Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.18 no.27 Montevideo mayo 2016
Alvarado Esteban*, Chanis Jonattan*, Barrientos Silvia**, Rodríguez Adriana***
* 5th Year Residents. Postgraduate Degree in Maxillofacial Surgery. Pontificia Universidad Javeriana. Bogotá.
Silvia Barrientos Sánchez: barrien@javeriana.edu.co
** Stomatologist. MSc in Microbiology. Research Professor. Dental Research Center - CIO. School of Dentistry. Pontificia Universidad Javeriana. Bogotá.
*** Bacteriologist. MSc in Microbiology. Research Professor. Dental Research Center - CIO. School of Dentistry. Pontificia Universidad Javeriana. Bogotá.
Abstract
Background: Panoramic radiography has acquired great diagnostic value given its low cost and its capacity to detect findings that are non-detectable in clinical practice. In maxillofacial surgery, they are useful to monitor major surgical procedures as they enable professionals to detect osteosynthesis materials and thus determine bone diseases with surgical indications.
Objective: to determine the prevalence of osteosynthesis material in panoramic radiographs of adult patients, looking for its association with bone defects, surgical pathology, dentofacial anomaly and trauma.
Method: 10,000 x-rays were evaluated and classified according to sex, age and presumptive diagnosis. Results: there were 173 x-rays with findings of rigid fixation, mostly among women aged between 21 and 30. Men tend to suffer more from trauma, while orthognathic surgery is more prevalent among women. Conclusion: Osteosynthesis material is more often associated with the correction of dentomaxillofacial anomalies in young women, while the rigid internal fixation associated with surgical pathology has low prevalence.
KEYWORDS: Panoramic radiography, Osteosynthesis material, Trauma, Surgical pathology, Orthognathic surgery.
Received on: 22 Jul 15 Accepted on: 30 Nov 15
Introduction
Panoramic radiography is one of the most commonly used complementary diagnostic tools due to its cost, as well as its sensitivity and specificity when it meets quality standards, because it makes it possible to see bone and dental structures, which cannot be accessed clinically. This makes it a valuable tool for collecting information for comprehensive diagnosis in dentistry (1). In maxillofacial surgery, findings associated with trauma, orthognathic or reconstructive surgery can be identified by the presence of osteosynthesis plates that enable the apposition and healing of fragments subjected to open surgery in a wide variety of surgical situations. Studies conducted in maxillofacial surgery clinics, with a sample of patients who have sustained facial trauma, provide no data on prevalence in the general population and show similar care practices. On average, 2 fractures per individual were found in an Australian population of 980 patients treated between 2009 and 2011 for maxillofacial trauma (MT), and in Latina, Italy, the ratio decreases to only 1 fracture per individual (2-3). Van den Bergh and collaborators analyzed a population of 579 patients treated in a hospital in Amsterdam for MT, which was related to traffic, followed by violence, and which more commonly affected young men in the mandible (4). This is consistent with the data obtained by Ortiz and collaborators in their review of the medical records of 663 patients who had undergone surgery in the Hospital General de Medellin, Colombia (5). Data regarding orthognathic surgery is limited, but some data obtained from a maxillofacial surgery clinic in Colombia shows that between 2005 and 2007, 55% of the surgical procedures performed were orthognathic surgeries, predominantly on young female adults (6). In an epidemiological analysis study of orthognathic surgery between 2002 and 2008 conducted in Brazil, the mean patient age was 25.8 years and the female to male ratio was 1.5:1. Most of the procedures affected the maxilla, and class III malocclusion was the dentomaxillofacial anomaly (DMFA) most frequently corrected (7).
In view of the high rates of traffic accidents and violence in the area, and the increased access to orthodontics for diagnosing DMFA (6), this study suggests using digital panoramic radiographs to determine the presence of osteosynthesis material (OM) and presumptively associating these findings with trauma, the correction of dentofacial anomalies, surgical pathology or bone graft, with the limitation that the management of closed traumas or grafts performed without screw fixation cannot be assessed using this method, for the purpose of providing an epidemiological basis that will serve as a guide for health care services, because it makes it possible to determine the need for maxillofacial surgery, be it due to trauma, orthognathic surgery or surgical pathology. These data are not currently available in health care studies in Colombia, and are required to evaluate the needs in this area.
