Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.18 no.28 Montevideo nov. 2016
Endocrowns: A retrospective patient series study, in an 8-to-19-year period
Borgia Botto, Ernesto*, Barón, Rosario**, Borgia Botto, José Luis***
*
Professor, Postgraduate Degree in Comprehensive Restorative Dentistry,
Post-graduate School, School of Dentistry, Universidad de la República.
Montevideo, Uruguay.
E-mail: eborgiabotto@gmail.com
** Associate Professor, Operative Dentistry Clinical Department, School of Dentistry, Universidad de la República. Montevideo, Uruguay.
*** Assistant Professor, Prosthodontics Clinic, School of Dentistry, Universidad de la República. Montevideo, Uruguay.
Abstract
Purpose. The aim of this paper is to present the retrospective clinical performance of 11 endocrowns, placed in a single private practice in an 8-to-19-year period. Materials and Methods. Inclusion and exclusion criteria for the sample and the restorations were established. One hundred and thirty patients were selected at random. Eleven endocrowns had been placed in 11 patients. Three restorative materials and three resin cements were used. Cohen’s Kappa coefficient, on the quality analysis of the restorations, ranged from 0.78 to 1. Due to the small sample, inferential statistical methods could not be used. Therefore, statistical descriptive methods were applied. Results. At the moment of the clinical examination, 10 (90.9%) endocrowns were in function and 1 failed (9.1%). Conclusions. Endocrown is a conservative and aesthetic technique-sensitive procedure used to restore posterior endodontically treated teeth, mainly molars, with a very good biomechanical and functional performance, and very acceptable longevity.
Keywords: Endodontically treated teeth, bonded onlays, restoration without post, aesthetic, adhesion.
Disclosure
The authors declare no conflicts of interest related with this study.
Received on: 31 May 16 – Accepted on: 30 Aug 16
Introduction
The rehabilitation of posterior endodontically treated teeth (PETT) always poses a challenge to dentists. Biological factors (periodontal and/or endodontic prognosis, assessment of the individual caries risk, root anatomy and coronal remnant tissues) and functional factors (gender, parafunctional habits, location of the tooth in the dental arch and the role of the tooth in the whole treatment), must be considered before making a treatment decision. Therefore, in some clinical situations, the restorative procedure arises from a multidisciplinary and/or interdisciplinary approach.
Moreover, clinical studies have shown no statistically significant differences in the success rate of endodontically treated teeth (ETT) restored with or without posts (1-4). One of the options to restore a PETT without posts is the restorative procedure introduced by Pissis in 1995 (5), described as the “mono-block porcelain technique”, later known as Endocrown (EC). Pressed lithium-disilicate ceramic, CAD-CAM feldspathic ceramic, CAD-CAM lithium-disilicate ceramic and CAD-CAM resin nanoceramic are the materials and techniques more widely used for ECs nowadays (6).
Nevertheless, clinical studies are scarce and there is not enough scientific-based evidence. There are some reports of one or two clinical cases (7-9) and a few longitudinal clinical studies that do not extend beyond twelve years (10-13). Therefore, it might be interesting to discuss the clinical results of a small but well-documented group of patients with ECs.
The clinical examination was performed with a mirror and a sharp explorer. An x-ray was taken in each PETT. The assessment of the restorations was blind between the authors. Cohen’s Kappa Coefficient (14) on the quality of the restorations and the radiographic examination ranged from 0.78 to 1 [(excellent according to Fleiss guidelines (15)]. In cases of disagreement regarding quality assessment of the restorations, the lowest rating was recorded.
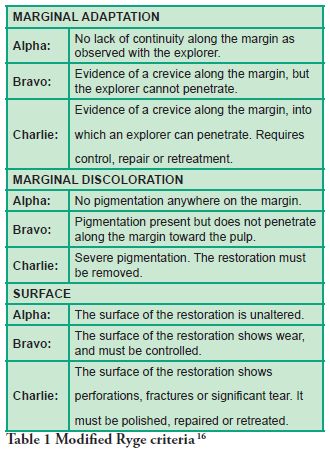
Marginal Adaptation, Marginal Discoloration and Surface were the variables studied to establish the quality of the restorations, following Ryge criteria (16) as modified by the authors (Table 1).
