Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.19 no.spe Montevideo Sept. 2017
https://doi.org/10.22592/ode2017n.esp.p13
Articles
Workshop 2 - Loading protocols
1 Asistente Cátedra de Rehabilitación, Prostodoncia Fija y TTM, Docente Carrera de Especialización en Implantologia, Integrante del Departamento de Implantología Oral y Maxilofacial.Facultad de Odontología. Universidad de la República, Uruguay. jorge.giribone@adinet.com.uy
2 Ayudante Cátedra de Rehabilitación, Prostodoncia Fija y TTM. Facultad de Odontología. Universidad de la República, Uruguay.
3 Facultad de Odontología. Universidad de la República, Uruguay.
4 Asistente Cátedra de Rehabilitación, Prostodoncia Removible I y Gerodontología. Facultad de Odontología. Universidad de la República, Uruguay.
INTRODUCTION
Implant treatment for replacing missing teeth is currently a highly predictable and reliable technique. New treatment protocols have been suggested to minimize treatment time and the number of clinical sessions, to improve patients’ comfort and, in many cases, final results in the short, medium and long term. Therefore, different times are defined when the implant/s start working using the scheduled prosthesis, either temporarily or permanently, that is to say, the loading mode. Determining the ideal time for each case remains a controversial decision among professionals, as a multiplicity of interrelated factors must be considered. These involve the patient, thoroughly evaluated at the general (physical and psychological, and social analysis), regional and local levels. In addition, there are variables related to the implant selected, the surgical expertise of the operator, and prosthetic factors at the laboratory and the clinic, which together contribute to the decision-making process and the success of the treatment. There are also differences regarding this decision-making process depending on the type of prosthesis, fixed or removable, and its extension: full arch, partial arch, or individual cases.
Workshop participants: Drs. Mario Pedreira, Matias Morales, Pablo Russo, Analía Melo, Virginia Lazo, Pedro Incio, Ademar Febo, Patricia Nicola and Jorge Giribone.
Workshop methodology. To visualize this multiplicity of variables, a study group was created-workshop-that worked within the First International Congress of Oral and Maxillofacial Implantology of the School of Dentistry, Universidad de la República (UDELAR). The starting point was a literature search on Timbó and Pubmed portals, using “loading” and “dental implants” as keywords. From the selection of the most relevant articles, of recent years, with the strongest scientific support, the guiding questions raised (Table 1) and their subsequent discussion, we state the following conclusions in order to achieve consensus at the national/regional level.
Table 1 Guiding questions
| 1. What is considered immediate loaging, early loading and conventional loading? |
| 2. Is immediate loading predictable? Is it more predictable in fixed restorations in full arches, partial arches, or in individual cases? |
| 3. What is the minimum insertion torque required for immediate loading? What is the purpose of measuring the Implant Stability Quotient (ISQ)? |
| 4. Which implant characteristics should be considered for immediate loading? |
| 5. When should immediate loading, early loading and conventional loading be performed? |
| 6. How should occlusal loads be managed in immediate and early loading? |
WORKSHOP
Question No. 1. What is considered immediate loading, early loading and conventional loading? It is currently somewhat difficult to establish uniform terminology regarding the concepts of immediate loading, early loading and conventional loading. First, we must state what we understand by the term “loading”, so as to establish when we can apply it. Loading is the time when implants are subjected to functional loads, be them occlusal, or those developed by soft tissue muscles (tongue and cheeks) and by the alimentary bolus (non-occlusal load). It is stated that the difference between loading times lies in the time that elapses from implant placement, using hours, days, or weeks, and the installation of the prosthetic component. Authors such as Shibly et al.8) consider immediate loading is when the prosthesis is placed on the same day as the implant, while others, such as Alsabeeha et al.14 and Harel et al.2 say it is when occlusion occurs until 48 hours after implant placement4,17. On the other hand, authors such as Barewall et al.3, extend this period up to 6 weeks. According to Alsabeeha et al.14, early loading occurs between 48 hours and 12 weeks, while for Grandi et al.1 it entails making the prosthesis functional after a healing period of two months. Regarding conventional loading, authors like Alsabeeha et al.14) say that it includes the period of three to six months after surgery, depending on whether the procedure was performed on the lower or upper jaw respectively. Therefore, the differing views of authors such as those mentioned above create confusion when establishing and protocolizing procedures for the rehabilitation of patients with partial or total loss of their natural dentition. After reviewing the suggested literature, it is concluded that the time period within which you can perform immediate loading extends to one week after implant placement13. A clear example would be the protocol to follow for immediate lower hybrid prosthesis14,17. For early loading13, the time elapses from the first week until the eighth, where the ISQ value of the stability of the implant is essential20,23,28. Conventional loading starts from the eighth week after implant placement.
Immediate loading (within the first week after implant placement)
Early loading (between the first week until the eighth week after implant placement)
Conventional loading (from the eighth week after implant placement)
These times can be correlated with the evolution of peri-implant bone healing and maturation.
