Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.18 no.27 Montevideo maio 2016
Periodontal Plastic Surgery: A clinical case report
Bueno Rossy, Luis Alexandro*
* Professor in the Department of Periodontics and Director of the Postgraduate Degree in Periodontics. Universidad de la República. Uruguay. Specialist in Implant Dentistry. Universidad de Guarulhos. Brazil.
catedradeperiodoncia@gmail.com
Abstract
The therapeutic approach to gingival recession requires a treatment plan involving basic therapy, which will focus on its etiologies and the most suitable periodontal plastic surgery therapy in each specific case. Surgical procedures with connective-tissue grafts, taken mainly from the palate, are the gold standard in gingival recession treatment. The aim of this paper is to present the step-by-step post orthodontic therapy treatment of a case of gingival recession and its long-term evaluation.
Keywords:
Gingival recession, Periodontal plastic surgery, Post orthodontic treatment
Received on: 04 Nov 15 Accepted on: 30 Jan 16
Background
According to the American Academy of Periodontology, gingival recession is defined as the exposure of the tooth root caused by the migration of the gingiva to a point apical to the cementoenamel junction. This frequently compromises dental and gingival aesthetics, and causes dental hypersensitivity (1). It can appear in its localized or generalized form (2).
There are four types of factors that aid the development of gingival recession: anatomical factors (lack of keratinized gingiva, muscle insertion close to gingival margin, inadequate tooth alignment, thin or absent vestibular table, prominent root); factors relative to inflammatory disease (Gum disease because of plaque build-up, Periodontitis); factors relative to iatrogenesis (e.g. prosthetics, orthodontic treatment); factors relative to trauma (traumatic brushing or other mechanical traumas) (3).
The elimination of causal factors and the detailed explanation provided to the patient are as important as the periodontal plastic surgery technique to implement (4-6).
The most widely accepted classification of gingival recession is Miller’s. It is based on the most apical gingival margin of the recession regarding the mucogingival junction, and on the amount of tissue loss (gingiva and bone) in interproximal areas adjacent to the recession site (7).
Complete coverage is achieved when the gingival margin is placed at the same level as the cementoenamel junction, the gingival sulcus has a probing depth lower than 2 mm and when there is no bleeding on probing (8).
Connective tissue grafts are considered the gold standard in periodontal plastic surgery given their predictability, stability over time, increase in thickness and length of keratinized gingiva (9).
In 2015, the Workshop on Regeneration organized by the American Academy of Periodontology showed that the tissue thickness achieved when using connective-tissue grafts has more stable outcomes over time and there is lower recurrence of gingival recession (6).
Case description
A systemically healthy 28-year-old female patient, a non smoker, is referred to the Clinic of Periodontics of the School of Dentistry (Universidad de la República) in April 2011. She seeks consultation because she feels pain when brushing and has hypersensitivity to thermal changes on the labial area of an anteroinferior tooth. The patient underwent orthodontic treatment between 2006 and 2010. The symptoms she relates started after such treatment.
Upon examination, the following was observed on tooth 41:
• Miller's class II gingival recession (Figure 1),
• Localized gingival inflammation,
• Thin periodontal biotype,
• Lack of attached gingiva.
We explained the diagnosis and suggested treatment plan in detail to the patient: basic periodontal therapy and periodontal plastic surgery therapy by means of a connective-tissue graft. We also told her about other plastic surgery treatment options such as xenografts and homografts, and their advantages and disadvantages.
The basic therapy included:
• Instructing the patient regarding dental plaque control.
• Tartar removal, prophylaxis and use of a soft toothbrush and of the necessary interproximal cleaning devices for each sector.
This therapy lasted four sessions and the results can be seen in Figure 2.
The plastic surgery therapy selected was coronal repositioning of flap by means of a connective-tissue graft taken from the palate (10).
