Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.21 no.34 Montevideo dez. 2019 Epub 01-Dez-2019
https://doi.org/10.22592/ode2019n34a7
Case Reports
Oral manifestations of pigmentary incontinence (Bloch-Sulzberger syndrome). Case report
1 Facultad de Ciencias de la Salud. Universidad Privada Juan Pablo II. Lima, Perú. yuricastro_16@hotmail.com
2 Facultad de Odontología. Sociedad Científica de Estudiantes de Odontología. Universidad Nacional Mayor de San Marcos. Lima. Perú
A 13-year-old female patient went to the pediatric dentistry service of the Oral Health Institute of the Central Air Force Hospital of Peru in September of 2018. She sought care to have her temporary partial prosthesis renewed. The extraoral clinical examination showed scar lesions on the skin of the nasal region; the intraoral evaluation showed the loss of multiple teeth, wide and thin edentulous ridges, alterations in dental morphology, as well as the inconsistency of the dental eruption with the patient’s age. The radiographic examination showed alteration and delay in dental eruption, impaction of a tooth in the jaw, lack of root development and persistence of temporary teeth. The definitive medical diagnosis was Bloch-Sulzberger syndrome, also referred to as “pigmentary incontinence” or “incontinentia pigmenti”. This syndrome is characterized by presenting a variety of oral manifestations such as dental agenesis, alteration in dental morphology, retained and/or impacted teeth as well as alteration and delay in tooth eruption. At a systemic level, this syndrome has lesions that affect the skin, hair, vision, central nervous system, among others.
Keywords: syndrome; tooth eruption; dental agenesis; tooth; impacted
Paciente de sexo femenino de 13 años de edad que acudió al servicio de Odontopediatría del Instituto de Salud Oral del Hospital Central de la Fuerza Aérea de Perú en el mes de setiembre del año 2018 debido a una renovación en la prótesis parcial provisional que utilizaba desde hace cinco meses. Al examen clínico extraoral se evidenció lesiones cicatrizales en la piel de la región nasal; durante la evaluación intraoral se evidenció la pérdida de múltiples dientes, rebordes edéntulos amplios y delgados, alteraciones en la morfología dentaria, así como discordancia de la erupción dentaria con la edad de la paciente. Al examen radiográfico se evidenció alteración y retardo en la erupción dentaria, impactación de un diente en la mandíbula, falta de desarrollo radicular y persistencia de dientes temporales. El diagnóstico médico definitivo fue el Síndrome de Bloch - Sulzberger también denominado como “incontinencia pigmentaria”. Este síndrome se caracteriza por presentar una variedad de manifestaciones orales como: agenesia dentaria, alteración en la morfología dentaria, dientes retenidos y/o impactados así como alteración y retraso en la erupción dentaria. A nivel sistémico este síndrome presenta lesiones que afectan a la piel, pelo, visión, sistema nervioso central, entre otros.
Palabras claves: Síndrome; Erupción dental; Agenesia dental; Diente impactado
Paciente do sexo feminino, 13 anos, que compareceu ao Serviço de Odontopediatria do Instituto de Saúde Bucal do Hospital Central da Força Aérea do Peru, em setembro de 2018, devido à renovação da prótese parcial provisória utilizada por ela. por cinco meses. O exame clínico extraoral mostrou lesões cicatriciais na pele da região nasal; Durante a avaliação intraoral, a perda de múltiplos dentes, cristas edêntulas, extensas e finas, alterações na morfologia dentária, bem como a incongruência da erupção dentária com a idade do paciente foi evidente. O exame radiográfico mostrou alteração e atraso na erupção dentária, impactação de um dente na mandíbula, falta de desenvolvimento radicular e persistência de dentes temporários. O diagnóstico médico definitivo foi a síndrome de Bloch - Sulzberger, também conhecida como "incontinência pigmentar". A síndrome é caracterizada por apresentar uma variedade de manifestações bucais, como: agenesia dentária, alteração na morfologia dentária, retenção e / ou impacto dos dentes, bem como alteração e atraso na erupção dentária. Em nível sistêmico, essa síndrome apresenta lesões que afetam a pele, o cabelo, a visão, o sistema nervoso central, entre outros.
Palavras-chave: Síndrome; Erupção cutânea; Agenesia dentária; Dente impactado
Introduction
Bloch-Sulzberger syndrome or incontinentia pigmenti (IP) is considered an X-linked genodermatosis 1. It is characterized by the presence of bullous lesions throughout the skin. It has four clinical stages: vesicularbullous, verruciform, hyperpigmented and hypopigmented. Patients rarely develop all four forms progressively, stages which sometimes overlap.
