Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.20 no.31 Montevideo June 2018
https://doi.org/10.22592/ode2018n31a9
Case Report
Ascher syndrome: clinical case care and treatment
1Department of Oral & Maxillofacial Surgery III, School of Dentistry, Universidad de la República, Montevideo, Uruguay.
2Periodontics Department, School of Dentistry, Universidad de la República, Montevideo, Uruguay
3Department of Oral & Maxillofacial Surgery III, School of Dentistry, Universidad de la República, Montevideo, Uruguay
We present a case report of a patient with Ascher Syndrome. It is a rare, benign disorder with few cases reported in the world. Clinically, it is an anomaly which may be either congenital or acquired, characterized by a triad: blepharochalasis, double lip (upper lip is involved more often than lower lip, although on occasion both may be involved), and nontoxic thyroid goiter. Surgical treatment may be indicated as it is a deformity that interferes with mastication and speech, and which might have aesthetic implications.
Keywords Ascher syndrome; double lip
Presentamos un paciente con “Sindrome de Ascher”. Se trata de una rara entidad benigna, que es una anomalía congénita o adquirida de etiología desconocida. Clínicamente el Síndrome de Ascher, está compuesto por una tríada de signos clínicos: doble labio (siendo el superior el más frecuentemente involucrado), blefarocalasia y bocio no tóxico (agrandamiento tiroideo, no funcional y ausente en aproximadamente la mitad de los casos). Cuando la deformidad labial interfiere con la masticación o provoca groseras alteraciones estéticas, el tratamiento quirúrgico está indicado.
Palabras clave: Síndrome de Ascher; Doble labio
Introduction
This work presents a case of Ascher Syndrome (AS), a condition characterized by concurrent double lip, blepharochalasis and nontoxic thyroid enlargement, though the thyroid enlargement is not evident in a large number of cases1,2,3,4,5,6. It is a syndrome of particular interest for dentists, because many times the patient wanders through different medical specialties without a positive diagnosis as the low incidence of cases makes identification difficult1-3.
The occurrence of double lip has been described as a benign, rare or very uncommon congenital or acquired anomaly, without sex or racial predilection, which can sometimes be a manifestation of a specific syndrome1,3,7,8.
Its etiology is unknown. According to Ascher5-6, the upper lip is more frequently affected than the lower lip, at a ratio of 10:1. This developmental alteration can often appear alone or as part of a triad of clinical features, known as Ascher Syndrome (AS).
Background
A review of the scientific literature showed that Laffler1,9 was the first to report a case of double lip associated with blepharochalasis in 1909. In 1920, Ascher5 completes the clinical picture described by Laffler in 1909 by adding the thyroid hypertrophy. That triad of features is what is known today as Ascher Syndrome (double lip, enlargement of the eyelid skin and nontoxic thyroid enlargement).
Thyroid hypertrophy is not included consistently in most of the articles reviewed among the criteria for a positive diagnosis1,2,3,4,5,6,7,8,9,10. On occasion, in AS the extent of the lip and/or eyelid volume alterations is such that it can cause severe aesthetic and functional alterations, for which surgical correction is the only effective therapeutic approach for the area affected1,10-12.
Clinical case
The patient is a 14-year-old male (Fig. 1) referred by the Clinic of Periodontics of the School of Dentistry to the Department of Oral & Maxillofacial Surgery III, Universidad de la República, because his upper and lower lip were enlarged, and this greatly affected him psychologically in his relationships. The enlargement had become very noticeable four years before. He visited several medical specialists and dentists that could not make a positive diagnosis or suggest a treatment plan.
His medical history was started in 2013, when he was admitted to the Department of Oral & Maxillofacial Surgery II. Psychosomatic development was consistent with his age. The patient has had asthma and allergic rhinitis for several years, and reports having used inhalers like Seretide®.
Visceral axis of the neck, temporomandibular joints and neck palpation were unremarkable.
The visual examination of the area showed bilateral enlargements in the upper and lower lips, which were strongly noticeable when the lips were not in resting position. The enlargements involved the mucosal aspect of both lips, were elliptical in shape with the major axis parallel to the free edge of the lip. Enlargements were found in each hemilip. The mucosa covering them was normal in color and texture, and they were painless and soft to the touch. There was no family history of this kind of malformation.
The intraoral examination showed permanent dentition in canine to canine cross-bite. Upper lateral incisors were conoid in shape. The patient was undergoing the planning stage of periodontal and orthodontic treatment.