Question No. 2. Is immediate loading predictable? Is it more predictable in fixed restorations in full arches, partial arches, or in individual cases? Successful treatments based on dental implants have been associated with rigid protocols and long periods of osseointegration of three to six months without load based on an empirical approach6. Immediate loading has several advantages over conventional loading:
A removable prosthesis is not used, which is clearly more comfortable for patients.
It eliminates uncontrolled transmucosal loading caused by the use of removable prostheses17.
There are advantages in the preservation of the peri-implant gingival architecture, which improve if associated with immediate placement after extraction (in the situations indicated) and alveolar preservation techniques, thus minimizing and/or compensating for vestibular bone remodeling26.
It has been shown that immediate loading achieves bone healing of better quality, maturation and percentage of contact of the bone-implant interface32.
Psychological benefits, and reduction in the number of necessary clinical sessions, as well as of surgical interventions, which improves patients’ acceptance of the treatment12,17.
Several factors should be considered for immediate loading to be successful, which can be divided into four categories: surgical considerations, characteristics of the host (bone density), implant selection and factors related to occlusion. A group led by David L. Cochran et al.29 was convened to conduct a review to determine when a procedure can be recommended, based on the available evidence. In the literature reviewed, the parameters included full-text articles in English, threaded titanium implants with a follow-up period of at least one year. Not many cases were found with these parameters, the format found being case reports. In edentulous jaws, the immediate loading of four implants with overdentures with rigid bar fixation and bilateral contacts is a predictable and well documented procedure. This predictability refers both to osseointegration and to preservation of the marginal bone. This indication is the only one for which the literature has randomized and controlled studies. This procedure, following the above criteria, is supported by seven studies involving 376 patients and 1529 implants. Regarding the immediate loading of implants supporting a fixed prosthesis in edentulous jaws, it was concluded that it is a predictable and well-documented procedure. The consensus group found 15 articles including 387 patients and 2088 implants, 1804 of which were loaded immediately. Regarding the edentulous maxilla, no article was found linking immediate loading to an overdenture. Therefore, this procedure should be considered experimental for now. Restoration or immediate loading of implants supporting fixed prostheses in partially toothed mandible and maxilla is not well documented. There is, however, a large number of clinical cases with satisfactory results. The height of the interproximal bone crest and the changes in the soft tissues reported in cases with immediate loading have been similar to those restored with conventional loading procedures. However, due to the limited number of implants (in comparison to those fitted for conventional loading cases) and the short follow-up period, new studies are necessary to consider this a usual procedure32. These data were confirmed by H.P. Weber et al. in 200920 in the 5th ITI Consensus Conference, and by clinical recommendations on loading protocols. Meloni et al.12, in a randomized controlled trial with a one-year follow-up, compared the results of immediate loading versus conventional loading in bilaterally missing mandibular first molars, where both protocols were applied respectively. Marginal bone loss was 0.83±0.16 mm in the immediate loading group, and 0.86±0.16 mm in the conventional loading group, which means there was not a statistically significant difference. In addition, probing depth was 2.76±0.48 for the immediate loading group, and 2.70±0.37 for the conventional loading group. Noga Harel et al.2 compared 110 implants placed in the maxilla randomly assigned to immediate loading (IL) or conventional loading (CL). The overall survival rate was 99.09% (CL: 98.11%, IL: 100%). Additionally, no evident bone loss was found in 83.49% of the implants, while in the rest there was no difference between immediate loading and conventional loading cases. H.E. Khorshid et al18, in a case report of patients with mandibular Kennedy Class I with multi-implant resolution, refer to different immediate loading protocols. Immediate Occlusal Loading (IOL), with maximum occlusal contact with the antagonist; Immediate Non-Occlusal Loading (INOL) without occlusal contact with the antagonist, and Immediate Progressive Loading (IPL), initially with slight occlusal contact. Subsequently, contact is added during the healing process to achieve the desired final occlusal contacts, concepts introduced in 1980. The authors studied the cases performing IOL and IPL respectively, with a follow-up period of 24 months. They concluded that patients who underwent an IPL procedure showed a more predictable bone reaction, lower marginal loss and better density measured in Hounsfield units. In their systematic review, F. Suárez et al. suggest that loading timing does not affect the marginal bone level around dental implants in a short follow-up time32. In addition to these data, the limited loss of height of the papillae and some regrowth after some years of function must be the result of the combination of surgical procedures reduced in number and volume, preservation of the bone spicule against the adjacent teeth, and preservation of the contour of temporary restorations. Despite this, at vestibular level there is recession over time, averaging 0.55 mm in the first year, and 1.13 mm after four years. The degree of recession varies according to gingival biotype, it being lower in thick biotypes.
It is very unlikely for progressive loading to bring clinical benefits; on the contrary, it makes procedures and times longer and more expensive13.
Immediate loading is predictable in terms of osseointegration and preservation of marginal bone.
There is more evidence on fixed restorations in full arches than in single or multiple partial cases.
Immediate loading in full fixed arches, both upper and lower, and in cases of mandibular overdentures with splinted parasymphyseal implants (two to four), is clinically and scientifically proven.
