Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.22 no.36 Montevideo 2020 Epub 01-Dic-2020
https://doi.org/10.22592/ode2020n36a3
Investigación
Comparative effect of aerobic physical activity and occlusal stabilization appliances on musculoskeletal orofacial pain in individuals with temporomandibular disorders
1Cátedra de Rehabilitación, prostodoncia fija y trastornos temporomandibulares, Facultad de Oodontología, Universidad de la República, Montevideo, Uruguay
2 Departamento de educación física y salud, Instituto Superior de Educación Física, Universidad de la República, Montevideo, Uruguay
3 Cátedra de Rehabilitación, prostodoncia fija y trastornos temporomandibulares. Facultad de Odontología, Universidad de la República, Montevideo, Uruguay
This study evaluated the efficacy of aerobic physical activity (APA) in managing musculoskeletal orofacial pain in individuals with temporomandibular disorders (TMD) compared to treatment with an occlusal stabilization appliance (OSA). Volunteers with musculoskeletal pain aged between 18 and 40 and with bimaxillary teeth involved. The analog verbal scale was used to evaluate the pain variable. Each treatment group included seven individuals evaluated for eight (APA) and six (OSA) weeks, respectively.
APA showed a significant weekly decrease of 0.155 points in pain measurement. As for the OSA, the trend was even stronger than in the APA treatment-the difference was substantial.
This study demonstrated that both the OSA and APA contributed to reducing musculoskeletal orofacial pain in volunteers suffering from TMD.
Keywords: temporomandibular disorders; musculoskeletal pain; aerobic exercise; occlusal devices
El presente estudio evaluó la eficacia comparativa entre la actividad física aeróbica (AFA) y los dispositivos ortopédicos estabilizadores(DOE) en el manejo del dolor orofacial de origen músculo esqueletal en individuos con trastornos temporomandibulares (TTM).
Participaron voluntarios dentados bimaxilar con dolor de origen músculo esqueletal con edades comprendidas entre 18 y 40 años. Para la evaluación de la variable dolor el instrumento de medición fue la escala verbal análoga. Cada uno de los grupos de tratamientos estuvo compuesto por siete individuos, los cuales fueron evaluados durante ocho (AFA) y seis (DOE) semanas respectivamente.
La AFA se caracterizó por un descenso semanal significativo de 0.155 puntos en la medición del dolor. En tanto con DOE la tendencia fue aún más pronunciada que en el tratamiento con AFA, siendo esta diferencia significativa.
El presente estudio demostró que, tanto la intervención con DOE como con AFA contribuyeron a la disminución del dolor orofacial de origen músculo esqueletal en voluntarios con TTM.
Palabras claves: Trastornos temporomandibulares; dolor muscoloesqueletal; ejercicio aeróbico; dispositivos oclusales
O presente estudo avaliou a eficácia da atividade física aeróbica (AFA) no tratamento da dor orofacial de origem muscular esquelética em indivíduos com disfunção temporomandibular em comparação ao tratamento com dispositivo ortopédico estabilizador (DOE). Participaram voluntários com dor muscular esquelética com idade entre 18 e 40 anos e dentes bimaxilares. Para a avaliação da variável dor, o instrumento de medida foi a escala verbal analógica. Cada um dos grupos de tratamento foi composto por sete indivíduos, avaliados por oito (AFA) e seis (DOE) semanas, respectivamente.
AFA foi caracterizada por uma diminuição semanal significativa de 0,155 pontos na medição da dor. Quanto ao DOE, a tendência foi ainda mais acentuada do que no tratamento com AFA, sendo essa diferença significativa.
O presente estudo demonstrou que a intervenção do DOE e do AFA contribuiu para a redução da dor musculoesquelética orofacial em voluntários com TTM.
