Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.20 no.31 Montevideo jun. 2018
https://doi.org/10.22592/ode2018n31a7
Case Report
Multidisciplinary rehabilitation with velopalatal obturator prosthesis: a case report
1 Assistant Professor, Oral and Maxillofacial Prosthesis Service. School of Dentistry, Universidad de la República. Uruguay.
2 Hired Assistant, Oral and Maxillofacial Prosthesis Service. School of Dentistry, Universidad de la República. Uruguay
3 Hired Assistant, Oral and Maxillofacial Prosthesis Service. School of Dentistry, Universidad de la República. Uruguay
A rehabilitation case is presented where the patient suffered a loss of velopalatal tissue following the surgical resection of a soft palate tumor-adenocarcinoma-performed by the multidisciplinary team of the Oral and Maxillofacial Prosthesis Service at the School of Dentistry, Universidad de la República. The care protocol includes the prosthetic rehabilitation and the participation of a speech therapist and a psychologist to provide the comprehensive rehabilitation treatment which is essential in these cases. Different procedures are described, such as clinical stages, laboratory processing, speech therapy records and psychological interviews.
Keywords velopalatal prosthesis; shutter bulb; rehabilitation; multidisciplinary team
Se presenta un caso de rehabilitación, en que el paciente sufrió una pérdida de sustancia velopalatal, por resección quirúrgica de un tumor a nivel del velo del paladar (Adenocarcinoma), abordado por el Equipo Multidisciplinario del Servicio de Prótesis Buco Maxilo Facial (S.P.B.M.F.). Se establece un Protocolo de Atención, que incluye: la labor protésica, de la Fonoaudiología y de la Psicología, para la obtención de un tratamiento rehabilitador integral indispensable en estos casos. Se describen distintos procedimientos realizados tales como: etapas clínicas, etapas de laboratorio, registros fonoaudiológicos y entrevistas psicológicas.
Palabras clave Prótesis velopalatal; bulbo obturador; rehabilitación; equipo multidisciplinario
Introduction
The rehabilitation of a loss of substance in the tissues of the soft palate poses a very specific challenge for the prosthesist and the speech therapist, for they must use a static prosthesis to restore mobile tissues.
This complex problem can be solved in a satisfactory manner with a multidisciplinary approach; it is thus imperative to work with a team of specialized professionals. The Oral and Maxillofacial Prosthesis Service has worked in this way since its creation under the direction of Dr. Isabel Jankielewicz.
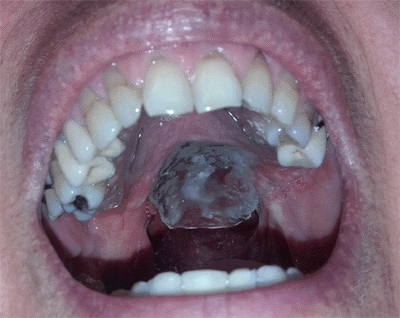
This case presents the complete rehabilitation of an extensive loss of velopalatal tissue as a consequence of the surgical resection of the soft palate to treat a tumor in the salivary gland (polymorphic low-grade adenocarcinoma) in a 61-year-old female patient, a working teacher, who is very self-conscious about her appearance1.
As the patient is an educator, she is considered to be a professional who works with her voice.
Definition
The main aim of the shutter prosthesis (from the Latin verb obturare, shutting, plugging) is to close the existing connection between the oral cavity and the nasal cavity.
Furthermore, the procedure seeks to restore the oral functions which were lost or altered by the lack of palatal tissue, both hard and soft. Said functions include: eating, speech quality, quality of the voice, breathing and hearing, all of which are detailed below.
The velopalatal prosthesis, a variant of the shutter prosthesis, is an anatomical and functional restoration using man-made, alloplastic, inert media, of the loss of tissue involving the soft palate area (velopalatal defects), which may have a congenital or acquired etiology, the latter including trauma and oncological surgery.
