Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.22 no.35 Montevideo 2020 Epub 01-Jun-2020
https://doi.org/10.22592/ode2020n35a5
Research
Facial trauma in children and adolescents: 10 years analysis in a hospital of south of Brazil
1Residente en Cirugía Oral y Maxilofacial de la Facultad de Odontología de la Universidad de Passo Fundo, Rio Grande Do Sul, Brasil, fran81gy@hotmail.com
2Residente en Cirugía Oral y Maxilofacial de la Facultad de Odontología de la Universidad de Passo Fundo, Rio Grande Do Sul, Brasil
3Residente en Cirugía Oral y Maxilofacial de la Facultad de Odontología de la Universidad de Passo Fundo, Rio Grande Do Sul, Brasil
4Doctor en Cirugía oral y Maxilofacial (phD). Hospital São Vicente de Paulo, Hospital Da Cidade De Passo Fundo, Facultad de Odontología de la Universidad de Passo Fundo, Rio Grande Do Sul, Brasil
5Master en Odontopediatria (Msc). Facultad de Odontología de la Universidad Federal de Santa Maria, Santa Maria, Rio Grande Do Sul, Brasil
6Académica de odontología de la Facultad de Odontología de la Universidad de Passo Fundo, Rio Grande Do Sul, Brasil
Facial trauma has important characteristics that affect the diagnosis and treatment of children and adolescents.
Objective:
To analyze the epidemiology of facial trauma in children and adolescents in a hospital of south of Brazil.
Materials and methods:
An analytical cross-sectional cohort study was conducted between 2000 and 2010 at the Hospital Sao Vicente de Paulo, Passo Fundo, Brazil. Identifying etiological agents, gender, facial fractures and the existence of body injuries associated with facial trauma.
Results:
Facial injuries were more common than in the adolescent group (75.6%) compared to the paediatric population (24.3%). The jaw was the most affected bone (33.5%). Cranial trauma was the most common associated lesion in the paediatric population (33%).
Conclusion:
Men have a higher prevalence of facial trauma, in the same way adolescents tend to be more affected.
Key words: facial injuries; epidemiology; pediatrics; adolescent; facial bones
El trauma facial presenta características importantes que repercuten en el diagnóstico y tratamiento de niños y adolescentes.
Objetivo:
Analizar el cuadro epidemiológico del trauma facial en niños y adolescentes en un hospital de la región sur de Brasil.
Materiales e métodos:
Se realizó un estudio de corte transversal analítico entre los años de 2000 hasta 2010 en el Hospital São Vicente de Paulo, Passo Fundo, Brasil. Identificando los agentes etiológicos, género, fracturas faciales y la existencia de injurias corporales asociadas a los traumatismos faciales.
Resultados:
Los traumatismos faciales fueron más frecuentes en el grupo de adolescentes (75.6%) en comparación con la población pediátrica (24.3%). La mandíbula fue el hueso más afectado (33.5%). El traumatismo craneano fue la lesión asociada más frecuente en la población pediátrica (33%).
Conclusión:
Los hombres presentan mayor prevalencia de trauma facial, siendo que los adolescentes tienden a ser más afectados.
Palabras Clave: traumatismos faciales; epidemiología; pediatría; adolescente; huesos faciales
O trauma facial apresenta características importantes que refletem no diagnóstico e tratamento de crianças e adolescentes.
Objetivo:
Analisar o quadro epidemiológico do trauma facial em crianças e adolescentes em um hospital da região sul do Brasil.
Materiais e métodos:
Realizou-se um estudo de coorte transversal analítico entre os anos 2000 e 2010, no Hospital São Vicente de Paulo, Passo Fundo, Brasil. Foram identificados os agentes etiológicos, gênero, fraturas faciais e a presença de lesões associadas aos traumatismos faciais.
Resultados:
Os traumatismos faciais foram mais frequentes no grupo de adolescentes (75.6%), comparado com a população pediátrica (24.3%). A mandíbula foi o osso mais acometido (33.5%). O traumatismo craniano foi a lesão associada mais frequente na população pediátrica (33%).
Conclusão:
Os homens apresentaram maior prevalência do trauma facial, sendo o grupo de adolescentes o mais acometido.