The following complementary tests were ordered: a complete blood count, which was normal; a thyroid blood test, which revealed normal levels of the thyroid stimulating hormone (TSH); and a thyroid ultrasound, which showed a slightly enlarged thyroid, as shown in Fig. 2.
Positive diagnosis of the case: Ascher Syndrome. The treatment plan chosen was surgical resection of lip enlargements with local anesthesia in two stages.
In the first stage we resected the upper lip enlargements (Fig. 3) and also performed a frenectomy of the upper lip for orthodontic reasons.
In the second stage, thirty days later, the surgical procedure was performed in the lower lip.
Both surgeries were performed using elliptical excision techniques with cold scalpel and the affected areas were sutured using separate stitches (Fig. 3).
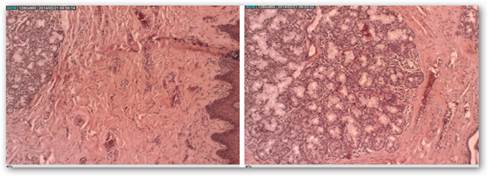
The histopathologic study of the surgical specimen obtained confirmed the clinical diagnosis. The two histological sections of the case presented here (Fig. 4) show, respectively:
- A panoramic view of labial mucosa.
- The submucosa of the lip with an abundance of collagen fibers, as well as a large number of mucous lip salivary glands.
The aesthetic surgical outcomes were very satisfactory for both patient and surgeon. This is shown in frontal images after thirty days (Fig. 5) and in profile images six months after surgery (Fig. 6). Frontal and profile images three years after surgery (Fig. 7)
Discussion
The complete form of the AS, double lip, blepharochalasis and thyroid enlargement, was described by Ascher in 19205,6.
The first case of double lip with blepharochalasis was described and reported by Laffer in 19091,9.
As a consequence, some authors such as Lebuisson D, Leroy L, Aron JJ, Jeaneau E, J. Guillard J P. refer to it as the “Laffer-Ascher Syndrome”13.
Because nontoxic thyroid goiter is not present in all cases (in only 10 to 50%)1,10,12-15, many authors recommend not considering it when diagnosing AS.
Other authors1,4,10,12-15 think nontoxic thyroid goiter is an inconsistent finding in some patients only during the initial stages of the syndrome, and that it can appear several years later, more slowly and delayed in relation to the lip and lid enlargements.
Blepharochalasis was first named and described by Fuchs in 1896, as an atrophic and progressive enlargement of the skin of the eyelids which can also include recurrent bouts of edema that may exacerbate the condition12,16, leading indirectly to vision impairment caused by the closure or narrowing of the palpebral aperture. In general, only the upper lids are affected and make it difficult for patients to keep their eyes open12. It is treated surgically, with a blepharoplasty to remove a wedge of the excess skin.
In AS, blepharochalasis can be larger or smaller in relation to the enlargement found in the double lip. Blepharochalasis and double lip usually appear at the same time and in more than 80% of cases they manifest before the age of 2017.
Double lip is a fold of excess or redundant hypertrophic tissue on the mucosal side of the lip and is the main element of the triad of features that characterize AS1.
It consists of excess tissue in the labial mucosa, located towards the inner part of the vermilion border, and not, strictly speaking, as its name seems to indicate, a duplication of the lip organ, but rather a localized enlargement of the labial mucosa.
In most of the cases reported the enlargement appears in only one lip. It frequently occurs bilaterally in the upper lip, and it less commonly affects the lower lip (ratio of 10:1 in favor of the upper lip)1-10,12-14.
The etiology of the syndrome is yet to be determined, and it can be of congenital or acquired origin4,10-12. Inheritance can be considered for some patients, due to the known familial cases reported by Franceschetti17 and Viallefot4,14.
Also, since most of the cases appear during puberty, some authors believe it could be triggered by hormonal disorders1,4.
In AS, the alterations in lips and eyelids occur abruptly and simultaneously, simulating an angioneurotic edema which partially diminishes.
The thyroid enlargement becomes noticeable more slowly and later, with a normal uptake of radioiodine (131I) and is only present in 10 to 50% of cases10-12,14,15.
As for double lip, the following have been described: a congenital form14 which develops during the second or third month of intrauterine life11, and an acquired form which may occur in isolation or as part of a syndrome such as AS1.
Isolated forms can be triggered by different factors such as habit or trauma (biting, suction, orthopedic and/or orthodontic appliances, etc.)11,18-20. They usually remit or their volume diminishes once the habit or trauma-causing agent is removed.