Background Michel Benoist describes the work of Ambroise Paré (1517-1590), the first author to describe a palatal shutter, as well as that of Pierre Fauchard (1678-1761), who developed an ingenious shutter design, which was placed in the palatal defects, opening and closing with a butterfly-style device made of silver and gold.
Around 1820, Goodyear vulcanizes rubber, and vulcanite rubber is introduced as a dental material and used to make this kind of shutters. At the same time, there is growing concern over how to combine the prosthesis with speech therapy.
Benoist also notes the work of Suersen (1877), who studied these aspects in depth, describing in his work not only the velopalatal restoration but also the functional nasopharyngeal obturation; as well as that of Claude Martin (1889), who designed velopharyngeal shutters with a double water pocket, a higher and a lower pocket which allow water to circulate from one to the other, accompanying the movement of the soft palate. The appearance of acrylic resin in 1950 made it the material of choice for dental prostheses2.
Regarding the design of velopalatal shutters, Ponroy and Psaume’s articulated shutter has a hinge that articulates the hard palate and the soft palate parts of the prosthesis. The Schiltsky shutter uses a metal guide between the base and the shutter, and the Froschel and Schalit shutter is projected behind and on top of the upper airways (meato-shutter)3..
Classification
According to Alfredo Álvarez Rivero et al. (CIMEQ-CUBA) velopharyngeal shutters can be classified into two groups:
a- Soft palate shutter, velopharyngeal shutter or pharyngeal shutter: designed to follow the curve of the palate, drawing near it and seeking contact to try to shut the velopharyngeal sphyncter.
b- Meatus shutter, differs from the above for it is projected backwards and up, partially shutting the air intake through the nasal cavities (whether perforated or not) improving the voice and preventing the reflux of solid food and liquids4.
Despite the advances in reconstructive surgery, in the cases of extensive loss of tissue in the soft palate, it is not always possible to use the patient's own tissue for the reconstruction. It is therefore necessary to proceed to an anatomical and functional restoration using man-made inert media, alloplastics, prostheses, supplementing surgery and prosthetics, which applies especially to oncological patients.
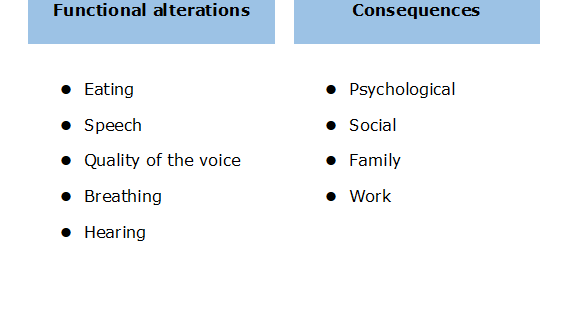
Functional alterations
One of the consequences of the loss of velopalatal tissue is that, as the mouth, nose, and sinuses communicate, it hinders all the functions of the mouth.
Eating: mainly due to the alteration of the oral and pharyngeal swallowing times5. The patient must make remedial movements in the mastication process and when containing the alimentary bolus. In other cases it is necessary to change both the consistency and the viscosity of the food, and the way in which the food is ingested (using a nasogastric tube or a gastrostomy tube in more severe cases).
Speech: it is affected because the patient loses the intraoral points of reference necessary to utter the different phonemes that make up the words. Points of articulation where the tongue makes contact with the palate are lost or altered. This makes the articulation of words blurry, which may lead to unintelligible speech6.
Quality of the voice: (resonance, intensity, duration): the oral and nasal cavities are part of the vocal resonation system, together with the larynx, the pharynx, and the paranasal sinuses. The connection between the oral and nasal cavities gives the voice a hypernasal resonance, also known as rhinolalia aperta. The air and the voice come out through the nasal cavity because the cavity cannot be fully closed, and there is a reduction in intraoral pressure due to the lack of palatal or soft palate tissue7. The intensity of the voice is low and the sounds produced are short.
