Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.22 no.36 Montevideo 2020 Epub 01-Dic-2020
https://doi.org/10.22592/ode2020n36a8
Research
Variations in heart rate, body temperature and blood pressure in patients undergoing dental implant surgery
1 Sociedad Científica de Estudiantes de Odontología. Universidad Nacional Mayor de San Marcos. Lima, Perú
2 Facultad de Odontología. Universidad Nacional Mayor de San Marcos. Lima, Perú
Objective:
To determine the variations in heart rate, blood pressure and temperature in patients undergoing dental implant surgery.
Methods:
Series of clinical cases that included 26 patients aged 20 to 60 and treated at the Naval Medical Center “Cirujano Mayor Santiago Távara” (Lima, Peru). The temperature, heart rate, and blood pressure were recorded five minutes before implant surgery, five minutes after local anesthesia, and five minutes after surgery. A digital thermometer and a digital wrist monitor were used to take measurements.
Results:
Body temperature in the preoperative period was 36.9 ± 0.3 °C, while in the intra- and postoperative phase, it was 36.7 ± 0.07 °C (p>0.05). The heart rate increased in the intraoperative period (80.3 ± 8 beats/min) and was restored in the postoperative period (72.5 ± 7.4 beats/min) (p<0.05). The mean arterial pressure in the intraoperative period and on average was 100.14 ± 6.35 mmHg, while in the postoperative phase, it was 93.97 ± 7.57 mmHg (p<0.05).
Conclusion:
The main variations were found from the intraoperative to the postoperative moment in terms of heart rate, mean, systolic, and diastolic blood pressure. Therefore, these are relevant parameters for clinical consideration.
Keywords: blood pressure; heart rate; body temperature; dental implants
Objetivo:
Determinar las variaciones de la frecuencia cardiaca, presión arterial y temperatura en pacientes con cirugía de implantes dentales.
Métodos:
Serie de casos clínicos que incluyó a 26 pacientes de 20 a 60 años de edad atendidos en el Centro Médico Naval “Cirujano Mayor Santiago Távara” (Lima. Perú). Se registró la temperatura, frecuencia cardiaca y presión arterial 5 min antes de la cirugía de implantes, 5 min después de la anestesia local y 5 minutos después de la cirugía. Para realizar las mediciones se utilizó un termómetro digital y un monitor digital de muñeca.
Resultados:
La temperatura corporal durante el preoperatorio fue de 36,9 ± 0,3 °C mientras que en el posoperatorio fue de 36,7°C ± 0,07 (p>0,05). La frecuencia cardiaca aumentó durante el intraoperatorio (80,3 ± 8 lat/min) y se restableció en el posoperatorio (72,5 ± 7,4 lat/min) (p<0,05). La presión arterial media en el intraoperatorio en promedio fue 100,14 ±6,35 mmHg mientras que en el posoperatorio fue 93,97 ± 7,57 mmHg (p<0,05).
Conclusión:
Las principales variaciones se encontraron desde el momento intraoperatorio hasta el posoperatorio en cuanto a la frecuencia cardiaca, presión arterial media, sistólica y diastólica; siendo parámetros relevantes para la consideración clínica.
Palabras clave: Presión arterial; frecuencia cardíaca; temperatura corporal; implantes dentales
Objetivo:
Determine as variações na freqüência cardíaca, pressão arterial e temperatura em pacientes com cirurgia de implante dentário.
Métodos:
Uma série de casos clínicos que incluíram 26 pacientes de 20 a 60 anos de idade atendidos no Centro Médico Naval "Prefeito Cirurgião Santiago Távara" (Lima, Peru). Temperatura, freqüência cardíaca e pressão arterial foram registradas 5 minutos antes da cirurgia do implante, 5 minutos após a anestesia local e 5 minutos após a cirurgia. Para a realização das medidas, foram utilizados termômetro digital e monitor de pulso digital.
