Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.19 no.spe Montevideo set. 2017
https://doi.org/10.22592/ode2017n.esp.p34
Articles
Workshop 4 - Challenges of implant-supported rehabilitation in the aesthetic area
1 Cátedra de Rehabilitación, Prostodoncia Fija y TTM. Facultad de Odontología. Universidad de la República, Uruguay. angelmangarelli@gmail.com
2 Cátedra de Rehabilitación, Prostodoncia Fija y TTM. Facultad de Odontología. Universidad de la República, Uruguay.
3 Facultad de Odontología, Universidad de la República, Uruguay.
Abstract: The constant evolution of Implantology in recent years has made osseointegrated implant an effective and safe anchorage for buco-maxillof-facial prostheses. The high success rates, whice arise from clinical studies, confirm tha osseointegrated implants are the treament of choice for certain patients. The objective of this work is the presentation of a clinical case, in which oral implants were installed, to anchor an orbital prosthesis. The patient was atended in the Faculty of Dentistry of the Universidad de la República, in the Service of Prosthesis Buco Maxillo Facial, in conjunction with the Department of Oral and Maxillofacial Implantology
Introduction
The outcomes of the practice of replacing missing dental organs with implants have reached such a degree of universalization and certainty1 that it has become an everyday tool in the clinical practice. Nevertheless, the better outcomes brought about greater demands from patients and also from professionals, who strive to reach dental aesthetics and, especially, the gingival aesthetics of natural teeth.
Achieving pleasing gingival aesthetics in teeth restored with implants has proven the main challenge to address in this branch of the profession. The literature review on this subject matter to be discussed in a workshop environment, aiming towards a consensus, was designed to make a contribution in this area.
Workshop methodology. The workshop was structured in the following stages:
- Literature review. The people leading the seminar accessed the Timbó, Pubmed, Medline and Lilacs portals, reviewed the literature of the last ten years, and selected 23 studies, all of them conducted on humans, considered to be representative of the topic under discussion.
- Guiding questions. Four guiding questions representing the subject matter of the seminar and the literature selected were formulated. The questions were:
1. What are the causes of gingival recession?
2. How important is the management of the provisional restoration in shaping peri-implant tissues in the aesthetic area?
3. What is considered optimal management of abutments regarding design, materials and aesthetics?
4. What aesthetic evaluation indices are there?
- Discussion with workshop participants. The selected literature and the guiding questions for discussion were emailed to participants for them to read and evaluate, and they were invited to two prior meetings to begin the scientific exchange.
- Scientific review. It was decided that a scientific reviewer should be present at the workshop without participating in the discussion. He would evaluate the quality of the suggested literature, the representativeness of the guiding questions, the scientific level reached during the discussion on the day of the seminar, and the connection between the conclusions of the seminar and the guiding questions and bibliography.
Workshop participants. The following professionals attended the workshop: Drs. Javier Trinidad, Enrique Elhordoy, Mariana Seoane, Natalia Panissa, Viviana Rocha, Sergio Montenegro, Carla Laurino, David Durán, Fernando Indart, and Susana Borrás.
Workshop.
Question No. 1. What are the causes of gingival recession linked to dental implants? In the workshop it was determined that gingival recession is associated to the following kinds of factors: A) Intrinsic (related to the patient) and B) Extrinsic (related to technical aspects), and that they are probably closely related to each other.
A. Intrinsic factors
A.1. Complete or partial absence of the vestibular table at the time of implant placement. The evidence from the literature consistently indicates that the risk of gingival recession in these cases is very high. Placing implants in sites with vestibular bone defects frequently leads to soft-tissue recession, with the potential risk of altering the harmony of the gingival margin2,3. In this situation, it is recommended to delay implant placement. In a literature review, Chen (2009) (4) concluded that regeneration procedures are effective in reconstructing defects in the vestibular table, in type 1 (immediate placement) and type 2 (early placement) implant placement situations. Despite this, less vestibular bone loss was observed with type 1, which has consequences in the aesthetic area. On the other hand, if the vestibular table is intact, and provided there is no acute disease, the implant could be placed immediately5,6. There is no scientific evidence that early placement guarantees a better outcome than immediate placement when correctly indicated, whether with or without provisionalization5,7,8. In order to reduce the treatment time, in 2008 Da Rosa9proposed, for cases with partial or total loss of the vestibular table, the Immediate Dentoalveolar Restoration (IDR) technique. The purpose of this technique is to repair the defect in the socket with a corticomedullary bone graft from the maxillary tuberosity and, simultaneously, to place the implant and perform immediate non-occlusal loading.