Question No. 3. What is the minimum insertion torque required for immediate loading? What is the purpose of measuring the Implant Stability Quotient (ISQ)? The first important concept to define is primary stability. This is the initial mechanical stability of the bone-implant interface before osseointegration or secondary stability4,5,11. There is no controversy in the literature about the importance of good implant stability for successful osseointegration, even more if early or immediate loading is considered. The primary stability of the implant is decisive and fundamental when applying an immediate loading protocol, whether it has occlusal contact or not5. To achieve this goal, and therefore minimize failures, it is essential to properly select the case and a well-trained operator, as it is a more sensitive technique. If adequate fixation is not achieved, or if other negative variables are suspected, the conventional loading protocol should be selected13. To objectively assess primary stability, the insertion torque value is used: the energy needed to insert an implant is measured in joules per cubic millimeter (J/mm³), as measured by a torque gauge that represents it indirectly in Ncm. You can also evaluate data obtained through the resonance frequency analysis (RFA), through the Osstell, an instrument that provides ISQ values. These values range between 1 and 100 ISQ units, derived from the rigidity of the transducer/implant/bone and the calibration parameters of the transducer5. Clinically, values are based on three elements: implant rigidity as per its geometry and composition, rigidity of the implant/tissue interface (bone to implant contact - BIC) and the height of the implant above the bone, and finally, the rigidity of the surrounding tissue (non-uniform relationship between cortical and medullary areas) and bone density3. The results of a meta-analysis of the capacity of RFA to predict immediate loading failures show that this technique has poor sensitivity, specificity and accuracy4. Therefore, they conclude that there is no significant advantage for the results of the immediate loading protocol when using this measurement at the time of the surgery. Resonance frequency analysis is a noninvasive method that measures implant stability, although it has not been the most accurate method to evaluate primary stability. There are problems for its use according to the implant system, its location and its rehabilitation (cement-retained restorations). It is a valid tool to measure implant stability over time (an indirect measure of osseointegration)3, although authors mention some ambiguity in the RFA data regarding exactly which biological parameter is measured and if it could predict early failures4. If the data fall below 45, failure should be considered a possibility, and healing without load should be allowed for 12 weeks3. In general, it could be considered as one more factor when deciding on immediate loading, following the minimum 65 ISQ established in the literature4,5. Both data provide quantifiable measures of stability, but of different aspects. The ISQ gives us data on the stability measured which is perpendicular to the axis of the implant (mesiodistal/buccolingual or vice versa), in reference to the bone walls. Rotational stability is evaluated with the insertion torque (point of view)3. The value of the insertion torque of an implant is directly related to its primary stability. The stronger the torque, the more stability. To achieve osseointegration it is necessary to maintain the micromotion of the bone-implant interface in average values of 50 to 100 µm4,6,11,31. The greater the primary stability, the lower probability of micromotion, but in cases of full or partial arches with multiple implants, cross-arch stability can be achieved by applying rigid splinting with the prosthetic element, which greatly reduces micromotion. Therefore, in these cases, insertion torque values for immediate loading must be between 20 and 30 Ncm6,17. Esposito13, in a systematic review published in 2013, states that 35 Newton is the minimum insertion torque for single restorations8,9, although in the literature reviewed, most authors agree on a 32 Ncm limit for immediate loading4,6. The possibility of obtaining sufficient insertion torque is seriously compromised in low-density bones3,11. A very high torque value (70 to 100 Ncm) might jeopardize implant viability, as when evaluating stability over time with RFA in cases of high initial insertion value, there is a marked decline in initial stages, which indicates that the biology of bone repair equates situations and then the final healing of the site begins. High torques (greater than 110 Ncm) do not cause peri-implant fibrosis, but induce increased bone remodeling, which modifies the bone healing process11. There was a minimal reduction in implant stability in the first four weeks in cases of immediate loading, measured in ISQ, if the insertion torque was around 20 Ncm3. The increase in primary stability can be achieved through under-drilling in cases of low bone quality. In contrast, randomized clinical trials establish that high insertion torques (greater than 80 Ncm) ensure the success of immediate loading1,9. We must remember that in cases with high torque, not all implant systems (composition and design) are sufficiently robust from a mechanical perspective. An in vitro study shows that with torque values over 45 (45-70-100 N. cm), micromotion variation is not statistically significant, and therefore high initial torque values are not considered necessary11. A connection is established between implant length and the requirement for higher torque values for immediate loading: at least 45 Ncm is necessary for short implants (6.5 mm)9.
To perform immediate loading, the minimum insertion torque value is 32 Ncm in individual cases, and between 20 and 30 Ncm for multiple cases. Short implants require 45 Ncm.
ISQ measurement has an evaluation and follow-up value.