Resultados:
A temperatura corporal no período pré-operatório foi de 36,9 ± 0,3 ° C, enquanto no pós-operatório foi de 36,7 ° C ± 0,07 (p> 0,05). A frequência cardíaca aumentou no intraoperatório (80,3 ± 8 batimentos / min) e foi restaurada no pós-operatório (72,5 ± 7,4 batimentos / min) (p <0,05). A pressão arterial média no período intraoperatório foi em média de 100,14 ± 6,35 mmHg, enquanto no pós-operatório foi de 93,97 ± 7,57 mmHg (p <0,05).
Conclusão:
As principais variações foram encontradas no momento intra-operatório para o pós-operatório em termos de frequência cardíaca, média, pressão arterial sistólica e diastólica; sendo parâmetros relevantes para consideração clínica.
Palavras-chave: Pressão arterial; freqüência cardíaca; temperatura corporal; implantes dentários
Introduction
Implant surgery can be supplemented with additional treatments such as exodontics, maxillary sinus floor augmentation, soft tissue grafts, etc. Events such as stress, anxiety, and fear occur while performing these procedures. Therefore, procedures could be associated with an intense cardiovascular response, often harmless in healthy patients but potentially harmful in individuals with heart disease.
The stress-related increased sympathetic activity could trigger an unfavorable cardiac response, as there is a vagal response and alpha beta-adrenergic stimulation. This can cause myocardial ischemia due to elevated cardiac output and possibly cause decreased left ventricular function1. It is essential to know the systemic physiological responses that oral surgical procedures, such as dental implant placement, can trigger. Circulating catecholamines can increase in surgical stress events, leading to higher blood pressure (BP) to a potentially harmful degree2-3.
Physiological responses are the body’s reactions to stressful stimuli. Therefore, a series of physiological reactions activate the autonomic nervous system and the hypothalamic-pituitary-adrenal axis4. Both systems produce substances made in the glands transported through the blood and inhibit, excite, or regulate organ activity (hormones)4. These physiological responses can have a more significant effect on medically compromised patients as those at increased risk of interactions between disease and implant surgery, which entails higher medical risk5.
The right diagnosis and planning for each patient are necessary to ensure that dental implants and treatments only cause manageable and temporary pain or discomfort. It is essential to monitor blood pressure, temperature, and heart rate in dental surgeries. An increase in heart rate is associated with an increased risk of heart disease. Furthermore, excessively high or decreased temperature can cause tissue deterioration, disturb organ function, or alter metabolic rates. In addition, a hypertensive crisis due to increased blood pressure can cause a stroke or an acute myocardial infarction.
Surgical dental implant procedures modify patients’ physiological responses, as they are subjected to stressful stimuli and therefore release hormones. These sustained physiological responses lead to a set of symptoms such as high blood pressure, precordial pain, increased body temperature, stomach disorders (indigestion, diarrhea), insomnia and anxiety, dry mouth and throat, tension, and muscle pain4. These symptoms do not appear frequently during dental implant placement. However, it is essential to consider whether systemic physiological responses are affected during the surgical procedures of implant placement; this would show us if such parameters are affected so professionals can monitor the patient and the surgical event more closely. Therefore, this study assessed whether physiological responses (body temperature, blood pressure, and heart rate) are altered before, during, and after dental implant placement.
Method
An observational and descriptive study (series of clinical cases) with multiple measurements was designed for the same study object (longitudinal type). The population included adult patients treated at the Periodontics Service of the Naval Medical Center “Cirujano Mayor Santiago Távara” (Lima, Peru) from June to December 2018. The sample size was determined through mean estimation and considering a 95% confidence level, a 5% accuracy error, and an expected variance of 13.02, as obtained by Carrasco et al.6, to estimate blood pressure variation. A minimum of 25 patients was required, according to the calculation.
Sample selection was performed through systematic sampling; it had an evaluation constant of K=2. The patient list for dental implant placement was provided by the operating room of the hospital’s Department of Stomatology. Patients had to meet the following criteria: adults aged between 20 and 60, planned placement of a maximum of two dental implants, and good general health (ASA I). Excluded patients: individuals with systemic conditions, a history of surgeries, under pharmacological treatment, totally edentulous, and having undergone oral and facial surgeries.
