Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.23 no.37 Montevideo 2021 Epub 30-Abr-2021
https://doi.org/10.22592/ode2021n37a10
Case report
Recurrent oral pyogenic granuloma with alveolar bone loss and tooth mobility: report of an unusual case
1Facultad de Estomatología, Universidad Peruana Cayetano Heredia, Perú. sandro.levano.l@gmail.com
2Departamento Académico de Medicina y Cirugía Bucomaxilofacial, Facultad de Estomatología, Universidad Peruana Cayetano Heredia, Perú
Oral pyogenic granuloma is a benign multifactorial lesion that appears as a highly vascular gingival enlargement. It can be located anywhere in the oral cavity, most often in the vestibular marginal gingiva. It occurs most frequently in adult women and male children. It does not usually compromise bone tissue or teeth; its safest treatment is surgical excision, with a high recurrence risk. This study aims to report the case of a 9-year-old female patient who underwent oral pyogenic granuloma excision in the maxilla. The following year, she presented a possible lesion recurrence with alveolar bone loss and the mobility of an adjacent tooth. A biopsy and thorough curettage were performed, confirming the diagnosis of oral pyogenic granuloma.
Keywords: pyogenic granuloma; giant-cell granuloma; diagnosis
El granuloma piógeno oral es una lesión benigna multifactorial, caracterizada por presentarse como un agrandamiento gingival muy vascularizado. Se puede localizar en cualquier área de la cavidad oral, con más frecuencia en la encía marginal vestibular. Se presenta con mayor incidencia en mujeres adultas y en niños varones. No suele comprometer tejido óseo ni dientes y su tratamiento más seguro es la exéresis quirúrgica, siendo el riesgo de recurrencia alto. El objetivo del presente estudio es reportar el caso de una paciente de 9 años de edad, que fue sometida a la exéresis de un granuloma piogénico oral en el hueso maxilar y al año siguiente presentó una recurrencia de la lesión con pérdida ósea alveolar y movilidad de un diente adyacente. Se le realizó una biopsia y un curetaje minucioso, confirmándose el diagnostico de granuloma piogénico oral.
Palabras clave: granuloma piogénico; granuloma de células gigantes; diagnóstico
O granuloma piogênico oral é uma lesão multifatorial benigna, caracterizada por apresentarse como um aumento gengival altamente vascularizado. Pode estar localizado em qualquer área da cavidade oral, mais frequentemente na gengiva marginal vestibular. Ocorre com maior incidência em mulheres adultas e em crianças do sexo masculino. Geralmente não compromete o tecido ósseo ou os dentes e seu tratamento mais seguro é a escisão cirúrgica, sendo alto o risco de recorrência. O objetivo do presente estudo é relatar o caso de uma paciente de 9 anos de idade, submetida a escisão de granuloma piogênico oral no maxilar e no ano seguinte apresentou uma recorrência da lesão com perda óssea alveolar e a mobilidade de umo de seus dentes adjacentes. Uma biópsia e uma curetagem completa foram realizadas, confirmando o diagnóstico de granuloma piogênico oral.
Palavras-chave: granuloma piogênico; granuloma de células gigantes; diagnóstico
Introduction
Pyogenic granuloma is a benign neoplastic vascular proliferation that occurs on the skin and in the oral cavity. It is wrongly called pyogenic because it is not an infectious process and does not produce purulent drainage. It has also been called a benign pedunculated granuloma, lobular capillary hemangioma, vascular epulis, or gravid granuloma and pregnancy tumor when it occurs in pregnant patients(1-3.
Background
Pyogenic granuloma can grow anywhere in the head and neck, torso, and limbs. When it occurs in the oral cavity, it is called oral pyogenic granuloma (OPG). The gingival area is the main site of onset, but it can also occur in the oral mucosa, cheeks, palate, lips, and, less frequently, the tongue(4-6. Its etiology is still unknown, but it is believed to be associated with chronic trauma, local irritants, tartar irritation due to poor oral hygiene, medications such as cyclosporine, and hormonal changes7-8.