Palavras Chave: traumatismos faciais; epidemiologia; pediatria; adolescente; ossos faciais
Introduction
Children are more likely to sustain facial trauma than adults due to the greater proportion of cranial mass in relation to total body volume1. Facial trauma in children has major characteristics in terms of prevalence, diagnosis and treatment, which makes pediatric trauma in children a significant subject given the psychological and physiological conditions of patients of that age. Both children and adolescents who are affected by trauma may have sequelae, mainly if the trauma reaches facial growth centers. Therefore, the approach and treatment applied are different for pediatric patients than for adults2.
Facial trauma among adults has been studied more frequently in recent decades due to its upward trend. According to some authors, this is mainly related to road traffic accidents, urban violence and everyday stress. The assessment of underage patients with craniofacial trauma or trauma in other anatomical regions must include fast initial treatment to decrease morbidity and mortality3.
Underage patients who have sustained facial trauma need to be thoroughly examined, as some traumas may include facial fractures. Facial fractures in children and adolescents require some form of surgery in at least 50% of cases, which can be performed with open reduction and internal fixation2. However, clinical treatment should be favored in most cases of facial fractures in children provided that the patient’s condition makes it possible2. Pediatric fractures may lead to facial bone disruption and impair tooth development. In these cases of facial fractures, biodegradable osteosynthesis, made of polymer of lactic and glycolic acid, has helped reduce sequelae when treating fractures surgically4-6.
The main aim of this work is to study the epidemiology of facial trauma in children and adolescents at Hospital São Vicente De Paulo Hospital, Passo Fundo, Brazil, between 2000 and 2010. This will enable us to determine the age group, gender, etiology, facial fractures and injury associated with the most frequent facial trauma seen in the maxillofacial surgery and trauma service.
Materials and methods
An analytical cross-sectional study was conducted between 2000 and 2010 at Hospital São Vicente de Paulo, Passo Fundo, Brazil. This was done jointly with the Medical and Statistical Record Service (SAME, for its Portuguese acronym), where standardized sheets of patients aged 0-19 with a history of facial trauma were analyzed. The patients were treated by professionals within the area of oral and maxillofacial surgery and trauma. This study was approved by the Ethics Committee of Hospital São Vicente de Paulo (HSVP) and the University of Passo Fundo (UPF) under registration number 342/2011.
The facial trauma records were classified: etiological agent, age, gender, and associated comorbidity. Similarly, if the patient was diagnosed with a facial fracture, the anatomical region of the fracture was recorded. Patients with only soft-tissue lesions were excluded.
The patients treated at the hospital were mostly Passo Fundo inhabitants. However, patients from nearby cities were included as they were referred to Hospital São Vicente de Paulo (HSVP) because it is a high complexity hospital and a reference in the region.
The etiological agents were divided into six groups, taking previous epidemiological studies on facial trauma as a reference7-9: assault, falls, road traffic accidents, sports accidents, work accidents and others. Firearm injuries, domestic violence, robbery and physical assault were grouped under “assault”. The item “road traffic accidents” includes motorcycle, bicycle and car accidents. The group “others” covers accidents with animals and trauma related to removing retained teeth. Correlations between age group and facial fractures were evaluated with a Pearson analysis and the Student t test was used to verify the statistical difference. SPSS 18.0 and Windows Microsoft Excel were used for this study, and the minimum significance level adopted was 5%.
Results
Of a total of 1385 records of patients with facial trauma analyzed, 283 met the 0-19 age inclusion criteria. In the 0-9 group of pediatric patients there were 69 records, in the group of adolescents aged 10 to 19 years, 214. These two groups amounted to 20.43% of the total number of records.
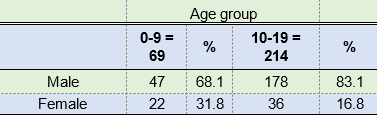
Regarding gender, 225 were male (79.50%) and 58 female (20.49%). Regarding age, 69 patients were children (24.38%) and 214 patients were adolescents (75.61%). If the patient had been diagnosed with facial fracture as a result of trauma, the fracture region was anatomically classified.
