Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.19 no.spe Montevideo Sept. 2017
https://doi.org/10.22592/ode2017n.esp.p5
Articles
Workshop 1 - Ideal time for implant placement: immediate, early or delayed
1 Prof. Adj. Cátedra de Oclusión y Prostodoncia. Docente Carrera de Especialización en Implantología Oral y Maxilo-Facial. Universidad de la República. Uruguay. ramosyannuzzi@gmail.com
Introduction
Deciding on the time to place the implant is essential to achieve the objectives set out in all implant-prosthodontic rehabilitation treatments, ensuring the long-term function and aesthetics of the restoration, with minimal morbidity. The need for extraction may have several causes: from extensive caries that prevent rehabilitation, to acute or chronic infectious processes of endodontic, periodontal or traumatic nature; the diagnosis and treatment plan must determine the indication for extraction and the right time to perform it. Functional and aesthetic rehabilitation through implants will depend on their optimal placement in a suitable alveolar process1. The alveolar bone is a tissue that depends on the tooth, and which develops during tooth eruption and is remodeled after tooth loss. Post-extraction dimensional changes will have a direct impact on the clinical procedure to follow. As a result of alveolar modeling and remodeling, the literature describes a loss in height and width in the first six months; these vertical changes are displayed at around 11 and 22% six months after extraction, and 32% horizontally after three months, reaching 63% at six months2. Studies have shown that the loss occurs mainly in the vestibular cortical bone3. The effect of bone loss is greater and varies if there have been multiple extractions, absence of adjacent teeth, poor bone quality and infection3,4. The highest percentage of dimensional changes occurs in the first month and continues in a lower percentage in the following months2, resulting in the loss of contour in soft and hard tissues. The range of these dimensional changes has an interindividual variation: the thin periodontal biotype has a higher predisposition to resorption and recession than the thick biotype with low scalloping. The literature points to the vestibular center as the area with greatest resorption risk, resulting in lower dimensional changes in the proximal area3,5. We identified a vestibular bone thickness lower than or equal to 1 mm as a critical factor associated with vestibular resorption; the thin wall phenotypes displayed marked vertical losses, measuring 7.5 mm compared with thick wall phenotypes with losses of 1.1 mm(6.7). Placing the implant immediately, in the fresh extraction site, does not affect the dynamics of bone remodeling. The results of clinical, radiographic and histological studies indicate that bone healing of sites with immediate placement continues its remodeling process3. According to Corbella8, immediate implantation in sites with periapical pathology has a clinical success equivalent to that achieved with implants placed in healthy sites when a rigorous medical and surgical protocol is implemented. However, further studies are needed to confirm the long-term predictability of the treatment. The bone destruction pattern resulting from periapical pathology should be taken into account when considering immediate placement. Fugazzoto9 suggests a classification system for periapical lesions: 1 to 3, depending on bone availability to ensure primary stability and to guide clinical procedures.
Type 1: There is enough periapical bone to achieve primary stability.
Type 2: There is no suitable periapical tissue to ensure primary stability, which is achieved laterally.
Type 3: There is no suitable bone, apical or lateral tissue to ensure adequate primary stability.
Regarding the failure rate of immediate implants in patients with severe periodontal disease, compared with delayed implants, the results indicate a greater risk of failure associated with the maxilla due to bone characteristics10. In recent years, researchers have tried to reduce the treatment times needed, in response to the demand for shorter treatments and less complex surgical procedures. In 1980, the standard post-extraction area treatment was to place the implant after six to twelve months of healing, which caused aesthetic and functional problems.
In 2004, Hammerle11 suggests a classification concerning the time of placement based on post-extraction morphological, histological and dimensional changes which includes four categories; Type 1: Immediate placement; Type 2: Early implant placement, with healing of soft tissues (4-8 weeks); Type 3: Early implant placement, with partial bone healing (12-16 weeks); and Type 4: Late placement, full bone healing (over 6 months). Esposito et al. (2006) suggest the use of the following terms: immediate, immediate-delayed and delayed. These classifications aim to achieve the primary and secondary goals of any rehabilitation treatment, as mentioned above.