Breathing: due to the nasal air escape, the patient must inhale more frequently, which modifies the breathing rhythm, so the patient gets more tired when speaking.
Hearing: it is indirectly compromised, since the lowered intraoral pressure does not allow for proper ventilation of the middle ear. After a resection of the soft palate, hearing declines severely because the internal and external stylopharyngeus muscles of the soft palate have been sectioned and removed during surgery. These muscles open and close the pharyngotympanic tube, which balances the air pressure between the middle ear and the outside. This creates mild to moderate conductive hearing loss. Some patients who undergo radiotherapy or chemotherapy lose their sense of hearing as a consequence.
These functional alterations also have psychological, social, family, and work-related impacts on the patient. (Chart 1)
For the velopalatal prosthesis to achieve its aims, it must relate well with the remaining velopalatal or oropharyngeal tissues. The velopalatal defect is not static, on the contrary, the velopalatal region is largely mobile, and it is a juncture between the digestive tract and the respiratory system.
It is therefore essential to record the movements of the surrounding tissues, which are caused by the different functions. This requires special impression techniques which allow the patient to reproduce said movements8.
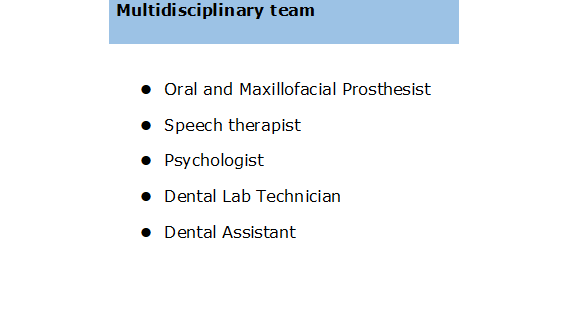
The rehabilitation of patients who receive this kind of prostheses must be conducted by a multidisciplinary team made up of an oral and maxillofacial prosthesist, a speech therapist, a psychologist, a dental lab technician, and a dental assistant9,10.
Materials and methods
- Impression and primary model: A primary, anatomical impression is made using a stock tray for dentulous patients, a distal extension of the same is customized with pink wax in order to include the area where the velopalatal tissue was lost. Alginate is used for the impression, being careful to place a piece of gauze on the surface, of the same size as the velopalatal defect. The main aim of the gauze is to prevent the alginate from going up the upper airways (Fig. 1 and 2).
- Survey: once the primary model has been obtained, a parallelometer is used to survey the teeth and the mucous areas, including the equator of the velopalatal defect. It is essential to survey the mucous areas and the area of the defect, for the size of the input and output shaft for the prosthesis and its corresponding shutter is determined by the hard dental structures, keeping the length of the base and sealing the communication following this axis. The axis for the introduction and removal of the future prosthesis is determined, and the carving of support beds, plans and guiding surfaces for the abutments is planned, all of which will be done in the following clinical session. We decided to make a plaque prosthesis with 0.9 mm stainless steel carved retainers11.
- Individual tray: a unique individual tray is made for the dental and mucous areas; the pyriform papilla and the median raphe are relieved for biological reasons, using pink wax. An individual acrylic tray will be made later, which is loose on the teeth and tight on the mucosa.
- Preparation of the mouth: the planned cutting is done with round and cylindrical diamond burs mounted on a handpiece.
- Impression and final model: the final impression is made with silicone elastomer, and the final survey is made with the final model, for a plaque prosthesis should follow the same guidelines as a cobalt-chromium structured one.
- Preparation of the final model: The retention areas are determined, with a 0.75 mm retentive undercutting to place 0.9 mm stainless steel active arms on pillars 17 and 24.