The surgical procedure was performed under local anesthesia. A partial-thickness flap was placed, with two vertical releasing incisions. The exposed root was mechanically prepared and irrigated with saline (Figure 3).
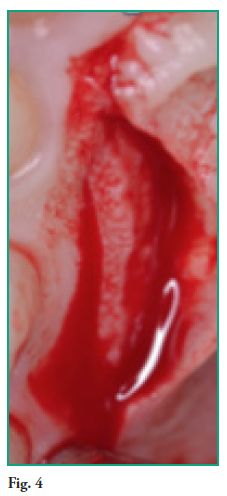
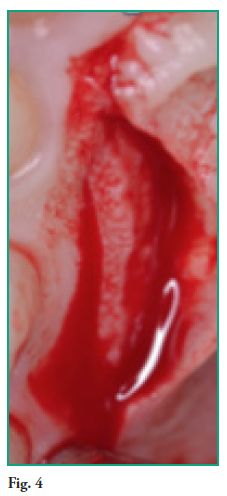
A connective-tissue graft was taken from the palate (Figure 4)(11). The graft was sutured on the recipient site using Vicril 5-0 suture (Ethicon, Johnson & Johnson) (Figure 5).
The flap was repositioned over the graft to cover it completely, 2 mm above the cementoenamel junction (Figure 6). Nylon 5-0 suture (Ethicon, Johnson & Johnson) was used.
The sutures were removed 14 days after the procedure, and the patient was prescribed Chlorhexidine Gluconate 0.12% oral rinse twice a day.
Two years after the treatment, gingiva stability and thickness seem adequate, which shows good hygiene of the sector and gingival tissue stability achieved with the graft (Figure 7).
The patient is grateful and satisfied with the treatment.
Discussion
The use of both connective-tissue grafts and their replacements, be them xenografts or homografts, might enable us to modify the thickness of gingival tissue (6).
In this case, the use of a connective-tissue graft made it possible to modify the thickness of the gingival tissue. This provided long-term root coverage, as described in the literature (3).
No complications were reported on any of the surgical sites (recipient and donor sites). The relevant literature states that there is a low incidence of complications (12).
In this case, connective tissue from the palate was used for three reasons: it is the gold standard, the donor site was good and the patient herself selected such option.
Coronally advanced flap without graft would not be indicated in this case as the gingival tissue was very thin.
The patient has adopted good hygiene practices, as seen in the periodontal check-ups conducted every 4 months. Dental plaque is removed professionally, which has also contributed to the positive outcomes achieved (3).
A recession reduction of at least 70% can be expected 2 or more years after the treatment (5, 13).
The literature describes better outcomes with maxilla grafts, where vestibular depth, flap tension and flap thickness are more favorable (14).
Selecting the best treatment according to scientific evidence led us to excellent clinical results.
We were able to modify the biotype on the surgical site with the connective-tissue graft, which resulted in the stability of the area. This was aided by the fact that the patient presented good dental plaque control practices.
Different surgical techniques are proposed for grafts: the envelope technique (Raetzke,1985; Allen, 1994), reposition of the flap partially covering a connective graft with an epithelial border (Langer; Langer), coronally advanced flaps with vertical releasing incisions (Nelson; Wennstrom); or without them (Bruno), or lateral sliding papillae flaps (Harris) (15-21). A coronally advanced flap with vertical releasing incisions was chosen given the local anatomic characteristics.
The exposed root in the recession area was treated with curettes, as there are no differences between this and other treatments (22).
By using connective tissue grafts or epithelial-connective grafts we can achieve the formation of a long junctional epithelium with a fibrous attachment (23, 24), although some studies report variable degrees of regeneration. New cementum was formed only in the areas where the cementum was preserved (25).






Conclusions
Basic periodontal therapy is fundamental when treating gingival recession. Subepithelial connective tissue grafts are the gold standard in periodontal plastic surgery as they modify tissue thickness, increase keratinized gingiva and improve root coverage. Periodontal maintenance is essential to avoid inflammatory events which might increase recession recurrence.
