Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.19 no.spe Montevideo set. 2017
https://doi.org/10.22592/ode2017n.esp.p28
Articles
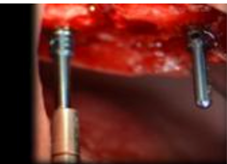
Workshop 3 - Short implants or sinus floor elevation
1Servicio de Prótesis Buco Maxilo Facial. Integrante Departamento de Implantología Oral y Maxilofacial. Facultad Odontología. Universidad de la República. Uruguay. consultorioborgia@gmail.com
2 Clínica Cirugía BMF I. Docente de la Carrera de Especialización en Implantología Oral y Maxilo-Facial. Facultad Odontología. Universidad de la República. Uruguay
INTRODUCTION
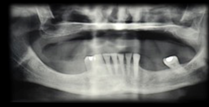
The use of dental implants to replace missing teeth is a safe and effective long-term treatment, given the high predictability of osseointegration. Nowadays, implants are placed where the rehabilitation is required. In all cases, bone availability is one of the reasons for concern for clinicians at the time of implant placement. The different areas in both jaws present their own challenges regarding the ideal location to place the implant. Bone with sufficient height and width, and of good quality, is essential for the correct placement of implants, so they can support a dental prosthesis.
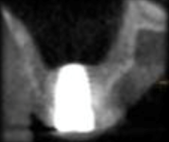
The aim of this workshop was to assess the posterior maxillary area. The posterior maxilla naturally presents low-height alveolar process, which is anatomically limited by the maxillary sinus. The roots of the molars are closely related to the floor of the maxillary sinus. In the center of the alveolar crest we find the root trifurcation area, which is the ideal site for implant placement from a prosthetic perspective, and where there is the lowest bone height in the sinus floor. This means that placing implants of standard dimensions after tooth loss
in this area is limited.
The resorption processes resulting from such loss, common to all regions of the alveolar process, may aggravate this situation. Maxillary sinus pneumatization, on account of increased osteoclastic activity along the sinus membrane and the absence of a dental “barrier” facing changes in sinus air pressure, may affect the morphology of the site. These conditions pose an anatomical challenge to the treatment of the edentulous posterior maxilla using dental implants. The techniques to repair defects in the residual alveolar ridge with autologous bone graft procedures have predictable results, which are described in the literature. A factor that explains their good results is that there are no immune reactions that may interfere with the process of tissue remodeling and development. They intrinsically have osteoblasts and growth factors responsible for the cellular changes that occur after implantation, and that end with remodeling and bone formation at the site1. Its disadvantage is the need for an additional donor surgical area which can be intraoral, in cases in which the need for reconstruction is small, or extraoral in cases of medium-sized or large reconstructions. In the 1980s, bone grafting techniques in the maxillary sinus were used to solve the problem of lack of bone, and to allow for implant placement. One of the techniques described is surgery to lift the floor of the maxillary sinus, known by its name in English: Sinus Lift2,3.
Various alternatives to the technique and different types of grafts and biomaterials of different nature have been proposed as an alternative to autogenous bone to fill the cavity resulting from the elevation of the sinus floor. The application of biomaterials has been encouraged given its ease of use and technique with a very good clinical performance, and the limited supply of autogenous bone in relation to the necessary volume for a sinus lift. Philip Boyne2 (1983) describes the reconstruction of fractures with bovine bone. His studies were part of the development of inorganic bovine bone: material which is very similar to human bone. Studies conducted on animals suggest that deproteinized bovine bone is resorbed and gradually replaced by viable bone tissue. It is a slow process compared with autografts4, which helps preserve the macrostructure rebuilt in the replacement process. Depending on bone availability (height and width) in the posterior maxillary area, the options for placing implants in the right place are:
No prior treatment if there is the necessary height and width, elevation of the sinus floor on account of drilling surface or lateral approach according to subantral bone availability.
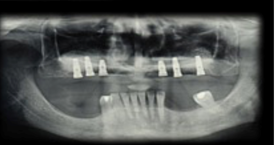
Use of short implants.
Block grafts.
Workshop methodology. The workshop aims to reach consensus on the indications and contraindications of sinus lift techniques and the use of short implants (8.5 mm or less). These were the main stages:
Literature review. Based on a review of the literature of the last ten years, the workshop leaders selected fifteen papers representative of the topic to be addressed. The papers were: Four systematic literature reviews; four clinical trials, three prospective studies, and four case reports. All the studies selected were conducted on humans, not on animals. The selection did not attempt to exhaust the search, but rather it was supposed to act as a trigger for a review process conducted by the workshop participants.
Guiding questions. To guide the debate, there were six questions representative of the selected bibliography and the topic of the workshop.
Short implants or maxillary sinus lift? Which technique is more predictable according to the literature?
