Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.20 no.31 Montevideo jun. 2018
https://doi.org/10.22592/ode2018n31a6
Research
Retrospective clinical study of 656 cast gold inlays/onlays in posterior teeth, in a 5 to 44-year period: Analysis of results
1Postgraduate Degree in Comprehensive Restorative Dentistry, Postgraduate School, School of Dentistry, Universidad de la República, Montevideo, Uruguay.eborgiabotto@gmail.com
2Operative Dentistry Clinical Department, School of Dentistry, Universidad de la República, Montevideo, Uruguay
3Prosthodontics Clinic, School of Dentistry, Universidad de la República, Montevideo, Uruguay
Objective.
1) To assess the clinical performance of 656 cast gold inlay/onlays in a 44-year period; 2) To analyze their indications and distribution regarding the evolution of scientific evidence.
Materials and Methods
. A total of 656 cast gold inlays/onlays had been placed in 100 patients. Out of 2552 registered patients, 210 fulfilled the inclusion criteria. The statistical representative sample was 136 patients; 140 were randomly selected and 138 were the patients studied. Twelve variables were analyzed. Data processing was done using Epidat 3.1 and SPPS software 13.0.
Results.
At the clinical examination, 536 (81.7%) were still in function and 120 (18.3%) had failed. According to Kaplan-Meier’s method, the estimated mean survival for the whole sample was 77.4% at 39 years and 10 months.
Conclusions.
Knowledge updating is an ethical responsibility of professionals, which will allow them to introduce conceptual and clinical changes that consider new scientific evidence.
Keywords: inlays/onlays; molar; premolar; dental bonding restorations; scientific evidence-based research; minimally invasive dentistry
Objetivos.
1) Evaluar el rendimiento clínico de las restauraciones posteriores de oro, durante 44 años; 2) Analizar su indicación y distribución, en relación con la evolución de la evidencia científica.
Materiales y Métodos
. En 100 pacientes, se estudiaron 656 restauraciones posteriores de oro colado. De 2552 pacientes registrados, 210 cumplieron los requisitos de inclusión. La muestra estadística representativa fue de 136 pacientes. Se seleccionaron al azar 140 y se estudiaron 138. Doce variables fueron analizadas. El procesamiento de datos se realizó con el software Epidat, versión 3.1 y del software SPSS versión 13.0.
Resultados.
Estaban en función 536 (81.7%) y 120 (18.3%) fracasaron. Según el Método de Kaplan-Meier, la sobrevida total estimada fue de 77.4% a los 39 años y 10 meses.
Conclusiones.
La constante actualización del conocimiento, responsabilidad ética del profesional, le permitirá introducir los cambios conceptuales y clínicos a la luz de las nuevas evidencias científicas.
Palabras Claves: incrustaciones intracoronarias; molar; premolar; evidencia científica; restauraciones adheridas; operatoria dental mínimamente invasiva
Introduction
Restorations in posterior teeth, mainly molars, withstand the greatest occlusal forces. Moreover, 40% greater forces could be observed in patients with bruxism, increasing their risk of failure1. Additionally, restorations covering more surfaces have had greater risk of failure2. For over 100 years, cast gold restorations have been widely used, mainly in posterior teeth. Several clinical studies show excellent quality, longevity and functional performance3-6.
Since the beginning of the nineties there has been a permanent scientific and technological development of adhesive ceramic materials for posterior inlays/onlays. Clinical studies and systematic reviews have shown very good results7-12. Moreover, improving biomechanical and optical properties in direct light-activated composite resins13-18, as well as in the adhesive systems19-22 has increased their use23-24, showing high long-term clinical success, performing extended and large restorations in posterior teeth25-32. This scientific evidence has provided the basis for using these materials as substitutes of cast gold restorations.
At the same time, cultural, sociological and psychological factors related to self-esteem33 and new aesthetic parameters34-36 have increased patients’ demand for tooth-colored restorations.