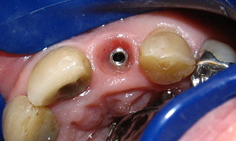
A.2. Absence of soft tissue. Delaying implant placement10 or performing soft tissue grafts and the placement simultaneously is recommended. It is currently believed that an adequate amount of soft tissue helps prevent marginal recession, hide the margins of the restoration and disguise the shadow in the implant platform11,12 (Figs. 1, 2). Moreover, from an aesthetic perspective, an adequate amount of keratinized tissue is crucial as it allows for a harmonious gingival contour without inflammation, light pink and spotted, synonymous with pink aesthetics. It is therefore impossible to achieve adequate aesthetic outcomes in the aesthetic area without the right amount of keratinized tissue.
A.3. Gingival biotype. A direct link between the gingival biotype and the final outcome has not been proven. A limited number of clinical studies which have researched the link between the gingival biotype and the aesthetics of implants were found in the available literature, with some authors claiming that a thick gingival biotype does not guarantee that there will not be any gingival recession13,14. Despite this, the literature agrees that a thick gingival biotype is a desirable characteristic which will positively impact the aesthetic outcome of an implant-supported restoration since it is more resistant to mechanical and surgical insult, making it less susceptible to gingival recession. (Fig. 2). Changing the biotype with connective tissue grafts could be considered for thin gingival biotypes. Some authors claim that the influence of the gingival biotype would manifest in the gingival margin, and not in the gingival papillae, an entity that could be influenced by other kinds of factors, such as the distance from the bone crest of the adjacent tooth to the contact point of the restoration 7,15
A.4. General factors which may be contraindications for implant therapy. A suitable assessment of the general condition of the patient is something important to be considered when planning a dental implant-based treatment. It is worth noting that the need for implants increases with the age of the patient, therefore, these treatment plans very often need to be tailored to their general condition. Patients who are deemed high risk due to chronic general diseases, and use of tobacco or a medication which affects bone tissue, should be treated with caution, since aesthetic outcomes are less predictable for them6.
B. Extrinsic factors
B.1. Correct implant selection. Aesthetic failures can occur when selecting an inappropriate implant, mainly as a consequence of using large diameter implants. The implant selected must not come into contact with the vestibular table in order to leave a gap between them, in anticipation of the dimensional changes in the socket after extraction8 (Figs. 3, 4). Evans and Chen (2008) 13 found that contact between the implant shoulder and the vestibular table was a significant factor in gingival recession. This proximity to the vestibular table can be due either to incorrect implant placement or to the fact that the diameter was incorrectly selected. Selecting the diameter of the implant based solely on the dimensions of the tooth to be replaced, or using implants with enlarged platforms or wide-neck implants, must be avoided. In these cases, the implant shoulder can be too close to the vestibular bone and adjacent teeth, considerably increasing the risk of recession2 (Fig. 5).
B.2. Three-dimensional position of the implant. There is agreement in the literature that a correct three-dimensional position of the implant is one of the main, if not the main, factor for good aesthetic outcome with implant-supported restorations. The relation between the implant shoulder and the planned restoration will provide stability to hard and soft tissues. According to most authors, the correct 3D position of the implant is as follows:
a. In the apical-coronal dimension, the implant platform must be located 3 or 4 mm from the gingival margin expected for the future crown.
b. In the buccal-palatal dimension, the emergence of the chimney should be at the level of the cingulum of the tooth to be replaced and the labial surface of the implant platform should be 1 or 2 mm palatal to an imaginary line passing through the most convex portion of the two adjacent teeth at the level of the gingival margin.
c. In the mesial-distal dimension, at least 1.5 mm from the adjacent tooth at the level of the bone crest and with a 3 mm distance between implants2,13,14 (Fig.6).