The Success Criteria were defined by the authors according modified Ryge criteria and the statements of Anusavice (17) and grouped as follow:
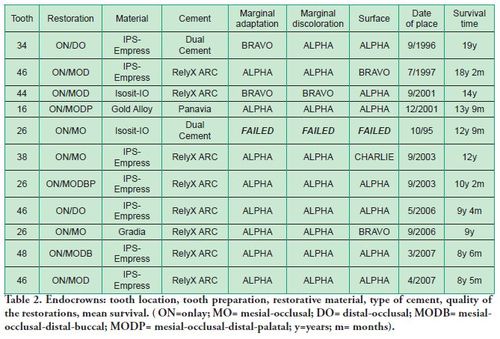
Three restorative materials and three resin cements were used (Table 2).
At the time of the examination, 10 (90.9%) ECs were in function in 10 patients. One EC had been lost after 12 years and 9 months due to periodontal disease in tooth #26. No restoration had loosened. Neither secondary caries nor radiographic failures were observed in the 10 PETT in function (Figs. 1a,1d; 2c; 3c,3d; 4c).
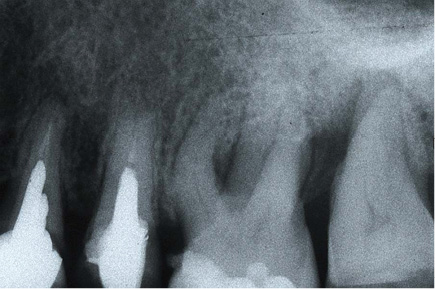
Fig. 1a Initial state in tooth #26. Buccal-Distal root must be resected.
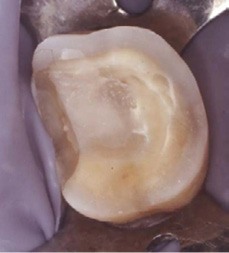
Fig. 1b Tooth preparation for EC in #26.

Fig. 1c EC after 9 years (Gradia, GC Corp., Japan)), (SC = Ex).
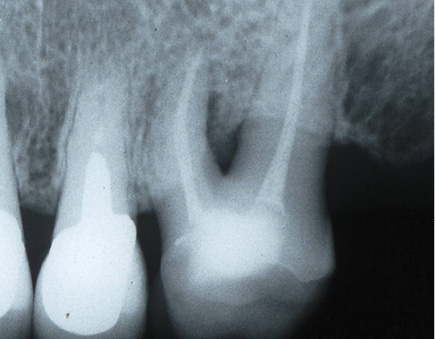
Fig. 1d X-ray control after 9 years.
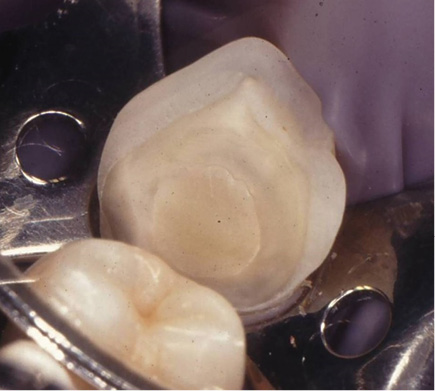
Fig. 2a Preparation for EC in tooth #34.

Fig.
2b EC in #34 after 19 years (IPS-Empress, Ivoclar, Vivadent,
Liechtenstein). The glass-ionomer in gingival had a survival time of 23
years and needed to be repaired
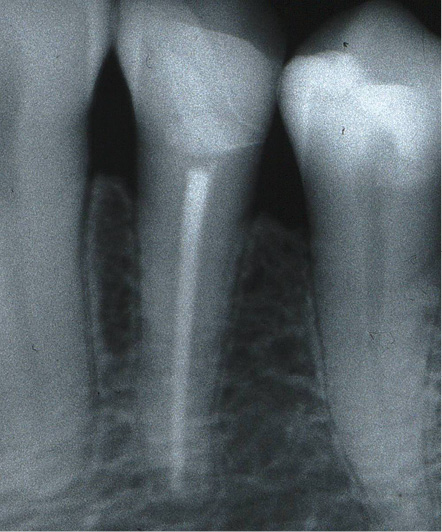
Fig. 2c X-ray control after 19 years.

Fig. 3a Preparation for EC in tooth #46. A chamfer was performed on buccal wall.

Fig.
3b EC after 18 years (IPS-Empress, Ivoclar, Vivadent, Schaan,
Liechtenstein). Note the parafunctional wear facets, the gingival
recession and the non-carious cervical lesion. This patient refused to
wear nocturnal stabilization splint, (SC = G).