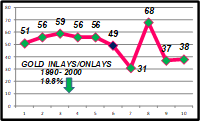
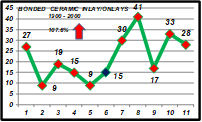
All the above can change concepts and clinical procedures, leading to a reduction in the indication and placement of cast gold inlays/onlays. These changes were observed in productivity studies conducted by the operator in his private office in over 25 years. In fact, between 1995 and 2000 there was a 19.8% decrease in the use of gold inlays/onlays (GIOs) (Fig. 1), an increase of 107.6% in the placement of bonded ceramic inlays/onlays (BCIOs) (Fig. 2) as well as a 44.7% increase in posterior direct light-activated composite resins (PCRs) (Fig. 3).
The right selection and the proper handling of the new materials are possible if the professional’s knowledge is scientific and evidence-based. In fact, it is an ethical responsibility.
Therefore the aims of this article were: 1) to assess the clinical performance of 656 cast gold inlay/onlays in a 44-year period, and 2) to analyze their indications and distribution in relation to the evolution of scientific evidence.
Materials y Methods
This work was approved by the Ethical Board of the School of Dentistry, Universidad de la República.
From April 2013, a retrospective clinical longitudinal study on six restorative procedures, performed by the first author in his private practice, has been conducted covering a 44-year period. Four articles have been published12,32,37,38. This paper presents the results of a new study in the series.
To be included in the study, the patients must have been treated and evaluated in the first author’s office for at least seven years and be still in the practice by 2013, with complete dental arches (healthy or restored teeth). The patients with removable dental prosthesis, disabilities, that had moved or passed away were excluded.
The GIOs must have been in function for at least five years to be included in the study. The failure criteria were: loosening, removal of the restoration or tooth lost.
Out of 2552 registered patients, 210 fulfilled the inclusion criteria and 136 patients were a statistically representative sample (at the lowest range, a 95% CI for a proportion, with a length of ± 5%). Of these 210 patients, 140 were selected at random by a dental assistant, who was blinded to the aim of the selection. They were invited to participate in clinical examinations between November 2013 and April 2014: 138 agreed to participate.
Considering the period of the clinical examination (11/2013 - 04/2014), the inclusion criteria for the GIO (> 5 years in function), and the second aim of this research, the restorations to be analyzed were divided into two groups, according to the date of placement: A - between April 1969 and April 1991, and B - between April 1991 and October 2008.
According to the Glossary of Prosthodontics Terms39, the meaning of inlay and onlay terms were slighty modified in this work for practical reasons: “inlay” is when the GIO covers partially the occlusal surface, including one or more cusps; “onlay” when the GIO covers the whole occlusal surface.
Patient-based data were collected from the clinical personal charts and clinical examinations for each patient, and then recorded on specially designed sheet forms.
All restorations were made by the first author. The co-authors participated as independent evaluators. The calibration between the authors was undertaken previously on 120 restorative procedures from outside the sample. Cohen’s Kappa Coefficient on the quality of restorations ranged from 0.78 to 1 (excellent according to Fleiss’s guidelines).
To establish the quality of the restorations, marginal adaptation (MA), marginal discoloration (MD), and occlusal surfaces (S) were the variables evaluated according to Ryge’s criteria40) ; however, these variables were modified by the authors (Table 1).
As was previously published32, four success criteria (SC) were established on the quality of the GIOs:
- Excellent (Ex): When MA, MD, and S were rated “Alpha” in the same GIO. This group represents the best quality restorations.
- Good (G): When at least one variable (MA, MD, S) was rated “Bravo” in the same GIO. This group was considered of satisfactory clinical acceptance.
- Functional survival (FS): When at least one variable (MA, MD, S) was rated “Charlie” in the same GIO. These restorations must be controlled, repaired or retreated.
- Clinically successful (CS): To establish clinical success, the GIOs in function rated “Excellent” and “Good”, were considered jointly.
Table 1: Ryge’s criteria(40), modified by the authors, to establish the quality of GIOs.
| MARGINAL ADAPTATION |
| Alpha: No lack of continuity along the margin observed with the explorer. |
| Bravo: Evidence of a crevice along the margin, but the explorer cannot penetrate. |
| Charlie: Evidence of a crevice along the margin, which an explorer can penetrate. Requires control, repair or retreatment. |
| MARGINAL DISCOLORATION |
| Alpha: No pigmentation anywhere on the margin. |
| Bravo: Pigmentation present but does not penetrate the margin toward the pulp. |
| Charlie: Severe pigmentation. The restoration must be removed. |
| SURFACE |
| Alpha: The surface of the restoration is unaltered. |
| Bravo: The surface of the restoration shows wear and must be controlled. |
| Charlie: The surface of the restoration shows perforations, fractures or significant tear. It must be polished, repaired or retreated. |
Patients signed an informed consent before the clinical examination. The clinical exams were blinded among the authors and performed with a mirror and a sharp explorer (Maillefer 6: Maillefer, Ballalgues, Switzerland). In cases of disagreement regarding the assessment of the quality of the restorations, the lowest rating was recorded.