B.3. Implant design. Platform switching implants, that is, implants with a connection in which the diameter of the abutment is smaller than the diameter of the implant, are recommended for the aesthetic area. The gap is therefore moved toward the center of the implant, which reduces crestal bone resorption and allows for an increased growth of soft tissue14,16,17 (Fig. 7).
B.4. Surgical technique. To finish with gingival recession, it is worth noting that although there is literature on it, it is not conclusive as to whether flapless techniques have better outcomes than flap techniques18. As for immediate implants, there is scientific evidence that flapless placement and immediate provisionalization result in better gingival stability.
Question No. 2. How important is the management of the provisional restoration in shaping peri-implant tissues in the aesthetic area?
-Gingival anatomy in natural dentition. The soft tissue that surrounds the crowns of natural teeth has a scalloped shape. This shape follows the design of the bone crests of the dental sockets -which are also scalloped- and these, in turn, mirror the scallop of the cementoenamel junction of the teeth. This junction is closer to the apical portion in the zenith of the free surfaces, and about 2 or 3 mm more toward incisal in the center of the proximal faces19,20.
-Usefulness of implant-supported provisional restorations. Restorations on implants must meet a series of requirements, some of which are aesthetic. Significant progress has been made in ceramic restoration materials in recent times, along with the growth in the aesthetic demands of patients. But an optimal aesthetic outcome does not depend solely on correctly replicating the hard tissues of the tooth (white aesthetics); it must be accompanied by the right anatomy of the surrounding soft tissue (pink aesthetics) 21. Provisional restorations are fundamental in all areas of restorative dentistry. Specifically, in implant rehabilitations, they serve different purposes in the stages prior to the final rehabilitation, making it possible to assess and decide on crown shapes and positions, curvatures and occlusal planes, incisal guide angle, among other clinical benefits which the dental technician will then transfer to the final restoration. They also play an important part in the maturation and shaping of the soft tissues which surround the implant, both by attempting to maintain in the best way possible the gingival anatomy of a tooth which was just removed, and altering the flat shape of the mucosa of an edentulous ridge, trying to replicate the naturally scalloped shape of the gums surrounding natural teeth. Afterwards, it is possible to transfer to the laboratory the shape obtained in the soft tissues during the phase with provisional restorations, when the final impression the dental technician22 is taken using personalized transfer copings (Figs. 6, 8).
-The problems of dental avulsion and the peri-implant anatomy of gums. When teeth are missing, there is major loss of volume of the alveolar ridge in the buccal-palatal dimension23, with minimal height bone loss24. In the case of individual edentulous gaps, which are adjacent to natural teeth with a healthy periodontium, the gap will remain in its place thanks to the conservation of the periodontium in the adjacent tooth. In edentulous ridges that have already been remodeled, where two or more adjacent teeth are missing, the height of the bone anatomy is approximately 1 mm more apical to where the vestibular bone crest of the missing teeth was, and is usually flat, not scalloped, due to the loss of the proximal bone crest that was between the teeth. The oral mucosa that lines said bone crest also has a flat shape. This is why in large gaps, after placing a provisional prosthesis on a dental implant, we find that the anatomy of soft tissues is flat because the anatomy of the edentulous bone crest is also flat. There will be a height deficit in peri-implant soft tissues in the part corresponding to the papillae. However, and depending on whether the three-dimensional location of the implant is correct(2), we will often have excess soft tissue in the vestibular surface. We must remember that the soft tissue can fill a maximum of 5 mm vertically between two natural teeth, measuring the distance from the bone crest to the base of the contact point25. Nevertheless, average clinical measurements of soft tissue height between two implants were 3.4 mm26. Another negative aspect to consider is the loss of height of the interdental bone crest after the two adjacent teeth have been removed. Therefore, soft tissue between two adjacent implants will be approximately 1.5 mm thinner, and the interproximal bone crest will be 3 mm more apical in relation to what happens between two natural teeth with a healthy periodontium.