Workshop methodology. People leading the workshop: President: Dr. Adriana Ramos, Secretary: Dr. Martín Sanguinetti, and Reviewer: Dr. Andrés Rodríguez. They organized debates and conducted a literature review in international databases: MEDLINE, PUBMED, LILACS, COCHRANE and SciELO. They selected 23 articles and then the bibliography was extended by the workshop members during the preliminary phase. The workshop was developed following six guiding questions, discussing and exchanging views with the participants, on the basis of pre-selected scientific papers, to find answers to the questions and to seek consensus around them. During the workshop, participants decided to group the questions that were complementary. These conclusions were compiled according to clinical research in which patients with the following risk factors were excluded: irradiated patients, smokers (more than ten cigarettes a day), immunocompromised individuals and untreated diabetes. The reviewer was fundamental to make the workshop a scientific event; he rated the performance of participants and authorities at the workshop, as well as the selected bibliography, the quality of the debate and the correlation between the conclusions and the scientific evidence considered at the workshop.
Participants: Doctors Aida Wodowoz, Victoria Pebé, Federico Riva, Gastón Olascuaga, Juan Brembilla, María Clara Bruzzone, Mario Delgado, Mónica Fernández, Salbhaí Alayón and Carolina Varela.
Workshop.
Question No. 1. In the 1980s it was considered that waiting 6 to 12 months after tooth extraction to place the implant was the health standard. Which is the current standard procedure? Based on the scientific literature, participants found three suitable times for implant placement in relation to the time elapsed from the extraction (Figure 1):
Immediate: placement in the same surgical act as the extraction.
Early: placement within 4 to 8 weeks after extraction.
Delayed: placement 16 weeks after extraction.
Each modality has specific indications according to the diagnosis, the available evidence, the operator’s experience and the patient’s requirements. According to the current state of knowledge about post-extraction alveolar remodeling, the most recent trend is to select an immediate or early placement protocol. Immediate and early implant placement has advantages regarding conservation of soft and hard tissues in comparison with a delayed implant protocol. Delayed post-extraction placement, with a healing period of 6 to 12 months, in a fully healed boned, ensures that the implant is inserted in a dimensionally stable ridge. However, bone availability may have been compromised by the changes caused by alveolar remodeling. Socket-preservation techniques minimize bone loss in the first months after tooth extraction, and allow the professional to place the implant in an ideal three-dimensional position; this reduces the need for additional surgical techniques12. The early implant-placement protocol has been suggested because it shares some of the advantages of immediate placement, such as using bone volume immediately after extraction, although already in the second month there is alveolar bone loss; it also allows for the primary closure (epithelium-connective tissue) of the wound(13). It is indicated in the presence of acute infectious processes, as the waiting time allows the process to be resolved. Recession of the vestibular mucosal margin is frequently found in immediate implants; risk indicators include a thin or damaged vestibular cortical bone, a thin periodontal biotype and an inaccurate three-dimensional position of the implant, which goes more into the vestibular area. Early implant placement is associated with a lower frequency of mucosal recession compared to immediate placement, when combined with regeneration procedures14,15.
Question No. 2. Could we develop a treatment protocol for post-extraction sockets that will receive implants immediately? (Fig. 2). Which would be the local risk factors to consider? Regarding immediate placement, the following conditions were considered favorable:
Absence of acute infections
Possibility of having the right three-dimensional location of the implant, as shown in Fig. 2
Presence of favorable bone tissue for immediate placement, with presence of the four walls and a maximum loss of 1.5 mm
Thick periodontal biotype
Bone phenotype higher than 1 mm (thickness of vestibular table)
Absence of dehiscence and/or fenestrations (no contraindications, nor relative parameters for immediate placement were found regarding these two points in the literature reviewed).