Material and methods
A transversal, observational, descriptive study of 10,000 radiographs of patients over 18 obtained from different radiological centers in Bogota was conducted between 2012 and 2013, after receiving the approval of the Research and Ethics Committee of the School of Dentistry of the Pontificia Universidad Javeriana, and following the regulations set forth in resolution No. 8430 of 1993, issued by the Ministry of Health of the Republic of Colombia. The study included digital panoramic radiographs with adequate density and contrast. The ones with images consistent with osteosynthesis material (plates, reconstructive mesh, screw and wire) were selected, excluding the ones with uncertain findings. The data were entered into Microsoft Excel® format and included sex, age and presumptive diagnosis associated with OM such as trauma, DMFA (orthognathic surgery), surgical pathology (reconstructive surgery) and bone defect (bone graft). The criteria used to determine the presumptive diagnosis of trauma included the presence of irregular fracture lines, cortical diastasis, overlapping bone fragments causing double density, extrusion or loss of teeth in the line of the fracture, missing bone segment with presence of osteosynthesis material. The characteristics and edges of the lesion, as well as the kind of osteosynthesis material used were observed in cases of surgical pathology. Linear osteotomies, orthodontics or orthodontic retention associated with surgical osteosynthesis, symphyseal osteotomy (genioplasty) and root parallelism were considered for dentofacial anomalies. Finally, the images selected for bone defects were the ones with toothless space with a screw associated with the alveolar bone ridge (1). An analysis was performed using descriptive statistics. The chi-squared test was used for comparisons, with a significant value of p<0.05
Results
Among the ten thousand radiographs reviewed, the average patient age was 38.4 years (SD: ±15.4), ranging from a minimum of 18 years to a maximum of 92 years, and 4,240 belonged to male patients (42.4%) and the remaining 5,760 (57.6%) to female patients.
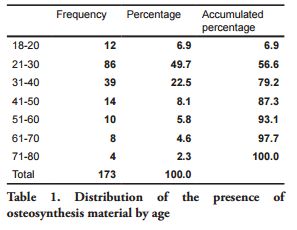
The number of radiographs with findings suggesting the presence of osteosynthesis material was 173 (1.7%). The mean age in this group of patients was 33.8 years, 104 (60.1%) were women and 69 (39.9%) were men (p=0.5). The 21-30 age group had the most presence of material, with 86 radiographs (48.7%), while 4 (2.3%) patients were found in the 71-80 age group. Table 1 summarizes the age distribution of the 173 radiographs.
Upon analyzing the distribution of the diagnostic impressions associated with the osteosynthesis material (Figure 1), it was found that the population under study has twice as many images consistent with orthognathic surgery as with trauma.
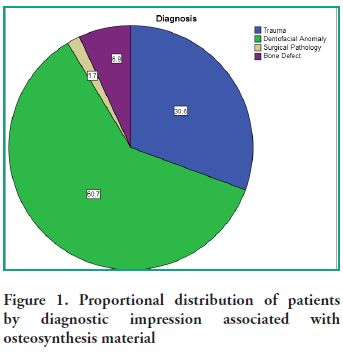
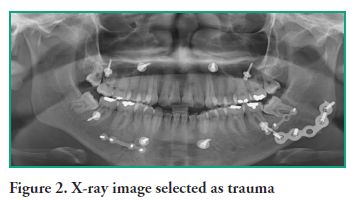
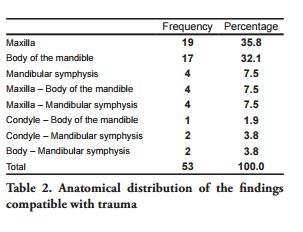
The analysis by presumptive diagnosis showed a higher frequency of images consistent with dentofacial anomaly (105, or 60.7%) than those consistent with trauma (53, or 30.6%) (p=0.00000002). As for the images associated with a diagnostic impression of trauma (Figure 2), 32 (60.4%) belong to male patients and 21 (39.6%) to female patients (p=0.0003). The Odds Ratio calculated for men was 3.42. The 21-30 age group had the highest frequency of trauma, with 21 radiographs (39.6%), and the 51-60 age group was the one with the lowest frequency, with 3 patients (5.6%). The anatomical distribution of injuries is summarized in Table 2.