-Usefulness of provisional restorations in post-extraction immediate implants. Immediate placement techniques, performed in the hope that the functional stimulation provided by the implant would prevent alveolar bone resorption, have been widely recommended in recent years. In the first years of this century, the research of Araujo, among others27, made it very clear that this assumption was wrong. Similarly, it is claimed that the immediate provisionalization of the implant placed right after extraction will maintain the position of the marginal gingiva unchanged, since placing an artificial crown that supports the soft tissues will prevent them from collapsing. It is very clear that immediate provisionalization provides great psychological and functional advantages to patients, aside from reducing treatment times and the number of surgeries. However, clinical research does not seem to be conclusive in showing clear advantages in final outcomes regarding the position of the vestibular marginal gingiva and the proximal papillae 7,28,29. Also, with immediate provisional restorations after extractions, with or without occlusal contact, special attention must be paid to the shape and thickness of the subgingival portion of the implant. Current criteria focus on avoiding subgingival overcontours, which reduce space for soft tissues and are responsible for their tendency towards retraction. Other factors, such as the three-dimensional position of the implant, its diameter and thickness, and the position of hard and soft tissues, greatly influence the final position of the soft tissue that surrounds the implant and its restoration, aside from the placement of an immediate provisional prosthesis at the time of extraction (Figs. 7, 9, 10, 11).
-Usefulness of provisional restorations in the modeling of peri-implant soft tissue. Starting from a flattened gingival anatomy, and having excess tissue in the middle vestibular zone, the vestibular gingiva can be moved toward the apical surface very easily, overcontouring the provisional restoration subgingivally in that zone(30). Likewise, it is also possible to move the zenith of the vestibular gingiva in the mesial or distal direction until said gingival margin is in a position that is correlated to the aesthetic standards established for the specific tooth and is in harmony with neighboring teeth. The possibility of changing the position of soft tissues in the proximal area between two adjacent implants is not that clear. In this case, the goal is not to retract the gingival margin in the apical direction, on the contrary, we should make it grow in the incisal direction. Techniques consisting of pressuring proximal tissues laterally in order to make them grow have been proposed30,31. These papers describe a compression technique wherein proximal soft tissues are compressed using the provisional restorations, after which they are reduced a few days later to allow for said tissues to grow (Figs. 6, 7, 8). In any case, we still need comparative clinical studies, with accurate clinical measurements which scientifically prove that these techniques achieve the desired outcomes. In contrast, papers referring to these techniques merely describe them, with some clinical illustrations, but nothing that would allow for definitive conclusions regarding whether better dimensions are achieved in interproximal tissues compared to the clinical situation in which provisionals are not used for compression. We must also consider the fact that papillae between implants have a natural tendency to grow somewhat within the first months after crown placement32,33. It would be important to design clinical studies aimed at comparing the outcome in the final position of soft tissues between adjacent implants or between an implant and a natural tooth, having used the compression technique with provisionals, and not having used it. Outcomes should be assessed based on objective aesthetic indices21 and taking measurements to compare, whenever possible, the position of said tissues before avulsion and after the treatment has been completed. It would also be desirable to compare the position obtained in relation to the soft tissue of the contralateral teeth in order to draw valid conclusions.
-Provisional restorations and cement-retained prostheses. Provisional restorations are also essential in cement-retained restorations. Excess subgingival cement is being cited as a risk factor for peri-implant disease34. It has been suggested that margins should not be located deeper than 2 mm in relation to the free edge of the peri-implant gingiva. If the restoration is completed after a sufficient tissue maturation process with screw-retained provisionals, we can leave the margins of the restoration a short distance from the free edge of the gingiva, with a small risk of them being visible in the future. Therefore, screw-retained provisional restorations are recommended over cement-retained ones. When placing cement-retained crowns, a minimal perforation, measuring 1 mm in diameter, located on the occlusal or palatal surface, helps avoid the confinement effect of the cementing material, by guiding the material out through the perforation and, consequently, preventing it from projecting beyond the crown margins. In conclusion, aside from the psychological and functional advantages the patient gets from having provisional fixed restorations for some time before the final rehabilitation, the aesthetic evaluation by both patients and professionals, for long periods of time, allows for better outcomes in the end. Moreover, by working in this manner, at the time the final impressions are taken, soft tissues will have a shape that is evaluated and stable enough to set the permanent positions of the final restoration, and unexpected changes in the stages after placement will be less likely. Aside from the limitations of interimplant soft tissues in the final outcome, provisional restorations play a vital role in the stage that goes from the end of the osseointegration period until the placement of the final restoration.