Palavras-chave: Distúrbios temporomandibulares; dor musculoesquelética; exercício aeróbico; dispositivos oclusais
Introduction
Temporomandibular disorders (TMD) are a heterogeneous group of pathologies that affect the temporomandibular joints (TMJ), the masticatory muscles, or both1. The glossary of prosthodontic terms describes them as conditions that produce an abnormal, incomplete, or altered function of the TMJ and the masticatory muscles2. Temporomandibular pain is relatively common, affecting approximately 10% of the population over the age of 18. This disorder mainly affects young adults, middle-aged people, and it is nearly twice as common in women as in men3.
TMDs are highly prevalent across the general population. The prevalence of signs in a study conducted in a European population is 34.5%4. Another study carried out in Australia, in a cohort of dental students, showed a prevalence of TMD symptoms of 77.2%5. In Uruguay, 55% of the population has at least one symptom, and 44% of the population has at least one sign6. These studies also show a higher prevalence in women.
It is crucial to identify the main factors leading to TMD to select the most appropriate and effective treatment for each patient. Reversible therapies most commonly used for the pain symptom include therapy with an occlusal stabilization appliance (OSA), pharmacotherapy, physiotherapy, psychotherapy (behavioral strategies), among others. These can be indicated separately or in combination7).
OSAs have proved to be efficient in treating myalgia and arthralgia of the masticatory system8. However, their action mechanism is unclear and still controversial.
Different methodological problems relating to research designs have made it difficult to understand the real effectiveness and action mechanisms of OSAs. For example, among the issues detected in previous studies are a small sample size, inadequate blinding, and short follow-up times9.
Aerobic physical activity (APA) and manual therapy are the therapeutic measures that have proved to be most effective in changing attitudes to pain and stress are 10.
Past studies have shown that APA interventions have positive results for pain reduction in fibromyalgia treatment11-13.
To date, no studies have been conducted to evaluate whether APA is effective in reducing pain in patients with TMD muscle pain.
Beta-endorphin (BE) is a hormone, an endogenous opioid, secreted by the anterior pituitary gland. Among the most relevant effects are analgesia, increased lactate tolerance, and decreased muscle discomfort14. Its bloodstream levels increase during prolonged APA, thus reducing pain. It shows greater resistance to enzymatic degradation compared to enkephalins15.
Valim, quoting other authors, argues that APA influences the serotonergic system, increases sympathetic activity, improves sleep, and promotes psychological well-being11.
This study assessed APA's efficacy in managing musculoskeletal orofacial pain in people with TMD, compared to treatment with an OSA.
Materials and methods
Materials
This was a comparative, prospective, longitudinal, controlled, and randomized clinical study.
The sample was selected among students of the School of Dentistry, Universidad de la República. Uruguay. It included 14 female volunteers. The recruitment method was consecutive, and a public call was made in 2016, seeking volunteers suffering from orofacial pain.
Ethical considerations: The project was approved by the Ethics Committee of the School of Dentistry of Universidad de la República (File 249/15).
Volunteers signed an informed consent before their participation.
Inclusion criteria: volunteers with musculoskeletal orofacial pain due to TMD, aged between 18 and 40 years, with bimaxillary teeth and who presented proof of physical fitness issued by a competent institution.
Exclusion criteria: volunteers with pain resulting from reasons other than musculoskeletal due to TMD, pregnant women who regularly do aerobic physical activity, OSA carriers at the time of the intervention, chronic and/or acute respiratory conditions, severe psychiatric disorders, unstable or untreated heart diseases and with a history of a heart attack in the past six months.
Elimination criteria: those who did not complete at least 80% of the APA sessions, as well as patients who did not meet the OSA indications for use and controls.
Method
A general, regional, and local clinical examination of the patients was undertaken to check the inclusion and exclusion criteria.
Volunteers with musculoskeletal orofacial pain-related TMD were separated from those of other origin, following the DC-TMD criteria16 and the calibration protocol of the Riva et al. study of May 20116. Palpation of masticatory muscles (masseter and temporal) and external pole of the TMJ was performed.