The same periodontist treated all patients. Lidocaine 1 was used as local anesthesia: 80,000 (Scandicaine®, Austria) with epinephrine (maximum three cartridges; if more was administered, the patient was excluded from the study). Five minutes before entering the operating room, patients were asked to take a seat and lift their tongue to insert the digital thermometer and close their mouth normally, without clenching their teeth or lips. A minute later, after the beep, the thermometer was removed. The temperature was taken with a digital thermometer (Citizen®, Japan), ensuring that the screen displayed no previous measurements. After this, heart rate, and blood pressure were assessed with a digital wrist monitor (Citizen®, Japan) (Fig. 1A). The patient remained seated and placed their elbow on a table. The cuff was placed over the wrist, checking that the monitor was in the right position.
Simple and fenestrated sterile fields were placed, asepsis and antisepsis were performed, and lidocaine was administered with 1:80000 vasoconstrictor (Scandicaine®, Austria). Five minutes later, the temperature was retaken with the digital thermometer and the digital wrist monitor. This was done with the patient lying, as it was more comfortable for both examiner and patient (Fig. 1B). After the dental implant surgery, examiners waited five minutes for the patient to sit up straight in the surgery room. Then, they took the patient’s temperature and blood pressure with the digital thermometer and digital wrist monitor (Fig. 1C).

Figure 1: A Presurgical recording of parameters (preoperative phase). B. Recording five minutes after local anesthesia (intraoperative phase). C. Recording five minutes after surgery has been completed (postoperative phase)
The Student t test for independent groups was used to compare numerical data and group by age, sex, and type of surgical technique (implant placement and implant placement with guided bone regeneration). The ANOVA test and a post-hoc Bonferroni analysis were used to compare evaluation times for related measures. Both tests were conducted after demonstrating the assumptions of normal distribution and homogeneity of means. A statistical significance of 0.05 was set to disprove the null hypothesis. Patients were not obliged to cooperate; each person freely chose to participate in the study by signing an informed consent. The study did not create any differences of any kind (equality). The research did not include names or individual reports. The information analyzed was shown accurately and as it was found. The study was approved by the Ethics Committee of the School of Tropical Medicine of Universidad Nacional Mayor de San Marcos, as well as the Ethics Committee of the Naval Medical Center “Cirujano Mayor Santiago Távara” (Lima, Peru).
Results
Twenty-six patients with a mean age of 51.69 ± 11.06 were evaluated, of which 65.4% were male (mean age 52.65 ± 11.59) and 34.6%, female (mean age 49.89 ± 10.4).
A dental implant was placed on each patient, 92.3% were delayed, and 7.7% were immediate; 73.1% had no additional procedure, and 26.9% had guided bone regeneration procedures.
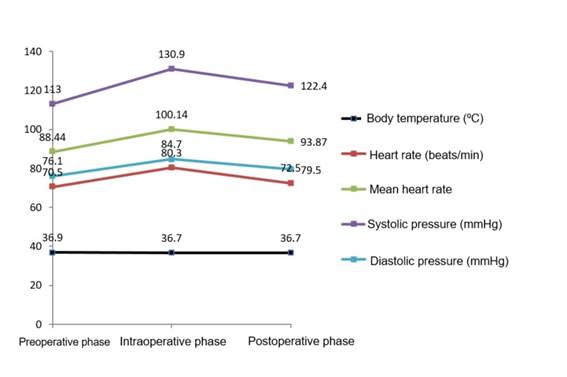
The evaluation of variations in body temperature showed that in the preoperative period, the average temperature was 36.9 °C, while in the intra- and postoperative phase, it was similar: 36.7 °C. Heart rate increased before the procedure (80.3 beats/min) and was restored postsurgically (72.5 beats/min). The average intraoperative blood pressure was 100.14 mmHg on average, while postoperative blood pressure was 93.97 mmHg (Table 1 and Figure 2).