The syndrome affects various organs and is characterized by the formation of band-shaped blisters, distributed in a linear way or diversified, and which commonly appear shortly after birth2. The lesions affect the skin, hair, teeth, eyes, central nervous system, among others3.
Background
It was first described by Garrod as a variety of Mongolian idiocy with a peculiar pigmentation”4-5. It was later defined by Bardach (1925), Bloch (1926), Sulzberger (1928) and Siemens (1929); this is why it is also referred to as Bloch-Siemens Syndrome6-7.
It most commonly affects females (95%) because males present high prenatal mortality rates1, although survival has been reported in males with a XXY genotype (Klinefelter syndrome) or somatic mosaicism (genetic alteration where two or more populations of cells with different genotypes coexist in the same individual)8-9.
The incidence is approximately 1 per 50,000 live births10. There is no current data on its prevalence, but it is reported that it may appear in all population groups, with a predominance in white-skinned people 11-12.
The main clinical manifestations are evident at the skin level, which is why its diagnosis is managed dermatologically; however, there are also alterations in the eyes, hair, nails, central nervous system, teeth, among other things3,9,12.
Regarding oral health, teeth are affected in 50 to 80% of patients; there is a delay in tooth eruption, partial or total tooth agenesis, atypical tooth morphology of the following types: conoidal, trapezoidal, pin-shaped, microdontia and accessory cusps. There often appear impacted teeth and malocclusions 13; Patients with this syndrome tend to develop a class III malocclusion due to a rotation of the jaw given the need to cover tooth loss 14.
Prevention of oral diseases is essential in this type of patient, with an emphasis on oral hygiene, diet consistency, frequency of sugar intake and regular dental check-ups to maintain oral health 3. This report presents a clinical case of Bloch-Sulzberger syndrome without complications. It discusses oral manifestations, clinical picture and includes a literature review.
Case description
A 13-year-old female patient from Talara (Piura, Peru). She was referred to the dentistry service of the Oral Health Institute of the Central Air Force Hospital of Peru in September 2018. She had a history of multiple missing teeth since childhood. The patient reported that her left posterior lower teeth never erupted and that several teeth showed morphological alterations.
In 2007, she was referred by the neurology department to the pediatric dentistry service. The intraoral evaluation revealed 14 teeth, a thin right alveolar ridge, twisted front teeth and a reverse front bite.
Clinical characteristics
The medical history showed that given the anterior crossover, the patient underwent orthopedic treatment with a Hawley plate with expansion screw and buccal clasps for maxillary retraction (Fig. 1A and 1B). As a result, the crossover was corrected and arch perimeter was gained for the eruption of permanent teeth. In addition, in 2011, a temporary removable partial prosthesis was made to restore functionality and aesthetics. Currently, the patient seeks assistance to have her prosthesis replaced.
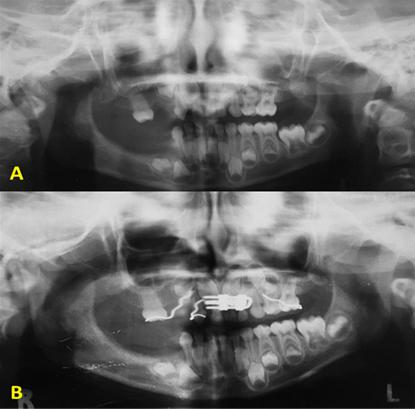
Fig. 1: A. (Panoramic radiography, 2007, before placing the orthopedic appliance). B. (X-ray of the orthopedic appliance with an expansion screw, posterior to the palatal disjunction stage).
Her medical history did not relate harmful or pathological habits; however, in 2009 the Dermatology Service of the Central Air Force Hospital reported linear hyperpigmented lesions in the arms, limbs and nasal region; no ocular or nail alterations were observed. The overall assessment showed that she was a hemodynamically stable patient, with vital functions (blood pressure, pulse, respiratory rate and temperature) within normal values, and was also asymptomatic; scar lesions in the nasal region were observed in the current dermatological evaluation (Fig. 2A, 2B and 2C).