Question No. 3. What is considered optimal management of abutments regarding design, materials and aesthetics? Different causes have been proposed in the literature to explain the loss of the peri-implant bone crest, some of which are: accumulation of stress due to occlusal forces, thin bone tissue and peri-implant mucosa, and recovery of the biological width naturally, surgical trauma and the implant-abutment connection, among others. The preservation of the bone crest is a fundamental objective in the aesthetic area, as a way of achieving a harmonious gingival architecture, thus avoiding gingival recession. Abutment selection plays a key role in this. Based on the literature reviewed, guidelines were established to select them correctly:
-Shape. The shape of the abutment is one of the factors to consider. Using straight abutments or abutments with diameters smaller than the implant platform is advisable to preserve as much peri-implant soft tissue as possible. Authors such as Zuhr35 recommend a subcontoured abutment, which favors the adaptation of gingival tissues during healing and prevents gingival recession due to excessive compression (Fig. 10).
-Platform. Another aspect to consider to preserve the bone crest is platform switching, in which the diameter of the abutment is smaller than the implant platform. Thus, the implant-abutment microgap is horizontally relocated, which creates a healthy biological width.
-Type of connection. The literature is not clear in determining whether one type is more favorable to preserve the bone crest, and none has been shown to have an inactive microgap since microbial contamination through the implant-abutment space is found in all systems36,37.
- Thickness of the gingival tissues. It is a significant factor in the selection of the abutment material. For gingival thicknesses smaller than 2 mm, zirconia displays better optical properties than metallic abutments38.
-Biocompatibility of the different materials. In some studies, zirconia abutments seemed to favor the health of gingival tissues given that there might be less biofilm adherence than with titanium abutments(39). Other authors, however, found no differences when comparing these materials40. Regarding epithelial adhesion, in a study conducted by Belser et al.(40 titanium and ceramic abutments showed a better performance compared to gold alloy and ceramic fused to metal abutments. Other authors mention that these outcomes depend on the adhesion properties of the materials studied and their differences in terms of resistance to corrosion39. According to the literature available today, it is difficult to reach a conclusion on the advantages of one material over others, since there are variables that were not considered in the different studies, including the degree of micro-roughness of the abutment, or the cleaning and sterilization procedure it requires before use. Studies that include all those variables are necessary to reach final conclusions for selecting the ideal material for abutments. There is agreement in the aesthetic sector in indicating zirconia abutments. However, different authors have recommended caution when using them due to the small scientific evidence available of long-term outcomes41. The authors of this work think that there are technical problems as a result of using zirconia as the material for abutments, such as the impossibility of replicating some internal connection systems, the fracture of the abutment when torque is applied to the retention screw, or the damage to the hexagon of the implant. To solve these problems, the industry offers zirconia abutments with metal bases that can be cement-retained (Ti Base, Biomet), which tends to increase the volume of the abutments in the emergence at the implant level. This can be a disadvantage in some clinical situations, for example, for lateral incisors (Figs. 11, 12).
Question No. 4. What aesthetic evaluation indices are there? The literature presents varied attempts at objectively measuring the degree of success of the different treatments on implants. Different authors have tried to develop a valid method (using different parameters). In the opinion of the workshop participants, none covers all the variables that can be considered to measure success42,43. Despite this, the Belser index was chosen as the most complete one in terms of evaluation criteria, since it evaluates both soft tissues: Pink Esthetic Score (PES) and the restoration: White Esthetic Score (WES). The PES covers five variables: mesial papilla, distal papilla, curvature of the facial mucosa, level of the facial mucosa, convexity, color and texture on the facial aspect of the zone of the implant. These variables are numbered from 0 to 2, with 2 being the maximum. The WES focuses on the restoration of the implant. It is based on five parameters: shape and volume of the clinical crown; color and texture of the surface, and translucency. A score of 0, 1 or 2 is assigned to each parameter, therefore, for an optimal restoration, the maximum WES is 10. The five parameters are evaluated by comparing them directly to the adjacent or contralateral natural tooth. Therefore, the highest possible PES/WES score is 20, which means that the peri-implant soft tissues and the clinical crown of the implant are a complete match to the reference tooth21.