In plaque prostheses, the reciprocation of the appliance is set on the guiding surface of the lingual sides of the teeth, the guiding planes contributing in a single entry and exit axis. All the retention areas of the teeth as well as the areas which protect the gingival margin must be blocked below the guiding surfaces and planes with plaster of Paris or overlay12. This is an essential step, for these areas should not be filled with an acrylic base; this would hinder the installation of the appliance and its retouching at the clinic, thus losing the corresponding reciprocation. It should be noted that the anatomy of the loss of tissue must always be analyzed in the survey in order to find the equator of the defect, and to make the shutter enter the area with the necessary retentive slope, without injuring the patient when introducing or withdrawing it.
- Final base: the final base technique is applied. The base is made from transparent acrylic based on the model obtained. This provides a stable base for the prosthesis as well as for the tertiary impressions (functional modeling of the velopalatal area).
An omega-shaped 0.9 mm wire loop is made and projected from the distal end of the base of the prosthesis towards the velopalatal area. It will be used for the functional impression of the remaining tissue in the posterior oral sphincter. This is done by the prosthesist together with the speech therapist (see a detailed explanation of the procedure below).
The final base is processed in transparent heat-curing acrylic by means of a muffling process.
Transparent or colorless heat-curing acrylic is chosen because it makes it easy to see the supporting points in the remaining structures, as well as the potential compression areas (Fig. 3 and 4).
A dynamic or functional impression (tertiary impression) is made by requesting the patient to utter certain phonemes, pronounce words or phrases as well as to make swallowing and cervical movements in order to reproduce the missing material following a tumor excision.
The processed prosthetic base is placed in the mouth and the space remaining between the wire omega and the surrounding tissues of the oropharynx are visually assessed. The patient is previously trained by requesting her to move her head to the side and forward towards the chest, to utter phonemes, preferably those which are articulated at the back in isolated syllable combinations, forming words, and associated with simple phrases, together with saliva swallowing movements.
Sealing wax is placed on top of the wire omega, thus creating a first approximate shape of the shutter bulb (Figs. 5 and 6). The next step is to add a regular consistency silicone elastomer. The aim of this particular technique is to record the stylopharyngeus muscles and the superior pharyngeal constrictor muscle (Passavant's ridge).
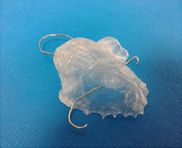
Fig. 5: Processing of the base of the prosthesis. Omega loop made of 0.9 mm wire. (a different angle)
The palate and the tongue are closely linked from the womb; it is thus not difficult to understand the reciprocity between the shape and the function of the oral cavity. Furthermore, as the child acquires language, she acquires the different phonemes in a sort of vocal play, where the tongue is in contact with the other oral components. This is how phonetic engrams and oropharyngeal proprioceptivities are formed and recorded in the brain, together with auditory perception.
Losses or alterations in the mouth after tumor excision alter the sensitivity, the intraoral proprioceptivities, the speech articulation points, the placement of the tongue to swallow, and even the saliva.
The alterations caused by this kind of surgery are manifold: the quality of the voice is altered with a nasal resonance (hypernasal resonance), as is the intensity of the voice (hypophonia), breathing is more frequent, the utterance of language tends to be blurred but not necessarily unintelligible, swallowing and hearing are also altered.
This is why it is so important to act early, resorting to the patient's neuromuscular and auditory memory, providing her with a structure that is as similar as possible to what she had prior to the surgery, allowing for the new intraoral propioception, and facilitating the compensatory maneuvers which occur naturally in the patient.
The selection of phonemes and combinations of phonemes in syllables and phrases for the patient to repeat, and the oral movements that increase intraoral pressure are selected based on the location and the size of the tumor excision and the patient’s possibilities13.
The phonemes used in this case were posterior articulated phonemes /k/, /g/, /x/, combined with the repetition of the vowel sounds /e/, /i/. The transitional phonemes chosen, articulated from the middle to the posterior area of the palate were /tʃ/ and /ɲ/ combined again with the above vowels.