Question No. 4. Which implant characteristics should be considered for immediate loading? Primary stability levels and loading protocols will vary according to the type of implant depending on changes in their geometry and technology for surface treatment. The implant must remain stable during peak bone resorption in the healing process that occurs between weeks two and three3. The factors that impact primary stability are bone quality and quantity, surgical technique, design, length and diameter of the implant and surface characteristics. However, influential factors for secondary stability include primary stability, bone remodeling and the conditions of the surface of the implant5,10,11. The design of threaded and tapered implants10,26 improves mechanical retention and increases the capacity to withstand compressive forces and to transform non-axial forces into compressive forces (upper or lower side of the thread, respectively). If the thread design provides a low torque and is combined with treated surfaces, an early loading protocol would be more suitable3. There are geometries designed especially for critical bone conditions12, square threads, greater thread depth, twin thread, number of threads per unit of length and their angles. However, it is noted that type IV bone is not suitable to support immediate/early occlusion in a single prosthetic design3. In a four-year clinical evaluation in fully edentulous mandibular and maxillary arches10 restored with immediate fixed multi-implant prostheses (six in the mandible and eight in the maxilla), most implants used had a diameter of 3.3 mm, and the others had a diameter of 5 mm, and were between 8 and 15 mm long. Success rates of 93.9% were observed for the 3.5 mm diameter, and 100% for those greater than 3.5 mm. Regarding length, the rates were 74.5% for under 10 mm, and 100% for over 10 mm. Implant diameter is inversely related to micromotion17,19. Therefore, the literature generally suggests the use of a 4 mm average diameter for implants (3.5-4-4.1-4.3-5)1,3,6,9,10,12,23 for immediate/early loading protocols. Regarding length, in general an average of 10 mm or greater1,2,3,6,10,19 is set for the same loading times, although some authors were successful with lower lengths: 8-8.5 mm9,12,21,23. As explained above, the crucial success factor is to preserve the stability of the bone/implant interface without movement. This is achieved in different ways, solutions which overlap or not, depending on the case: by immersing the implant (conventional loading:); good insertion torque; modifications in surgical technique (bicortical anchorage-under drilling); use of a greater number of implants with optimal location, distribution and alignment. This optimizes load function and dispersion by increasing the contact area, reducing the risk of overload. Splinting with the prosthetic element is necessary2, and when possible, the cross arch should be stabilized, thus minimizing occlusal contacts and accelerating healing through surface treatments (varying degrees and types of surface roughness and chemical variations), achieving better bone apposition in less time (induction of contact osteogenesis)31. The advantages of these treated surfaces are clear. All the papers reviewed agree on this, some with greater scientific evidence or with better properties, detailed according to each company. These surfaces allow for earlier bone apposition and increase the level of differentiation and osteoblastic activity according to in vivo and in vitro studies, showing a positive correlation between the treated surface and bone adhesion and its maintenance over time6,21. This is a significant characteristic in cases of low-density bones (upper jaw)9, and it can also stimulate soft tissue. These features not only improve bone healing times, but also the quality of the bone obtained, increasing BIC14,17,20. The key factors are topography, chemical variations, surface energy, wettability and capillarity. These qualities affect processes such as protein adsorption, cell-surface interaction and cell/tissue development in the implant/tissue interface21,26. Surface energy (free energy) and wettability improve the interaction between the surface of the implant and the biological environment, not only increasing osteoblastic differentiation and activity, but also the production of osteocalcin and local growth factors, inducing vascular proliferation and the early formation of mature bone at six weeks.
Implant selection is important for the different loading protocols.
For immediate loading protocol, we must consider: implant design (tapered and threaded), length (minimum of 10 mm), diameter (minimum of 3.5 mm except in cases of low bone quality, where larger diameter is indicated), and characteristics of implant surface (treated surfaces).
Question No. 5. When should immediate loading, early loading and conventional loading be performed? Certain characteristics of the development of prosthetic-surgical treatment lead us to make decisions regarding which protocol to follow, although most of them were evaluated accordingly in case planning. There might be modifications as clinical activities take place. Therefore, we present below a great variability of factors to consider for decision-making.
Immediate loading: Immediate loading is a clinical procedure sensitive to the operator’s skills and experience, with more heterogeneous bone loss, which is slightly higher than in early loading. This explains the sensitivity of the prosthetic and surgical technique, and of the factors to consider when selecting the patient.
Adequate primary stability1: This has already been considered in depth in section 3, although it is worth noting that low-density bone cases, detected subjectively when drilling, can lead to a change in the protocol to follow9. In these cases, it is difficult to achieve a level of stability around 35 Ncm12. Another point to remember is the serious loss of stability and the possible mobility of the implant in the early stages of healing, as definitive stability is hindered, as well as preserving resistance to micromotion above threshold levels27,30,32.
Sufficient bone quality and volume1: In relation to the point made above, failure rates of 3% are observed for type 1 to type 3 bones, and 35% in type 4 bone2. There must be sufficient height and width for proper implant placement with the characteristics mentioned in section 4 (10 mm average height, and 6 mm width)12, without major dehiscence or fenestrations that require significant grafts at the time of placement3. However, immediate loading is not discarded in these cases, and an accurate diagnosis is recommended for each particular case.