Fig. 3c Final control of endodontic treatment.
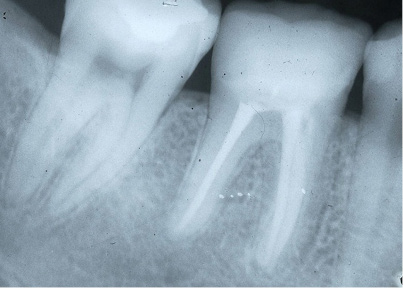
Fig. 3d X-ray control after 18 years.

Fig. 4a Preparation for EC in tooth #26. A chamfer was performed on buccal, distal and palatal walls.

Fig. 4b EC after 10 years (IPS-Empress) (SC = Ex).
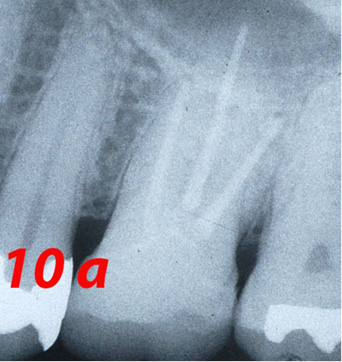
Fig. 4c X-ray control after 10 years (a=years).
Three ECs in function were placed in maxillary molars, 5 in mandibular molars and 2 in mandibular premolars, yielding a ratio of 4.0 molars/premolars (Table 2).
Two small “chippings” in occlusal surfaces were polished. However, the Success Criteria on the quality of the restorations was rated as follows: Excellent 5 (50%), Good 4 (40%) and Functional Survival 1 (10%) (Table 2).
Five patients (50%) underwent maintenance therapy at least once a year.
There is not enough scientificbased evidence on the clinical performance of EC. In fact, longitudinal clinical studies are scarce. Lander and Dietschi (7) presented 2 successful cases in a 3 year-period; Biacchi et al (8) one case in a 3 year-period and Fages and Bennasar (9) one case without a follow-up. After one year, Otto (10) found that Bravo increased from 30% to 55% on Marginal Adaptation in 10 EC. Meanwhile, Bernhart et al (11) in 20 ECs, had a success rate of 90% in two years.
In this paper, 90.9% (10) of ECs remained in function, with an observed mean survival time of 12 years and 3 months. Considering the quality of the restorations in function, 90% of Clinical Success was observed. This is better than the result reported in four articles reviewed (7-10) and could be similar or better than Bernhart et al (11) if we consider the high percentage of failures observed in only two years.
On the other hand, Otto and Mörmann (12) in 25 ECs had a success rate of 90.5% in molars and 76% in premolars up to 12 years, and Bindl et al (13) in a 7-year-long prospective study of 86 ECs (70 molars and 16 premolars), the success rate was 80% in molars and 68.8% in premolars. These authors concluded that ECs appeared inadequate for premolars.
Considering the ratio molar/premolar in this work, it was similar to Otto and Mörman (12) and Bindl et al (13). The location in the dental arches didn’t influence the clinical outcome in this study. Moreover, the percentage of ECs in function was similar to that observed by Otto and Mörmann (12) and higher than the results in Bindl et al (13). Besides, 14 ECs were loosening in Bindl et al (13) and none in this paper.
Therefore, the clinical results in this paper were better or similar than the results reported in the articles reviewed (7-13). In spite of this, differences in sample sizes between this study and two articles abovementioned (12, 13) could restrict the comparisons made.
On the other hand, several clinical studies concluded that the coronal remnant was the most important factor in the clinical success of ETT (18-21). Therefore, a conservative approach is essential in tooth preparation for EC. According to the above definition, the entire occlusal surface must be covered by the restoration. Onlays mainly transmit compressive forces on the tooth-restoration adhesive interface, improving biomechanical behavior (22-4). A 3 mm of occlusal reduction was suggested (25): a higher fracture resistance was found when increasing occlusal thickness (26). Furthermore, if the buccal and/or palatal/lingual walls have a thickness greater than 2.0 mm, a 1.2 mm chamfer in the occlusal wall could have a ferrule effect, improving the fracture resistance of the teeth and the retention of the restoration (Figs. 3a, 4a).