References
Bueno Rossy, Luis Alexandro*
* Professor in the Department of Periodontics and Director of the Postgraduate Degree in Periodontics. Universidad de la República. Uruguay. Specialist in Implant Dentistry. Universidad de Guarulhos. Brazil.
catedradeperiodoncia@gmail.com
Abstract
The therapeutic approach to gingival recession requires a treatment plan involving basic therapy, which will focus on its etiologies and the most suitable periodontal plastic surgery therapy in each specific case. Surgical procedures with connective-tissue grafts, taken mainly from the palate, are the gold standard in gingival recession treatment. The aim of this paper is to present the step-by-step post orthodontic therapy treatment of a case of gingival recession and its long-term evaluation.
Keywords:
Gingival recession, Periodontal plastic surgery, Post orthodontic treatment
Received on: 04 Nov 15 Accepted on: 30 Jan 16
Background
According to the American Academy of Periodontology, gingival recession is defined as the exposure of the tooth root caused by the migration of the gingiva to a point apical to the cementoenamel junction. This frequently compromises dental and gingival aesthetics, and causes dental hypersensitivity (1). It can appear in its localized or generalized form (2).
There are four types of factors that aid the development of gingival recession: anatomical factors (lack of keratinized gingiva, muscle insertion close to gingival margin, inadequate tooth alignment, thin or absent vestibular table, prominent root); factors relative to inflammatory disease (Gum disease because of plaque build-up, Periodontitis); factors relative to iatrogenesis (e.g. prosthetics, orthodontic treatment); factors relative to trauma (traumatic brushing or other mechanical traumas) (3).
The elimination of causal factors and the detailed explanation provided to the patient are as important as the periodontal plastic surgery technique to implement (4-6).
The most widely accepted classification of gingival recession is Miller’s. It is based on the most apical gingival margin of the recession regarding the mucogingival junction, and on the amount of tissue loss (gingiva and bone) in interproximal areas adjacent to the recession site (7).
Complete coverage is achieved when the gingival margin is placed at the same level as the cementoenamel junction, the gingival sulcus has a probing depth lower than 2 mm and when there is no bleeding on probing (8).
Connective tissue grafts are considered the gold standard in periodontal plastic surgery given their predictability, stability over time, increase in thickness and length of keratinized gingiva (9).
In 2015, the Workshop on Regeneration organized by the American Academy of Periodontology showed that the tissue thickness achieved when using connective-tissue grafts has more stable outcomes over time and there is lower recurrence of gingival recession (6).
Case description
A systemically healthy 28-year-old female patient, a non smoker, is referred to the Clinic of Periodontics of the School of Dentistry (Universidad de la República) in April 2011. She seeks consultation because she feels pain when brushing and has hypersensitivity to thermal changes on the labial area of an anteroinferior tooth. The patient underwent orthodontic treatment between 2006 and 2010. The symptoms she relates started after such treatment.
Upon examination, the following was observed on tooth 41:
• Miller's class II gingival recession (Figure 1),
• Localized gingival inflammation,
• Thin periodontal biotype,
• Lack of attached gingiva.
We explained the diagnosis and suggested treatment plan in detail to the patient: basic periodontal therapy and periodontal plastic surgery therapy by means of a connective-tissue graft. We also told her about other plastic surgery treatment options such as xenografts and homografts, and their advantages and disadvantages.
The basic therapy included:
• Instructing the patient regarding dental plaque control.
• Tartar removal, prophylaxis and use of a soft toothbrush and of the necessary interproximal cleaning devices for each sector.
This therapy lasted four sessions and the results can be seen in Figure 2.
The plastic surgery therapy selected was coronal repositioning of flap by means of a connective-tissue graft taken from the palate (10).
The surgical procedure was performed under local anesthesia. A partial-thickness flap was placed, with two vertical releasing incisions. The exposed root was mechanically prepared and irrigated with saline (Figure 3).
