Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.22 no.36 Montevideo 2020 Epub 01-Dez-2020
https://doi.org/10.22592/ode2020n36a10
Case Report
Dental care for a pediatric patient with neurofibromatosis type 1: a clinical case report
1Facultad de Odontología, Universidad Federal de Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brasil
2Facultad de Odontología, Universidad Federal de Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brasil
3Facultad de Odontología, Universidad Federal de Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brasil
4Facultad de Odontología, Universidad Federal de Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brasil
This clinical case report presents a 7-year-old girl diagnosed with neurofibromatosis type 1 and treated at the Dental Clinic for Patients with Special Needs of the School of Dentistry of the Federal University of Rio Grande do Sul in Brazil. The physical examination revealed a plexiform neurofibroma involving the right upper eyelid and causing ptosis, vision loss, and facial asymmetry. It also showed café-au-lait spots and freckles on the skin. The oral clinical examination showed atresia of the upper dental arch, active dental caries lesions, generalized microbial biofilm on dental surfaces, and gingival bleeding. All the necessary dental treatments were provided with the appropriate care. Dental surgeons need to have knowledge of neurofibromatosis and be prepared to participate in transdisciplinary health teams.
Keywords: Recklinghausen’s disease of the nervous system; mouth; child
Este relato de caso clínico presenta a una niña de 7 años de edad, con diagnóstico de neurofibromatosis tipo 1, que fue atendida en la clínica de Odontología para Pacientes con Necesidades Especiales de la Facultad de Odontología de la UFRGS. Al examen físico se observó neurofibroma plexiforme que afectaba el párpado superior del ojo derecho, que causaba ptosis, pérdida de visión y asimetría facial. Además, manchas color café con leche y pecas en la piel. Al examen clínico bucal, se observó atresia de la arcada dentaria superior, lesiones de caries dental activas y presencia generalizada de biopelicula microbiana sobre las superfícies dentárias y sangrado gingival. Fueron realizados todos los tratamientos odontológicos necesarios para la paciente, con los cuidados pertinentes. Concluímos que es de extrema importancia que los cirujanos dentistas cuenten con conocimiento sobre la neurofibromatosis y estén preparados para formar parte de equipos transdisciplinarios en salud.
Palabras clave: Enfermedad nerviosa de Recklinghausen; Cavidad bucal; Niño
Este caso clínico apresenta uma menina de 7 anos de idade, com diagnóstico de neurofibromatose tipo 1, que foi levada à clínica de Pacientes com Necessidades Especiais do Hospital de Ensino Odontológico da Faculdade de Odontologia da UFRGS. Ao exame físico, observou-se que ela apresentava neurofibroma plexiforme acometendo a pálpebra superior do olho direito, provocando ptose, perda da visão e assimetria facial. Também apresentava manchas cor de café com leite e efélides na pele. Ao exame clínico da cavidade bucal, observou-se atresia maxilar, lesões de cárie ativas e presença generalizada de biofilme e sangramento gengival. Foram realizados os tratamentos odontológicos necessários para a paciente, com os devidos cuidados. Concluímos que é de extrema importância o conhecimento da NF1 por parte dos odontólogos e trabalhar com equipe transdisciplinar.
Palavras chave: Doença Nervosa de Recklinghausen; Cavidade bucal; Criança
Introduction
Neurofibromatosis (NF) is a genetic disease passed on by parents to children or occurring spontaneously at conception and involving the development of tumors in any part of the nervous system, which can alter the development of other tissues, such as skin and bones. Most tumors are benign but can become cancerous over time and affect hearing, vision, motor skills, language, learning, thinking, the cardiovascular system, among other areas1.
