Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.18 no.28 Montevideo nov. 2016
Erupted odontoma: a case report and a literature review
de Pró Lizuaín Carlos*, Fungi Monetti Myriam**, Beovide Cortegoso Verónica***
* Assistant Prof. Anatomic Pathology Department, School of Dentistry, Universidad de la República. Uruguay.
cardepro@hotmail.com
** Assistant Professor, Anatomic Pathology Department, School of Dentistry, Universidad de la República. Uruguay.
*** Professor. Anatomic Pathology Department, School of Dentistry, Universidad de la República. Uruguay.
Abstract
Odontomas are classified by the WHO as odontogenic tumors composed of enamel, dentin, cement and pulp, considered hamartomatous lesions rather than true neoplasms. In exceptional cases, odontomas erupt into the oral cavity.
This study reports a case of odontoma spontaneously exposed to the oral cavity, which is known as “erupted odontoma”, in a 22-year-old male patient. A review of the literature between 1980 and 2015 of the existing cases of this pathology is also presented.
Keywords: Odontogenic tumors, odontomas, Erupted odontoma.
Received on: 16 Jun 16 – Accepted on: 30 Aug 16
Introduction
Maxillary tumors of odontogenic origin are lesions that occur only on both jaws and that arise from odontogenic tissue.
They have clinical and histological peculiarities. In its 2005 classification, the WHO divides odontogenic tumors into three groups: odontogenic epithelial tumors with mature stroma without odontogenic ectomesenchyme, odontogenic epithelial tumors with ectomesenchyme with or without hard tissue formation, and tumors with mesenchyme and/or ectomesenchyme with or without odontogenic epithelium.
Odontomas fall into the third category and are considered benign malformations (hamartomas) composed by dental tissue and ectomesenchymal cells (1, 2).
Background
Broca was the first person who used the term odontoma in 1867 in a broad sense to refer to any tumor of odontogenic origin. Although the WHO classifies them as benign odontogenic tumors, odontomas are considered hamartomas or development defects rather than true neoplasms (1). They are the most frequent non-cystic odontogenic lesions and account for between 22 % and 67 % of all odontogenic tumors (3).
Odontomas are formed by enamel, dentin, cementum and pulp, and are classified into compound odontomas and complex odontomas. There are also mixed lesions (compound-complex odontomas). Compound odontomas (CpOD) display dental tissues in an organized manner and might present tooth-like structures known as denticles. Complex odontomas (CxOD) present all dental tissues but they are haphazardly arranged (2, 4, 5).
Clinically, odontomas can be classified into central (intraosseous), peripheral (extraosseous), and erupted (6). Central odontomas are the most frequent odontogenic tumors. Peripheral odontomas occur only in the soft tissue covering the mandible and maxilla. Erupted odontomas are intraosseous odontomas that appear exceptionally in the oral cavity through processes discussed below.
Odontomas grow slowly, are usually asymptomatic, and occur most frequently in the maxilla. They are usually detected during the first two decades of life, within an age range of 6 to 46. Shafer reports an average age of 23 and no sex predilection (7).
They are often detected on routine radiographies or when lack of eruption or delayed eruption is investigated. Most are linked to tooth malformation, impaction, malposition or delayed eruption.
In some cases it can cause pain, bone plate expansion, tooth displacement, lip numbness and swelling (7). Some patients with erupted odontomas have reported pain on account of infection in deeply impacted third molars (8).
On a radiography, these lesions appear radiopaque, well-defined, denser than bone and surrounded by a radiolucent rim representing the connective tissue of the dental follicle. As these elements go through several calcification stages, their appearance through imaging techniques depends on their stage of development. CpOD appear as unilocular lesions that may have multiple tooth-like structures known as denticles. CxOD are solid radiopaque, sometimes papilliform masses, surrounded by a thin radiolucent layer that separates them from the surrounding bone (2, 4, 5).
Histollogically, CpOD have a fibrous capsule of connective tissue which surrounds denticles, formed by pulp tissue, surrounded by primary or immature dentin, partially demineralized enamel and primary cementum.
CxOD have an external capsule of fibrous connective tissue, and the calcified tissue is formed mainly by primary or immature dentin, enamel with different degrees of calcification and immature cementum (9, 10).
The etiology of odontomas is not clear, and various theories have been suggested: local trauma during primary dentition, inflammatory and infectious processes, hereditary anomalies and alteration in genetic components responsible for tooth development (11).