Absence of parafunctional habits: The literature reviewed clearly agrees on this1,2,3,4,6,8,9,12,17,18,19,20,21. This is absolutely logical as the low tolerance regarding effort absorption in the early stages of healing (first two to three weeks) is well known. Therefore, it is essential to observe the patient and to evaluate the patient’s habits regarding teeth grinding and/or rubbing, as well as tongue interposition and/or thrust, biting on soft tissue or external elements such as nails, pens, musical instruments, etc.
Favorable occlusal relationships1: The type of occlusion of the antagonist tooth is important, which should be stable. In cases of prosthetic rehabilitation on individual implants or partial dentures of short extension, it is recommended that you correctly design a mutually protected occlusion, either with natural antagonist and/or restored antagonist, and with edentulous limited spaces in the mesial and distal areas of the gap, to provide adequate posterior vertical support6,8,30. In cases of single teeth, it is necessary to leave an edentulous area in the buccolingual direction which must be greater than 6 mm, and in the mesiodistal direction of 6 to 10 mm, and at least 7 mm of space between the collar of the implant and the occlusal platform2,3,17. For overdentures that have as antagonist a conventional complete removable prosthesis, it is suggested that overdentures be used for some time before the surgery to achieve proper setting and the development of all relevant occlusal adjustments, thus reaching a balanced occlusion10,15,16. In full arches, it is better to have a fully edentulous antagonist with full removable prosthesis restoration. Severe skeletal discrepancies need to be evaluated when deciding on the loading time, whether given by the patient's natural intermaxillary relations17,18, as well as those caused by resorption patterns (Class V or VI according to Cadwood and Howell) that lead to an axis mismatch between the possible position of the implants and their rehabilitation, and which determine increased lever arms10. They are not considered favorable for the technique. The literature suggests the periodic and regular control of the stability of the temporary prosthesis, the occlusion, the patient’s diet and the stability of the implant28.
Early loading: Those who advocate for early loading describe a more conservative approach regarding bone and technical requirements. They also state that it can be performed jointly with procedures to minimally increase hard tissues with greater predictability. Although surface technology displays a suitable BIC after three weeks, it is considered favorable to wait longer by making provisionals, as well to wait for the maturation of soft tissues. The final restoration should be performed after six to eight weeks, with a final torque of 35 N20,23. There is greater risk of osseointegration failure than in conventional loading, and no significant differences with immediate loading. It is necessary to assess the advantages and disadvantages of this protocol in the posterior sectors with the patient, unlike the anterior sector, where there are aesthetic and functional limitations . Improvements in surface treatments are essential. It also requires greater clinical experience22,24.
Stability. Stability measurement must be performed with RFA at ISQ >65- 70 parameters3,4. When used in multiple measurements taken over time, it assesses the stability of the implant and helps determine the appropriate loading time or predict early signs of failure.
Sufficient bone quality and volume. As well as the considerations for immediate loading, an important factor is the existence of sufficient volume and bone tissue of suitable quality. Implant diameter does not appear to be significantly important in ISQ values, but length is, as better values are obtained with an increase in the BIC area4.
Absence of parafunctional habits. The articles reviewed establish similar parameters regarding the loads received by the implants. Therefore, they suggest avoiding this type of habits, especially before six to eight weeks have elapsed20.
Favorable occlusal relationships. As in the immediate loading protocol, occlusal relationships must be evaluated to avoid situations where the rehabilitation exposes the implant to movement above the threshold that allows for osseointegration.
Conventional loading: No parameters were established in the study group that contradict the conventional loading protocol, except when implant placement is contraindicated or impossible on account of local and/or general conditions.
Factors to evaluate. All the papers reviewed established various factors to consider to define or exclude a particular loading procedure. There follows a list of factors in the knowledge that some of them are more important than the others. However, the professional must know them all to be able to assess and assign the importance required by each case.
Age. Implant is placed in patients with full maxillary growth (over 18 years of age)2,3 with a normal capacity of bone cells (remodeled) (30 to 65 years: parameter for inclusion in the study)1.
Good oral hygiene. Several authors insist on a plaque index lower than 2 or 1 in cases of IL or EL1,2,3. A five-year prospective study with patients with periodontal susceptibility or periodontally treated establishes it is a risk factor regarding marginal bone loss, and relates 9/10 failures with immediate loading and immediate implants7. Other authors9,12,27 recommend not treating patients without prior periodontal treatment or with poor hygiene, and suggest the presence of 5-mm keratinized gum on the bone crest.
Generally compromised patients3. General Conditions that may be a contraindication for implant surgery, according to the American Society of Anesthesiologists, patients with severe but non-disabling systemic disease (ASA 3), immunodeficiency (HIV) (leukocyte dysfunction), rheumatoid arthritis, systemic lupus erythematosus, vascular disorders, herpes, anticoagulant therapy, or hematological disorders, kidney failure, liver diseases, severely compromised cardiovascular function, chemotherapy, antimetabolite therapy (methotrexate) or treatment with corticosteroids in the last two years4,9,10,12,15,17,20,21.