There are two types of neurofibromatosis: Neurofibromatosis type 1 (NF1) or Von Recklinghausen’s disease, with an incidence of 1 in 2,500 - 3,500 births. It involves a genetic mutation on chromosome 17 that causes uncontrolled cell growth. Signs and symptoms include café-au-lait spots, which usually increase in size and number over time; skin fold freckling such as in armpits and the groin; small pigmented iris hamartomas called Lisch nodules; lumps on or under the skin, which may also develop within the body in the form of benign tumors of the nerve sheath called neurofibromas, bone abnormalities, and learning difficulties. Neurofibromatosis type 2 (NF2) is less common, with an incidence of 1 in 40,000 births. It is caused by genetic mutations on chromosome 22 and also causes uncontrolled cell proliferation. Hearing is compromised due to benign tumors developing in the vestibulocochlear nerve, which carries sound and balances information from the inner ear to the brain. These patients may experience gradual hearing loss, ringing in the ears, lack of balance, and headaches. Other nerves might also be compromised, such as the cranial, spinal, optic, and peripheral nerves2.
NF1 usually appears during childhood, from birth, or shortly after that, usually around the age of ten. However, NF2 occurs mostly in late adolescence or early adulthood. In both types, signs and symptoms can vary in severity and quantity among individuals3-4.
Although it is passed on through autosomal dominant inheritance, approximately half of those affected have no family history and show new mutations5-6.
Neurofibromas are malignant in only 2 to 5% of cases. According to Korf and Bebin7, there is an estimated risk that 3 to 15% of patients with NF1 will undergo a sarcomatous transformation, most commonly myeloid disorders, rhabdomyosarcoma, osteosarcoma, and ganglioneurofibroma8.
Neurofibromas can appear anywhere; however, oral lesions are rarer than in other parts of the body. Any area of the oral cavity may be compromised, most frequently the tongue9. According to Cunha Filho et al.10, some patients may have an elongated canal and mandibular foramen, as observed on panoramic radiographs.
Clinically, neurofibromas appear as a painless, soft, and slow-growing nodular mass, which can become a large, non-encapsulated, and infiltrative mass that is true hyperplasia of the nerve endings. Surgical treatment is difficult, as it often invades several areas and tends to relapse11.
Clinical case
Female patient aged seven who was taken to the Dental Clinic for Patients with Special Needs of the School of Dentistry of the Federal University of Rio Grande de Sul (FO-UFRGS) by her grandmother for the child to be treated for dental caries.
In the medical history, the grandmother reported that the girl had a NF1 diagnosis and that she had a younger sister with the disease too. The girl performed her own oral hygiene without adult supervision and had a low cariogenic diet regarding oral health habits.
Regarding NF1 clinical signs, the patient had a plexiform neurofibroma (involvement of several nerve groups) that affected the right upper eyelid and caused ptosis, vision loss, and facial asymmetry (Fig. 1). In addition, she had café-au-lait spots and freckles on her skin. Her cognitive and communication skills were unaffected.
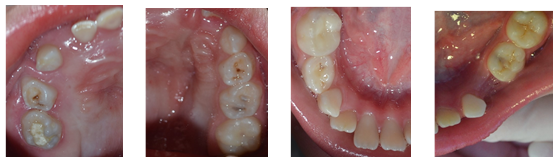
The examination of the oral cavity (Fig. 2, 3, 4, 5, and 6) showed no mucous membrane lesions. It showed atresia of the upper dental arch with right unilateral crossbite and anterior open bite. The examination also showed the widespread presence of microbial biofilm on dental surfaces and gingival bleeding, a root residual in tooth 74, a temporary restoration in poor condition on the occlusal and lingual faces of tooth 85, as well as active microcavitated dental caries lesions on the occlusal face of teeth 26, 65 and 75.
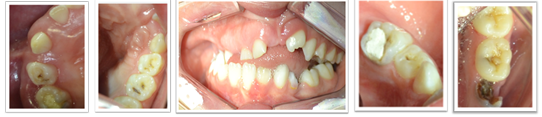
Figs. 2, 3, 4, 5, and 6: Initial clinical aspects; arch and hemiarch of the oral cavity at the beginning of the treatment
The panoramic radiograph (Figure 7) showed a significant alteration in the right mandibular branch in the form of a cluster and elongation of the mandibular canal on the same side. Some delays in tooth eruption requiring treatment were also observed.
The protocol of the FO-UFRGS was followed: a letter was sent to the patient’s pediatrician through her grandmother in order to explain the planned dental treatment and requesting her medical guidance on the use of anesthetic solutions and general clinical management of the patient. The physician responded that care should be taken not to cause any bone fractures.