If there are compromised sockets, such as those with partial or total resorption of the vestibular cortical bone, vertical defects that involve bone walls, with localized recession of the vestibular gingival margin, the immediate dentoalveolar restoration (IDR) technique is implemented to repair the compromised socket, at the same time as the implant with non-occlusal function. The IDR technique suggests the tuberosity as the donor area for the corticomedullary graft, depending on the type of defect in the recipient area. The emergence profile characteristics determine the support required for the graft16. In the literature reviewed, clinical studies excluded patients with the following local risk factors: periodontal disease, active caries and inadequate oral hygiene. It is clear from the literature that the geometric design of the implant does not affect the final aesthetic result17,18. In the treatment of intact sockets, the size of the gap (horizontal gap that remains between the bone walls and the surface of the implant after placement) requires special attention. If there is a gap, bone formation can occur in two ways: (a) directly on the surface of the implant, in areas in contact with the residual bone (osteogenic contact) or (b) by apposition, where the new bone is formed from the surface of the implant (osteogenic gap). For gap treatment, when there is a vestibular table with the right height, the literature has established an arbitrary measurement of 2 mm in relation to the gap to guide the clinical procedure to follow. Biomaterials should be used if the gap is greater than 2 mm, and if lower, the professional should wait for healing through a blood clot12. The filling procedure modifies the final result in terms of amount of bone tissue18 and architecture of soft tissue19. If there is favorable bone phenotype, the aim of the bone filling of the gap is to preserve tissue. There is no difference in relation to the gap regarding the use of different types of filling and their combination with membranes (new studies are needed in this regard).
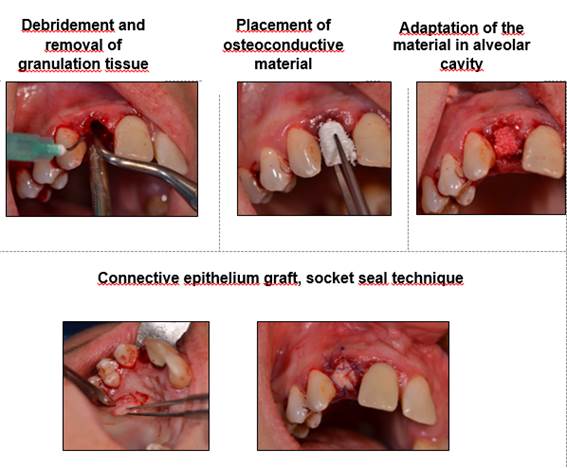
Question No. 3. Could we develop a treatment protocol for post-extraction sockets that will receive delayed implants? General guidelines and definitions have been established. We understand alveolar preservation as the conservation or prevention of dimensional changes of the alveolar anatomy. Alveolar recovery procedures are understood as the maneuvers aimed at recovering the socket’s lost dimensions20. Regarding clinical situations:
If it is necessary to extract the tooth because of acute infection, professionals wait 4-8 weeks, and at that time evaluate the possibility of alveolar recovery and early placement, or alveolar recovery and delayed implant placement.
If there is a need for extraction with no acute infection, hard and/or soft tissue will be repaired in the sockets if necessary, and implant placement will be delayed.
There is scientific evidence supporting preservation maneuvers (aimed at preserving socket dimensions, Fig.3) and alveolar recovery (aimed at restoring socket dimensions), with better end results when compared to a healing process from the blood clot only 14,15,21,22,23,24
Conclusions
Based on this literature review, immediate or early placement techniques are predictable clinical approaches, and can be considered an alternative to delayed placement. It is essential to carefully select cases, and surgical and prosthetic protocols.
Scientific review. The reviewer, Dr. Andrés Rodríguez Figueroa, stated the following: The members made their contributions with solid scientific support, and with an interesting pragmatic attitude. Opinions were exchanged regarding the papers selected and other papers individually chosen. Many were criticized for their methodology in the research process, which proves the participants’ deep understanding of the scientific method. They showed very good handling of previously selected papers, an organized debate, good time management, and the search for consensus to answer the questions. The workshop conclusions were then taken to the authorities of the First Congress of Oral and Maxillofacial Implantology of Uruguay for their dissemination
Referencias