Measuring instruments and variables
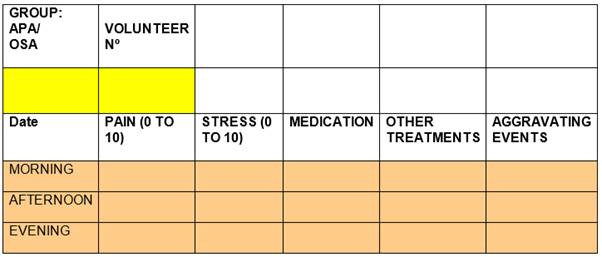
The verbal analog scale (VAS) was used to evaluate the pain and emotional stress variables. For data collection, we used a survey that includes the aforementioned measuring instrument (Fig. 1). The survey was used on several occasions, from the beginning to the end of the interventions, to evaluate the progression of the symptom reported by the patient. Each of the treatment groups consisted of seven people, who were evaluated for eight (APA) and six (OSA) weeks, plus an initial evaluation to determine mean values at baseline. In each assessment, self-reports of pain and stress were recorded at three times of the day: morning, afternoon, and evening. For the initial evaluation, they were provided with a pain journal two weeks before the intervention to determine an average baseline pain. This considers pain symptoms and fluctuations.
Interventions and Groups
The sample was randomly divided into two groups of seven volunteers each:
Group A (GA): people who did APA exclusively and Group B (GB) people who were fitted with an OSA.
The OSAs were made at the School of Dentistry clinic using a printed splint technique and made by a specialist considering ideal occlusion criteria.
The APA was supervised by advanced students and teachers from the Higher Institute of Physical Education (ISEF) of Universidad de la República. The type of APA was 60-minute aerobic fitness sessions. Each session started with a 5 to 10 min warm-up, followed by moderate aerobic exercises, which did not exceed 10 to 30% of the VO² max14; the central part with planned exercises and the final stretch, in which aerobic activity is maintained, at a low to moderate intensity (5 to 10 minutes), with an exercise progression approach17.
Due to the study's limitations, to ensure BE release, we used a heart rate meter (Advanced 3 Müller Pulse Oximeter) and Karvonen's formula; by entering the data, we obtained the oxygen consumption level. To be considered BE release-related, it had to be between 60% and 85%18-19.
Statistical methodology
Pain and stress levels were recorded multiple times (weekly and three times a day). The reduction in both variables (pain and stress) was compared using mixed-effect regression models [1], where inferences were made with a 5% significance level. The statistical software used was R[2].
The evolution of each group was compared using a regression model that compared the trends for each treatment at different times of the day. It should be noted that the control variable for this model was the presence of aggravating factors since this could skew each person's measurements at the different points in the study. This article presents the results of the pain variable.
Results
Pain variable
Descriptive analysis
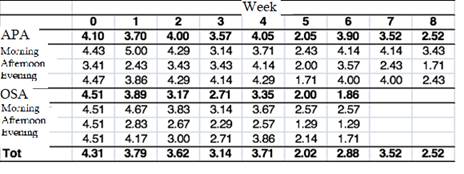
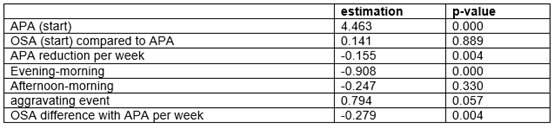
Table 1 shows the average evolution of both treatments. The APA group had a longer follow-up period where a downward trend in pain values seems to be observed (Table 2).
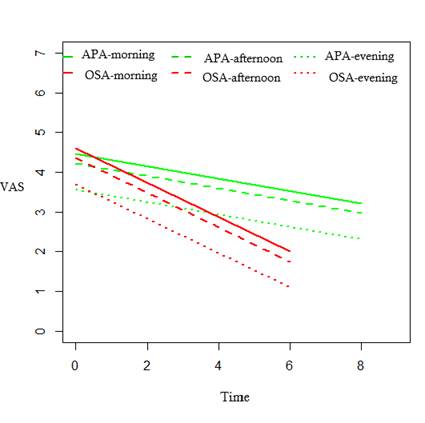
Figure 1 shows the average evolution based on the results of the previously estimated regression model.