Hitchin (1971) suggests that odontomas are inherited through the mutation of a gene in charge of tooth development, possibly after birth. The dental lamina that gives rise to dental germs usually disappears after fulfilling its function. However, some of it might remain, known as rests of Serres. These rests may have a major role in odontoma etiology, as both CpOD and CxOD might appear where a tooth should be. A mutation in the epithelial cells that form dental lamina or germ rests may change the capacity of odontogenic epithelium to go through the cap and bell stages necessary for tooth formation and yet retain its ability to stimulate the mesenchymal differentiation necessary for dentin formation and to form functional ameloblasts and odontoblasts, which leads to the formation of an odontoma (12).
Clinical case
Male 22-year old patient that attends the Oral and Maxillofacial Surgery Clinic I at the School of Dentistry of the Universidad de la República Oriental del Uruguay on account of a swelling on the mandible affecting teeth 36 to 38. No relevant medical or family history.
Upon clinical examination, a swelling was detected. It deformed both mandibular cortical bones, exposing a yellowish hard matter, with an irregular surface and which resembled dentin tissue. There were no pain or infection symptoms (Fig. 1).

Fig. 1 – Irregular mass deforming both mandibular cortical bones
The panoramic radiograph showed a 3.6 cm x 3 cm compact radiopaque mass surrounded by a thin radiolucent area. The first left lower molar was retained underneath the mineralized mass. Upper molars were in contact with the mass (Fig. 2)

Fig. 2 – Panoramic radiograph showing radiopaque mass with radiolucent rim
The surgery was performed intraorally under local anesthesia: the lesion was removed and the first retained molar preserved to allow for eruption.
Upon histopathological examination, we detected enamel, dentin and pulp matrix: an erupted complex odontoma according to its clinical-pathological features (Fig. 3).
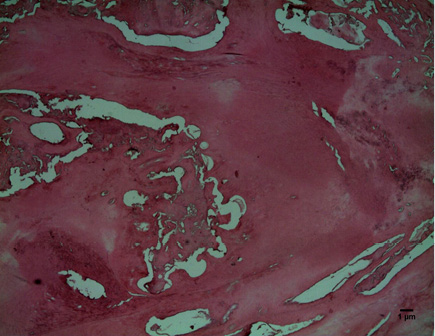
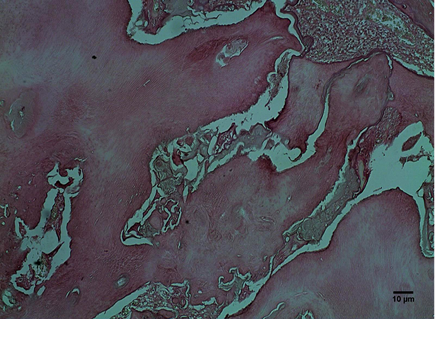
Fig. 3 – enamel, dentin and pulp matrix A: HE 40 and B: HE 100X
A panoramic radiograph was taken after 2 years to follow up on the patient. It showed good bone repair and the first left lower molar in advanced eruption (Fig. 4).
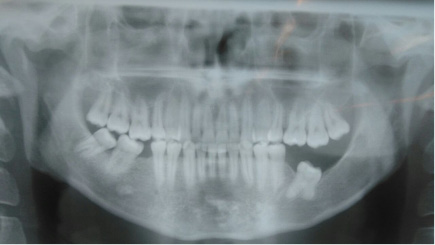
Fig. 4 – Control panoramic radiograph
Discussion
The WHO classifies odontomas as benign mixed odontogenic tumors. Given their behavior, they are considered hamartomatous lesions arising from dental tissues (2). Their frequency varies depending on the report: between 22 % and 67 % of odontogenic tumors (3, 13, 15). They account for 30 % of odontogenic tumors in the Anatomic Pathology Department of the School of Dentistry, Universidad de la República, Uruguay.
Clinically, odontomas can be classified into central (intraosseous), peripheral (extraosseous), and erupted (6).
Erupted odontomas are intraosseous lesions that appear in the oral cavity. Most are connected with a retained tooth, usually a second molar. This is why some authors suggest that the eruptive force of these teeth may impact odontoma eruption (6).
It is actually inaccurate to say that there is odontoma eruption, as the process seems to be different from tooth eruption. This is due to the lack of periodontal ligament and root. The strength necessary to remove an odontoma is not connected to fibroblast contractility as is the case with teeth. Although an odontoma has no root, its increasing size might lead to pressure-related resorption of the overlying bone and to its exposure. Odontoma eruption in the oral cavity might also be explained by bone remodeling in an edentulous area: the bone decreases in height until the odontoma is exposed (13).