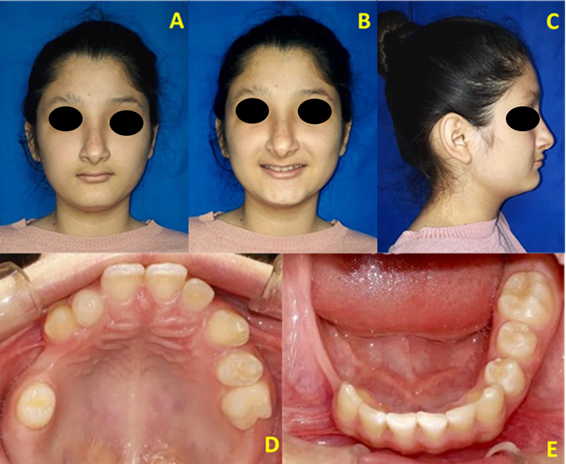
Fig. 2: A, B, (Atrophic lesions in the nasal region that occur cumulatively). C (Protruded chin, depressed malar region). D (Multiple missing teeth, morphological alterations and persistence of deciduous teeth). E (Thin alveolar ridge at the lower right area).
A routine odontogram was performed in the intraoral examination. Molars and premolars were missing in the posteroinferior area, as well as upper premolars on the left side (Fig. 2D and 2E); morphological alterations in teeth and persistence of primary teeth (Fig. 3A, 3B and 3C). In addition, the ridges were reduced in height and thickness; during palpation, the patient reported slight localized and short-lived pain in the right posteroinferior area. The periodontal examination showed good gingival health.
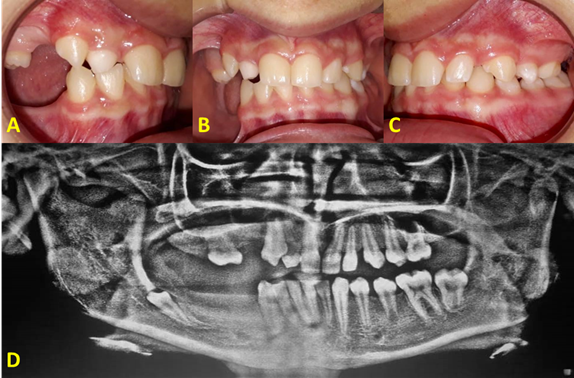
Fig. 3: A. (Agenesis and diminished ridges in sextants 1 and 6). B. (Intraoral asymmetry due to missing teeth) C. (Occlusal accommodation) D. (Current panoramic radiography).
Radiographic features
A panoramic radiography was taken and we observed the asymmetry of the mandibular bodies, slight maxillary sinus pneumatization, apparently normal nasal septum and turbinates. Temporary teeth were observed, as well as agenesis of permanent teeth, delay in apical maturation, delay in eruption chronology and a retained tooth (Fig. 3D).
Diagnosis
The definitive medical diagnosis since childhood was Bloch-Sulzberger syndrome (incontinentia pigmenti), which was compatible with the skin and extracutaneous (dental) manifestations observed.
A comprehensive and multi-specialized treatment was planned to extract the retained tooth in the left posteroinferior area, in addition to orthodontic-prosthetic management for the rehabilitation of mastication and aesthetics.
Discussion
This case report shows the most common oral manifestations of Bloch-Sulzberger syndrome; a rare dominant hereditary alteration linked to the X chromosome1.
The etiology of this syndrome involves pigment mosaicism, which in the past has been erroneously divided into two phases: sporadic IP (or IP1) associated with an Xp11 locus mutation, and congenital IP (or IP2) associated with the Xp28.20 region15.
This clinical case presents the oral diagnostic characteristics of incontinentia pigmenti. Typical signs like hypodontia and conical teeth were observed; tooth anomalies of number and shape that usually entail no major clinical relevance.
The following steps are essential to make a diagnosis: clinical examination (major and minor criteria); blood tests (high levels of IgE, leukocytosis, eosinophilia are usually found, as well as chemotaxis defects); anatomopathological studies (to confirm and observe free melanin grains in the hyperpigmentation zone, “eosinophilic spongiosis”, as well as dyskeratosis); alternative molecular genetic analysis is also recommended (IKBKG molecular study (NEMO) locus Xq28) 3.
The major criteria (skin manifestations) show an evolution divided into four stages: 1. vesicularbullous or inflammatory, 2. verruciform, 3. hyperpigmented, 4. hypopigmented or also referred to as atrophic. Each stage presents characteristic skin lesions, although they usually coexist and do not develop sequentially in all patients. Lesions are more common in limbs and the torso; the least affected areas are the flexion creases and the face.