A connective-tissue graft was taken from the palate (Figure 4)(11). The graft was sutured on the recipient site using Vicril 5-0 suture (Ethicon, Johnson & Johnson) (Figure 5).
The flap was repositioned over the graft to cover it completely, 2 mm above the cementoenamel junction (Figure 6). Nylon 5-0 suture (Ethicon, Johnson & Johnson) was used.
The sutures were removed 14 days after the procedure, and the patient was prescribed Chlorhexidine Gluconate 0.12% oral rinse twice a day.
Two years after the treatment, gingiva stability and thickness seem adequate, which shows good hygiene of the sector and gingival tissue stability achieved with the graft (Figure 7).
The patient is grateful and satisfied with the treatment.
Discussion
The use of both connective-tissue grafts and their replacements, be them xenografts or homografts, might enable us to modify the thickness of gingival tissue (6).
In this case, the use of a connective-tissue graft made it possible to modify the thickness of the gingival tissue. This provided long-term root coverage, as described in the literature (3).
No complications were reported on any of the surgical sites (recipient and donor sites). The relevant literature states that there is a low incidence of complications (12).
In this case, connective tissue from the palate was used for three reasons: it is the gold standard, the donor site was good and the patient herself selected such option.
Coronally advanced flap without graft would not be indicated in this case as the gingival tissue was very thin.
The patient has adopted good hygiene practices, as seen in the periodontal check-ups conducted every 4 months. Dental plaque is removed professionally, which has also contributed to the positive outcomes achieved (3).
A recession reduction of at least 70% can be expected 2 or more years after the treatment (5, 13).
The literature describes better outcomes with maxilla grafts, where vestibular depth, flap tension and flap thickness are more favorable (14).
Selecting the best treatment according to scientific evidence led us to excellent clinical results.
We were able to modify the biotype on the surgical site with the connective-tissue graft, which resulted in the stability of the area. This was aided by the fact that the patient presented good dental plaque control practices.
Different surgical techniques are proposed for grafts: the envelope technique (Raetzke,1985; Allen, 1994), reposition of the flap partially covering a connective graft with an epithelial border (Langer; Langer), coronally advanced flaps with vertical releasing incisions (Nelson; Wennstrom); or without them (Bruno), or lateral sliding papillae flaps (Harris) (15-21). A coronally advanced flap with vertical releasing incisions was chosen given the local anatomic characteristics.
The exposed root in the recession area was treated with curettes, as there are no differences between this and other treatments (22).
By using connective tissue grafts or epithelial-connective grafts we can achieve the formation of a long junctional epithelium with a fibrous attachment (23, 24), although some studies report variable degrees of regeneration. New cementum was formed only in the areas where the cementum was preserved (25).






Conclusions
Basic periodontal therapy is fundamental when treating gingival recession. Subepithelial connective tissue grafts are the gold standard in periodontal plastic surgery as they modify tissue thickness, increase keratinized gingiva and improve root coverage. Periodontal maintenance is essential to avoid inflammatory events which might increase recession recurrence.
References
Conclusiones
La terapia básica periodontal es muy importante en todo tratamiento de recesiones gingivales. El uso de injertos de tejido conjuntivo subepitelial son el gold standard en cirugía plástica periodontal ya que dan lugar a cambio del espesor tisular, aumento de encía queratinizada y cobertura radicular. El mantenimiento periodontal es prioritario para evitar eventos inflamatorios que faciliten la recidiva de la recesión.
Referencias
1. Chambrone, L. Rationale for the Surgical Treatment of Single and Multiple Recession-Type Defects, In: Chambrone, L. Evidence Based Periodontal and Peri Implant Plastic Surgery, 1er Ed, Springer, 2015: 45-146.
2. Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J Clin Periodontol, 1996; 23: 770-777.