Table 1: Changes in systemic parameters according to assessment times
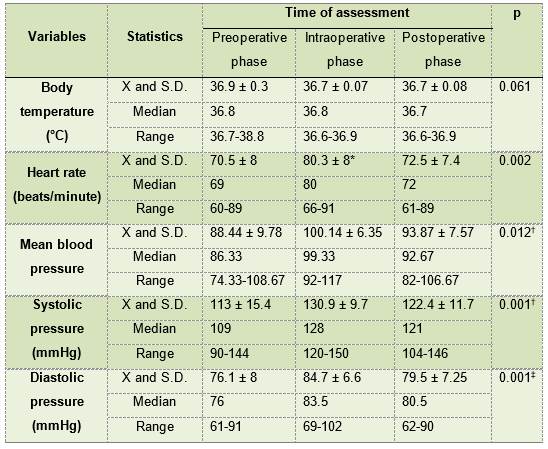
X= Average S.D.= Standard deviation * Friedman test. Significantly different value from the two readings † Friedman test. Significantly different values when comparing the three reading ‡ ANOVA test for repeated measurements. Significantly different values when comparing the three readings
Discussion
Low or high body temperatures can alter metabolic rates, organ function and cause tissue damage7. Hemodynamic changes such as heart rate must be considered in the clinical examination. Extreme tachycardia or bradycardia could have fatal consequences8. An increase or decrease in blood pressure is subject to certain factors and poses a considerable risk to the patient’s health if proper care is not provided during surgery9.
In this paper, we evaluated how these parameters are modified during implant surgery; other studies evaluated partial pressure of oxygen (SpO2)8,10-11, as well as the degree of anxiety12 and the patient’s character13. Implant placement was the dental procedure where temperature, blood pressure, and heart rate were assessed in this and other studies6,12-14. Other authors did so during exodontics1,9-11,15-16, endodontics17, and routine dental treatments (root planing, prophylaxis, operative and impressions)18.
This research studied changes in mean blood pressure and found evidence of a significant increase in subjects from intraoperative time. Although it decreased postoperatively, the reading was not equal to the baseline. Carrasco et al.6 also found a significant increase in mean blood pressure during implant surgery; this may be due to surgical stress that can increase circulating catecholamines (4. However, Masahiro et al.13) found a correlation between neuroticism and increased mean blood pressure in people who received implants, while Weber et al.19) reported that an individual with a high degree of neuroticism tends to choose situations that could lead to adversity and distress and modify their systemic parameters. Richmond et al.20 also found an increase in mean blood pressure in people undergoing routine dental treatments without local anesthesia. This may be because, when a procedure is performed without anesthesia, there is a greater chance of feeling discomfort or pain. These variations increase with age because the elasticity of the artery walls decreases; this increase is more frequent in people over 4018. Nakamura et al.21) mention that the administration of local anesthesia activates the adrenal sympathetic system, so it could lead to higher blood pressure.
When studying changes in systolic and diastolic blood pressure, this paper found that they increase during the surgery (five min after anesthesia is administered) and show a slight decrease postsurgically, which is significantly different in the intraoperative phase. In this regard, Nagao et al.14 found that systolic blood pressure increased significantly, and diastolic blood pressure did not change significantly throughout the surgery compared to the preoperative reading. Tiwari et al.10) found an increase in systolic blood pressure during anesthesia administration and a minimal change in diastolic blood pressure during dental extraction. Nuñez et al.15) found that blood pressure variation most frequently occurred five minutes after administering anesthesia for tooth extractions.
Regarding heart rate, we found a significant increase in pulse rate only in the intraoperative phase, and it returned to its baseline values after surgery. Tiwari et al.10) and Matsumura et al.22) found an increase in heart rate during local anesthesia administration in extractions. Arias et al.8) found that heart rate increased significantly after administering anesthesia and remained stable during flap lifting, decreased again during osteotomy, and remained the same during suture and discharge during extractions. Nagao et al.14) found that it increased just after local anesthesia was administered and decreased in the course of dental implant surgery.
Fuentes et al.5) report that catecholamines produced in surgical stress situations increase blood pressure and heart rate. However, Vintanel et al.11) state that the degree of stress is a variable to consider at the onset of systemic variations (heart rate and diastolic blood pressure). Nagao et al.14) say that increased age, surgical time, and the number of implants are linked to increased variations in systemic parameters (heart rate, systolic, and diastolic blood pressure).