Conclusions
The topic of this workshop is one of the most interesting in the current literature. Achieving aesthetically pleasing outcomes is the main objective of any treatment in the anterosuperior sector, but this depends on the evaluation of multiple factors that the professional must consider when selecting the treatment. The success of implant-supported restorations is the result of the right diagnosis and, then, of a treatment plan that considers the advantages and disadvantages of the different options available. Despite this and even if the case has been correctly evaluated, small deviations occur frequently with discouraging aesthetic outcomes.
Scientific review. The workshop leaders selected papers that were representative of the subject matter to be discussed, based on which they asked questions that covered the contents of those papers, facilitating an enriching scientific exchange among participants. The workshop followed the planning and coordination schedule. The members of the workshop showed varying degrees of level and participation. Few participants knew the literature suggested and the value of publications based on the type of study (systematic review, meta-analysis, a series of clinical cases). The discussion resulted in the conclusions presented in this paper. These conclusions are representative of the literature reviewed and the scientific development of the workshop
Referencias
1. Papaspyridakos P, Chen CJ, Singh M, Weber HP and Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012; 91: 242-8. [ Links ]
2. Buser D, Martin W and Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004; 19 Suppl: 43-61. [ Links ]
3. Hammerle C, S.TChen and Wilson TG. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004; 19: 26-8. [ Links ]
4. Chen ST and Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009; 24 Suppl: 186-217. [ Links ]
5. Tortamano P, Camargo LO, Bello-Silva MS and Kanashiro LH. Immediate implant placement and restoration in the esthetic zone: a prospective study with 18 months of follow-up. Int J Oral Maxillofac Implants. 2010; 25: 345-50. [ Links ]
6. Belser U, Buser D and Higginbottom F. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004; 19 Suppl: 73-4. [ Links ]
7. Kan JY, Rungcharassaeng K, Lozada JL and Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011; 26: 179-87. [ Links ]
8. Levin BP and Wilk BL. Immediate provisionalization of immediate implants in the esthetic zone: a prospective case series evaluating implant survival, esthetics, and bone maintenance. Compend Contin Educ Dent. 2013; 34: 352-61. [ Links ]
9. Martins Da Rosa,JC. Implantes con Carga Inmediata en Alveolos Comprometidos. Edit Santos Brasil, 2012. [ Links ]
10. Buser D, Chen ST, Weber HP and Belser UC. Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures. Int J Periodontics Restorative Dent. 2008; 28: 441-51. [ Links ]
11. Chung DM, Oh TJ, Shotwell JL, Misch CE and Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006; 77: 1410-20. [ Links ]
12. Schrott AR, Jimenez M, Hwang JW, Fiorellini J and Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009; 20: 1170-7. [ Links ]
13. Evans CD and Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008; 19: 73-80. [ Links ]
14. Fu JH, Lee A and Wang HL. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants. 2011; 26: 499-508. [ Links ]
15. Chow YC, Eber RM, Tsao YP, Shotwell JL and Wang HL. Factors associated with the appearance of gingival papillae. J Clin Periodontol. 2010; 37: 719-27. [ Links ]
16. Lazzara RJ and Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006; 26: 9-17. [ Links ]
17. Canullo L, Fedele GR, Iannello G and Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res. 2010; 21: 115-21. [ Links ]
18. Caneva M, Botticelli D, Salata LA, Souza SL, Bressan E and Lang NP. Flap vs. »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ flapless »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ surgical approach at immediate implants: a histomorphometric study in dogs. Clin Oral Implants Res. 2010; 21: 1314-9. [ Links ]