The inner walls of the coronal portion and the pulp chamber must have an occlusal divergence greater than 60. Retentions or undercuts must be locked with glass-ionomer cement and a layer of this cement was dispensed in the floor of the pulp chamber. In this study, four preparations had three coronal walls (Figs. 1b, 2a), four had two walls (Fig. 3a) and two covered at least four surfaces. Besides, extending the preparation to the buccal surface is only considered for aesthetic reasons or given reduced dimensions of the wall. In the latter situation, 1.2 mm of axial reduction in the buccal wall with a chamfer finish line was performed (Fig. 4a). These criteria are not in accordance with the total coronal reduction proposed by Fages and Benassar (9).
Meanwhile, when proximal boxes must be performed, they must follow the established protocols for bonded ceramic inlays/onlays (27,28). The authors disagree with Rocca and Krejci (29), who partially restore these surfaces with direct light-activated composite resin, increasing the number of interfaces and reducing the surface for bonding the EC.
Therefore, the above discussed criteria in teeth preparations and the presence and preservation of coronal teeth structure could have improved the clinical results in this study.
Furthermore, recent laboratory studies have shown: 1) teeth restored with ECs were potentially more resistant to failure than those with FRC posts (30, 31) or had similar fracture resistance (32-36); 2) by eliminating the use of a post and filling core, the number of adhesive bond interfaces is reduced, thus making the restoration less susceptible to the adverse effects of degradation of the hybrid layer (8), and 3) using resin nanoceramic blocks for the manufacture of ECs may result in better fracture resistance and a more favorable fracture mode than other investigated ceramic blocks, but more microleakage might be expected with this material (37).
Meanwhile, dual and chemical curing resin cements, performed better than light or self-etching curing resin cements, in laboratory and clinical research (38-44). Nevertheless, increasing the exposure time through different thickness of ceramic materials and using high power light-emitting diode (LED) curing units, recent laboratory studies have found a greater degree of conversion and after 24 hours, greater microhardness values in light and dual-polymerization resin cement (45, 46). Therefore, the clinical procedures and the types of cements used, could have influenced the good Clinical Success (90%), (Figs. 1c, 2b, 3b, 4b).
In a recent publication, bruxism was statistically found as the highest factor risk of fractures in ETT (47). In the present paper, 7 patients (70%) had or had had history of parafunction, which is in relative accordance with epidemiological studies of bruxism and TMD (48, 49). Moreover, when considering gender as a variable, men develop stronger forces than women (50). In this paper, gender could have improved the clinical outcome (ratio: 4.5 women/men). However, in the work of Bindl et al (13), the patients with a history of TMD were excluded from the sample. Therefore, this criterion might have improved their clinical results.
Besides, there were no secondary caries in this study. This outcome might be due to the fact that individual caries risk was assessed, the patients were enrolled in a comprehensive prevention plan and ongoing periodical maintenance therapy. Still, only 50% of the patients attended the clinic at least once a year.
The variables age, restorative material and maintenance therapy, cannot be studied in this work, due to the small sample and only one restoration failed.
Therefore, EC can be indicated in almost all cases of PETT, mainly molars, especially in short crowns, calcified root canals and very slender roots. It is contraindicated when the thickness of the wall at the cervical margin is less than 2mm9.
Moreover, longevity of posterior restorations depends on factors related to the material, the patient and the operator (51, 52). In the present study, all restorations were performed by an experienced operator, which might have improved the clinical results.
Referencias
2. Creugers NH, Mentink AG, Fokkinga WA, Kreulen CM. 5-year follow-up of a prospective clinical study on various types of core restorations. Int J Prosthodont 2005;18:34-39.
3. Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported post-endodontic restoration: a prospective observational clinical study. J Endod 2012;38:432-435.
4. Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH. Up to 17-year controlled clinical study on post-and-cores and covering crowns. J Dent 2007;35:778-786.
5. Pissis P. Fabrication of a metal-free ceramic restoration utilizing the mono-block technique. Prac Periodontics Aesthet Dent 1995;5:83-94.
6. Ferencz JL, Silva NRFA, Navarro JM. High-strength ceramics. Interdisciplinary Perspectives. Quintessence Publishing Co Inc, 2014.
7. Lander E, Dietschi D. Endocrowns: A clinical report. Quintessence Int 2008;39:99-106.
8. Biacchi GR, Mello B, Basting RT. The endocrown: An alternative approach for restoring extensively damaged molars. J Esthet Restor Dent 2013;25:283-291.