Regarding temperature, there was a significant decrease compared to intraoperative time and it remained constant after surgery, although this was not clinically significant. In this regard, there is a marked decrease in temperature when general and regional anesthesia is used, but not with local anesthesia23. However, Kimberger and Quast7 indicate that patients typically undergo accidental cooling when the surgical procedure begins. External factors such as wearing few clothes or low temperatures in the environment induce the involuntary temperature to decrease. While it is generally true that air conditioning provides surgeons with a pleasant and comfortable environment, it is also an external factor during all dental implant treatments. Air conditioning must have the right technical qualities since many surgical procedures performed in hospitals require an aseptic environment.
The limitation of this study is that partial pressure of oxygen (PpO2) could not be evaluated because measurement materials were not available. Therefore, we recommend considering this critical variable in the different surgical processes as it reflects saturation of hemoglobin and, therefore, oxygen supply to the tissues. Only healthy patients receiving a maximum of two implants were evaluated; it is necessary to conduct studies evaluating patients with systemic diseases-provided bioethical considerations or expert opinions are respected-and requiring more complex dental implant placement procedures. It should be noted that the variable “pain” must also be considered in future studies as it could affect blood pressure values. It is advisable to analyze the patients’ degree of anxiety; we recommend using psychometric scales or tests before placing a dental implant. Additionally, the main antecedents were considered for the sample size. However, this number was small, and data generalization is not applicable, so we recommend a larger sample size for future studies.
Conclusion
There is a non-significant decrease in temperature as of intraoperative time, and it becomes constant until completing the dental implant placement. Heart rate increases from intraoperative time, and although it decreases in the postoperative phase, it does not match the baseline value. Something similar happens when the average blood pressure is evaluated in healthy patients who have had one or two dental implants placed.
REFERENCES
1. Pando P, Expósito F. Exodoncia dental y riesgo cardiovascular. Variabilidad de las constantes hemodinámicas durante la exodoncia dental. Cient Dent. 2008;5(3):175-81. [ Links ]
2. Huang JI, Yu HC, Chang YC. Occurrence of trigeminocardiac reflex during dental implant surgery: An observational prospective study. J Formos Med Assoc. 2017;116(10):742-747. [ Links ]
3. Schimmel M, Srinivasan M, McKenna G, Müller F. Effect of advanced age and/or systemic medical conditions on dental implant survival: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):311-330. [ Links ]
4. Nogareda C. Fisiología del estrés. Consultado el 15 de abril del 2019 (Internet). Available from: Available from: http://www.insht.es/InshtWeb/Contenidos/Documentacion/FichasTecnicas/NTP/Ficheros/301a400/ntp_355.pdf [ Links ]
5. Nobre Mde A, Maló P, Gonçalves Y, Sabas A, Salvado F. Outcome of dental implants in diabetic patients with and without cardiovascular disease: A 5-year post-loading retrospective study. Eur J Oral Implantol. 2016;9(1):87-95. [ Links ]
6. Carrasco R, Cordero E, Goldberg I, Martinez B, Pacheco C. Evaluación de la presión arterial media durante la cirugía de implante dental. Rev Esp Cir Oral Maxilofac. 2014;36(3):95-8. DOI: http://dx.doi.org/10.1016/j.maxilo.2013.02.002. [ Links ]
7. Kimberger O, Quast S. La importancia de la temperatura corporal central. 1ra ed. Alemania. Dräger Medical GmbH; 2016. 9-60 p. [ Links ]