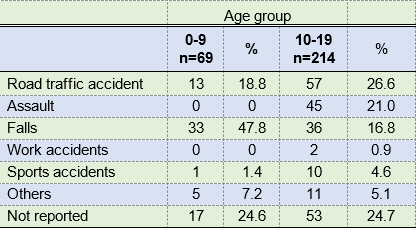
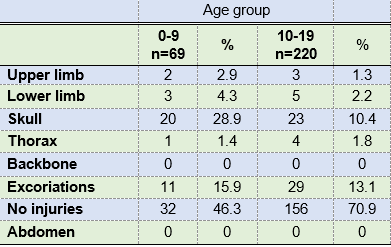
The adolescent group was the most affected within facial trauma, also having a high incidence of facial fractures and associated injuries (Tables 1, 2, 3 and 4). Mandible and nasal bone fractures were found to be more prevalent in both age groups. Le Fort fractures were also significant, as they had occurred in 24 patients in the adolescent group, and also naso-orbito-ethmoid fractures with 15 cases in the pediatric group (Table II). The relationship between these fractures and both age groups was significant: p<0.01.
Similarly, males predominated in the pediatric group, accounting for 68.11%. Therefore, the male gender is the most affected one, regardless of age group (Table 1).
Table 2: Distribution of cases by age group and facial fracture region
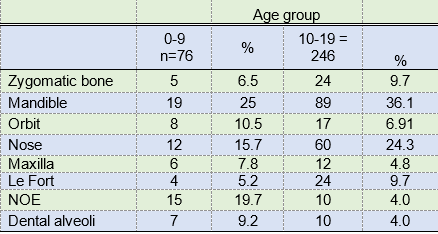
NOE: Naso-orbito-ethmoid Le Fort: Classifications II, II, III
The most frequent causes in both age groups were road traffic accidents, followed by falls, there being a significant connection with the age group: p>0.001. The number of falls (n=70) and road traffic accidents (n=69) were similar. However, in children, falls were more frequent (47.8%), and in the second age group, road traffic accidents were more frequently represented (26.6%). Additionally, assault ranked second in the adolescent group. It should be noted that 70 records analyzed were classified as “not reported” regarding etiological agents, amounting to 25% of each group approximately (Table 3).
The associated injuries were collected from the clinical records analyzed, observing those patients who sustained facial trauma and an additional injury elsewhere in the body. This was the case because the same patient could have several injuries associated with the facial trauma event. There were no associated injuries in 66.5% of the cases between ages 0 and 19. In the 0-9 age group, the most frequent associated injury was head trauma (30%) followed by excoriation (16%). In contrast, in the 10-19 age group, excoriation was the most common type of associated injury (13.1%) followed by head injuries (10.4%) (Table 4).
Discussion
Trauma is among the leading causes of death and morbidity in the world, accounting for 7.4% to 8.7% of hospital emergency care cases10. One of the consequences of facial trauma is facial fractures. Although they are less frequent in children than in adults, significant care and attention must be taken mainly when considering the patient’s age, development phase and bone growth3.
Only 1% to 15% of all facial fractures occur in the pediatric population1,11. This low incidence of pediatric facial fractures compared to facial fractures in young adults is probably related to the elasticity of children’s bones, the lack of sinus pneumatization and the projection of the prominent malar with the presence of abundant adipose tissue in the region12-13. We should also consider the fact that children live in a more protected environment, usually monitored by an adult1,3,5.
Male patients in the 10-19 age group had about four times more cases than the 0-9 age group. Previous studies on facial trauma show that males are more affected than females among the pediatric population and in adolescents, including late adolescence6,14-15. The fact that males are the most affected can be explained by the difference in behavior compared to females16-17.
This study showed that the most affected bone within the two age groups was the mandible, with a total of 108 cases, amounting to 38.1% of the records analyzed. Similarly, the mandible was cited in other studies as the most affected bone considering the same two age groups6,18-19. The mandible is the most affected due to its topography, anatomy, and projection into the lower third of the face. Like the skull, it absorbs a large part of the traumatic impact; additionally, the bones of the middle third of the face are extremely elastic20.
Regarding etiology, falls were the main cause of trauma for the 0-9 age group. The figure was also considerable in the 10-19 age group. Similarly, road traffic accidents were also significant, accounting for 25% of cases. These statistics are consistent with a study conducted in Brazil, in the city of São Paulo, where 110 records were analyzed between 2008 and 2011. The most common etiological agent was falls, followed by road traffic accidents15.
