Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.18 no.27 Montevideo maio 2016
Antimicrobial therapies for odontogenic infections in children and adolescents. Literature review and clinical recomendations.
Caviglia Inés *, Techera Adriana *, García Graciela *.
* Facultad de Odontología, Universidad de la República, Uruguay.
dragracielagarcía@gmail.com
Abstract
Oral infections are caused by an imbalance in the patient’s indigenous flora which changes from commensal to opportunistic. Odontogenic infections are the most common reason for consultation in children and adolescents. Rational use of antibiotics is the best strategy to avoid microbial resistance. Dental infections should first receive proper local treatment, which can also be complemented with a systemic method. Appropriate drug selection and dosing should be made. Amoxicilin is the first choice for antimicrobial agents in pediatric dentistry. Clindamycin and clarithromycin are the best alternative for patients with penicillin hypersensibility. In this literature review, the authors intended to establish clear clinical management guidelines for emergency treatment and subsequent final resolution.
Keywords: Antibiotics, microbial drug resistance, dental focal infection, children and adolescents.
The original version of Antimicrobial therapies for odontogenic infections in children and adolescents. Literature review and clinical recomendations was published in J Oral Res 2014; 3(1): 50-56 (DOI: 10.17126/joralres.2014.013). Permission to reproduce the paper in Odontoestomatología was granted on 31 March,2016.
Receipt: 10/19/2013 Revised: 11/11/2013 Acceptance: 12/10/2013 Online: 12/10/2013
Introduction
Oral infections are polymicrobial and mixed. They arise when normal flora changes from commensal to opportunistic due to a broken balance with the host in certain circumstances (1). The oral microbial flora starts to grow in the newborn’s mouth about 8 hours after birth.
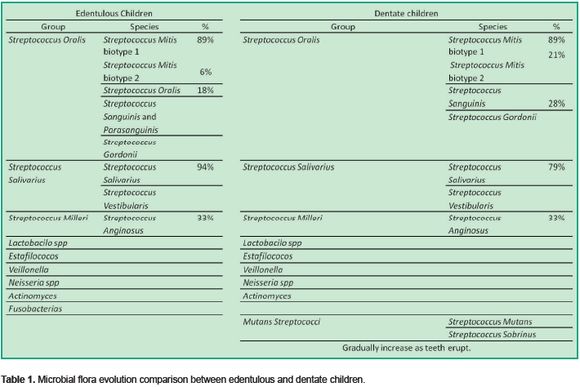
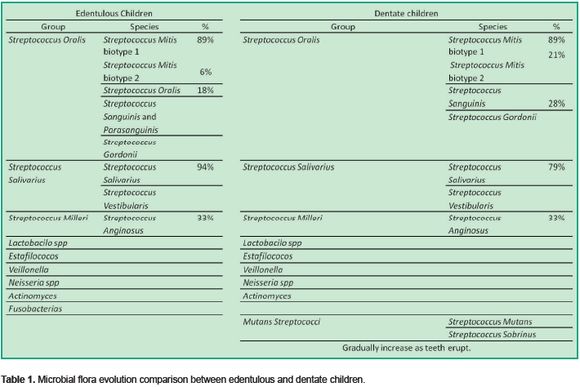
This is followed by a continuous change in its composition from the time the child is edentulous until teeth appearance (2-5). (Table 1)
These oral infections can show themselves in an acute form (acute onset, quick evolution and evident signs and symptoms), or in
a chronic form (slow onset and evolution showing less obvious signs and symptoms). They are classified as odontogenic and nonodontogenic.
Odontogenic infections are the most frequent and begin affecting peridental and dental structures. Non-odontogenic infections start in extra dental structures,
such as mucous, glands, tongue, etc (6).
These infections are usually localized and respond well to treatment. However, favored by children’s special features, they can spread to remote regions and cause serious processes compromising even the patient’s life. General anatomical and physiological characteristics of children are varied because the age range covered by Pediatric Dentistry is wide. For instance, the percent of body water and fat, as well as liver enzymes and plasma proteins levels, are different in neonates and infants from those of children and adolescents. Therefore, body size and composition, immature gastrointestinal, renal and immune system and nutritional status should be considered when assessing odontopediatric patients (7-8).