The operator always conducted a clinical and functional study of the Stomatognathic System (SE). These data, as well as the clinical procedures performed, the materials applied and the patient’s biological response were thoroughly recorded.
Since its availability in the market, a panoramic radiograph was always indicated. When restorations, carious lesions and/or periodontal disease were present, standard X-rays were requested.
All the patients were enrolled in a comprehensive prevention plan and advised to undergo periodical maintenance therapy. Since the late eighties, if caries disease was present, biochemical and microbiological saliva tests were indicated and a dietary form filled. The aim was to establish the individual caries risk and to implement the specific etiological treatments41-44. Furthermore, non-cavitated carious lesions were treated with topical fluorides.
Tooth preparation is considered by the operator as the most important factor in the clinical success of the restorative treatment. It must be based on a conservative approach, according to the extension of the carious lesion, remnant tooth structure, location of occlusal contacts, crown height, occlusal plane, habits of the patient, biomechanical properties of the restorative materials and aesthetic considerations. In deep cavities, a thin layer of self-cured calcium hydroxide was applied in the pulpal wall and covered with glass-ionomer cement.
The variables analyzed were age, gender, type of restoration, number, location, extension, quality and longevity of the restorations, type of cement, secondary caries, parafunctional habits and maintenance therapy.
Data processing was performed using Epidat software (Conselleria de Sanidade de la Xunta de Galicia, Santiago de Compostela, Spain) v 3.1 developed by the Consellería de Sanidade de la Xunta de Galicia with the support of PAHO-WHO and SPSS software v13.0 (SPSS Inc., Chicago, IL). In all cases, the variables considered corresponded to an identically distributed independent random variable that was generated from a probability sample. A result was considered statistically relevant when, upon the rejection of a null hypothesis, the probability of error was less than 5%. Statistical significance was set at P < 0.05. When analyzing the complete and censored values, the mean and median values were used to describe the central tendency. If the number of complete values was too small, a Kaplan-Meier’s curve could not be used. Therefore, a Fisher’s exact test, Chi-square test, Kruskal-Wallis test, and Mann-Whitney non-parametric test could be indicated to analyze significant differences.
Results
Six hundred and fifty-six GIOs had been placed in 100 patients. The observed mean age was 63 years and 9 months for both sexes. The observed mean time of attendance per patient was 30 years and 5 months.
Carious lesions 557, endodontic treatment 85, functional requirements 7, trauma 4 and periodontal disease 3 were the reasons to perform the GIOs.
The number of GIOs per patient varied from 1 to 20. The average was 6.56 GIOs per patient: 6.22 in women and 7.07 in men. No statistical significant difference was found regarding sex (Mann-Whitney Test, p = 0.92).
GIOs in function and failed
At clinical examination, 536 GIOs (81.7%) were in function. The observed mean survival (OMS) was 27 years and 1 month. According to the date of placement, 343 were in group A- and 193 in Group B-.
One hundred and twenty GIOs failed (18.3%), 61 in 16 men and 59 in 17 women; 119 in Group A- and 1 in Group B-. The OMS for failures was 18 years and 4 months. No statistically significant differences between the IOOs in function (Student T Test, p = 0.65), nor in the failures (Student T Test, p = 0.99) were observed in both sexes.