Diseases that affect bone metabolism1,3 and degenerative diseases21
Patients irradiated in the head and neck1 for a minimum of 12 months3,9,10,12,15
Patients with treatment with bisphosphonates, completely excluding those with I/V treatments9, and paying special attention to osteoporotic patients(1.3)
Untreated diabetes1,3) or insulin-dependent patients6,8,9,12
Drugs, substance use and/or abuse can affect the healing of the surgical site; minimum waiting time of five years is recommended1,3,9,12,21.
Alcohol. As in the previous item a waiting period of five years is recommended3.
Tobacco. Regarding this factor, the literature consulted establishes three categories: non-smokers, light smokers (less than 10 cigarettes/day or less than 10 packs/year, who should be warned and/or avoided), and heavy smokers, who smoke over 10 cigarettes/day and for a period of 5 years, for whom immediate loading and/or early loading protocols are avoided1,3,6,7,9,10,12,15,21,27.
Pregnancy. These maneuvers should be avoided during pregnancy because it is considered elective surgery, therefore, there is no strict need to cause possible complications to the patient1,3,9. Other authors also recommend not performing IL or EL in the breastfeeding period9,12
Infection or severe inflammation of the implant site. No implant placement should be performed in sites with acute infection1,3,9,10,21,27. Here the indications overlap with those for periodontal patients7.
Large space of 1.5 to 2 mm between the implant and the bone walls. This influences the possibility of achieving primary stability, as well as to the inability of the remaining bone walls to oppose the side loads the implant will be subjected to in immediate and early loading1,2.
Loss of one of the bone walls. The absence of one or a large part of one of the tables, usually the vestibular one, and therefore the need to repair it with grafting procedures, except the use of special techniques that require more skill and surgical complexity, is a limiting factor2,27. Studies recommend the use of immediate loading in cases of scarred ridges, with a post-extraction period of at least with weeks3 or four months15,21.
Need for bone volume increase procedures, including the maxillary sinus or sites treated with grafts should be avoided for protocols with reduced load times1,3,4,9,20. Immediate loading techniques can be used with transalveolar maxillary sinus lift, because of the bicortical anchorage of the implants, jointly with prosthesis with multiple attachments10,12.
Mucosal diseases or oral mucosa pathologies, such as oral lichen planus, should be avoided3,6,21.
Operator’s experience. We have already discussed the increased difficulty of immediate and early loading techniques, at the time of the surgery, as well as in their prosthetic performance and clinical-laboratory interrelation27.
Psychophysical tolerance. Performing the surgery and prosthetic maneuvers at the same time requires more time and tolerance from the patient. It is an important factor which is difficult to assess previously. These techniques should not be used with psychologically unstable patients or patients with psychiatric problems6,9,10,12.
Understanding of and commitment to the treatment are important factors to consider, especially when the patient is told about the daily care in the early days of treatment regarding soft diet and/or to avoid compromising by whatever means the success of the treatment, since after the period in the clinic, the final results depend on these attitudes2,3,15,27.
Question No. 6. How should occlusal loads be managed in immediate and early loading? Opinions vary on the handling of occlusion in immediate loading. Occlusal contacts are selected only in cases of full arches without occlusal contacts for individual restorations, with spaces without occlusion with the antagonist that vary in microns. These are evaluated by sliding tapes of known thickness, up to 1 mm clearances for the anterior sector, and 1.5 mm for the posterior sector1,6,9,12. However, regarding the patient’s appreciation, the difference is not significant as the patient has a new tooth as soon as possible. Additionally, although the restoration has no occlusal contacts, it is functional during mastication13. For all cases, soft diet is indicated after 4 to 8 weeks, as well as avoiding chewing on the compromised side1,18. In partial cases, the occlusal table decreases and occlusal contacts are restricted to a single contact in maximum intercuspation, which allows for sliding 10 μm tape, without excursive contacts1,18. Other authors17 recommend immediate functional loading in partial or total multi-implant arches, and in partial arches with a smaller number of implants or single implants without occlusal relationship with the antagonist32. These contacts must only be centric or in maximum intercuspation, mild and within the implant platform, using prosthetic parts with low cusp height to minimize side loads by distributing them on the largest area (large cusp-to-fossa relationship), with symmetrical distribution of the same and without cantilever18,19. They recommend checking the occlusion and the behavior of the prosthesis as there might be fractures, bond failure or loosening in the first few weeks, as well as checking the distribution of preferred occlusal loads in the remaining teeth17,19. Full arches with implants should have simultaneous bilateral posterior and anterior contact to distribute the load in the largest possible area in central and eccentric group function for an even distribution of forces17,27. Partial arches should have symmetrical soft contacts, with subsequent restorations without side contact. If it is a canine, decrease the guide to achieve group function. In the event of anterior restorations, contacts should be evenly distributed among all teeth17,32. For lower overdentures with four splinted implants with a bar, and the antagonist rehabilitated with a conventional removable complete prosthesis, there should be balanced occlusion. In the event of antagonist tooth with toothed arch, there should be group side excursive function30. It is suggested that screwed immediate provisional prosthesis be used (use of angulated abutments in two parts), reinforced with metallic elements, avoiding the use of cement that may result in inflammation, and therefore compromise the soft tissues with inflammation and/or retractions, facilitating removal. This is also beneficial regarding times and the prevention of laboratory complications. Avoid touching up the definitive prosthesis, mainly after the healing and stabilization of soft tissues and occlusal conditions. It makes it possible to adjust the occlusal diagram at the right time, and to develop a reduced dental arch. Additionally, it prevents the need to prepare a new definitive prosthesis in case of implant failure, and allows the professional to complete the work with all the surrounding elements properly set17.