The graph shows pain reduction is more significant with an OSA (red lines) than APA interventions (green lines). The three lines, corresponding to each treatment, show the evolution in the three moments of the day. Note that pain values at night are lower than those recorded in the morning and afternoon.
Discussion
The first two lines of Table 2 indicate that the average pain value of the two groups was not significantly different, and the average was 4.463 points. The third line shows the first relevant result, which indicates that APA treatment resulted in a significant weekly reduction of 0.155 points in pain measurement. Building on the above statement, the last row shows that the trend was even more pronounced with OSA treatment than with APA treatment, and the difference is significant. By combining the two estimates, we see that pain reduction among the OSA group was almost half a point (0.434) per week.
In addition, the pain perceived by the participants was less intense (almost one VAS point) at night compared to the morning, and that the aggravating factors recorded were significant, so much so that when faced with these factors, participants' perception of pain was on average 0.794 points higher than usual.
This study found significant differences between the two groups following interventions considering the pain variable. Although APA significantly reduced pain, the trend was higher with OSA, and the difference in reduction between the two groups was significant. The evaluation period of the OSA group was six weeks. This study shows its effectiveness in reducing pain. This result is in line with studies such as that of Dao and Lavigne 1994, which shows pain reduction across a ten-week evaluation period, but without explaining the mechanism for pain reduction8). In a subsequent literature review, Kreiner concluded that with the data available so far, the use of OSA for muscle and joint pain had sufficient scientific support (9. In 2011, a randomized clinical study compared the efficacy of OSA and physical therapy (Tens) for TDM pain management across a four-month period for OSA and a four-week period for physical therapy. The study found a significant difference in pain reduction between the two, and OSA is the most effective20. The latter is in line with other studies on the efficacy of OSA for pain reduction in five-week21) and ten-week periods, respectively22.
Our work is consistent with the studies reviewed, and despite controversy regarding the action mode or mechanism, OSAs do reduce musculoskeletal pain in patients with TMD, and despite varying evaluation times, their effectiveness is recognized.
APA showed a slower reduction than OSA; this could be because volunteers were sedentary and the intensity of the APA was gradually increased as the days of the intervention progressed. APA intensity is required to ensure BE release14. Some studies have shown that BE levels did not vary with low-intensity exercise, with oxygen volumes ranging from 25% to 60%23-25).
Another study of 12 untrained men found that pedaling at 60% oxygen volume did not significantly change BE levels. However, at 70 and 80% intensities, increases were significant, 2 to 5 times the baseline values, respectively26. Years later, the same author didn’t find a gender difference in BE levels at 60% and 80% intensity, respectively27.
One of the most difficult parameters to estimate is the intensity of physical activity. There are different methods for measuring it: measuring heart rate, the person's perception of the activity, and perceived intensity using a standardized classification system28. Oxygen volume was not measured directly in our study; it was done using Karvonen's formula19. The study did not aim to measure BE.
The 2006 review article by Nishishiya assessed the efficacy of APA in fibromyalgia patients. It confirmed that APA is the most studied exercises and concluded that there is moderate evidence that APA helps improve pain in these patients. Likewise, there is no evidence that APA worsens the clinical manifestations of people with fibromyalgia29.
More recently, a review article published in 2017 states that the quality of the evidence to assess physical activity and exercise for chronic pain is low. This is primarily due to small sample sizes and potentially weak studies. Favorable effects were detected in reducing the severity of pain and improving physical function, although these were mainly of low to moderate impact and were not consistent in all reviews30. In this sense, our study would have the same effects as those reported in that article in terms of pain.