Minor criteria (extracutaneous manifestations) have been reported in almost 80% of cases, but are less common in males (probably due to mosaicism)12. These criteria include:
a)Hair: present in almost 50% of cases. Hair loss at crown level (28-50%). There is also agenesis of eyebrows and partial aplasia of sweat glands 6.
b)Nails (hands and feet): they are usually affected in 40% of cases in a mild and transient way; wrinkles, holes and onychogryphosis also occur.
c)Eyesight: in 35-77% of cases there are no ocular alterations; the ones that do appear most commonly are in the retina (60%), strabismus (18-43%), as well as decreased visual acuity and blindness. There is often myopia (46%) or hyperopia (37%); exudative chorioretinitis is the classic pathology.
d)Central nervous system: present in 30-50% of cases: psychomotor disorders, hydrocephalus, brain atrophy and intellectual disability are observed 12.
e)Teeth: They are the most frequent manifestations, in up to 80% of cases. Both deciduous and permanent dentition are affected. It is characterized by delayed tooth eruption (18%), partial agenesis (43%), shape anomalies (30%): conoidal, trapezoidal, pin-shaped, microdontia, accessory cusps. Included teeth are observed in the X-ray. Most patients have a class III malocclusion with decreased vertical dimension and mandibular rotation. The constitution and internal structure of the tooth and enamel is normal3,6,12,16.
This case was diagnosed conducting an interdisciplinary evaluation that included consultations with dermatology, neurology and pediatric dentistry specialists. As this is a hereditary disease, it requires a detailed family history and a complete physical examination if they were not performed in other services; a genetic analysis might also be included.
This clinical case included lesions typical of the different stages of IP (hyperkeratotic lesions, accumulated brown-grey maculae, vesicles and hypopigmented maculae in different parts of the body). No neurological or ocular conditions were observed.
An interdisciplinary approach is recommended for dental management, which should include the different specialties.
-Prevention and care of oral health should be prioritized through rigorous oral hygiene, correct brushing and proper flossing.
-Diet monitoring: physical consistency (related to its adhesiveness), high rate of cariogenecity (especially at night when salivary secretion decreases) and frequency of intake of cariogenic foods.
Highly refined sugary products should be avoided, as they promote biofilm accumulation and the appearance and development of carious lesions and periodontal disease. The following are essential: periodic dental check-ups, fillings, topical fluoride applications and use of mouthwash.
Therapeutic alternatives will depend on etiology. Early orthopedic treatment may include the use of chin cups, facial masks, and/or class III function regulators; later, in addition to orthopedic treatment, surgical alternatives may be added to correct severe skeletal dysmorphia 3,12,17,18 .
The partial absence of some teeth may benefit orthodontic treatment as the position of other teeth can be modified by opening spaces or closing diastemas. They can also be used as abutments for partial prostheses, using self-tapping titanium implants or miniscrews, as anchorage for retrusive and intrusive movements 19-20.
Removable prostheses with acrylic teeth are also indicated for aesthetic reconstitution until further development of the maxillary bone can be achieved and an implant-supported prosthesis can be placed. In adults, fixed or adhesive conventional prostheses, and even dental implants, can be indicated; in these cases, it is essential to identify family patterns in order to detect the mutation 3.
In this case, the patient’s removable partial prosthesis was adapted to allow for the functional restoration of the dental arches in order to maintain the vertical space and dimension of the occlusion, facilitate mastication, avoid interfering with the child’s own development and allow for harmonious growth.
Conclusions
Bloch-Sulzberger syndrome (incontinentia pigmenti) is a rare genetic disease. Its main clinical signs and manifestations appear in the skin; however, the main extracutaneous manifestations are found in the oral cavity and both are the basis of the diagnosis. Neurological signs are the most serious in the disease and are the main prognostic factor. In this case, clinical examination, background review (medical history) and X-ray testing were used to enable the functional and aesthetic treatment, in order to have a positive impact on the patient’s quality of life and psychosocial relationships.