3. Bueno, L; Chambrone, L. Management of multiple recessions type defects after Orthodontic Therapy: A clinical case report based of Scientific Evidence, Clinical Advanced of Periodontology; 2015; 10: 1- 14.
4. Chambrone L, Sukekava F, Ara.jo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol 2010;81:452–78.
5. Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: A systematic review from the AAP Regeneration Workshop. J Periodontol 2015, 86 (2 Supplement):S8-S51.
6. Richardson CR, Allen EP, Chambrone L, Langer B, McGuire MK, Zabalegui I, Zadeh HH, Tatakis DN. Periodontal soft tissue root coverage procedures: Practical applications from the AAP Regeneration Workshop. Clin Adv Periodontics 2015; 5:2-10.
7. Miller, PD. A classification of marginal tissue recession. Int J Periodontol Rest Dent, 1985; 5: 9-13.
8. Bueno, L; Ferrari, R; Shibli, J. Tratamiento de recesiones y defectos mucogingivales mediante injertos de tejido conjuntivo en piezas dentarias e implantes. Odontoestomatología, 2015; 17 (25): 35-46.
9. Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence- based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. J Periodontol 2012; 83: 477-490.
10. Zuchelli, G. Casos Clínicos Complejo En: Zuchelli, G. Cirugía Estética Mucogingival, 1era. Ed, España, Quintessence, 2014: 693-747.
11. Hurzeler, M; Weng, D. A single incision technique to haverst subepithelial connective tissue grafts from the palate. Int. J. Periodontics Restorative Dent, 1999, 19, 279-287.
12. Harris, R; Miller, R; Harris, L. Complications with Surgical Procedures Utilizing Connective Tissue Grafts: A Follow up of 500 Consecutively Treated Cases. Int. J. Periodontics Rest. Dent. 2005; 25: 449-459.
13. Tatakis DN, Chambrone L, Allen EP, Langer B, McGuire MK, Richardson CR, Zabalegui I, Zadeh HH. Periodontal soft tissue root coverage procedures: A consensus report from the AAP Regeneration Workshop. J Periodontol 2015; 86 (2 Supplement): S52-S55.
14. Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession-type defects? J Dent 2008;36:659–71.
15. Langer, B; Langer; L. Subepithelial connective tissue grafts technique for root coverage. J. Periodontol; 1985; 56: 715-720.
16. Raetzke, P. Covering localized areas of root exposure employing the “envelope” technique. J. Periodontol, 1985; 56: 397-401.
17. Allen, A. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. II. Clinical results. Int J Periodontics Restorative Dent 1994; 14: 303-315.
18. Nelson, S. The subpedicle connective tissue graft. A bilaminar reconstructive procedure for the coverage of denuded root surfaces. J. Periodontol, 1987; 58: 95-102.
19. Wennstrom, J; Zuchelli, G. Increase gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2 year prospective clinical study. J. Clinical Periodontol, 1996; 23: 770-777.
20. Bruno, J. Connective tissue graft technique assuring wide root coverage. Int J Periodontics Restorative Dent 1994; 14: 127-137.
21. Harris, R. The connectivetissue and partial thickness doublé pedicle graft: a predictable method of obtaining root coverage. J. Periodontol, 1992; 63: 477-486.
22. Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession-type defects? J Dent 2008; 36: 659-671.
23. Wilderman MN, Wentz FM. Repair of a dentogingival de- fect with a pedicle flap. J Periodontol 1965;36: 218–231.
24. Caffesse RG, Kon S, Castelli WA, Nasjleti CE. Revascu- larization following the lateral sliding flap procedure. J Periodontol 1984; 55:352–358.
25. Pasquinelli, K. Histología de la nueva inserción al utilizar un injerto autógeno de tejido blando grueso en un área de profunda recesión: Reporte de un caso. Int J Periodontics Restorative Dent 1995; 15:248-257.











 texto em
texto em 