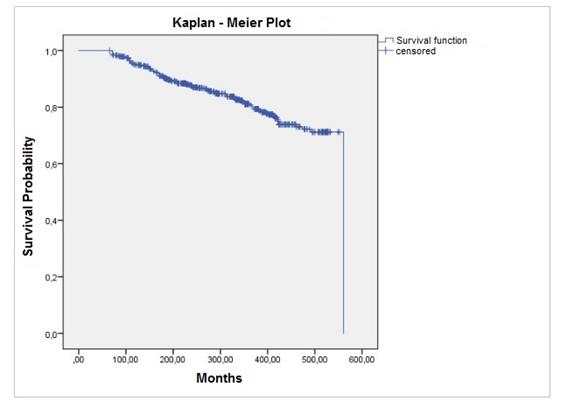
The annual failure rate was 0.08%. The estimated mean survival time (EMS), according to the Kaplan-Meier’s method, was 85% at 25 years and 77.4% at 39 years and 10 months (Fig.4).
Considering location, 331 GIOs in function were in molars and 205 in premolars. There was a statistically significant difference in the number of GIOs in function, restoring molars and premolars, between the two groups (OR = 0.42, p < 0.001) (Fig. 5).
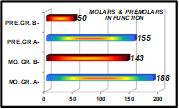
Fig. 5: Distribution and number of GIOs in function in molars and premolars in both groups (MO. =molars; PRE. = premolars; GR. = group).
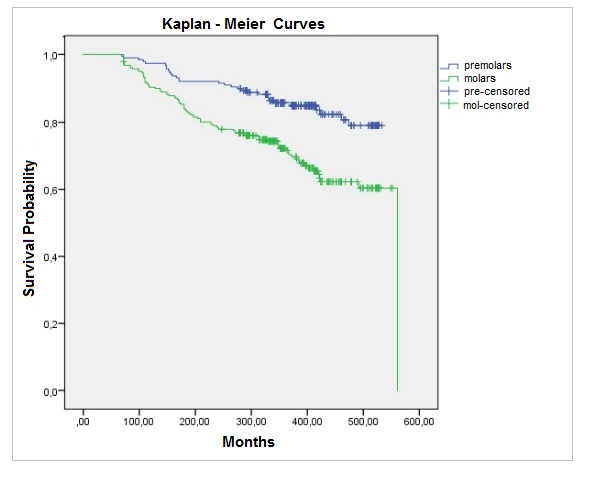
Out of 120 failures, 89 were in molars and 31 in premolars. Premolar survival was significantly higher (Log Rank Test, p < 0.0001). According to Kaplan-Meier’s method, EMS was 479.8 months (39 years and 11 months) for premolars and 437.4 months (35 years and 5 months) for molars (Fig. 6).
Regarding type of restoration, 424 GIOs were onlays and 112 inlays. A statistically significant difference was observed in the number of onlays and inlays in function between the two groups (OR = 13.9, p < 0.0001). Thirty-eight onlays and 82 inlays failed. Onlays presented a higher statistical survival rate (Log Rank Test, p < 0.0001). The Kaplan-Meier’s curves showed an EMS of 498.4 months (41 years and 6 months) for onlays and 402.2 months (33 years and 6 months) for inlays (Fig.7).
Considering extension, 95% of the all GIOs, covered 3 surfaces: 507 in function and 116 failures; 20 covered 2 surfaces (4 failures) and 13 more than 3 surfaces.
Regarding pulp state at the moment of placement, 86.6% of the GIOs, restored vital teeth (VT): 457 in function and 111 failed. Out of 88 (13.4%) endodontically treated teeth (ETT), 79 remained in function and 9 restored with casts posts failed, but only one was fractured. Furthermore, 9 GIOs in VT had to be removed for endodontic treatment (1.4%).
Three GIOs were fixed with resin cement (Panavia, Kuraray, Japan) and 653 with zinc phosphate cement. One GIO fixed with zinc phosphate cement loosened after 32 years in function.
Secondary caries was the major reason for failures (14.9%): 89 in occlusal surfaces and 9 in gingival location. Of the 120 failures, 15 teeth (14 in group A and 1 in group B) were lost.
Table 2 summarizes the information on failures presented above.
In addition, 105 teeth in group A-, that had lost their GIOs could be retreated: 90 with new GIOs, that were included in this study, and 15 with other restorative procedures. Out of 90 GIOs (89 onlays and 1 inlay), 39 were retreated before April 1991, remaining in group A. Fifty one performed after April 1991 were included in group B- .