REFERENCES
1. Mühlenstädt E, Eigelshoven S, Hoff NP, Reifenberger J, Homey B, Bruch-Gerharz D. Bloch-Sulzberger syndrome. Hautarzt. 2010; 61 (10): 831-3. [ Links ]
2. Morrell DS, Burkhart CN, Siegel D. Enfermedades hereditarias seleccionadas. En: Eichenfield L, Frieden I, Esterly N. (eds.). Dermatologia Neonatal. 2da ed. Barcelona, España: Elsevier, 2009. p485 [ Links ]
3. Pipa VA, González GM, López-Arranz ME, Fernández TJ. Incontinencia Pigmentaria. Consideraciones odontoestomatológicas: Profilaxis y terapéutica. Av Odontoestomatol. 2005; 21 (4): 211-5. [ Links ]
4. García DJ, De Unamuno P, Fernández LE, Salazar VJ, Armijo M. Incontinentia pigmenti: XXY male with family history. Clin Genet. 1990; 38 (2): 128-38. [ Links ]
5. Ormerod AD, White MI, McKay E, Johnston AW. Incontinentia pigmenti in a boy with Klinefelter´s syndrome. J Med Genet. 1987; 24 (7): 39-41. [ Links ]
6. Landy SJ, Donnai D. Incontinentia pigmenti (Bloch-Sulzberger syndrome). J Med Genet.1993; 30 (1): 53-9. [ Links ]
7. Geiges ML. Traces of Marion B. Sulzberger in the Museum of Wax Moulages in Zurich and their importance for the history of dermatology. J Am Acad Dermatol.2009; 60 (6): 980-4. [ Links ]
8. The International Incontinentia Pigmenti (IP) Consortium. Genomic rearrangement in NEMO impairs NF-(kappa)B activation and is a cause of incontinentia pigmenti. Nature. 2000;405 (6785): 466-72. [ Links ]
9. Kenwrick S, Woffendin H, Jakins T, Shuttleworth SG, Mayer E, Greenhalgh L, Whittaker J, Rugolotto S, Bardaro T, Esposito T, D'Urso M, Soli F, Turco A, Smahi A, 10.Hamel-Teillac D, Lyonnet S, Bonnefont JP, Munnich A, Aradhya S, Kashork CD, Shaffer LG, Nelson DL, Levy M, Lewis RA; International IP Consortium. Survival of male patients with incontinentia pigmenti carrying a lethal mutation can be explained by somatic mosaicism or Klinefelter syndrome. Am J Hum Genet. 2001; 69 (6): 1210-7. [ Links ]
11. Chang JT, Chiu PC, Chen YY, Wang HP, Hsieh KS. Multiple clinical manifestations and diagnostic challenges of incontinentia pigmenti - 12 years' experience in 1 medical center. J Chin Med Assoc. 2008; 71(9): 455-60. [ Links ]
12. Carney RG. Incontinentia pigmenti: A world statistical analysis. Arch Dermatol.1976; 112 (4): 535-42. [ Links ]
13. Gómez VR, Juárez M, Plascencia GA, Reyes MG, Saénz CC, Káram M et al. Incontinentia pigmenti. Artículo de revisión. Dermat Cosmet Méd Quir. 2010;8 (2): 104-9. [ Links ]
14. Rouse JS. Incontinentia pigmenti: overcoming cosmetic challenges. Compend Contin Educ Dent.1999; 20 (11): 1034-6. [ Links ]
15. Rouse JS. Incontinentia pigmenti: overcoming cosmetic challenges. Compend Contin Educ Dent. 1999; 20 (11): 1040-1. [ Links ]
16. Berlin AL, Paler AS, Chan LS. Incontinentia pigmenti: A review and update on the molecular basis of pathophysiology. J Am Acad Dermatol. 2002; 47(2): 169-87. [ Links ]
17. Kasmann KB, Jurin BB, Ruprech KW. Incontinentia pigmenti (Bloch-Schulzberger syndrome): case report and differential diagnosis to related dermato-ocular syndroms. Ophthalmologica. 1999; 213 (1): 63-9. [ Links ]
18. Romero A, Tufiño M, Villacís A, Salazar M. Incontinencia pigmentaria o síndrome de Bloch-Sulzberger. Dermatol Rev Mex. 2014; 58 (6): 539-43. [ Links ]
19. Atamari AN, Solórzano GS. Incontinentia pigmenti (Síndrome de BlochSulzberger) en un paciente varón. Reporte de un caso. Rev Med Hered. 2015;26 (4): 238-41. [ Links ]
20. Maino BG, Pagin P, Mura P. Spider Screw (r): Anclaje absoluto de carga inmediata. Rev Esp Ortod. 2003;33 (1): 21-30. [ Links ]
21. Puigdollers A. Anclaje estable sobre implantes palatinos. Rev Esp Ortod. 2003; 33 (2): 121-31. [ Links ]
Authorship contribution: 1.Conception and design of study 2.Acquisition of data 3.Data analysis 4.Discussion of results 5.Drafting of the manuscript 6.Approval of the final version of the manuscript YCR has contributed in: 1, 3, 5, 6. JCQ has contributed in: 2, 4, 6. EJG has contributed in: 2, 4, 5, 6.
Received: February 28, 2019; Accepted: July 27, 2019











 texto em
texto em 