Clinically it is usually a reddish lesion, which can show ulcerations and bleed easily, with a soft and lobular surface, and a pedunculated base9. It is usually a small lesion (<2 cm) and does not alter the alveolar bone(10. It has no age or sex predilection but appears more frequently in the second decade of life and in women(11-13. Histologically, it can be classified as lobular and non-lobular capillary hemangioma. However, the lobular type has an endothelial lining and a layer of smooth muscle that is characteristic of venules and not of capillaries. Therefore, the best name would be lobular hemangioma (14.
Its characteristics lead to a diversity of differential diagnoses such as peripheral odontogenic fibroma, hemangioma, inflammatory gingival hyperplasia, peripheral giant-cell granuloma, non-Hodgkin’s lymphoma, angiosarcoma, peripheral ossifying fibroma, Kaposi sarcoma3,5.
The treatment of choice is surgical excision; some authors report no recurrence with this method(15-16. However, recurrence is between 5.8% and 16%(1,17. Conversely, follow-up studies after one year have shown no lesion recurrence when a modified excision with deep curettage is performed(18.
This study aims to report the case of a 9-year-old female patient who underwent oral pyogenic granuloma excision in the maxilla. The following year, she presented a possible lesion recurrence with alveolar bone loss and the mobility of an adjacent tooth. An excisional biopsy was taken, and thorough curettage was performed, confirming the diagnosis of oral pyogenic granuloma.
Clinical case
A 9-year-old female patient with no systemic history sought care at the Oral and Maxillofacial Surgery Service of the Teaching Dental Center of Universidad Peruana Cayetano Heredia for an apparent lesion recurrence at the posterior maxilla. The patient reported seeking care a year before and undergoing an excisional biopsy. The pathology report described a pyogenic granuloma. Clinical check-ups were carried out until she was discharged.
The intraoral clinical examination showed a tumor-like lesion that was painful to palpation and chewing at the marginal and alveolar gingiva level of teeth 1.4 and 1.5 (Fig. 1), approximately 3x3x3 cm in diameter, covering the buccal and palatal areas, and part of the clinical crown. Its consistency was firm, lobular, and pedunculated. It had a rough and bleeding texture when stimulated, with grade II mobility in tooth 1.4 (Fig. 2). The radiographic examination showed the alveolar crest’s effacement between teeth 1.5 and 1.4, with mesioangular and widened periodontal space 1.4 (Fig. 3). The presumptive diagnosis was pyogenic granuloma or peripheral giant-cell granuloma based on the evolution and clinical characteristics.
A rotation flap, excisional biopsy, and thorough curettage of healthy tissue were performed by removing 2 to 3 mm of the adjacent periosteum, and then the wound was sutured.
Clinical check-ups were performed after seven days (Fig. 4) and then after a week. The surgical wound had no dehiscence or secretions; it underwent a good healing process with stable sutures. The pathology report described a pyogenic granuloma, which confirmed its recurrence.
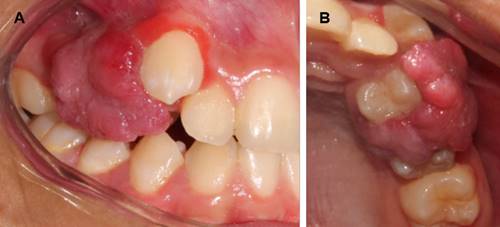
Figure 2: A: Front view of the lesion covering the buccal faces of teeth 1.4 and 1.5. B: Occlusal view of the lesion covering the palatal faces and part of the clinical crown of teeth 1.4 and 1.5

Figure 3: Periapical radiography of the lesion-affected region showing clear horizontal alveolar bone loss between teeth 1.4 and 1.5. In addition, the mesioangular position of tooth 1.4 is clear
Discussion
The diameter of the recurrent OPG (3 cm) was greater than that published in the literature. However, Rebolledo et al.(19 report that it can measure up to 4.5 cm in diameter.
Depending on the age, the oral pyogenic granuloma is more common in adult women than in men. However, OPG develops in boys more frequently than in girls 20, so this case does not fit the epidemiological age and sex characteristics.