Five outpatient dental appointments were planned based on the examinations performed and the contact with the medical team. In the first appointment, the root residual was removed under local anesthesia with 2% lidocaine with epinephrine 1:100000. In the second appointment, the clinician started the pulp treatment (mechanical-chemical preparation of root canals and intracanal medication with calcium hydroxide paste) of tooth 85. In the third appointment, the root canals of tooth 85 were filled with calcium hydroxide, zinc oxide, and propylene glycol paste and sealed with self-polymerizing glass ionomer and composite resin, under total isolation and local anesthesia. In the fourth appointment, resin-based sealants were applied to the occlusal faces of teeth 26, 65, and 75 under relative isolation. Oral hygiene and nutrition guidance was provided to the girl and her grandmother. Finally, in the last appointment, oral health guidelines were reinforced. Figures 8, 9, 10, and 11 show the oral cavity after dental treatment.
The patient attended the clinic for the preventive dental check-up three months after the treatment. In this appointment, oral health education and its impact on general health were reinforced. A periapical radiograph was taken to evaluate pulp treatment of tooth 85, which was asymptomatic, with no edema or fistula and no radiographic signs of pulp alteration. Tooth 51 showed exfoliation and fibrous tissue hindering the eruption of tooth 11. As tooth 21 had been in the mouth for over six months, an operculectomy was performed under local anesthesia in the area of tooth 11. A week later, the patient presented healing in the area and eruption of tooth 11.
Guidance was provided on the patient’s orthopedic/orthodontic needs. However, this treatment could not begin at the FO-UFRGS due to the limited availability at the undergraduate and postgraduate orthodontic clinics.
The girl, who had no intellectual disabilities, showed a positive attitude in all the appointments. Professionals responsible for her care and behavior applied the tell-show-do and positive reinforcement techniques. There was no crying or need for physical restraint.
The dental care project for patients with special needs of the School of Dentistry of the Federal University of Rio Grande do Sul (UFRGS) was submitted to the Research Ethics Committee of the institution and that of the UFRGS, under number CEP 1499511, on April 14, 2016.
Discussion
NF1 affects individuals who suffer from it in various ways. However, when it appears on the skin or in the form of facial tumors, it causes the most significant harm. This affects them physiologically and anatomically but mainly psychologically and socially, even considering that this disease does not usually cause cognitive deficits. In the case presented, the patient’s intelligence was unaffected, which significantly contributed to behavior control during dental treatments.
On the other hand, the patient’s grandmother says that the family had sought dental care for the girl for a long time, without any success, since professionals refused to treat her. This made us ask ourselves: Was she rejected because of the complexity of the case or the aesthetic impact of the condition? Was the rejection based on negative impressions?
This situation confirmed that dental care for patients with special needs requires professionals involved in several areas: prior knowledge of pathologies and syndromes, physical structure and technical contribution, availability of consultation time and a trained team, and most of all, personal availability to care for these patients. Perhaps this last point is the most difficult to find among health professionals, particularly dental surgeons.
This case was complicated, mainly in planning and selecting treatments, highlighting the importance of transdisciplinarity and a holistic approach to patient care through constant communication and information exchange among the professionals involved. Thus, the patient’s physician highlighted the possibility of orofacial trauma since one of the main characteristics of NF1 is bone dysplasia and susceptibility to fractures12.
This reinforced the conservative and minimal intervention nature of the treatment plan, which focused on prevention, control of complications, and avoiding exodontics as much as possible, as it could cause significant trauma. Dental treatment should also maintain oral health and improve these patients' quality of life13.
Treatment of patients with systemic involvement, such as our patient, reaches high success rates when there is an individualized treatment plan based on knowing the pathologies’ peculiarities and implementing a transdisciplinary approach. The literature3,5,9,11 emphasizes positive perspectives regarding the importance of dentists in the diagnosis and treatment of oral lesions/manifestations, even if they are unrelated to their main ailment. In this case, we must remember that facial deformities strongly interfere with aesthetics and affect social coexistence; psychological support was necessary, which was discussed with her caregivers. It was gratifying to perceive the positive impact of holistic patient care
Conclusions
Neurofibromatosis type 1 is a rare disease that can cause orofacial manifestations, such as tumors, bone dysplasia, and specific intraoral lesions. Dental treatment for these patients requires a more personalized and transdisciplinary approach, so all the professionals involved can discuss ideas and exchange knowledge.