In general, the lip deformity is not visible when patients keep their lips closed (except in the larger cases), but it appears when they open their mouths or smile.
Macroscopically, in the upper lip it can manifest as a soft, mobile, overhanging mass which on occasion can extend from one commissure to the other, or can frequently be divided in the middle by the labial frenum, resulting in two globular or oblong, middle-sized masses1.The latter applies to the case presented here.
In the lower lip (very uncommon) it almost exclusively appears as two middle-sized bun-shaped masses, as shown in the patient’s photograph.
It can exceptionally be found in both lips1,4,14, as in this patient.
Histological examination showed masses of loose connective tissue, associated with numerous mucous salivary glands, like the ones normally occurring in the area1,12, which is consistent with the histopathologic study of the surgical specimen obtained.
To make a positive diagnosis of AS, we must find the clinical triad described above, and differential diagnosis with other lip enlargements, such as trauma macrocheilitis, cheilitis glandularis, lymphangioma, angioedema, granulomatous cheilitis, inflammatory fibrous hyperplasia, sarcoidosis and salivary gland tumors.
Surgical treatment is indicated when there is interference with phonation or mastication, habit of suctioning the hyperplastic tissue and, mainly, for aesthetic reasons, when it affects the psychological state of the patient, as in this case. As for the prognosis, these lesions tend not to relapse.
Different surgical techniques to correct a double lip have been described in the literature, all of which are for the upper lip, with the most common one being the elliptical excision of the enlargement, proposed by Digman in 194721.This technique is used by many authors until today, like Cortes-Aroche1, who published a description in 2007.
Reddy and Kotewara22 and Dorrance23 also advocate using the elliptical excision to remove the excess mucosa and the direct suture.
Guerrero Santos and Altamirano24 suggest using a W-plasty to avoid removing too much mucous tissue, a mistake which, according to them, can be made with the elliptical excision.
Lamster25 described a technique consisting of a triangular excision of mucosa, while Eski26 described a technique with a bilateral elliptical excision for the cases in which there is a central bridle, associated with a Z-plasty at the level of the bridle.
Other authors describe combinations and small alterations of the techniques that have already been described27-30.
As it was explained above, in this case we planned to resect in a first stage the upper lip enlargements and, on the following month, in a second surgical stage, those in the lower lip.
Both procedures were conducted using locoregional anesthesia.
We used elliptical excisions for both lips, suturing the affected areas using separate stitches, as described by Digman21 Fig. 3.
We also performed a simultaneous labial frenectomy in the upper lip, as indicted by the treating orthodontists.
Conclusions
1. The Ascher Syndrome is a very rare condition with only a few cases reported in scientific publications.
2. It can even more rarely involve the upper and lower lips simultaneously, as in this patient, who suffers major psychological and emotional consequences.
3. Despite its low incidence, it is of particular interest for dentists, because they are often the first healthcare professionals to detect it, and they can make a diagnosis and treatment plan.
4. Treatment with the elliptical surgical excision technique, used in both lips in this specific case, provided very satisfactory psycho-emotional results for the patient in the short and long term (three years)
Referencias
1. Cortes-Aroche S. Labio doble tratado con incisión en media luna. Presentación de un caso. Rev. Med. Inst.Mex.Seguro Soc. 2007; 45(3):277-80. [ Links ]
2. Kara IG, Kara CO. Ascher syndrome. Otolaryngol. Head Neck Surg. 2001;124(2):236-7. [ Links ]