Considering that speech is part of the dynamic communication process, she was asked to repeat words with the phonemes mentioned above.
The functional record is made by the dentist in the presence of the speech therapist. The patient is sitting upright, regular silicone is placed on the wire loop, and with the prosthesis in place, she is asked to utter phonemes, words, and phrases during the active period (vulcanization) of the silicone elastomer (figs. 7 and 8).
The different combinations of phonemes are uttered during the 3:30 minutes it takes the elastomer to be vulcanized, in order to record the different groups of muscles (lingual and pharyngeal).
The patient must be sitting on the dental chair at a 90 degree angle for the dynamic impression, for the normal position we are in when we speak is standing or sitting at the axis of gravity.
The velopalatal section of the prosthesis or the shutter bulb must have the following features:
a) In the silent resting position of the oropharyngeal muscles (while the person breathes) the prosthesis must be separated from the muscles, allowing the air to pass towards the pharynx when breathing through the nose.
b) The oropharyngeal muscles are contracted both when eating and speaking. For these movements, the shutter must touch said structures softly in order not to damage the mucous tissues.
The velopalatal extension of the prosthesis, made based on the records created in the clinic, is created with a mold and a plaster countermold which are connected by means of guides, which reproduce both the nasal side and the mouth side, respectively, and between both peripheral edges of the shutter bulb. This molding chamber is loaded and processed with transparent heat-cured acrylic. The prosthesis must be carefully finished so as not to damage the remaining tissues involved (Fig. 9), both on the oral and the nasal side of the shutter bulb (Fig. 10, 11 and 12).
The prosthesis is finally installed (Fig. 13), with the relevant prosthetic and speech therapy controls14.
The rehabilitation will not be comprehensive if it is not approached from the psychological perspective as well, in which sense, rehabilitation shall be understood as “re-enabling the person, restoring someone back to their previous state”, making reference to the healthcare process aimed at caring for the consequences of an illness or trauma which cause dysfunction or disability, to restore the person back to their social, working, and comprehensive functions.
The psychologist is in charge of seeing the patient through the process of mourning for the body part they lost. This loss or mutilation, whose impact depends on the patient, is also discussed in terms of their fantasies and expectations15.
The psychologist accompanies the elaborate process of coming to terms with the loss. This is not just any loss: the patient has lost a part of herself, which is experienced as an anticipation of death or a loss of integrity.
There are five stages or mourning:
Denial stage: The person protects herself from what has happened, and uses denial as a defense mechanism.
Anger stage: She cannot avoid what happened and this creates discontent. She expresses her anger towards her surroundings or her own self. The fantasies associated to the loss and how the person experiences them will define where she projects her anger. She will look for reasons or people to blame.
Bargaining stage: She tries to negotiate with her environment or with herself, assessing the pros and cons of what happened.
Depression stage: She experiences grief.
Acceptance stage: At this stage, the person accepts that the loss is inevitable16.
A good and healthy mourning process allows the patient to accept the replacement, the prosthesis in this case, as part of her new body image. Raich defines body image as a complex construct which involves the whole body and its parts, as well as the perception of movement and the subjective perception of feelings, thoughts, and appreciations, as well as the way in which the individual behaves in relation to her cognitions and feelings17.
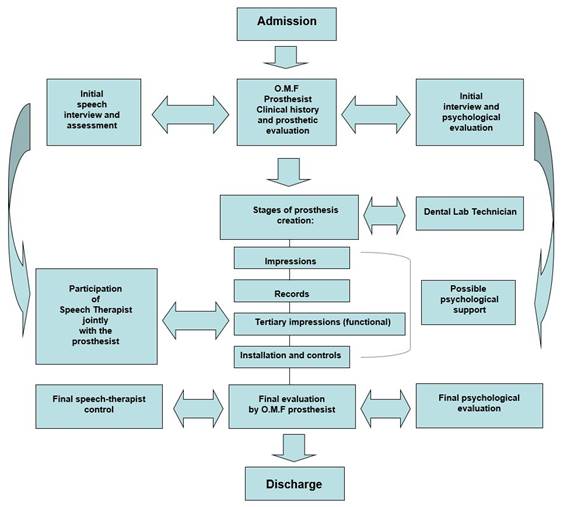
The members of the Oral and Maxillofacial Prosthesis Service team (Chart 2) involved in the resolution of this particular case followed a care protocol that was put together over time in the team’s monthly meetings (R. Soler, oral communication).