Available evidence suggests that physical activity and exercise have few adverse effects and can improve pain intensity, physical function, and the resulting quality of life. However, further research is needed and should focus on increasing the number of participants, including participants with a broader VAS pain level range, and extend both the intervention itself and the follow-up period30.
Conclusions
This study showed that both OSA and APA helped reduce musculoskeletal orofacial pain in TMD volunteers.
The comparative study between these treatments showed that pain reduction was most effective in the OSA group.
Future studies should review and analyze the possibility of implementing other methodological designs for more accurate results: longer evaluation periods, larger samples, more diverse APA interventions.
It would be interesting to work with designs where both groups are fitted with an OSA, and one of the groups also undertakes APA. It would also be interesting to work with three groups: one with OSA, another with APA, and the third one with OSA and APA
Referencias
1. Okeson JP. Tratamiento de la oclusión y afecciones temporomandibulares. 7ª ed. Barcelona: Elsevier, 2013. p102-128. [ Links ]
2. GPT-9 Glossary of Prosthodontics Terms, Edition 9, J Prosthet Dent 2017; Vol.117:1-106 [ Links ]
3. Le Resche L. Epidemiology of Temporomandibular Disorders: Implications for the Investigation of Etiologic Factors. Crit Rev Oral Biol Med. 1997; 8 (3): 291- 305. DOI:10.1177/10454411970080030401 [ Links ]
4. Jussila P, Kiviahde H, Näpänkangas R. Prevalence of Temporomandibular Disorders in the Northern Finland Birth Cohorts 1966. J Oral Facial Pain Headache. 2017; 31: 159-164. doi: 10.11607/ofph.1773 [ Links ]
5. Lung J, Bell L, Heslop M, Cuming S, Ariyawardana A. Prevalence of Temporomandibular disorders among a cohorts of university undergraduates in Australia. J Invest Clin Dent. 2018; 1-5 dos.org/10.1111/jicd.12341. [ Links ]
6. Riva R., Sanguinetti M, Rodriguez A, Guzzetti L, Lorenzo S. Prevalencia de trastornos temporomandibulares y bruxismo en Uruguay Parte 1. Odontoestomatología. 2011; 8 (17): 54-71. [ Links ]
7. Michelotti A, De Wijer A, Steenks M, Farella M. Home-exercise regimes for the management of non-specific temporomandibular disorders. Journal of Oral Rehabilitation. 2005; 32: 779-785. [ Links ]
8. Dao T, Lavigne G, Charbonneau A. The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: a controlled clinical trial. Pain. 1994; 56: 85-94. [ Links ]
9. Kreiner M, Bentancor E, Clark G. Occlusal stabilization appliance. Evidence of their efficacy JADA. 2001; 132: 770-777 [ Links ]
10. Lopez-Rodriguez M, Castro-Sanchez A, Fernandez-Martinez M. Comparacion entre biodanza en medio acuático y stretching en la mejora de la calidad de vida y dolor en los pacientes con fibromialgia. Aten Primaria. 2012; 44(11): 641-650. [ Links ]
11. Valim V, Natour J, Xiao Y. Efeitos do exercício fisico sobre os níveis sericos de serotonina e seu metabolito na fibromialgia: um estudio piloto randomizado. Rev. Bras Reumatol. 2013; 53 (6): 538-541 [ Links ]
12. Sañudo B, Gailano D, Carrasco L, de Hoyo M, McVeigh JG. Efects of a prolonged exercise program on key health outcomes in women with fibromyalgia: A randomized controlled trial. J. Rehabil Med. 2011; 43: 521-526 [ Links ]