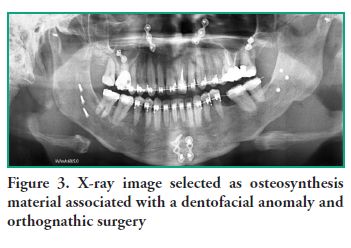
Of the patients with a diagnostic impression of dentofacial anomaly (Figure 3), 30 were men (28.5%) and 75 were women (71.4%) (p=0.0002), with an OR of 3.36 for women. The largest number of surgical corrections of dentofacial anomalies was found in the 21-30 age group, with 40 patients (53.3%) and the smallest number was found in the 61-70 age group, with 1 patient (1.3%), and 50 x-ray images (47.6%) showed orthodontics. Condylar anchorages were found in 8 radiographs (7.6%), and 58% of the x-rays showed evidence of bimaxillary surgery. The anatomical distribution of the location of osteosynthesis material in DMFA findings is presented in Table 3.

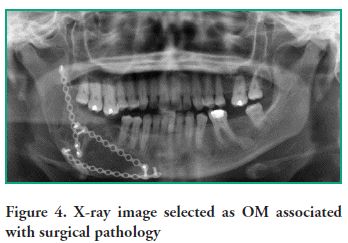
The cases associated with surgical pathology were 3 (1.7%), 2 women and 1 man. These findings were located in the body of the mandible, whereas 13 radiographs (7.5%) showed screws for placing bone grafts, with 6 (46.1%) belonging to men and 7 (53.8%) to women. The largest number of grafts were performed in patients aged 40 or older; 12 bone grafts (92.3%) were identified in the maxillary region and 1 (7.6%) in the mandible (Figure 4).
The analysis showed that the most used osteosynthesis materials were plates and screws in 130 patients (75.1%). Screws were used in 19 patients (11%) and wire was used as the sole osteosynthesis material in 5 patients (2.9%). The combination of plates (screws) and wire was present in 14 patients (8.1%).
Discussion
Procedures related to the practice of the maxillofacial surgeon are diverse, but undoubtedly, the ones associated with trauma, orthognathic surgery and surgical pathology pose the greatest risks because of the anatomical region affected (6). Trauma is the main cause of death in patients under 40, and it is also the main cause of work productivity loss, representing a greater loss of work years than heart disease and cancer combined (8). The incidence of major and facial trauma combined varies from country to country: 34% from a North American database on trauma (9), 24.5% in London and 15% in Liverpool. Patients with major trauma combined with MT have high mortality rates, with up to 33% of them dying at the site of the incident and 21% in hospitals (10).
This study provides no information about patients deceased due to facial trauma, either isolated or combined with major polytrauma, or those who underwent a closed or conservative management of the trauma. However, it does show that the frequency of trauma is greatly surpassed by the correction of dentofacial anomalies. Research studies conducted in different countries have shown that male patients are affected by facial trauma the most, and this is consistent with the data obtained in this study (2-4, 11). An Odds Ratio of 3.42 indicates that men have a higher risk than women of suffering trauma to the craniofacial region, and this is explained by traffic accidents, interpersonal violence, alcohol use and the practice of contact sports (12). The same studies showed that the anatomical region with the highest incidence of trauma was the mandible, unlike other studies that found a higher incidence of fractures in the middle third of the face (3, 8). Some fractures in the middle third of the face can be managed in a closed manner, as is the case in the study conducted by Cabalag and collaborators (2), who reported that the largest number of fractures appeared near the orbit, but the anatomical region in which more open procedures were performed to reduce fractures was the mandibular region. Isolated studies conducted in Colombia have revealed a higher prevalence of trauma in young male adults, associated with interpersonal violence, and mention mandibular fractures as the most prevalent (12).