This protocol establishes the role played by each one of the professionals, as well as their interaction with the others, at the different stages of the treatment (Chart 3).
The main features of the protocol are as follows:
The treatment plan is put together based on the prosthetic, speech therapy, and psychological assessment.
Essential interaction between the prosthesist and the specialized dental lab technician.
Joint clinical work of the prosthesist and the speech therapist.
Ongoing pshychological assessment.
Joint discharge.
The patient receives a satisfaction survey form to assess the care provided. The form collects the patient’s opinion and that of her friends and family; it is given to the patient at the moment of installation, and she is expected to return it to the team in the subsequent check-up sessions during the adaptation period.
Discussion
The technique applied emphasizes the importance of the functional impression of the remaining tissues of the soft palate with the participation of the speech therapist, thus obtaining a shutter bulb which adapts to the many ways in which these tissues change according to the different functions they perform.
The patient starts working with the speech therapist prior to the surgery. The professional in charge records the patient’s voice and assesses the different functions of the mouth to compare pre-surgery records to post-surgery records.
Once the prosthesis has been made and installed, it will be possible to assess its functional gain by using the speech therapy file to compare the quality of the voice achieved, eating, mastication, speech intelligibility, intraoral pressure (kissing, blowing, whistling, clicking, sucking).
One of the main concerns of the patient, who is a working teacher, was the quality of the voice she would have to use in front of her students18. With this in mind, the team tried to improve the hypernasal resonance, the articulation of words, and to prevent the reflux of food and liquids to the rhinopharynx.
From the prosthetic point of view, the distal extension provided by the velopalatal prosthesis makes it necessary to consider its mechanics. The extension creates additional weight, apart from an inevitable lever arm. For this purpose, the distal section of the prosthetic base must be as light as possible, while providing the highest possible retention.
The height of the palate must follow the curvature of the palatal vault (the tongue has the same mobility); a low palate may trigger the gag reflex and a feeling of a full mouth due to insufficient intraoral space. An average person swallows about 70 times per hour during the day, and produces 1 to 2 liters of saliva per day, which must be swallowed; this must be taken into account for the tertiary impression (dynamic or functional impression).
Finally, all the clinical procedures are carried out with the support of a psychologist, who is one of the first professionals to establish contact with the patient and the case, and is the one that discharges the patient.
Conclusions
Working with a multidisciplinary team helps the patient recover from the aesthetic and functional point of view, as well as in a more comprehensive manner (from the psychological and social perspective), offering her the possibility of going back to work and reactivating family, social, and work relations.
The multidisciplinary team must be in touch with the patient before the surgery, plan a solution for the case with the surgical team and prepare the pre-surgical prosthetic and speech therapy records.
The work of the psychologist is essential not only for the patient but also for the prosthesist, as it will allow him to treat the patient in a more personalized manner.
The prosthesis is designed jointly by the dentist and the speech therapist, and it is assessed by both at the different clinical stages; the patient should be ready to be discharged once she has undergone all the dental, speech therapy, and psychological assessments.
Within this framework, the patient can receive support during the treatment, making it easier for her to express her fears and fantasies, thus allowing her to better accept what happened, taking the person as a bio-psycho-social being.