Table 2
| PERIOD | O/C | G/C | End. | Perio. | Fra. | Loos. | R.R. | TOTAL |
| < 10 y | 24 | 3 | 2 | 1 | 1 | 0 | 1 | 32 |
| 10 - 20 y | 34 | 1 | 3 | 4 | 0 | 0 | 1 | 43 |
| 20 - 30 y | 21 | 0 | 4 | 1 | 0 | 0 | 0 | 26 |
| 30 - 40 y | 10 | 3 | 0 | 3 | 0 | 1 | 0 | 17 |
| > 40 y | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| TOTAL | 89 | 9 | 9 | 9 | 1 | 1 | 2 | 120 |
| % | 74.2 | 7.5 | 7.5 | 7.5 | 0.8 | 0.8 | 1.7 | 100 |
Failures of GIOs: causes, number, distribution in decades and percentages (O/C = occlusal caries; G/C = gingival caries; End.= endodontic treatement; Perio.= periodontal disease; Fra.= root fracture; Loos. = loosened; R.R.= rooth resorption; y = year).
Meanwhile, group B- included 194 GIOs placed after April 1991 (193 in function, 1 failure). The distribution of the 193 GIOs in function was: 48 in 22 patients that had not been in group A-; the above mentioned 51 GIOs retreated, and the 94 new GIOs placed in 62 patients in group A- (Table 3).
Table 3
| PERÍOD | Gr. B | Gr. A/B | RETR. | TOTAL |
| 04/91 - 04/95 | 9 | 35 | 19 | 63 |
| 04/95 - 04/99 | 15 | 29 | 18 | 62 |
| 04/99 - 04/04 | 12 | 18 | 8 | 38 |
| 04/04 - 10/08 | 12 | 12 | 6 | 30 |
| TOTAL | 48 | 94 | 51 | 193 |
Success criteria
According to Ryge’s criteria40 modified by the authors, the results on the quality of the variables analyzed are presented in Table 4. Considering these results, and the previous established criteria32, the CS of the GIOs in function was 93.6%. The CS for the whole sample was 76.1%.
Table 4 Number, distribution and quality of the variables analyzed, according to Ryge’s criteria40 modified by the authors.
| MARGINAL ADAPTATION | MARGINAL DISCOLORATION | OCCLUSAL SURFACE | |
| ALPHA | 390 | 533 | 465 |
| BRAVO | 129 | 2 | 50 |
| CHARLIE | 17 | 1 | 21 |
Three GIOs in Figure 8 were qualified Ex, and 2 in Figure 9 were qualified B. The GIOs repaired in Figure 10 were qualified as FS.
Occlusal function and maintenance.
Twenty-four patients (24%) had had history of parafunction, and 33 (33%) were using stabilization occlusal splints due to bruxism. Thirty-seven patients (37%), 21 women and 16 men, attended at least once a year for maintenance therapy.
Repairs
Meanwhile, in 21 patients, 27 repairs were performed (23 in occlusal and 4 in gingival areas). The materials applied were Direct Light-activated Composite Resin 20, Glass-Ionomer 1 and Amalgam 6. These GIOs were considered in function and qualified as functional survival. The OMS of the repairs was 12 years and 8 months (range: 3 years to 22 years and 9 months). Two GIOs repaired are shown in Figure 10.
Discussion
The high percentage of GIOs in function (81.7%) and their EMS were in line with other clinical studies3,4,6. Regarding statistical data previously presented in this paper, the variables age and gender did not influence the results. Secondary caries were 81.7% of the all failures, higher than in other studies: 33.7%3) and 40%4.
Occlusal carious lesions could be related to biomechanical factors associated with bruxism (marginal and/or surface wear of GIO, cement dissolution), biological factor (bacterial microfiltration) and the lack of periodic maintenance control. Besides, the operator, according to the minimal invasive criteria, preferred to repair before retreating. This agrees with Fisher and Morgan WW45. The fact that 63% of the patients did not attend at least once a year for maintenance therapy could be considered a biological and biomechanical risk factor for failure. Furthermore, parafunction might be a biomechanical risk factor of failure.
Only one GIO loosened (0.15%). This result was very low compared to other clinical studies: 32.7%3) and 31%4. This could be due to the design of the tooth preparation, the quality of the restoration and a thorough fixation protocol by the operator.