Immediate loading:
In cases of full-arch fixed restorations: immediate occlusal loading located within the implanted arch
In case of multiple fixed restorations: immediate occlusal loading
In case of single fixed restorations: immediate non-occlusal loading
Early loading:
In cases of full-arch restorations, single and multiple partial restorations: definitive occlusal diagram selected according to the case
Conventional loading:
All implant indications can follow this protocol.
Scientific reviewer report: Dr. Diego Imas. The workshop was based on the six guiding questions, and participants discussed and exchanged views on the basis of scientific papers previously selected by the workshop leaders. The guiding questions were well made, except one, whose formulation was controversial. The seven participants had prepared by reading the literature assigned, some contributing more than others. Views were exchanged, which stimulated discussion among participants based on the reading and interpretation of the material. Participants tried to reach a consensus to answer the different questions raised. Some participants had done extensive reading, which was seen as they supported their answers citing the articles addressed, even criticizing some of them. The president and secretary of the workshop led the session in a very orderly manner, making a presentation with the questions, defining basic concepts with reference to the literature, in order to begin discussing each question. They involved the participants in the debate and participated themselves by discussing the material studied and contributing their experience on the subject. They evidenced a good command of scientific articles, as well as significant personal experience. The scientific articles were of a very high standard, which evidenced an excellent academic level. The workshop complied with the allocated times, the debate was very well organized and guided, seeking to reach a consensus on the issues addressed.
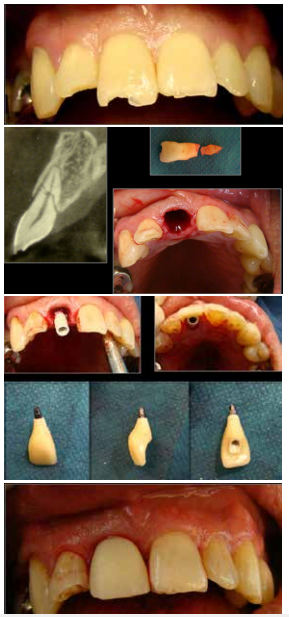
Clinical case: solved with immediate implant and immediate non-occlusal loading (Fig. 1).
Referencias
1. Grandi T, Guazzi P, Samarani R. et al. A 3-year report from a multicentre randomized controlled trial: immediately versus early loaded implants in partially edentulous patients Eur J Oral Implantol 2013;6(3):217-224. [ Links ]
2. Harel N, Piek D, Livne S, Palti A. et al. A 10-Year Retrospective Clinical Evaluation of Immediately Loaded Tapered Maxillary Implants. Int J Prosthodont 2013;26:244-249. [ Links ]
3. Barewal RM, Stanford C, Weesner TC. A Randomized Controlled Clinical Trial Comparing the Effects of Three Loading Protocols on Dental Implant Stability. Int J Oral Maxillofac Implants 2012;27:945-956. [ Links ]
4. Atieh MA, Alsabeeha NHM, Payne AGT. Can Resonance Frequency Analysis Predict Failure Risk of Immediately Loaded Implants? Int J Prosthodont 2012;25:326-339. [ Links ]
5. Ji-Su Oh, Su-Gwan Kim. Clinical study of the relationship between implant stability measurements using Periotest and Osstell mentor and bone quality assessment. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;113:e35-e40 [ Links ]
6. Pinheiro Ottoni J. M.; Fagundez Lima Oliveira Z.; Mansini R. et al. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants 2005;20:769-776 [ Links ]
7. Horwitz J, Machtei EE. Immediate and delayed restoration of dental implants in patients with a history of Periodontitis: A prospective evaluation up to 5 years. Int J Oral Maxillofac Implants 2012;27:1137-1143. [ Links ]
8. Shibly O, Kutkut A, Patel N, et al. Immediate implants with immediate loading vs. conventional loading: 1-year randomized clinical trial. Clinical Implant Dentistry and Related Research, 2012, Volume 14, Number 5,663-671. [ Links ]
9. Cannizzaro G, Leone M, Ferri V, Viola P, Federico G, Esposito M. Immediate loading of single implants inserted flapless with medium or high insertion torque: a 6-month follow-up of a split-mouth randomized controlled trial. Eur J Oral Implantol 2012;5(4):333-342. [ Links ]
10. Covani U, Orlando B, D'Ambrosio A, et al. Immediate rehabilitation of completely edentulous jaws with fixed prostheses supported by implants placed Into fresh extraction sockets and in healed sites: A 4 year clinical evaluation. Implant Dent 2012;21:272-279 [ Links ]