The patient had aesthetic alterations that could hinder her social interaction; however, she did not have emotional or cognitive issues. This made it easier to control her behavior in the appointment. Treatment was satisfactory for tooth decay, gingivitis, and its consequences. In addition, a regular preventive oral health maintenance program was established, which includes monitoring, detection, and early treatment.
REFERENCES
1. Marocchio, LS. Neurofibroma isolado na região de cabeça e pescoço: considerações clínicas e histopatológicas, 2004. Dissertação de Mestrado Faculdade de Odontologia de Bauru /FOB, Universidade de são Paulo/USP. DOI 10.11606/D.25.2004.tde-12012006-165250 [ Links ]
2. Sua´rez GMV; Go´mez GP. Neurofibromatosis de von Recklinghausen en la nin~ez. Medisan. 2010; 14 (5): 719. [ Links ]
3. Marques AC, Dinis F. Neurofibromatose tipo 1: relato de um caso clínico Rev Port Med Geral Fam. 2013; 29:322. [ Links ]
4. Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis Type I in children. Neurosurg Focusm. 2006; 19 (6): E2. [ Links ]
5. Alves PM; Arau´jo CRF; Pereira JV; Martins FAP; Queiroz LMG. Neurofibromatose tipo 1 com manifestação oral: relato de caso e revisa~o da literatura. J Bras Patol Med Lab. 2008; 44 (2):141-145. [ Links ]
6. Nallanchakrava S, Mallela MK, Jeenepalli VSK, Niharika HM. A Rare Case Report of Neurofibromatosis Type 1 in a 12-year-old Child: A 15-month Follow-Up Oral Maxillo fac Pathol. 2020; 24 (Suppl 1): 106-109. [ Links ]
7. Korf BR; Bebin ME. Neurocutaneous Disorders in Children. Pediatr Rev. 2017; 38 (3): 119-128 [ Links ]
8. Apostolidis C; Anterriotis D; Rapidis AD; Angelo-poulos AP. Solitary intraosseous neurofibroma of the inferior alveolar nerve: report of a case. J Oral Maxillo fac Surg. 2001; 59 (1): 232-235. [ Links ]
9. Martorelli SBF; Andrade FBM; Martorelli FO; Marinho, EVS; Coelho E. Neurofibroma isolado da cavidade oral: Relato de Caso. Rev. Cir. Traumatol. Buco-Maxilo-fac. 2010; 10 (1): 43-48. [ Links ]
10. Cunha Filho JJ; Scortegagna A; Martins F; Schwengber MMB; Robinson WM. Neurofibromatose tipo 1 e suas manifestações bucomaxilofaciais. Revista de Odontologia da UNESP. 2008; 37(3): 283-289. [ Links ]
11. Freitas JM; Mata LL; Ramos RQ; Arau´jo MS. Tumor de células granulares intra-orais: apresentação de dois casos cli´nicos. Rev port estomatol med dent cir maxilofac. 2019; 60 (4): 210-215. [ Links ]
12. Darrigo Jr G, Bonalumi Filho A , D'Alessandro DS, Gelller M. Neurofibromatosis type 1 in childhood: review of clinical aspects. Rev Paul Pediatr. 2008; 26 (2): 176-82. [ Links ]
13. Shang L; Liu ZFJ, Jing FD, Xu HY; Dong K; Zhang X; Wu H; Jing C ; Li L. Case report of ascending colon cancer and multiple jejunal GISTs in a patient with neurofibromatosis type 1 (NF1) BMC. Cancer. 2019; 19 (1196): 2-6. [ Links ]
Authors' contribution note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript. MCF 1, 2, 3, 4, 5, 6 ARVP 4, 5, 6 DBG 4, 5, 6 XCM 4, 5, 6
Received: April 20, 2020; Accepted: September 22, 2020











 texto em
texto em