8. Arias B, Romero M, Hita C, Bravo M, Vallecillo M. Seguimiento de la frecuencia cardiaca y la presión parcial de oxígeno durante la cirugía bucal. Av Odontoestomatol. 2003;19(2):1-6. [ Links ]
9. Castillo C, Manotas A, Vargas D. Variabilidad de la presión arterial pre y post-quirúrgica en pacientes sometidos a cirugía oral que asistieron a la clínica odontológica de la Universidad del Magdalena en los meses de abril y mayo periodo 2008. Duazary. 2011;8(1):1-10. [ Links ]
10. Tiwari V, Sridhar M, Teja P, Rama K, Tiwari H. Evaluation of systolic and diastolic blood pressure, pulse rate and spo2 levels pre and post dental extraction under local anesthesia. J Oral Med. 2018;4(2):74-8. [ Links ]
11. Vintanel M. Influencia del anestésico, ansiedad e hipertensión en los cambios hemodinámicos de pacientes sometidos a extracción dental.Tesis de licenciatura. Madrid. Facultad de Odontología, Universidad Complutense de Madrid; 2015. 57p [ Links ]
12. Schwartz D, Bar Y, Ilana E. Efecto del estrés en el procesamiento de la información en el contexto de la cirugía de implante dental. Clin Oral Implants Res. 2006;1:1-8. [ Links ]
13. Masahiro W, Syunta M, Tomoaki M, Tohru S, Kazunori I, Yoshinobu M. Un estudio prospectivo de la relación entre el carácter del paciente y la presión arterial en la cirugía de implantes dentales. Rev Int Implantol. 2016;2(21):1-5. [ Links ]
14. Nagao H, Munakata M, Tachikawa N, Shiota M. Clinical study of risk management for dental implant treatment--changes of blood pressure and pulse rate during implant surgery under local anesthesia (Article in Japanese). Kakubyo Gakkai Zasshi. 2002;69(1):27-33 [ Links ]
15. Núñez M, Tore A, Mico G, Pratt G, Pratt G, Keim M. Variabilidad de la presión arterial en pacientes normotensos sometidos a cirugía bucal ambulatoria. Rev Fac Cienc Salud UDES. 2015;2(2):125-32. [ Links ]
16. Gungormus M, Buyukkurt M. La evaluación de los cambios en la presión arterial y la frecuencia del pulso de los pacientes hipertensos durante la extracción dental. Acta Med Austriaca. 2003;30(5):127-9. [ Links ]
17. Macías A, Oliver P, Luna L, Guerrero A, Cornejo P. Efecto del tratamiento endodóntico en los valores de la presión arterial en pacientes hipertensos. Rev ADM. 2013;70(1):30-4. [ Links ]
18. Aranzazu M, Delgado J, Pieschacón G. Variaciones de riesgo en valores de tensión arterial en pacientes hipertensos durante procedimientos odontológicos. Rev la Univ Ind Santander. 2014;46(2):1-10. [ Links ]
19. Weber M, Schiffrin E, White W, Mann S, Lindholm L, Kenerson J, y cols. Clinical practice guidelines for the management of hypertension in the community. J Clin Hypertens. 2014;16(1):14-26. doi: 10.1097/HJH.0000000000000065. [ Links ]
20. Richmond A, Gortzack D, Johannes O, Abraham I. Respuesta de la presión arterial al tratamiento dental de restauración de rutina con y sin anestesia local: registro continuo no invasivo de la presión arterial con un manómetro para dedos. Cir Oral. 1992;73(6):677-81. [ Links ]
21. Nakamura Y, Matsumura K, Miura K, Kurokawa H, Abe I, Takata Y. Cardiovascular and sympathetic responses to dental surgery with local anesthesia. Hypertens Res. 2001;24(3):209-14. [ Links ]
22. Matsumura K, Miura K, Takata Y, Kurokawa H, Kajiyama M, Abe I, y cols. Changes in Blood Pressure and Heart Rate Variability During Dental Surgery. Am J Hypertens. 1998;1:1376-80. [ Links ]
23. Uriostegui S, Nava L, Mendoza E. Alteraciones de la temperatura y su tratamiento en el perioperatorio. Rev Mex Anestesiol. 2017;40(1):29-37. [ Links ]
Authors' contribution note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript. AQA has contributed in: 1, 3, 5 y 6. LRO has contributed in: 2, 4 y 6. YCR has contributed in: 2, 4, 5 y 6. SGP has contributed in: 2, 4, 5 y 6.
Received: July 22, 2020; Accepted: September 29, 2020











 texto en
texto en