11. Trisi P, Perfetti G, Baldoni E, et al. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Impl. Res. 20, 2009/467-471. [ Links ]
12. Meloni S M; De Riu G; Pisano M, et al. Immediate versus delayed loading of single mandibular molars. One-year results from a randomised controlled trial. Eur J Oral Implantol 2012;5(4):345-353 [ Links ]
13. Espósito M, Grusovin MG, Maghaireh H, et al. Interventions for replacing missing teeth: Different times for loading dental implants. Cochrane Database of Systematic Reviews, Issue11, 2013. [ Links ]
14. Alsabeeha N, Atieh M, Payne A. Loading Protocols for Mandibular Implant Overdentures: A Systematic Review with Meta-Analysis. Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010. [ Links ]
15. Moustafa Abdou Elsyad M A, Fathy Al-Mahdy Y, Fouad MM. Marginal bone loss adjacent to conventional and immediate loaded two implants supporting a ball-retained mandibular overdenture: a 3-year randomized clinical trial. Clin. Oral Impl. Res. 23, 2012 / 496-503 [ Links ]
16. Sunyoung Ma; Payne A Marginal Bone Loss with Mandibular Two-Implant Overdentures Using Different Loading Protocols: A Systematic Literature Review. Int J Prosthodont 2010;23:117-126. [ Links ]
17. El Ghoul W, Chidiac JJ. Prosthetic Requirements for Immediate Implant Loading: A Review. J Prosthodont 2012; 21:141-154 [ Links ]
18. Khorshid H E; Fotouh Hamed H A; Aziz E A.The Effect of Two Different Immediate Loading Protocols in Implant-Supported Screw-Retained Prostheses. Implant Dent 2011;20:157-166. [ Links ]
19. Menini M, Signori A, Tealdo T, et al. Tilted implants in the immediate loading rehabilitation of the maxilla: A Systematic Review. J Dent Res 2012; 91(9):821-827, [ Links ]
20. Weber HP, Morton D, Gallucci GO, et al. Consensus statements and recommended clinical procedures regarding loading protocols. Int J Oral Maxillofac Implants 2009; 24 (Suppl): 180-183. [ Links ]
21. Zôllner A, Ganeles J, Korostoff J,. et al. Immediate and early non-occlusal loading of Straumann implants with a chemically modified surface (SLActive) in the posterior mandible and maxilla: interim results from a prospective multicenter randomized-controlled study. Clin. Oral Impl. Res. 2008; 19: 442-450. [ Links ]
22. Rocuzzo M, Aglietta M, Cordaro L. Implant loading protocols for partially edentulous maxillary posterior sites. Int J Oral Maxillofac Implants 2009; 24 (Suppl): 147-57 [ Links ]
23. Grütter L, Belser UC. Implant loading protocols for the partially edentulous esthetic zone Int J Oral Maxillofac Implants 2009;24(Suppl):169-179. [ Links ]
24. Cordaro L, Ferruccio Torsello F, Roccuzzo M. Implant loading protocols for the partially edentulous posterior mandible. Int J Oral Maxillofac Implants 2009;24(Suppl):158-168 [ Links ]
26. Tim De Rouck T, Collys K, Cosyn J. Single-Tooth Replacement in the Anterior Maxilla by Means of Immediate Implantation and Provisionalization: A Review. Int J Oral Maxillofac Implants 2008; 23:897-904 [ Links ]
27. Del Fabbro M, Ceresoli V, Taschieri S,et al. Immediate loading of postextraction implants in the esthetic area: Systematic Review of the Literature. Clinical Implant Dent Related Res 2015; 17(1):52-70 [ Links ]
28. Nedir R, Bischof M, Smuckler-MonclerS, et al. Predicting osseointegration by means of implant primary stability A resonance-frequency analysis study with delayed and immediately loaded ITI SLA implants. Clin Oral Impl Res 2004;15:520-528 [ Links ]
29. Cochrane DL, Morton D, Weber HP. Consensus statements and recommended clinical procedures regarding loading protocols for endossoeus dental implants. Int.J. Oral Maxillofac Implants 2004; 19(suppl): 109-113. [ Links ]
30. Morton D, Jaffin R, Weber HP. Immediate restoration and loading of dental implants: Clinical considerations and protocols Int J Oral Maxillofac Implants 2004;19 (suppl): 103-108 [ Links ]
31. Cochrane DL. The evidence for immediate loading of implants. J Evid Based Dent Pract 2006; 6: 155-163. [ Links ]
32. Degidi M, Scarano A, Lezzi G, et al. Perimplant bone in immmediately loaded titanium implants: Histologic and histomorphometric evaluation in human. A report of two cases. Clin Oral Implant Dent Relat Res 2003; 5 (3): 170-175. [ Links ]
Received: March 28, 2017; Accepted: July 11, 2017











 text in
text in