9. Fages M, Bennasar B. The endocrown: a different type of all-ceramic reconstruction for molars. J Can Dent Assoc 2013;79:d140
10. Otto T. Computer-aided direct all-ceramic crowns: preliminary 1-year results of a prospective clinical study. Int J Periodontics Restorative Dent 2004;24:446-455.
11. Bernhart J, Bräuning A, Altenburger MJ, Wrbas KT. Cerec 3D endocrowns-two-year clinical examination of CAD/CAM crowns for restoring endodontically treated molars. Int J Comput Dent 2010;2:142-154.
12. Otto T, Mörmann WH. Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int J Comput Dent 2015;2:147-161.
13. Bindl A, Richter B, Mörmann WH. Survival of Ceramic Computer-aided Design/Manufacturing Crowns Bonded to Preparations with Reduced Macroretention Geometry. Int J Prosthodont 2005;18:219-224.
14. Cohen J. Weighed Kappa: Nominal scale agreement with prevision for scaled disagreement or partial credit. Psychological Bulletin, 1968;70:213-220.
15. Fleiss J L. Statiscal methods for rates and proportions (2nd. Ed), New York: John Wiley, 1981:38-46.
16. Ryge G. Clinical criteria. Int Dent J 1980;30:347-358.
17. Anusavice K. Standardizing failure, success and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent Mat 2012;
28:102-111.
18. Hikasa T, Matsuka Y, Mine A, Minakuchi H, Hara ES, Van Meerbeek B, Yatani H, Kuboki T. A 15-year clinical comparative study of the cumulative survival rate
of cast metal core and resin core restorations luted with adhesive resin cement. Int J Prosthodont 2010;23:397-405.
19. Weine FS, Wax AH, Wenckus CS. Retrospective study of tapered, smooth post system in place for 10 years or more. J Endod 1991;17:293-297.
20. Jung RE, Kalkstein O, Sailer I, Roos M, Hämmerle ChHF. A comparison of composite post buildups and cast gold post-and-core buildups for the restoration of
non vital teeth after 5 to 10 years. Int J Prosthodont 2007;20:63-69.
21. Gómez-Polo M, Llidó B, Rivero A, Del Río J, Celemín A. A 10-year retrospective study of the survival rate of teeth restored with metal prefabricated posts
versus cast metal posts and cores. J Dent 2010;38:916-920.
22. Magne P, Belser UC. Porcelain versus composite inlays/onlays : effects of mechanical loads on stress distribution, adhesion and crown flexure. Int J Periodontics Restorative Dent 2003; 23:543-555.
23. Kececi AD, Heidemann D, Kurnaz S. Fracture resistance and failure mode of endodontically treated teeth restored using ceramic onlays with or without fiber
posts-an ex vivo study. Dent Traumatol 2015;doi: 10.1111/edt. 12252.
24. Yamada Y, Tsubota Y, Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont 2004;17:
94-98.
25. Sevimli G, Cengiz S, Oruc MS. Endocrowns: Review. J Istanbul Univ Fac Dent 2015;2:57-63.
26. Mörmann WH, Bindl A, Lüthy H, Rathke A. Effects of preparation and luting system on all-ceramic computer-generatedcrowns. Int J Prosthodont
1998;11:333-339.
27. Borgia E. Restauraciones Indirectas Adheridas Posteriores. In: Henostroza Haro G (ed). Adhesión en Odontología Restauradora . España: M. Ripano S.A,
2010:389-430.
28. Dietschi D, Spreafico R. Tooth preparation. In: Dietschi D, Spreafico R. Adhesive Metal-Free Restorations. Current Concepts for the esthetic treatment of posterior
teeth. Germany: Quintessence, 1997:88-99.
29. Rocca GT, Krejci I. Crown and post-free adhesive restorations for endodontically treated posterior teeth: from direct composite to endocrowns. Eur J Esthet Dent
2013;8:156-179.
30. Dejak B, Mlotkowski A. 3D-finite element analysis of molars restored with endocrowns and posts during masticatory simulation. Dent Mater 2013;12:309-317
31. Biacchi GR, Basting RT. Comparison of fracture strength of endocrowns and glass fiber post-retained conventional crowns. Oper Dent 2012;37:130-136.
32. Rocca GT, Saratti CM, Cattani-Lorente M, Feilzer AJ, Krejci I. The effect of a fiber reinforced cavity configuration on load bearing capacity and failure mode of
endodontically treated molars restored with CAD/CAM resin composite overlay restorations. J Dent 2015; 43:1106-1115.