3. Gorlin RJ, Cohen MM, Levin LS, eds. Syndromes of the head and neck. 3rd. Ed. New York: Oxford University Press.1990;p.420-1 [ Links ]
4. Gomez - Duaso AJ, Seoane J, Vazquez- Garcia J, Arjona C. Ascher Syndrome: report of two cases. J Oral Maxillofac Surg. 1981;34:31-4. [ Links ]
5. Ascher KW. Blepharochalasis mit struma und doppellippe. Klinische Monatsbl Augenheilkd 1920;65:86-97. [ Links ]
6. Ascher KW. Das syndrom blepharochalasis, struma und doppellippe kiln. En: Gorlin RJ, Pindborg JJ, editors Syndromes of the head and neck. New York: McGraw- Hill;1964.p.2287-88 [ Links ]
7. Barnett ML, Bossahardt LL, Morgan F. Double lip and doble lip with blepharochalasis (Ascher's syndrome). Oral Surg.1972; 34:727. [ Links ]
8. Alkan A, Metin M. Maxillary double lip: Report of two cases. J Oral Surg. 2001;4369-72. [ Links ]
9. Laffler WB. Blepharochalasis: Report of a case this trophoneurosis involving also the upper lip. Cleveland Med. J. 1909;8:131-35. [ Links ]
10. Gomez-Duaso AJ, Seoane J, Vázquez-Garcia J, Arjona C. Sindrome de Ascher reporte de dos casos. J Oral Maxillofac Surg. 1997 Jan.; 55(1): 88-90. [ Links ]
11. Costa-Hanemann JA, et all: Labio doble congénito asociado a hemangiomas: a propósito de un caso. Med. Oral 2004;9:155-8 [ Links ]
12. Gilvani AOC, et all: Síndrome de Ascher: aspectos clínicos y terapéuticos desta rara deformidade da face. Rev. Bras. Cir. Craniomaxilofac. 2008;11(3):116-8. [ Links ]
13. Dalmau J, Puig L, Huevas E, Peramiquel L, Pimentel CL, Alomar A. Blepharochalasia y dos labios: diagnóstico y tratamiento del síndrome de Ascher. J. Eur. Acad Dermatol Venereol. 2006 Nov; 20 (10):1390-1. [ Links ]
14. Reddy KA, Roa AK. A congenital double lip: a review of seven cases. Plast Reconstru. Surg. 1989, 84(3):420-3 [ Links ]
15. Lebuisson D, Leroy L, Aron JJ, Jeaneau E, J. Guillard J P. Síndrome de Laffer-Ascher. Ophtalmol . 1978 Dec. 1 (12) :751-2. [ Links ]
16. Ali K. Ascher syndrome: a case report and review of the literature. Oral surg Oral Med Oral Pathol Oral Radiol. Endod. 2007;103(2):26-8. [ Links ]
17. Franceschetti A. Manifestation the blepharochalasis chez de pére associé á double lévre apparaissant également chez sa fillette agée dún mois. J. Genet Hum. 1955;4:181-2 [ Links ]
18. Narang R. Double lip due to injury. A case report. J Indian Dent Assoc. 1970;42(4):112-3. [ Links ]
19. Rintala AE. Congenital double lip Ascher syndrome: Relationship to the lower lip sinus syndrome. Br J Plast surg 1981; 34:31-4. [ Links ]
20. Swerdloff G. Double lip report of a case. Oral surg Oral Med Oral Pathol. 1960;15:627-9. [ Links ]
21. Dingman RO, Billman H. Double Lip. J Oral Surg 1947; 5: 146-148 [ Links ]
22. Reddy KA, Kotewara A Congenital double lip: a review of seven cases. Plast Reconstr Surg. 1988; 84:420 [ Links ]
23. Dorrance GM. Double Lip Ann Surg 1922 [ Links ]
24. Guerrero Santos J. Altamirano JT, The use of W- plasty for the correction of double lyp deformity. Plast Reconstr Surg 1967; 39:478 [ Links ]
25. Lamster l.B. Mucosal reducción for correction of a maxillary double lip. Report of case. Oral Surg Oral Med Oral Pathol 1983; 55(5) :457-458 [ Links ]
26. Eski M., Nisanci M., Aktas A., Sengezer M. Congenital double lip: review of 5 cases. Br. J. Oral Maxillofac. Surg. 2007;45:68-70. [ Links ]
27. Beinhoff U, Piza-Katzer H. Double lip in a patient with Ascher´s syndrome. Eur. J. Plast Surg.1998;21(7):370-3. [ Links ]
28. Alkan A, Metin M. Doble labio maxilar: presentación de dos casos. J Oral Sci . 2001 Mar; 43 (1):69-72. [ Links ]
29. Chander R, Mal J, Jain A, Jaykar K. Ascher Syndrome: A Case Report. Pediatr. Dermatol. 2009 Sep-Oct; 26 (5) :631-3 [ Links ]
30. Atzeni M, Ceratola E, Zaccheddu E, Manca A, Saba L, Ribuffo D. Corrección quirúrgica y la RM de doble labio en el síndrome de Ascher: registro de un caso y revisión de la literatura. Eur Rev Med Sci. Pharmacol. 2009 Jul-Aug; 13 (4):309. [ Links ]
Received: May 05, 2017; Accepted: December 18, 2017










 text in
text in