Indications and factors to consider to perform a maxillary sinus lift.
Indications and factors to consider when placing short implants.
Is there a gold standard for filling materials?
Crestal approach or lateral window approach in the sinus lift technique?
In the lateral approach, is it necessary to place a collagen membrane in that window?
Exchange with participants of the seminar. Workshop participants were emailed the selected bibliography and discussion guiding questions for them to read and evaluate, and they were invited to two prior meetings to begin the scientific exchange.
Scientific review. It was decided that a scientific reviewer should be present at the workshop without participating in the discussion. He would evaluate: the quality of the suggested literature, the representativeness of the guiding questions, the scientific level reached during the discussion on the day of the seminar, and the connection between the conclusions of the seminar and the guiding questions and bibliography.
Workshop participants. The following professionals attended the workshop: Drs. Agustín García, Álvaro Rivero, Beatriz Cabral, Bernadet Herrera, Célica Laens, Constanza Panissa, Hugo Rodríguez, Marcelo Yaque, Mariana Suarez, Marisa Raffo, Natalia Terzaghi, Ronald Daga, Esmir Cabrera.
Work done at the workshop.
Question No. 1. Short implants or maxillary sinus lift? Which technique is more predictable according to the literature? According to the literature studied, the maxillary sinus lift technique is better documented, showing long-term implant survival rates. However, there are possible complications, such as: sinusitis (3%) and infections (1%), in addition to a higher morbidity. This makes it relevant to evaluate other techniques, which show similar results5. Currently, the use of short implants (less than 8 mm) is a practice that in the last six years (medium term) has acquired sufficient scientific support to be applied, depending on the clinical situation6,7,8.
Question No. 2. Indications and factors to consider to perform a lateral approach maxillary sinus lift.
Reduced subantral bone height (5 to 8 mm) is required. Less invasive and simpler techniques are needed for specific reasons, such as: systemic problems, psychological profile or patient’s choice.
The patient should be properly informed of other options, advantages and disadvantages, as well as of the availability of scientific evidence.
The professional should be able to provide such information as objectively as possible, and avoid leading the patient to choose the technique that the professional masters.
Question No. 3. Indications and factors to consider to perform a lateral approach maxillary sinus lift. Indicated in the absence of sufficient alveolar bone for implant placement with predictability in the maxillary sinus. The techniques for such a procedure would be:
Lateral window in two times: Best-documented procedure, showing long-term implant survival rates. This technique can be applied in the most diverse clinical situations, except when there are local and general contraindications for oral surgeries.
Lateral window in one time: The literature supports this procedure with implant long-term survival rates similar to the lateral window in two times technique. There is not enough scientific evidence to reach a consensus regarding a minimum bone height. To achieve good primary stability, the following minimum measures may be suggested for the subantral bone tissue: 3 mm in height and 5 mm wide9. This primary stability depends not only on quantity but also on implant quality, technique and design. Some studies show that rough surfaces have a better survival rate than machined implants10.
Crestal approach technique: Summers technique. Osteotomy is performed for the implant up to 1mm subantrally, until the sinus floor is reached with osteotomes, allowing for increases in height of 2 to 5 mm. This technique also shows high survival rates, similar to the traditional technique11. A minimum height of 5 mm of residual bone is recommended9. A problem with this technique is that the perforation of the membrane may go unnoticed, so placing bone substitutes is recommended11.
Question No. 4. Is there a gold standard for maxillary sinus filling materials? The biological gold standard is the autologous graft, as it is the only one which is osteoconductive, osteoinductive and osteogenic. However, this does not appear to be very relevant for maxillary sinus filling, except that it accelerates the times for implant(s) placement. Furthermore, the literature shows that the resorption rate is greater than that of most bone substitutes. Therefore, there is no gold standard for filling materials, but rather there are several slow-resorption osteoconductive biomaterials with solid scientific evidence. These can be used alone or combined, showing similar survival rates in the implants12,13.
Question No. 5. Crestal approach or lateral window approach in the sinus lift technique? There is no antagonism. On the contrary, both techniques have excellent results and are complementary. Implant survival rate is similar.
Question No. 6. In the lateral approach, is it necessary to place a collagen membrane in the window? The literature reports similar success rates in both techniques. However, there are studies that show a higher percentage of vital bone when using the membrane14,15. Therefore, though unnecessary, we suggest placing a membrane in the window to cover the regeneration site beyond the borders of the osteotomy (window).