The higher survival of premolars is in line with other studies1,2. Meanwhile, the higher survival of onlays could be explained because onlays transmit mainly compressive forces, giving better protection to the remnant tooth structure46,47. Besides, due to the extension, their margins could be less affected by the greater forces exerted in patients with bruxism. In addition, Studer et al.4 did not find differences between inlays and onlays. The CS of the GIOs in function was 93.6%, in line with Donovan and Chee5 and Donovan T et al.6. The development above supports the first objective of this work.
The second aim of this study was to analyze the indication and distribution of GIOs, related to the new scientific evidence. Therefore, both groups must be compared to analyze the constitution of Group B- and to assess the possible coexistence of restorations as substitutes of the GIOs.
In fact, the number of GIOs in function in Group B- (193) was 43.7% less than in Group A-. These patients had been using GIOs for a long time, they knew their results and did not refuse to use gold restorations. Nevertheless, when analyzing Table 3, 32.1% of GIOs were placed in the “transitional period” (1995-1999), 19.7% and 15.6% in the two following periods, respectively. This gradual and constant reduction in the use of GIOs might be due to alternative restorative procedures proposed by the operator.
Using the same global sample, similar inclusion end exclusion criteria than in this work, and relative similar period of placement than restorations in Group B-, in two articles published by the authors12,32 the following was studied:
- 93 IOCAs in 47 patients, placed between 10/1995 - 10/2008 and assessed in a 5 to 18 - year period. Eighty-seven onlays (93.5%) remained in function12.
- 105 RCDPs in 61 patients were installed between 10/1993 - 10/2008 and assessed in a 5 to 20-year period; 103 (98%) were in function and 41% were large or extended restorations32.
Therefore, in the 04/1991 - 10/2008 period, in the same global sample, 50.4% of the partial posterior restorations performed were GIOs and 49.6% RCDPs or IOCAs. Meanwhile, comparing the two groups, in Group B- we observed a reduction of 94.3% and 67.7% in the number of inlays and premolars restored with GIOs, respectively. This could be due to the application of more conservative, aesthetic and efficient restorative materials such as RCDPs.
Besides, the reduction of onlays (21.1%) in Group B-, might be linked to greater use of IOCAs. Whereas in Group B-, only one GIO failed due to periodontal problems. This result could be due to the scientific and clinical changes related to the new preventive actions taken by the operator41-44.
Considering all the above, besides the very good clinical results, this work also showed a close connection between the clinical and conceptual changes applied by the operator and the updated scientific evidence.
Only one operator can reduce bias in the analytical comparison, but might improve the clinical success48. The results could not be reproducible, but the operator believes this could be a relative limitation49.
Conclusions
In this study, a high clinical performance of GIOs was observed. However, as there are more aesthetic restorative materials, with good longevity and requiring simpler and less invasive teeth preparations, GIOs are less indicated by dentists and less accepted by patients.
Updated knowledge is an ethical responsibility of the professional. It will allow dentists to introduce the clinical and conceptual changes, taking into consideration the new scientific evidence, as was observed in this paper.
