2.85 (1.29) |
| 23. I believe I can successfully remove the majority of plaque to help prevent cavities and gum disease. | SE | 20.41 | 26.53 | 36.73 | 16.33 | 0 | 2.48 (1.0) |
| 24. I believe that one method of brushing is just as effective as any other. | EL | 26.53 | 22.45 | 22.45 | 22.45 | 6.12 | 3.40 (1.27) |
| 25. I believe gum diseases can be prevented. | IL | 53.06 | 34.69 | 8.16 | 4.08 | 0 | 1.63 (0.80) |
| 26. If the gums bleed when you brush, this usually means that you should stop brushing. | OHCB | 10.2 | 6.12 | 4.08 | 32.65 | 46.94 | 2 (1.3) |
| 27. I believe that our patients eat better if they have a healthy, clean mouth. | IL | 75.51 | 16.33 | 6.12 | 2.04 | 0 | 1.34 (0.69) |
| 28. I believe brushing can prevent cavities. | IL | 69.39 | 24.49 | 2.04 | 2.04 | 2.04 | 1.42 (0.81) |
IL: Internal locus of control; EL: External locus of control; SE: Self-efficacy; OHCB: Oral health care beliefs.
Discussion
This study aimed to analyze oral health care related beliefs among caregivers of the institutionalized elderly in Antofagasta, Chile, in 2019. One of the strengths of this research is the sample obtained since all the caregivers of the long-stay facilities in Antofagasta agreed to participate and only one was excluded because he had been working for less than two months. This makes the results highly representative.
All the participating caregivers were women. This coincides with the literature, which associates the caregiving role with women as explained by cultural patterns that lead to the feminization of caregiving. This was also observed by Godoy et al.,11 Garrido-Urrutia et al.,4-14 Fuentes et al.,10 and Cornejo-Ovalle et al.5) among caregivers of the elderly. The average age of the caregivers was 39, a figure similar to that found in Chile by Godoy J et al.11 and Garrido-Urrutia et al.14 among caregivers of institutionalized older adults in long-stay facilities in Valparaíso and a residential care home in Santiago. However, this age was lower than that found by Fuentes et al.,10 who evaluated caregivers of disabled patients and institutionalized older adults in the Bío-Bío region, finding an average age of 52.7 years among caregivers. These differences can be attributed to the fact that most participants in the study conducted by Fuentes al.10 were informal caregivers, with a high percentage of spouses acting as caregivers. Regarding educational levels, approximately 86% have a secondary school or higher educational level, and almost 33% of them have attended higher education—either complete or incomplete—which may also be related to the fact that our sample was made up entirely of formal caregivers, who by definition should be trained to fulfill this role and for which they are paid.
Regarding how long they had been caregivers, 46.94% had worked for one to two years, and 36.73% for three or more years. However, only 36.73% reported oral health training, a result somewhat higher than that reported by Godoy et al.11 and Fuentes et al.,10 where only 24% and 25% of the formal caregivers underwent oral care training. However, this remains a low level of training. The analysis of the self-perceived need for training showed that practically all the caregivers in this study felt the need for training in oral care for the elderly. This is relevant because it indicates that an oral health education intervention would be welcome by this group.
Regarding the analysis of oral health care beliefs, there was a high percentage of "don't know" answers in the self-efficacy dimension. These are related to the belief of knowing how to treat oral mucosa diseases (71.43%), how to use dental floss correctly (46.94%), and how to avoid oral candidiasis (57.14%), and to the belief of being able to correctly eliminate bacterial plaque to prevent caries and gum disease (36.73%). The self-efficacy dimension is essential to identify circumstances that caregivers may feel unable to cope or deal with.15
Additionally, unfavorable oral health beliefs appeared in the oral health beliefs and external locus of control dimensions. In the oral health beliefs dimension, most caregivers believe that the patients themselves should say when they need help with their oral health care (55.11%). They think that fluoride only benefits children (40.82% have negative beliefs and 36.73% do not know). They also think that if gums bleed when flossing, it usually means that they should stop flossing (48.98%).
Regarding the external locus of control, most believe that diseases and medications cannot be prevented from destroying teeth (36.74% have unfavorable beliefs and 24.49% do not know), that losing teeth is part of normal aging (69.39%), that if they take good care of their teeth, they will still fall out as they get older (51.02%), and that one method of brushing is as effective as any other (48.98% have unfavorable beliefs and 22.45% do not know). The external locus of control occurs when the individual perceives or believes that others control their health decisions and health status. It has been shown that locus of control can predict health behaviors and that health education interventions are more successful when participants have internal locus of control.13
Finally, trained caregivers have significantly lower averages, i.e., favorable to oral health, in the internal locus of control and self-efficacy dimensions (p < 0.05). This might indicate that an oral health educational intervention that targets the unfavorable or erroneous beliefs described by this group of caregivers could improve and benefit the oral health of the elderly under their care. In fact, a systematic literature review on the effect of oral health education programs in caregivers of the elderly1 showed that these programs significantly improved oral health parameters in institutionalized elderly people and their oral hygiene. In addition, they proved that oral health education and its connection with other pathologies can improve caregivers' attitudes towards the importance of oral health in institutionalized people. Furthermore, interventions including several health education sessions proved much more effective in increasing knowledge and practical oral hygiene procedures.