33. Salameh Z, Ounsi HF, Aboushelib MN, Al-Hamdan R, Sadig W, Ferrari M. Effect of different onlay systems on fracture resistance and failure pattern of
endodontically treated mandibular molars restored with and without glass fiber posts. Am J Dent 2010; 23:81-86.
34. Carvalho AO, Bruzi G, Anderson RE, Maia HP, Giannini M, Magne P. Influence of adhesive core buildup designs on the resistance of endodontically treated
molars restored with lithium disilicate CAD/CAM crowns. Oper Dent 2016; 41:76-82.
35. Scotti N, Coero Borga FA, Alovisi M, Rota R, Pasqualini D, Berutti E. Is fracture resistance of endodontically treated mandibular molars restored with indirect
onlay composite restorations influenced by fibre post insertion? J Dent 2012; 40:814-820.
36. Magne P, Carvalho AO, Bruzi G, Anderson RE, Maia HP, Gianini M. Influence of no-ferrule and no-post buildup design on the fatigue resistance of endodontically
treated molars restored with resin nanoceramic CAD-CAM crowns.. Oper Dent 2014;6:595-602.
37. El-Damanhoury H, Haj-Ali R, Platt J. Fracture resistance and microleakage of endocrowns utilizing three CAD-CAM blocks. Oper Dent 2015;40(2):201-210.
38. Frankenberger R, Taschner M, García-Godoy F, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J. Adhes Dent
2008;10:393-398.
39. Cal E, Celik EU, Turkun M. Microleakage of IPS Empress 2 inlay restorations luted with self-adhesive resin cements. Oper Dent 2012;37:417-424.
40. Behr M, Hansmann M, Rosentritt M, Handel G. Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin Oral Investig
2009;13:459-464.
41. Uludag B, Ozturk O, Ozturk AN. Microleakage of ceramic inlays luted with different resin cements and dentin adhesives. J Prosthet Dent 2009;102:235-241.
42. Peumans M, Voet M, De Munck J, Van Landuyt K, Van Ende A, Van Meerbeeck B. Four-year clinical evaluation of a self-adhesive luting agent for ceramic inlays.
Clin Oral Invest 2013;17:739-750.
43. Taschner M, Krämer N, Lohbauer U, Pelka M, Breschi L, Petschelt A, Frankenberger R. Leucite-reinforced glass ceramic inlays luted with self-adhesive resin
cement: a 2-year in vivo study. Dent Mater 2012;28:535-540.
44. Lohbauer U, Pelka M, Belli R, Schmitt J, Mocker E, Jandt KD, Müller FA. Degree of conversion of luting resins around ceramic inlays in natural deep cavities: a
micro-Raman spectroscopy analysis. Oper Dent 2010;3:579-586.
45. AlShaafi MM, AlQahtani MQ, Price RB. Effect of exposure time on the polymerization of resin cement through ceramic. J Adhes Dent, 2014;16:129-135.
46. Gregor L, Bouillaguet S, Onisor I, Ardu S, Krejci I, Rocca GT. Microhardness of light- and dual-polymerizable luting resins polymerized through 7.5-mm-thick
endocrowns. J Prosthet Dent 2014;4:942-948.
47. Borgia Botto E, Barón R, Borgia, J L. Cast posts: a forty-four year retrospective clinical study in a specialized private practice. Odontoestomatología [online]
2015;17: 11-22 . Available from: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-93392015000100003&lng=en&tlng=en
48. Riva R, Sanguinetti M, Rodríguez A, Guzzetti L, Lorenzo S, Alvarez R, Massa F. Prevalencia de trastornos témporo mandibulares y bruxismo en Uruguay.
Odontoestomatología 2011;17:54-71.
49. Carlsson GE, MagnussonT. Epidemiologic studies of TMD. In: Carlsson GE, Magnusson T. Management of Temporomandibular Disorders in the general dental
practice. Quintessence,1999:13-17.
50. Arlan CV, Dimitriu B, Arlan VV, Bodnar D, Suciu I. Current opinions concerning the restoration of endodontically treated teeth: basic principles. J Med Life
2009;15:165-172.
51. Laegreid T, Gjerdet NR, Johansson A, Johansson A-K. Clinical decision making on extensive molar restorations. Oper Dent 2014;6:231-240.
52. Frankenberger R, Reinelt C, Petschelt A, Krämer N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent Mater 2009;25:960-968.











 texto en
texto en