13. Fontaine K, Conn L, Clauw D. Effects of Lifestyle Physical Activity in Adults with Fibromyalgia: Results at Follow-up. J Clin Rheumatol. 2011; 17 (2): 64-68. doi: 10.1097/RHU.0b013e31820e7ea7. [ Links ]
14. Cunha G, Ribeiro J, Oliveira A. Níveis de Beta-Endorfina em Resposta ao Exercício e no Sobretreinamento. Arq Boas Endocrinol Metab. 2008; 52 (4): 589-598. [ Links ]
15. Schwarz L, Kinderman W. Cannes in B- Endorphin levels in response to aerobic an anaerobic exercise. Sports Medicine. 1992; 13 (1): 25-36 [ Links ]
16. Shiffman E, Ohrbach R, Truelove E. Diagnostic Criteria for Temporomandibular Disroders (DC/TMD) for clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014; 28 (1): p6-27. [ Links ]
17. Gonzalez F, Guardia L, Schiavone G,. Programa de ejercicios aerobicos o de resistencia cardiorespiratoria. En Mazza M. Manual para la prescripción de ejercicio: actividad física y ejercicio para la salud. 1era. ed. Montevideo, Cátedra de Medicina del ejercicio y deporte: DEDOS; 2011, p129-165 [ Links ]
18. Deppiésse F. La prescription des activités physiques en practique médicale courante. En : Depiésse F, Coste O. Prescription des activités physiques en prévention thérapeutique. 2ª edition Issy-les-Moulineaux: Elsevier, 2016, p129-165. [ Links ]
19. Karvonen J, Vourimaa T. Heart rate and exercice intensity during sports activities. Practical application. Sports Med.1988; 5 (5): p303-11. [ Links ]
20. Azam S. Madani, Amirtaher Mirmotazavi. Comparison of three treatment options for painful temporomandibular joint clicking. Journal of Oral Science. 2011; 53 (3): 349-354. [ Links ]
21. Vicente-Barrero M, Yu-Lu S., Zhang B. The efficacy of acupunture and decompression splints in the treatment of temporomandibular joint pain-dysfunction syndrome. Med Oral Patol Oral Cir Bucal. 2012. 17 (6): 1028-1033. [ Links ]
22. Ficnar T, Middelberg C, Rademacher B. Evaluation of the effectiveness of a semi-finished occlusal aplaiance- a randomized, controlled clinical trial. Head Face Medicine- 2013; 9: 5 http://www.head-face-med.com/content/9/1/5 [ Links ]
23. Langenfeld M, Hart L, Kao P. Plasma B-endorphin responses to one-houre bicycling and running at 60% O2 max. Medicine&Science in Sports&Exercice. 1987; 19 (2): 83-86. [ Links ]
24. Rahkila P, Hakala E, Salminen K. Response of plasma endorphin to running exercises in male and female endurance athletes. Med Sci Sports Exerc. 1987; 19 (5): 451-5. [ Links ]
25. Maresh C, Sökmen B, Kraemer W. Pituitary-adrenal responses to arm versus leg exercise in untrained man. Eur. J Appl Physiol 2006. 97: 471-477. [ Links ]
26. Goldfarb A, Hatfield B, Potts J. Beta-endorphin time course response to intensity of exercise: effects of training status. Int J Sports Med. 1991; 12 (3): 264-8 [ Links ]
27. Golfarb A., Jamurtas A., Kamimori G. Gender effects on beta-endorphin response to exercise. Med Sci Sports Exerc. 1998; 30 (12):1672-6. [ Links ]
28. Hayot, M. La réhabilitation du malade respiratoire chronique. En Préfaut C. y Ninot G. Les test d`exercice: lépreuve dexercice, a charge croissant.Issy les Moulineaux: Elsevier Masson, 2009; p86-112. [ Links ]
29. Nishishinya M, Rivera J, Cayetano A. Intervenciones no farmacológicas y tratamientos alternativos en la fibromialgia. Med Cin (Barc). 2006; 127 (8): 295-9. [ Links ]
30. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews. 2017; 1 (1): CD011279. [ Links ]
Received: May 04, 2020; Accepted: September 14, 2020











 texto en
texto en