Root resorption caused by oral pyogenic granuloma is a rare condition, which usually occurs in cases with long evolution(21. Extensive alveolar bone loss and tooth mobility are observed in 3% of patients(22). Shenoy et al.23 reported the case of an 8-year-old boy with oral pyogenic granuloma associated with bone resorption. Goodman-Topper et al.(24 also reported a case of oral pyogenic granuloma with alveolar bone loss in a 12-year-old boy. In addition, Ababneb et al.(25 reported the case of a 28-year-old pregnant woman with the same lesion and alveolar bone loss. In this case, we observe alveolar bone loss in a recurrent lesion, a rare feature of OPG. Such resorption is likely to have occurred at the time of recurrence.
Differential diagnosis of OPG includes peripheral odontogenic fibroma, hemangioma, inflammatory gingival hyperplasia, peripheral giant-cell granuloma, non-Hodgkin lymphoma, angiosarcoma, peripheral ossifying fibroma, Kaposi sarcoma, lymphangioma, syphilis, tuberculous ulcer, and traumatic ulcer(3,5,26. In this case, the OPG clinically simulated most of the above pathologies as differential diagnoses. Added to bone loss and tooth mobility, this makes diagnosis a real challenge. Therefore, pathological analysis was essential to reach an accurate diagnosis and treatment.
Recurrence occurs at intervals of 10 months to 1 year (18, which coincides with this case. It is also known that recurrence would be associated with multiple factors, most prominently poor oral hygiene rather than systemic compromise. Our patient had good oral hygiene habits, so that factor was not decisive. However, emphasis was placed on improving oral hygiene also to prevent other oral diseases. Removing 2 mm of normal tissue and deep curettage help prevent lesion recurrence(18. Therefore, we performed thorough curettage by removing 2 to 3 mm of adjacent periosteum.
Conclusions
Oral pyogenic granuloma is a well-known benign lesion. However, when it does not present its most common characteristics, such as average size, evolution, and radiographic features, it becomes a challenge for diagnosis because a malignant lesion must be ruled out.
The safe diagnosis and treatment of oral pyogenic granuloma include excisional biopsy and thorough curettage, eliminating 2 to 3 mm of adjacent periosteum, thus preventing potential recurrence.
Recurrence of oral pyogenic granuloma may result in alveolar bone loss with tooth mobility. Therefore, the clinician should provide the proper treatment early to prevent lesion progression.
REFERENCES
1. Al-Khateeb T, Abhabneh K. Oral pyogenic granuloma in Jordanians: a retrospective analysis of 108 cases. J Oral Maxillofac Surg. 2003; 61:1285-8. [ Links ]
2. García I, Hinojosa A, Aldape B, Valenzuela E. Hemangioma lobular capilar (granuloma piógeno) asociado a la erupción: reporte de dos casos clínicos. Rev Odont Mex. 2004; 8(4):127- 32. [ Links ]
3. Sharma S, Chandra S, Guptya S, Srivastava S. Heterogeneous conceptualization of etiopathogenesis. Oral pyogenic granuloma. Natl J Maxillofac Surg. 2019; 10:3-7. [ Links ]
4. Concepción L, Belmonte R, Acosta M, Torres E, Infante P, Torres D, Gutierrez JL. Manejo del granuloma piógeno gigante. Revista SECIB. 2005; 4: 74-89. [ Links ]
5. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012; 16(1):79. [ Links ]
6. Papageorge MB, Doku HC. An exaggerated response of intraoral pyogenic granuloma during puberty. J Clin Pediatr Dent. 1992;16(3):213-6 [ Links ]
7. Chandrashekar B. Minimally invasive approach to eliminate pyogenic granuloma: A case report. Case Reports in Dentistry. 2012; 26. doi:10.1155/2012/909780 [ Links ]