Erupted odontomas are rare lesions: the first case was reported in 1980 by Rumel et al. (14). In their 2005 literature review, Junquera et al. (6) cite an average age of 20.3 years, with a 9 to 59 range. Most odontomas appeared in the maxilla and were complex. Serra-Serra et al., 2009 (13) present a review of 20 cases of erupted odontoma. The average patient age was 25.35 years; most appeared in women and were of the complex type.
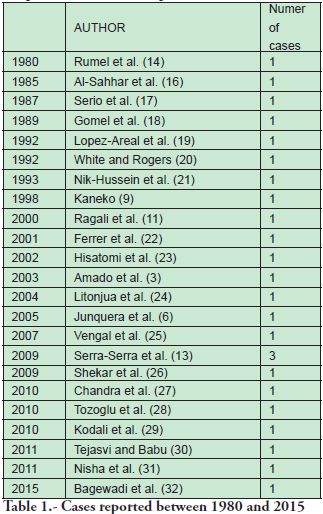
In our PubMed literature review covering cases between 1980 and 2015, we found 33 erupted odontomas reported (Table 1).
Although the papers reviewed (Table 1) do no report all the clinical-pathological data, it is reported that 59.25 % of erupted odontomas appear in the mandible, between the ages of 8 and 27, the average age being 17.6, there being no significant sex predilection. Histologically, complex odontomas are most frequent: 42.4 % of erupted odontomas.
In our cases, of 107 odontomas, 1.8 % were erupted odontomas (n 2), the average patient age was 15, one female with a compound odontoma on the maxilla, and one male with a complex odontoma on the mandible.
In this report we discuss the case of a male 22-year-old patient, with a complex erupted odontoma on the mandible, over the first retained molar. No symptoms were reported.
The lesion was removed and the impacted tooth preserved. This required the clinical and radiographic follow-up of the patient for at least a year. If there are no changes in tooth position, the tooth is surgically exposed and orthodontic traction is performed. Extraction is recommended when the retained tooth is ectopic or heterotopic, with morphological alterations, or when it presents cystic lesions (13, 23). In this case the odontoma was removed, which allowed the molar to erupt normally.
Conclusions
Odontomas are the most frequent benign lesions, and they rarely erupt into the oral cavity. Erupted odontomas are mainly complex, appear later in life than other odontomas, and are usually linked to impacted teeth. They might present pain, inflammation and infection.
The treatment selected was surgical removal with tooth preservation to facilitate its eruption, which might be spontaneous or favored by surgical exposure and orthodontic traction.
Acnowledgements
To Dr. Pablo Scarrone, Surgeon at the Surgical Department I, School of Dentistry of the Universidad de la República, Uruguay, for providing the clinical data on the case presented.
Referencias
2. Barnes L, Everson JW, Reichart P, Sidransky D. Eds., World Health Organization Classification of Tumours. Pathology and Genetics of E558 Head and Neck Tumours. Lyon: IARC Press, 2005
3. Amado Cuesta S, Gargallo Albiol J, Berini Aytes L, Gay Escoda C. Revisión de 61 casos de odontoma. Presentación de un odontoma complejo erupcionado. Med Oral 2003; 8:366-73
4. Philipsen H, Reichart P, Praetorius F. Mixed odontogenic tumours and odontomas. Considerations on interrelationship. Review of the literature and presentation of 134 new cases of odontomas. Oral Oncol
1997;32:86-99.
5. Kramer JRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumours. WHO International Histological Classification of tumours. Berlin: Springer-Verlag; 1992.p. 21
6. Junquera L, de Vicente JC, Roig P, Olay S, Rodriguez-Recio O. Intraosseous odontoma erupted into the oral cavity: An unusual pathology. Med Oral Pathol Oral Cir Bucal 2005; 10:248-51
7. Shaffer WG, Hine BM, Levy MK . Cyst and Tumours of the Jaws. En: A Textbook of Oral Pathology. 4ed. Philadelphia: WB Saunders, 1997.p308-311
8. Bertolai R, Acocella A, Sacco R, Agostini T. Submandibular cellulitis (Ludwig’s angina) associated to a complex odontoma erupted into the oral cavity. Case report and literature review. Minerva Stomatol.