In this study, falls are the leading cause of trauma among the 0-9 age group, probably because children in this age group begin to walk and have contact with the outside environment. When toddlers take their first steps, they still lack some motor skills and stability, which can generally result in falls and facial trauma15. Furthermore, after reaching an age in which motor skills and stability when walking would be widely developed, usually after age five, the social environment changes and children begin to have more contact with the outside world, connecting with other people and coming into contact other environments. These children go to school and participate in sports, their height, weight and strength also increase, making them more prone to trauma6,19.
The 10-19 age group includes the transition between children and adolescents. Adolescence in turn is divided into early and late. Early adolescence includes the ages between 10 and 14, and late adolescence stretches between 15 and 1921. Given these circumstances, most adolescents tend to interact with society and also start operating machinery19. The hospital where this study was conducted admits a large number of patients from rural areas, where there is little police control over motor vehicles. This has an impact on road traffic accidents, as individuals operate machinery without being qualified, for example by riding motorcycles without the necessary protective equipment and exposing themselves to facial trauma. As set forth in Brazilian legislation, only people over 18 are allowed to drive vehicles, which means that only people over that age can become road traffic accident perpetrators. However, when underage adolescents are affected, they are restricted to the status of passengers or victims of a run over accident1,6,9,14-15.
Forty-five assault cases were recorded in this study (Table III) in the 10-19 age group. This might entail that individuals that are freer are more exposed to the outside environment and new people. This, together with alcohol, can be linked to fights and on many occasions to being attacked by their close relatives22.
Facial injuries can often be accompanied by bodily injuries such as head injuries, abdominal, thoracic, cervical injuries, as well as dentoalveolar injuries and soft-tissue lacerations23-24. This study did not find concomitant injuries associated with facial trauma in 66.4% of all the records analyzed. In the 10-19 age group, excoriations were the most commonly found type of injury (13.1%) followed by skull injuries (10.4%). Already in the 0-9 age group, the most frequent associated injury was head trauma (28.9%). This may be related to the patients’ increased craniofacial proportion and frontal prominence1. Likewise, a study revealed that out of 215 children with facial trauma, 6.3% had serious injuries associated mainly with skull injuries (80.5%)13.
Conclusions
The epidemiological survey conducted in this study allows us to conclude that facial trauma is a health problem among children and adolescents, mainly male patients. Adolescents (aged 10-19) tend to be more commonly affected. The mandible and nasal bones were the most prone to fractures. About a third of the cases had some type of associated injury, head trauma being the most frequent one (15.1%).
REFERENCES
1. Wymann NME, Hölzle A, Lizuka T. Pediatric Craniofacial Trauma. J Oral Maxillofac Surg. 2008; 66 (1): 58-64. [ Links ]
2. Shand JM, Heggie AA. Maxillofacial injuries at the Royal Children's Hospital of Melbourne: a ?ve year review. Ann R Australas Coll Dent Surg. 2000; 15:166-9. [ Links ]
3. Vyas RM, Dickinson BP, Wasson KL, Roostaeian J. Bradley JP. Pediatric facial fractures: current national incidence, distribution, and health care resource use. J Craniofac Surg. 2008;19 (2): 339-50. [ Links ]
4. Iatrou I, Theologie-Lygidakis N, Tzerbos F. Surgical protocols and outcome for the treatment of maxillofacial fractures in children: 9 years' experience. Journal of Cranio-Maxillo-Facial Surgery. 2010; 38 (7): 511-16. [ Links ]