8. Isola G, Matarese G, Cervino G, Matarese M, Ramaglia L, Cicciù M. Clinical Efficacy and Patient Perceptions of Pyogenic Granuloma Excision Using Diode Laser Versus Conventional Surgical Techniques. J Craniofac Surg. 2018; 29(8):2160-3. [ Links ]
9. Epivatianos A, Antoniades D, Zaraboukas T, Zairi E, Poulopoulos A, Kiziridou A, Iordanidis S. Pyogenic granuloma of the oral cavity: comparative study of its clinicopathological and immunohistochemical features. Pathol Int. 2005; 55: 391-7. [ Links ]
10. Thada SR, Pai KM, Agarwal P. A huge oral pyogenic granuloma with extensive alveolar bone loss and 'sun-ray' appearance mimicking a malignant tumour. BMJ Case Rep. 2014; 3:101-36. [ Links ]
11. Dojcinovic I, Richter M, Lombardi T. Occurrence of a pyogenic granuloma in relation to a dental implant. J Oral Maxillofac Surg. 2010; 68 (8): 1874-6. [ Links ]
12. Silk H, Douglass AB, Douglass JM, Silk L. Oral health during pregnancy. Am Fam Physician. 2008; 77 (8): 1139-44. [ Links ]
13. Saravana GH. Oral pyogenic granuloma: a review of 137 cases. Br J Oral Maxillofac Surg. 2009; 47(4):318-9. [ Links ]
14. Santa Cruz D, Plaza JA, Wick MR, Gru AA. Inflammatory lobular hemangioma (ILH): a vascular proliferation with a prominent lymphoid component. Review of a series of 19 cases. J Cutan Pathol 2020. Doi: 10.1111/cup.13844. [ Links ]
15. Kaya A, Kaya B. Oral pyogenic granuloma. Review of 10 cases. Indian J Med Res Pharm Sci. 2015; 2:44-8. [ Links ]
16. Tiwari S, Neelakanti A, Sathyanarayana S. An innovative and less invasive management of recurrent pyogenic granuloma in the esthetic zone: A case report with 18-month follow-up. J Indian Soc Periodontol. 2017; 21:241-4. [ Links ]
17. Hasanoglu GN, Senguven B, Gultekin SE, Cetiner S. Management of a recurrent pyogenic granuloma of the hard palate with diode laser: A case report. J Lasers Med Sci. 2016; 7:56-61. [ Links ]
18. Al-Noaman AS. Pyogenic granuloma: Clinicopathological and treatment scenario. J Indian Soc Periodontol. 2020; 24:233-6. [ Links ]
19. Rebolledo M, Harris J, Cantillo O, Carbonell Z, Díaz A. Granuloma telangiectásico en cavidad oral. Av. Odontoestomatol. 2010; 26 (5): 249-53. [ Links ]
20. Mohapatra S, Singh K, Singh L, Kumar P. Oral pyogenic granuloma: A review. Journal of Odisha Dental Association. 2014; 3(1): 5-9. [ Links ]
21. Angelopoulos AP. Pyogenic granuloma of the oral cavity: Statistical analysis of its clinical features. J Oral Surg. 1971; 29:840-7. [ Links ]
22. Silverstein L, Burton CH. Jr, Singh B. Oral pyogenic granuloma in pregnancy. Int. J. Gynaecol. Obstet. 1995; 49:331-2. [ Links ]
23. Shenoy SS, Dinkar AD. Pyogenic granuloma associated with bone loss in an eight-year-old child: a case report. J. Indian Soc. Pedod. Prev. Dent. 2006; 24:201-3. [ Links ]
24. Goodman-Topper ED, Bimstein E. Pyogenic granuloma as a cause of bone loss in a twelve-year-old child: report of a case. ASDC J. Dent. Child. 1994; 61:65-7. [ Links ]
25. Ababneb K, Al-Khateeb T. Aggressive pregnancy tumor mimicking a malignant neoplasm: a case report. J. Contemp. Dent. Pract. 2009; 10: E072-8, 2. [ Links ]
26. Singh RK, Kaushal A, Kumar R, Pandey RK. Profusely bleeding oral pyogenic granuloma in a teenage girl. BMJ Case Rep. 2013. Doi:10.1136/bcr-2013-008583. [ Links ]
Declaration of interests: The authors certify that they have no commercial interests that represents a conflict of interests in connection with the manuscript
Authors' contribution note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript. S.A.L.L has contributed in 1, 2, 3, 4, 5, 6 A.Y.P has contribuited in 1, 3, 4, 5, 6
Received: June 30, 2020; Accepted: November 08, 2020











 texto en
texto en 