The number of findings associated with the correction of dentofacial anomalies is higher and could be explained in urban populations, as is the case here, by the current trend of improving face and body aesthetics, and the lower frequency of TM by the fact that it is associated with higher mortality rates that cannot be detected in this study. The statistics obtained by Venugopalan show that out of 10,435 hospitalizations in North America for orthognathic surgery in 2008, 56.2% were in women and the segmental osteotomy in the upper jaw the most frequent reason (13, 14). The proportions regarding sex and DMFA treatment in North America are similar as the ones found in Latin America. In this study, the percentage of the population with a presumptive diagnosis of DMFA was higher in women (71.4%) than men (28.5%), and women are 3.36 (Odds Ratio) times more likely to undergo a DMFA correction. Bimaxillary surgery was performed in 58% of the procedures, which is consistent with a multi-center study conducted in the United Kingdom between 2005 and 2008, where 53% of the orthognathic surgeries were bimaxillary procedures (15). In the eighties, monomaxillary surgeries were performed to correct malocclusions. As of 2000, the percentage of surgeries for setting back the mandible as the only surgical approach for class III patients decreased to less than 10%; maxillary advancement is used in between 45 and 50% of class III patients, and bimaxillary surgery is performed in 40 and 45% of the remaining cases (16), since it has been proven to result in more stability and aesthetically more predictable outcomes when both sides of the maxilla are operated on (17, 18).
The low percentage of bone surgical pathology, using reconstructive plates, is consistent with data presented in previous studies that showed a trend of prevalence in women, which was also observed in this study. The great majority of pathological lesions in the oral cavity take place in soft tissue, and the most common bone lesions, such as odontomas or cysts, and fibro-osseous lesions, tend not to require large surgical resections. This information, combined with the fact that these patients are highly complex surgical pathology cases usually managed in hospitals, and mostly with volumetric imaging, could explain their low incidence (19, 20).
Most of the block grafts performed in this study were placed in the upper jaw, and seven of them in the anterior area; the only graft observed in the mandible was placed in the anterior alveolar area. The majority of grafts, 69.2%, were found in patients aged 40 or older, and it is noted that this kind of treatment is increasingly being applied considering the possibility of rehabilitation with implants (21, 22).
The epidemiological data obtained in this population show that the need for treatments in oral and maxillofacial surgery clinics is significant, given the trauma injuries and genetic anomalies that require their care. Additionally, considering the aesthetic and functional consequences on facial structures, epidemiologic surveillance is imperative in order to establish behavior patterns and take preventive measures both for MT and for DMFA, especially in high-risk groups.
References
1. Farman AG. Panoramic Radiology Seminars on Maxillofacial Imaging and Interpretation. New York: Springer, 2007; 155-163
2. Cabalag M, Wasiak J, Andrew N, Tang J, Kirby J, Morgan D. Epidemiology and management of maxillofacial fractures in an Australian trauma center. J Plastic Reconstruct Aesthetic Surg 2014 Feb;67(2):183-189.
3. Arangio P, Vellone V, Torre U, Calafati V, Capriotti M, Cascone P. Maxillofacial Trauma in the Province of Latina, Lazio , Italy: Review of 400 injuries and 83 cases. J Craniomaxillofac Surg. 2014 Jul;42(5):583-7.
4. Van den Bergh B, Karagozoglu K, Heymans M, Forouzanfar T. Aetiology and incidence of maxillofacial trauma in Amsterdam: A retrospective analysis of 579 patients J Craniomaxillofac Surg 2012 Sep;40(6):165-169.
5. Ortiz G, Arango JC, Giraldo C, Ramírez D, Uribe JC. Análisis Retrospectivo de historias clínicas de pacientes intervenidos por Cirugía Maxilofacial en el Hospital General de Medellín. Rev. CES Odont 2007; 20(2):17-21.