5. Qing-Bin Z, Qiang ZZ, Dan C, Yan Z. Epidemiology of maxillofacial injury in children under 15 years of age in southern China. Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115 (4): 436-441. [ Links ]
6. Ferreira PC, Amarante JM, Silva PN, Rodrigues JM, Choupina MP, Silva AC, Barbosa RF, Cardoso MA, Reis JC. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005; 115 (6):1500-8. [ Links ]
7. Bittencourt OTC, Londero RLC, Marques CG, Piatto VN, Maniglia JV, Molina FD. Six years of facial trauma care: an epidemiological analysis of 355 cases. Braz. j. otorhinolaryngol. (Impr.) [Internet]. 2010 Oct; 76 (5): 565-574. [ Links ]
8. Portoman M, Torriani MA. Estudo de prevalência das fraturas bucomaxilofacias na região de Pelotas. Revista Odonto Ciênc. 2005; 20:63-8. [ Links ]
9. Andrighetti RZ, Birnfeld WJC, Volkweis RM, Gerhardt EL, Buchmann EM, Bavaresco CS. Epidemiological study of facial fractures at the Oral and Maxillofacial Surgery Service, Santa Casa de Misericordia Hospital Complex, Porto Alegre - RS - Brazil. Rev. Col. Bras. Cir. 2017; 44 (5): 491-497. [ Links ]
10. Barker R, Hockey R, Spinks D, Miles E. Facial Injury. Injury Bulletin Queensland Injury Surveillance Unit . 2003; 79:1-6. [ Links ]
11. Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90 (2): 126-134. [ Links ]
12. Holland AJ, Broome C, Steinberg A, et al: Facial fractures in children. Pediatr Emerg Care. 2001; 17 (3):157-60 [ Links ]
13. Gassner R, Tarkan T, Hachl O, Moreira R, Ulmer H. Craniomaxillofacial Trauma in children: A Review of 3,385 Cases With 6,060 Injuries in 10 Years. J Oral Maxillofac Surg. 2004; 62 (4): 399-407. [ Links ]
14. Rahman RA, Ramli R, Rahman NA, Hussaini HM, Idrus SM, Hamid AL. Maxillofacial trauma of paediatric patients in Malaysia: a retrospective study from 1999 to 2001 in three hospitals. Int J Pediatr Otorhinolaryngol. 2007; 71 (6): 929 - 936. [ Links ]
15. Nardis AC, Costa SAP, Silva RA, Kaba SCP. Patterns of paediatric facial fractures in a hospital of Sao Paulo, Brazil: a retrospective study of 3 years. Journal of Cranio-Maxillo-Facial Surgery. 2013; 41(3): 226-229. [ Links ]
16. Crockett DM, Mungo RP, Thompson RE. Maxillofacial trauma. Pediatr Clin North Am. 1989; 36:1471-1494. [ Links ]
17. Oji C. Fractures of the facial skeleton in children: A survey of patients under the age of 11 years. J Craniomaxillofac Surg .1998; 26: 322-325. [ Links ]
18. Ukpong DI, Ugboko VI, Nduke K C, Gbolahan O. Psychological Complications of Maxillofacial Trauma: Preliminary Findings From a Nigerian University Teaching Hospital. J Oral Maxillofac Surg. 2007; 65 (5): 891- 4. [ Links ]
19. Scariot R, de Oliveira IA, Passeri LA, Rebellato NL, Muller PR. Maxillofacial injuries in a group of Brazilian subjects under 18 years of age. J Appl Oral Sci. 2009; 17 (3): 195-8. [ Links ]
20. Jennings RB. Facial Fractures in Children. Otolaryngologic Clinics of North America. 2014; 47 (5): 747-761. [ Links ]
21. Johnson SB, Blum RW, Giedd J. Adolescent Maturity and the Brain: The promise and pitfalls of neuroscience research in adolescent health policy. Journal of Adolescent Health. 2009; 45 (3): 216-221. [ Links ]
22. Li Z, Li ZB. Characteristic changes of paediatric maxillofacial fractures in China during the past 20 years. J Oral Maxillofacial Surg. 2008; 66 (11): 2239-2242. [ Links ]
23. Zimmermann CE, Troulis MJ, Kaban L. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2005; 34:823-33. [ Links ]
24. Thorén H, Snäll J, Salo J, Taipale LS, Kormi E, Lindqvist C, Törnwall J. Occurrence and Types of Associated Injuries in Patients With Fractures of the Facial Bones. J Oral Maxillofac Surg. 2010; 68 (4): 805-10. [ Links ]
Authorship Note: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript Authors: Franklin David Gordillo Yépez has contributed in 1,2,3,4,5,6 Tiago Nascimento Mileto has contributed in 3,4,6 Cassian Taparello has contributed in 1,4,5 Janessa Luiza Engelmann has contributed in 3,5,6 Simone Pinheiro Siqueira has contributed in 4,5 Ferdinando De Conto has contributed in 1,2,3,5,6
Received: September 17, 2018; Accepted: February 18, 2020











 texto en
texto en