2007 Nov-Dec; 56(11-12):639-47.
9. Kaneko M, Fukuda, M, Sano T, Ohnishi T, Hosokawa Y. Microradiographic and microscopic investigation of a case of complex odontoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85:131-4
10. Patiño Illa C, Berini Aytés L, Sanchez Garcés MA, Gay Escoda C. Odontomas complejos y compuestos: Análisis de 47 casos. Arch Odontoestomatol 1995; 11:423-9.
11. Ragalli CC, Ferreira JL, Blasco F. Large erupting complex odontoma. Int JOral Maxillofac Surg 2000; 29(5):373-4.
12. Hitchin AD. The aetiology of the calcified composite odontomas. Br Dent J 1971; 130(11):475-82
13. Serra- Serra G, Berini-Aytes L, Gay- Escoda C. Erupted odontomas: a report of three cases an review of the literature. Med Oral Patol Oral Cir Bucal 2009; 14(6): 1-5
14. Rumel A, de Freitas A, Birman EG, Tannous LA, Chacon PT, Borkas S. Erupted complex odontoma. Report of a case. Dentomaxillofacial Radiol 1980; 9(1): 5-9
15. Daley TD, Wysocky GP, Pringle GA. Relative incidence of odontogenic tumors and oral jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol 1994;77:276-8
16. Al Sahhar WF, Putrus ST. Erupted odontomas. Oral Surg Oral Med Oral Pathol 1985; 59:225-6
17. Serio FG, Levy BA. Erupted compound odontoma. Review and report of case. Ann Dent 1987; 46:41-2
18. Gomel M, Secki T. An erupted odontoma: case report J Oral Maxillofac Surg 1989; 47:999-1000
19. Lopez –Areal L, Silvestre Donat F, Gil Lozano J. Compound odontoma erupting in the mouth: 4 years follow up of a clinical case. J Oral Pathol Med 1992; 21:285-8
20. White CS, Rogers J. Erupted compound odontoma: review and case report. Gen Dent. 1992 Jan-Feb; 40(1):43-4.
21. Nik-Hussein NN, Majid ZA. Erupted compound odontoma. Ann Dent 1993. Winter, 52(2):9-11.
22. Ferrer M, Silvestre F, Estelles E, Grau D. Infección recurrente de un odontoma complejo tras su apertura a la boca. Med Oral 2001; 6:269-75
23. Hisatomi M, Asaumi J, Konouchi H, Honda Y, Wasaka T, Kishi K. A case of complex odontoma associated with an impacted lower deciduous second molar and analysis of the 107 odontomas. Oral
Dis.2002; 8:100-5
24. Litonjua LA, Suresh L, Valderrama LS, Neiders ME. Erupted complex odontoma: a case report and literature review. Gen Dent. 2004 May-Jun; 52(3):248-51.
25. Vengal M, Arora H, Ghosh S, Pai KM. Large erupting complex odontoma: a case report. J Can Den Assoc 2007; 73:169- 71
26. Shekar SE, Rao R, Gunasheela B, Supriya N. Erupted compound odontome. J Oral Maxillofac Pathol 2009 Jan-Jun; 13(1):47-50. Disponible en: https://dx.doi.org/10.4103%2F0973-029X.48758
27. Chandra S, Bagewadi A, Kelushkar V, Sah K. Compound composite odontoma erupting into the oral cavity. Contemp Clin Dent. 2010; 1(2):123-6
28. Tozoglu S, Yildirim U, Buyukkurt MC. An erupted complex odontoma. State Dent J. 2010 Aug-Sep; 76(5):52-3
29. Kodali R, Venkat B, Ramanjaneya P, Vora S. An unusual complex Odontoma. J Maxillofac Oral Surg[en línea]. 2010; 9(3):314-317. Disponible en: https://dx.doi.org/10.1007%2Fs12663-010-0085-9
30. Tejasvi A, Babu B. Erupted compound Odontomas: A case report. J Dental Research, Dental Clinic, Dental Prospects. 2011; 5(1):33-36. Disponible en:https://dx.doi.org/10.5681%2Fjoddd.2011.007.
31. Nisha D, Rishabh K, Ashwarya T, Sukriti M, Gupta SD. An unusual case of erupted composite complex odontoma. J Dent Sci Res 2011; 2(2):5-9. Disponible en:
https://dx.doi.org/10.1155%2F2013%2F570954
32. Bagewadi S, Kukreja R, Gundareddy S, Yadav B, Sharma H. Unusually large erupted complex odontoma: A rare case report. Imag Sci Dent 2015; 45: 49-54











 texto en
texto en