This shows that the educational intervention to be implemented in this group must focus on the aspects analyzed through their beliefs. It should have a theoretical and practical-participatory component seeking to increase caregivers' self-efficacy since this is associated with a higher probability of favorable health behaviors.15 The unfavorable results or beliefs were found mostly in the external locus of control and oral health beliefs dimensions. Accordingly, health education interventions should include techniques that help people with a strong external locus of control to become more oriented towards an internal locus of control, and also to consider that health education must be a driver of change for health promoting changes to occur.13
In this sense, the analysis shown in this study is relevant since the oral health beliefs of this group from Antofagasta had never been evaluated. Therefore, the results of our study contribute evidence to help understand the ideas of caregivers of the elderly in the long-stay facilities in Antofagasta that can help plan educational interventions to support their role.
Conclusions
Caregivers of the institutionalized elderly in Antofagasta, northern Chile, have little training in oral health care and unfavorable oral health care beliefs regarding institutionalized older adults. It is necessary to design oral health educational interventions to allow this group of professionals to improve their oral health care beliefs.
Acknowledgments
The authors would like to thank Dr. Casandra Bracamonte Wolf, Director of the Dentistry Department of Universidad Pedro de Valdivia, Antofagasta campus in 2019, for her work with the long-stay facilities of Antofagasta, and each of their technical directors for agreeing to participate in this study.
REFERENCES
1. Wang TF, Huang CM, Chou C, Yu S. Effect of Oral Health Education Programs for Caregivers on Oral Hygiene of the Elderly: A Systemic Review and Meta-Analysis. Int J Nurs Stud. 2015; 52(6):1090-6. [ Links ]
2. Weening-Verbree L, Huisman-de Waal G, van Dusseldorp L, van Achterberg T, Schoonhoven L. Oral Health Care in Older People in Long Term Care Facilities: A Systematic Review of Implementation Strategies. Int J Nurs Stud. 2013; 50(4):569-82. [ Links ]
3. Baumgartner W, Schimmel M, Müller F. Oral health and dental care of elderly adults dependent on care. Swiss Dent J. 2015;125(4):417-26. [ Links ]
4. Garrido-Urrutia C, Romo-Ormazábal F, Araya D, Muñoz-López D, Espinoza I. Cuidado bucal en mayores dependientes de un programa de cuidados domiciliarios. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2016; 9(2):140-145. [ Links ]
5. Cornejo-Ovalle M, Costa-de-Lima K, Péres G, Borrell C, Casals-Peidro E. Oral Health Care Activities Performed by Caregivers for Institutionalized Elderly in Barcelona-Spain. Med Oral Patol Oral Cir Bucal. 2013;18(4):e641-9. [ Links ]
6. Riquelme-Pérez M. Metodología de educación para la salud. Rev Pediatr Aten Primaria. 2012; (21):77-82. [ Links ]
7. Muñoz AD, Flores P, Cueto A, Barraza A. Salud bucodental de postrados severos. Int J Odontostomat. 2012;6:181-7. [ Links ]
8. Quinteros ME, Nunez Franz L. Salud oral en adultos mayores postrados. Int J Odontostomat. 2014;8:337-43. [ Links ]
9. Araya C, Oliva P, Canete E, Zapata H. Salud oral en pacientes adultos mayores del programa postrados. CESFAM Los Volcanes, Chillán. Ciencia Ahora. 2009;23:70-9. [ Links ]
10. Fuentes PC, Escobar IC, Muñoz MP, Ottone NE. Creencias en Salud Oral de Cuidadores de Pacientes Discapacitados y Adultos Mayores Institucionalizados de la Comuna de Quilaco, Región del BioBío. Int. J. Odontostomat. 2015; 9( 2 ): 301-306. [ Links ]
11. Godoy J, Rey P. Conocimiento en higiene oral de cuidadores establecimientos geriátricos de larga estadía, Valparaíso. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2019;12(1):12-14. [ Links ]
12. Garrido-Urrutia C, Espinoza-Santander I, Romo-Ormazabal F. Traducción al español y validación del cuestionario de creencias en salud bucal para cuidadores (DCBS-SP). Rev Esp Salud Publica. 2010; 84(4):409-16. [ Links ]
13. Misrachi C, Sassenfield A, Abarca G, Rojas G. Fundamentos psicosociales de las conductas en salud oral. Rev Dent Chile. 2006; 07(3): 30-34. [ Links ]
14. Garrido-Urrutia C, Romo-Ormazabal F. Espinoza-Santander I, Medics-Salvo D. Oral Health Practices and Beliefs Among Caregivers of the Dependent Elderly. Gerodontology,. 2012; 29(2):e742-7 [ Links ]
15. Kakudate N, Morita M, Fukuhara S, Sugai M, Nagayama M, Kawanami M & Chiba I. Application of self-efficacy theory in dental clinical practice. Oral Dis. 2010; 16(8):747-52. [ Links ]
Authorship contribution 1. Conception and design of study 2. Acquisition of data 3. Data analysis 4. Discussion of results 5. Drafting of the manuscript 6. Approval of the final version of the manuscript JG has contributed in: 1, 2, 4, 5, and 6 ER has contributed in: 1, 4, 6. CG-U: 1, 3, 4, 5, and 6
Conflict of interest: The authors declare they have no conflict of interest regarding the authorship and/or publication of this paper.
Approval note issued by the Ethics Committee: Study approved by the Ethics Committee of Universidad Pedro de Valdivia.
Received: July 11, 2021; Accepted: August 24, 2021











 texto en
texto en