Referencias
1. Arlan CV, Dimitriu B, Arlan VV, Bodnar D, Suciu I. Current opinions concerning the restoration of endodontically treated teeth: basic principles. J Med Life 2009;15:165-172. [ Links ]
2. Demarco FF, Corrêa MB, Cenci MS, et al. Longevity of posterior composite restorations: Not only a matter of materials. Dent Mater 2012;28:87-101. [ Links ]
3. Stoll R, Sieweke M, Pieper K, Stachniss V, Schulte A. Longevity of cast gold inlays and partial crowns--a retrospective study at a dental school. Clin Oral Investig. 1999;2:100-104. [ Links ]
4. Studer SP, Wettstein F, Lehner C, Zullo TG, Schärer P. Long-term survival estimates of cast gold inlays and onlays with their analysis of failures. J Oral Rehabil. 2000;6:461-472. [ Links ]
5. Donovan T.E., Chee W.W.- Conservative indirect restorations for posterior teeth. Cast versus bonded ceramic. Dent Clin North Am. 1993;3:433-443. [ Links ]
6. Donovan T., Simonsen R.J., Guertin G., Tucker R.V.- Retrospective clinical evaluation of 1314 cast gold restorations in service from 1 to 52 years. J Esthet Restor Dent. 2004;3:194-204. [ Links ]
7. Beier US, Kapferer I, Burtscher D, GIesinger JM, Dumfahrt H. Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth. Int J Prosthodont 2012;25: 395-402. [ Links ]
8. van Dijken JW, Hasseirot L. A prospective 15-year evaluation of extensive dentin-enamel-bonding pressed ceramic coverages. Dent Mater 2010; 26: 929-939. [ Links ]
9. Guess PC, Selz CF, Steinhart YN, Stampf S, Strub JR. Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7 year results. Int J Prosthodont 2013;26:21-25. [ Links ]
10. Santos MJ, Mondelli RF, Navarro MF, Francischone CE, Rubo JH, Santos GC Jr. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: five-year follow-up. Oper Dent 2013;38:3-11. [ Links ]
11. Freire Y, Gonzalo E, Lopez-Suarez C, Suarez MJ. The marginal fit of CAD-CAM monolithic ceramic and metal-ceramic crowns. J Prosthodont. 2017,doi: 10.1111/jopr.12590. [ Links ]
12. Borgia E, Baron R, Borgia JL. Clinical performance of bonded ceramic inlays/onlays: A 5- to 18-year retrospective longitudinal study. Am J Dent. 2016;29:187-192. [ Links ]
13. Rubinstein S, Nidetz A. The art and science of the direct posterior restoration: recreating form, color and translucency. Aloha Omegan 2007;100:30-35. [ Links ]
14. Illie N, Hickel R, Valceanu AS, et al. Fracture toughness of dental restorative materials. Clin Oral Investig. 2012,16:489-498. [ Links ]
15. Sripetchdanond J, Leevailoi C. Wear of human enamel opposing monolithic zirconia, glass ceramic and composite resin: an in vitro study. J Prosthet Dent. 2014;112:1141-1150. [ Links ]
16. Belli R, Geinzer E, Muschweck A, et al. Mechanical fatigue degradation of ceramics versus resin composites for dental restorations. Dent Mater. 2014;30:424-432. [ Links ]
17. Perdigão J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater 2010;26:24-37. [ Links ]
18. Brackett MG, Li N, Brackett WW, et al. The critical barrier to progress in dentine bonding with the etch-and-rinse technique. J Dent 2011;39:238-248. [ Links ]
19. Liu Y, Tjäderhane L, Breschi L. et al. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J Dent Res. 2011;8:953-968. [ Links ]
20. Peumans M, De Munck J, Mine A. et al. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent Mater. 2014;10:1089-1103 [ Links ]
21. Ozer F, Blatz MB. Self-etch and etch-and-rinse adhesive systems in clinical dentistry. Compend Contin Educ Dent. 2013;1:12-14. [ Links ]
22. Mahn E, Rousson V, Heintze S. Meta-Analysis of the influence of bonding parameters on clinical outcome of tooth-colored cervical restorations. J Adhes Dent. 2015;5:391-403. [ Links ]
23. Lynch CD, Frazier KB, McConnell RJ et al. Minimally invasive management of dental caries: contemporary teaching of posterior resin-based composite placement in U.S. and Canadian dental schools. J Am Dent Assoc. 2011;142:612-620. [ Links ]
24. Nascimento GG, Correa MB, Opdam N et al. Do clinical experience time and postgraduate training influence the choice of materials for posterior restorations? Results of a survey with Brazilian general dentists. Braz Dent J 2013;6:642-646. [ Links ]