19. Becker W, Ochsenbein C, Tibbetts L and Becker BE. Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol. 1997; 24: 727-31. [ Links ]
20. Gallucci GO, Belser UC, Bernard JP and Magne P. Modeling and characterization of the CEJ for optimization of esthetic implant design. Int J Periodontics Restorative Dent. 2004; 24: 19-29. [ Links ]
21. Belser UC, Grutter L, Vailati F, Bornstein MM, Weber HP and Buser D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009; 80: 140-51. [ Links ]
22. Elian N, Tabourian G, Jalbout ZN, et al. Accurate transfer of peri-implant soft tissue emergence profile from the provisional crown to the final prosthesis using an emergence profile cast. J Esthet Restor Dent. 2007; 19: 306-14; discussion 15. [ Links ]
23. Botticelli D, Berglundh T and Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004; 31: 820-8. [ Links ]
24. Schropp L, Wenzel A, Kostopoulos L and Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003; 23: 313-23. [ Links ]
25. Tarnow D, Magner A and Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992; 63: 995-6. [ Links ]
26. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003; 74: 1785-8. [ Links ]
27. Araujo MG, Sukekava F, Wennstrom JL and Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005; 32: 645-52. [ Links ]
28. Tsuda H, Rungcharassaeng K, Kan JY, Roe P, Lozada JL and Zimmerman G. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011; 26: 427-36. [ Links ]
29. Cabello G, Rioboo M and Fabrega JG. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res. 2013; 24: 1094-100. [ Links ]
30. Su H, Gonzalez-Martin O, Weisgold A and Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int J Periodontics Restorative Dent. 2010; 30: 335-43. [ Links ]
31. Wittneben JG, Buser D, Belser UC and Bragger U. Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: the dynamic compression technique. Int J Periodontics Restorative Dent. 2013; 33: 447-55. [ Links ]
32. Jemt T. Restoring the gingival contour by means of provisional resin crowns after single-implant treatment. Int J Periodontics Restorative Dent. 1999; 19: 20-9. [ Links ]
33. Priest G. Predictability of soft tissue form around single-tooth implant restorations. Int J Periodontics Restorative Dent. 2003; 23: 19-27. [ Links ]
34. Wilson TG, Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009; 80: 1388-92. [ Links ]
35. Zuhr O. Maintenance of the Original Emergence Profilefor Natural Esthetics with Implant-SupportedRestorations. Implant Prosthodontics. 2002. [ Links ]
36. Dibart S, Warbington M, Su MF and Skobe Z. In vitro evaluation of the implant-abutment bacterial seal: the locking taper system. Int J Oral Maxillofac Implants. 2005; 20: 732-7. [ Links ]
37. Schwarz F, Hegewald A and Becker J. Impact of implant-abutment connection and positioning of the machined collar/microgap on crestal bone level changes: a systematic review. Clin Oral Implants Res. 2014; 25: 417-25. [ Links ]
38. Iñaki Gamborena MBB. The Gray ZoneAround Dental Implants:Keys to Esthetic Success. The American Journal of Esthetic Dentistry. 2011; 1: 26-46. [ Links ]
39. Nakamura K, Kanno T, Milleding P and Ortengren U. Zirconia as a dental implant abutment material: a systematic review. Int J Prosthodont. 2010; 23: 299-309. [ Links ]
40. Belser UC, Schmid B, Higginbottom F and Buser D. Outcome analysis of implant restorations located in the anterior maxilla: a review of the recent literature. Int J Oral Maxillofac Implants. 2004; 19 Suppl: 30-42. [ Links ]
41. Guess PC, Att W and Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res. 2012; 14: 633-45. [ Links ]
42. Furhauser R, Florescu D, Benesch T, Haas R, Mailath G and Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005; 16: 639-44. [ Links ]
43. Annibali S, Bignozzi I, La Monaca G and Cristalli MP. Usefulness of the aesthetic result as a success criterion for implant therapy: a review. Clin Implant Dent Relat Res. 2012; 14: 3-40 [ Links ]
Received: March 28, 2017; Accepted: July 11, 2017











 texto en
texto en