Scientific reviewer report. Quality of work: The planning and coordination of the workshop complied with the allocated times. The academic level was very satisfactory. Workshop leaders showed solid knowledge of the topic, having read well beyond the material assigned. The guiding questions were conceptual, well formulated, and thoroughly discussed. The members of the workshop showed varying degrees of level and participation. No participant had vast experience in the specific topic in question, which did not hinder a discussion based on academic material. The level of scientific evidence was achieved mainly based on selected reading. Few participants knew the value of publications based on the type of study (systematic review, meta-analysis, a series of clinical cases), and they tended to evaluate the work based on the number of cases. The methodology used was correct: question and time allocated to each participant for contributions. The person in charge of the workshop may have partially led participants to conclusions based on their own. In brief, the findings are consistent with the most serious and high-level publications in the subject. Prof. Dr. Susana Vázquez
Referencias
1. Marx RE, Miller RI, Ehler WJ, Hubbard G, Malinin TI. A comparison of particulate allogeneic and particulate autogenous bone grafts into maxillary alveolar clefts in dogs. J Oral Maxillofac Surg 1984; 42: 3-9. [ Links ]
2. Boyne P, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 1980; 38(3):613-616. [ Links ]
3. Lamberti-Salagaray V, Losada-Lorencez J. Tecnica de elevación sinusal. Madrid: Unidad de implantologia oral y prótesis biointegrada, 1993. [ Links ]
4. Sohn DS, Kim WS, An KM, Song KJ, Lee JM, Mun YS. Comparative histomorphometric analysis of maxillary sinus agumentation with and without bone grafting in rabbit. Implant Dent 2010; 19(3): 259-270. [ Links ]
5. Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants 2009; 24(suppl):237-259. [ Links ]
6. Gioacchino Cannizzaro PF, Minciarelli AF, Leone M, Viola P, Esposito M. Early implant loading in the atrophic posteriormaxilla: 1-stage lateral versus crestal sinus liftand 8 mm hydroxyapatite-coated implants. A 5-year randomised controlled trial. Eur J Oral Implantol 2013; 6(1):13-25. [ Links ]
7. Corrente G, Abundo R, Bermond des Ambrois A, Savio L, Perelli M. Short Porous Implants in the posterior maxilla: A 3-year report of a prospective study. Int J Periodontics Restorative Dent 2009; 29:23-29. [ Links ]
8. Deporter D, Ogiso B, SeokSohn D, Ruljancich K, Pharoahi M. Ultrashort sintered porous-surfaced dental implants used to replace posterior teeth. J Periodontol 2008;79:1280-1286. [ Links ]
9. Taschieri S, Corbella S, Del Fabbro M. Mini-invasive osteotome sinus floor elevation in partially edentulous atrophic maxilla using reduced length dental implants: interim results of a prospective study. Clin Implant Dent Relat Res. 2014;16:185-93. [ Links ]
10. Del Fabbro M, Wallace SS, Testori T. Long-term implant survival in the grafted maxillary sinus: A systematic review. Int J Periodontics Restorative Dent 2013; 33:773-783. doi: 10.11607/prd.1288. [ Links ]
11. Corbella S, Taschieri S, Del Fabbro M. Long-term outcomes for the treatment of atrophic posterior maxilla: A systematic review of literature. Clin Implant Dent Relat Res. 2015 Feb;17(1):120-32. [ Links ]
12. ChackartchiT., Iezzi G., GoldsteinM., KlingerA., SoskolneA., PiattelliA., Shapira L. Sinus floor augmentation using large (1-2 mm) or small (0.25-1 mm) bovine bone mineral particles: a prospective, intra-individual controlled clinical, micro-computerized tomography and histomorphometric study. Clinical Oral Implants Res 2011; 22: 473-480 [ Links ]
13. Froum SJ, Wallace S, ChoonCho S, Rosenberg E, Froum S, Schoor R, Mascarenhas P P, Tarnow DP, Corby P, Elian N, Fickl S, Ricci J, BinHu, Bromage T, Khouly I. A histomorphometric comparison of Bio-Oss alone versus Bio-Oss and Platelet-derived growth factor for sinus augmentation: A postsurgical assessment. Int J Periodontics Restorative Dent 2013; 33:269-279. doi: 10.11607/prd.1614. [ Links ]
14. Wallace SS, Tarnow D, Froum SJ, Choon Cho S, Zadeh HH, Stoupel J, Del Fabbro M, Testori T. Maxillary sinus elevation by lateral window approach: Evolution of technology and technique. J Evid Base Dent Pract 2012:S1:161-171. [ Links ]
15. Barone A, Ricci M, Grassi RF, Nannmark U, Quaranta A, Covani U. A 6-month histological analysis on maxillary sinus augmentation with and without use of collagen membrans over the osteotomy window: randomized clinical trial. Clin Oral Impl Res. 2013; 24: 1-6 [ Links ]
Received: March 28, 2017; Accepted: July 11, 2017











 texto en
texto en