25. Opdam NJ, van de Sande FH, Bronkhorst E, et al. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res 2014;93:943-949. [ Links ]
26. Heinze SD, Rousson V. Clinical effectiveness of direct class II restorations-a metanalysis. J Adhes Dent 2012;14:407-431. [ Links ]
27. van Dijken JW, Pallessen U. A randomized 10-year prospective follow-up of Class II nanohybrid and conventional hybrid resin composite restorations. J Adhes Dent 2014;16:585-592. [ Links ]
28. da Rosa Rodolpho PA, Donassollo TA, Cenci MS, et al. 22-year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent Mater 2011;27:955-963. [ Links ]
29. van de Sande FH, Opdam NJ, Rodolpho PA, et al. Patient risk factors apos; influence on survival of posterior composites. J Dent Res 2013;92 (Suppl):78S-83S. [ Links ]
30. Laegreid T, Gjerdet NR, Johansson AK. Extensive composite molar restorations: 3 years clinical evaluation. Acta Odontol Scand 2012;70:344-352. [ Links ]
31. Beck F, Lettner S, Graf A, et al. Survival of direct resin restorations in posterior teeth within a 19-year period (1996-2015): A meta-analysis of prospective studies. Dent Mater. 2015;31:958-985. [ Links ]
32. Borgia E, Baron R, Borgia JL. Quality and survival of direct light-activated composite resin restorations in posterior teeth: A 5- to 20-year retrospective longitudinal study. J Prosthodont.2017 (ahead of print), doi: 10.1111/jopr.12630. [ Links ]
33. Patzer G. Understanding the causal relationship between physical atractiveness and self- esteem. J Esthet Dent 1996;3:144-147. [ Links ]
34. Bauer J, Vasilache I, Schlegel AK, et al. Esthetics and Psyque-Part 1: Assessment of the influence of patient apos; perceptions of body image and body experience on selection of existing natural tooth color. Int J Prosthodont 2012;25:36-43 [ Links ]
35. Witt M, Flores-Mir C. Laypeople preferences regarding frontal dentofacial esthetics: periodontal factors. J Am Dent Assoc 2011;142:925-937. [ Links ]
36. Gul-e-Erum, Fida M.- Changes in smile parameters as perceived by orthodontists, dentists, artists, and laypeople. World J Orthod. 2008;9:132-140 [ Links ]
37. Borgia E, Barón R, Borgia, J L. Cast posts: a forty-four year retrospective clinical study in a specialized private practice. Odontoestomatología 2015;25: 11-22. Available from: http://www.scielo.edu.uy/pdf/ode/v17n25/en_v17n25a03.pdf [ Links ]
38. Borgia E, Barón R, Borgia JL. Endocrowns: A retrospective patient series study, in a 8 to 19-year period. Odontoestomatología; 2016;28: 45-59. Available from: http://www.scielo.edu.uy/pdf/ode/v18n28/en_v18n28a07.pdf [ Links ]
39. The Glossary of Prosthodontic Term. J Prosthet Dent. 2005; 1:10-85. [ Links ]
40. Ryge G. Clinical criteria. Int Dent J 1980;30:347-358. [ Links ]
41. Axelsson P, Lindhe J. Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. Results after 6 years. J Clin Periodontol 1981;3:239-248. [ Links ]
42. Krasse Bo. Caries Risk: A practical guide for assessment and control. Introduction to Chapter 14. Quintessence Publishing, Chicago,Illinois, 1985:11-96. [ Links ]
43. Emilson CG. Effect of chlorhexidine gel treatment on Streptococcus mutans population in human saliva and dental plaque. Scand J Dent Res 1981; 89:239-246. [ Links ]
44. Maltz M, Zickert I, Krasse B. Effect of intensive treatment with chlorhexidine on number of Streptococcus mutans in saliva. Scand J Dent Res 1981; 89:445-449. [ Links ]
45. Fisher DW, Morgan WW. Modification and preservation of existing dental restorations. Chicago: Quintessence, 1987; Chapter 1:15-28 [ Links ]
46. Kois DE, Isvilanonda V, Chaiyabutr Y, Kois JC. Evaluation of fracture resistance and failure risks of posterior partial coverage restorations. J Esthet Rest Dent, 2013;25:110-122. [ Links ]
47. Laegreid T, Gjerdet NR, Johansson A, Johansson A-K. Clinical decision making on extensive molar restorations. Oper Dent 2014;6:231-240. [ Links ]
48. Frankenberger R, Reinelt C, Petschelt A, Krämer N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent Mater 2009;25:960-968. [ Links ]
49. Borgia E. On Knowledge Update in Planning Comprehensive Dental Treatment: A Personal Overview. Int J Prosthodont. 2017;1:11-12. [ Links ]
Received: April 13, 2017; Accepted: February 06, 2018











 texto em
texto em