1. Weng D, Stock V, Schliephake H. Are socket and ridge preservation techniques at the day of tooth extraction efficient in maintaining the tissues of the alveolar ridge? Systematic review,consensus statements and recommendations of the 1st DGI consensus conference in september 2010, Aerzen, Germany. Eur J Oral Implantol 2011; 4 (suppl): s59-s66. [ Links ]
2. Tan W, Wong T, Wong M, Lang N. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Impl Res. 23 (suppl. 5), 2012: 1-21. [ Links ]
3. Araujo M, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 2005; 32: 212-218. [ Links ]
4. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio A. Relationship between the buccal bone plate thickness and the healing of postextraction Sockets With/Without Ridge Preservation. J Periodontics Restorative Dent 2014;34:211-217 [ Links ]
5. Caneva M, Botticelli D, Salata L, Scombati S, Bresan E, Lang N. Flap vs. ''?apless'' surgical approach at immediate implants: a histomorphometric study in dogs. Clin. Oral Impl. Res. 21, 2010 / 1314-1319 [ Links ]
6. Chu S, Tarnow D. Managing esthetic challenges with anterior implants. Part 1: Midfacial recession defects from etiology to resolution. Compendium; 2013, 34 (No. spec, 7): 26-31 [ Links ]
7. Chappuis V, Engel O, Reyes M, Shahim K, Nolte L, Buser D. Ridge alteraciones post-extraction in the esthetic zone: A 3D analysis with CBCT. JDR Clinical Research Supplement, 2013; 92 (suppl Nº2): 195S- 201S. [ Links ]
8. Corbella S, Taschieri S, Tsesis I, Del Fabro M. Postextraction implant in sites with endodontic infection as an alternative to endodontic retratment: A review of literature. J Oral Implantol 2013; 39(3): 399-405. [ Links ]
9. Fugazzotto P. A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: results and clinical considerations. Int Oral Maxillofac Implants 2012; 27: 192 - 202. [ Links ]
10. Feilong D, Hua Z, Hui Z, Haibin S, Qifen H, Peifen Z. A comparison of clinical outcomes for implants placed in fresh extraction sockets versus healed sites in periodontally compromised patients: A 1-year follow-up report. Int J.Oral Maxillofac Implants 2010;25:1036-1040. [ Links ]
11. Hämmerle Ch, Chen S, Wilson Jr.T. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants 2004; (19, supplement): 26-8 [ Links ]
12. Juodzbalys G, Wang H. Socket Morphology-Based Treatment for Implant Esthetics: A Pilot Study. Int J Oral Maxillofac Implants 2010; 25: 970 - 978. [ Links ]
13. Sanz I, García-Gargallo M, Herrera D, Martin C, Figuero E, Sanz M. Surgical protocols for early implant placement in post - extraction sockets: a systematic review Clin. Oral Impl. Res. 2012; 23 (Suppl.5): 67-79. [ Links ]
14. Chen S, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites.. Int J Oral Maxillofac Implants 2009; 24(suppl):186-217. [ Links ]
15. Buser D, Chapuis V, Kuchler U, Bornstein M, Wittneben J, Buser R, Cavusoglu Y, Belser U. Long term stability of early implant placement with contour augmentation. JDR Clinical Research Supplement. 2013; 92 (suppl Nº2): 176S- 182S. [ Links ]
16. Martins Da Rosa JC. Restauración dentoalveolar inmediata. Ed Santos, 2012. [ Links ]
17. Sanz M, Cecchinato D, Ferus J, Pjetursson E, Lang N, Lindhe J. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla. Clin Oral Impl Res. 2010; 21: 13-21. [ Links ]
18. Ferrus J, Cecchinato D, Pjetursson E, Lang N, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Impl Res. 2010; 21: 22-29. [ Links ]
19. Araujo M, Linder E, Lindhe J. Bio-Oss Collagen in the buccal gap at immediate implants: a 6 month study in the dog. Clin Oral Impl Res. 22,2011: 1-8. [ Links ]
20. Hämmerle Ch, Araujo M, Simion M. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Impl Res.23 (Suppl. 5), 2012:80-82. [ Links ]
21. Chen S, Darby I, Reynolds E. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin. Oral Impl. Res. 2007; 18: 552-562. [ Links ]
22. Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martín C, Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Impl. Res 2012; 23 (Suppl. 5): 22-38. [ Links ]
23. Orgeas G, Clementini M, De Risi V, Sanctis M. Surgical techniques for alveolar socket preservación: A systematic review. Int J Oral Maxillofac Implants. 2013; 28:1049-1061 [ Links ]
24. Favero G, Botticelli D, Favero G, García B, Mainetti T, Lang N. Alveolar bony crest preservation at implants installed immediately after tooth extraction: an experimental study in the dog. Clin Oral Impl. Res. 2003; 24: 7-12 [ Links ]
Received: March 28, 2017; Accepted: July 11, 2017











 text in
text in