6. Elorza C, Hincapié E, Ramírez P, Correa P. Caracterización de pacientes tratados por Cirugía Maxilofacial en la Clínica CES 2005-2007. Rev.CES Odont. 2009; 22(1)15-19.
7. Scario R, da Costa DJ, Barbosa NL, Müller PR, da Conceição R. Epidemiological analysis of orthognathic surgery in a hospital in Curitiba, Brazil: Review of 195 cases. Rev Esp Cir Oral Maxilofac 2010 Nov-Dec; 32(4):147-151.
8. Gassner R, Tuli T, Ha.chl O, Rudisch A.,Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. J Craniomaxillofac Surg 2003 Feb; 31(1):51–61.
9. Sastry SM, Sastry CM, Paul BK, Bain L, Champion HR: Leading causes of facial trauma in the major trauma outcome study. Plast Reconstr Surg 1995 Jan;95(1):196-197
10. Down KE, Boot DA, Gorman DF: Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg 1995;24(6):409-412
11. Gasshour A, Khateery S. Maxillofacial Trauma in Al Madina Region of Saudi Arabia: A 5-Year Retrospective Study. Asian J Oral Maxillofac Surg 2002;14(1):10-14
12. Fuertes LF, Mafla AC, López EA. Análisis epidemiológico de trauma maxilofacial en Nariño, Colombia. Rev CES Odont.2010; 23(2):33-40.
13. Venugopalan SR, Nanda V, Turkistani K, Desai S, Allareddy V. Discharge patterns of orthognathic surgeries in the United States. J Oral Maxillofac Surg. 2012 Jan;70(1):77-86.
14. Allareddy V, Ackerman MB, Venugopalan SR, Yadav S, Nanda VS, Nanda R. Longitudinal trends in discharge patterns of orthognathic surgeries: is there a regionalization of procedures in teaching hospitals? Oral Surg Oral Med Oral Pathol Oral Radiol. 2013 May;115(5):583-8.
15. Garg M, Cascarini L, Coombes DM, Walsh S, Tsarouchi D, Bentley R, Brennan PA, Dhariwal DK. Multicentre study of operating time and inpatient stay for orthognathic surgery. Br J Oral Maxillofac Surg. 2010 Jul;48(5):360-3.
16. Guglielmi M, Schneider KM, Iannetti G, Feng C, Martinez AY. Orthognathic surgery for correction of patients with mandibular excess: don’t forget to assess the gonial angle. J Oral Maxillofac Surg. 2013 Jun;71(6):1063-72.
17. Eggensperger N, SmolkaqW, Rahal A, et al: Skeletal relapse after mandibular advancement and set back in single-jaw surgery. J Oral Maxillofac Surg 2004 Dec;62(12):1486-96
18. Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB, van’t Hof MA, van der Linden FP, Nottet SJ. Skeletal and dento-alveolar stability of Le Fort I intrusion osteotomies and bimaxillary osteotomies in anterior open bite deformities. A retrospective three-centre study. Int J Oral Maxillofac Surg 1997 26(3):161-75.
19. Romero de León E, Sepúlveda R. Frecuencia de diagnósticos histopatológicos en un periodo de 20 años (1989-2008). Rev Cuba Estomatol [en línea] 2010; 47;(1):96-104. Citado: noviembre 2015. Disponible en: http://www.bvs.sld.cu/revistas/est/vol_47_01_10/est08110.htm
20. Aldape B, Padilla G, Cruz B. Frecuencia de lesiones bucales histopatológicas en un laboratorio de patología bucal. Revista ADM 2007; 64(2):61-67.
21. Esposito M, Maghaireh H, Grusovin MG, Ziounas I, Worthington HV. Interventions for replacing missing teeth: management of soft tissues for dental implants. Cochrane Database Syst Rev. 2012 Feb 15;2:1-69.
22. Chiapasco M, Zaniboni M. Failures in jaw reconstructive surgery with autogenous onlay bone grafts for pre-implant purposes: incidence, prevention and management of complications. Oral Maxillofac Surg Clin North Am. 2011 Feb; 23(1):1-15.











 texto en
texto en 