Referencias
1. Jatin P. Tumores de la cavidad oral. Oncología de Cabeza y cuello. 3era ed. Barcelona: Medicina stm Editores, 2002. p.135 - 45 [ Links ]
2. Benoist M. Pertes de substance des maxillaires. Réhabilitation et Prothese Maxillo Faciales. 1era ed. Michigan: Julien Prelat, 1978. p. 65-132 [ Links ]
3. Psaume M, Ponroy M, Lemaître F. Restauration et prothese maxillo-faciales. 1era ed. Paris: Masson et Cie; 1935. 503p [ Links ]
4. Alonso Travieso ML. (coord.). Procederes clínicos en Prótesis Bucomaxilofacial. CIMEQ. Cuba 2008. [ Links ]
5. Cámpora H, Falduti A. Anatomía y fisiología aplicada a la deglución normal. 1era ed. Buenos Aires: Journal; 2015. p3-25 [ Links ]
6. Turkaslan S, Babykul T, Aydin MA, Ozarslan MM. Articulation performance of patients wearing obturators with different buccal extension designs. Eur J Dent. 2009; 3 (3): 185 - 90. [ Links ]
7. Yoshida H, Furuya Y, Shimodaira K, Kanazawa T, Kataoka R, Takahashi K. Sprectral characteristics of hypernasality in maxillectomy patients. J Oral Rehabil. 2000; 27 (8):723 - 30 [ Links ]
8. Bekerman S. Pacientes maxilectomizados. Enfoque fonoaudiológico. En: Jankielewicz I y co autores. Prótesis Buco Máxilo Facial. 1era ed. Barcelona: Quintessence, 2003. p277 - 281 [ Links ]
9. Fumero M, Wodowóz A, Soler R, Nidegger A. Prótesis Obturatriz, trabajo de equipo multidisciplinario. Rev. Prost.Dent. 1990; 60 (95). [ Links ]
10. Cabrera, C. Rehabilitación Bio Psico Social en Prótesis Buco Maxilo Facial. Servicio de Prótesis Buco Maxilo Facial. Uruguay. Abril 2008. Disponible en: http://odon.edu.uy/bmf/?page_id=495. Citado: 13/03/2017 [ Links ]
11. Bocage M, Feuer L. Planificación. En: Bocage M. Prótesis Parcial Removible. Montevideo: Facultad de Odontología, 2009. p103-155 [ Links ]
12. De Lima J, Cabrera C, Estrada Esquivel B, Sánchez Rubio R, Soler R. Prótesis Parcial Obturatriz Paralelizada en Paciente Oncológico. Odontoestomatología 2015; 17 (25): 42-52 [ Links ]
13. Segre R. Nociones de fonética general y experimental. En: Tratado de foniatría. Trastornos de la voz y del habla y su corrección.1era ed. Buenos Aires: Paidós, 1955. p101 - 28 [ Links ]
14. Arigbede AO, Dosumu OO, Shaba OP, Esan TA. Evaluation of spreech in patients with partial surgically acquired defects: pre and post prosthetic obturation. J Contemp Dent Pract. 2006; 17(1): 89 - 96 [ Links ]
15. Freud S. Duelo y melancolía (1917-1915). En:OBRAS COMPLETAS- Tomo XIV. Buenos Aires- Amorrortu Editores- 1993. p 235-245. [ Links ]
16. Kübler-Ross E. Attitudes Toward Death and Dying. En:On Death and Dying. New York: Scribner, 2014. p.15-123 [ Links ]
17. Raich RM. Una perspectiva desde la psicología de la salud de la imagen corporal. Av. Psicol. Latinoam. 2011; 22 (1): 15-27. [ Links ]
18. Rieger JM, Wolfaardt JF, Jha N, Seikaly H. maxillary obturators: the relationship between patient satisfaction and speech outcome. Head and Neck. 2003; 25 (11): 895-903. [ Links ]
Received: October 26, 2017; Accepted: March 26, 2018











 texto em
texto em