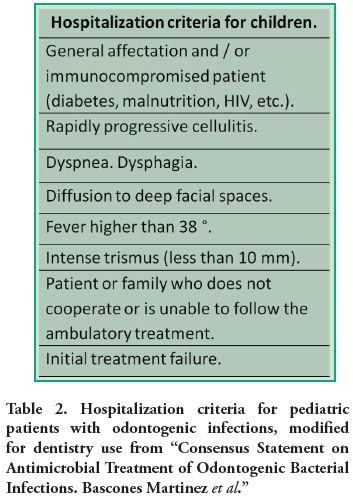
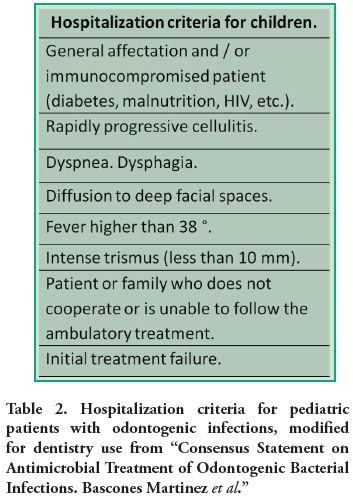
In the same way, jaw anatomical features also differ. They present dental follicles, more cancellous bone with bigger medular holes and growth sites which make the infectious process spread quicker than in adults. For this reason, control in children should be in a short time. The pediatric dentist must take patient evolution into account and pay attention to alarm signs which may lead to hospitalization. The Consensus Document on Antimicrobial Treatment of Odontogenic Bacterial Infections (9), written by specialists in microbiology and odontology in Spain and modified for Pediatric Dentistry (Table 2), considers these causes for hospitalization of a child or adolescent with odontogenic cellulitis:
• General affectation and/or immunocompromisedpatient (diabetes, malnutrition, HIV, etc).
• Rapidly progressive cellulitis.
• Cellulitis extending to deep facial spaces.
• Fever higher than 38°C, dyspnea and/or dysphagia and/or severe trismus limiting mouth opening less than 10 mm.
• Patient or family unable to comply with the prescribed treatment.
• Failure of initial treatment.
About 10% of prescribed antibiotics are used for treating oral infections (6, 10-13). Antimicrobials are indicated for therapeutic purposes: to eliminate infection, make it less severe, make evolution shorter and prevent general complications. Besides, they are used for preventive purposes in subjects with underlying diseases such as cardiac illnesses or immunocompromised patients.
Inappropriate and irrational use of antimicrobials creates favorable conditions for resistant organisms to appear, spread and persist, causing infections which do not respond to standard treatment (14).
For odontogenic infections in temporary or young permanent dentition, local treatment is imposed. It always includes access opening to the infected tooth debridement with or without ducts in order to decompress the affected area. Sometimes, it must be supplemented with mucosal drainage if there is a real collection of suppurative process. This is performed by an incision or mucosal necrosis with trichloroacetic acid in the largest decline. For limited to ground tooth abscesses, for example, local procedure is usually enough. However, if the abscess is more diffuse (covering neighboring areas, bottom of vestibule or other facial regions or affecting the patient’s general appearance), local treatment should be supplemented with an antibiotic therapy to limit the infectious process expansion. If local handling is not properly done and only antibiotics are prescribed, the virulence process decreases. Consequently, it will become acute again when medication is discontinued.
Once the process is reverted, it is time to decide whether the best treatment is conservation of the causal tooth with proper endodontic treatment and restoration or extraction. Just then, the urgency is considered resolved. Extracting the causal tooth during the emergency while the infection is acute is absolutely contraindicated in children and adolescents. Local treatments are always performed with and without adjuvant antimicrobial medication, as described, until the infection is controlled and becomes chronic or the process cools; the reason is to avoid producing bacteremia through the spreading routes. When anesthesia does not go deep in infected areas with acid pH, it produces pain which can affect children and adolescents’ subsequent care.
There is enough scientific evidence linking oral infections to systemic diseases (15-19). However, although odontogenic infections are common in children and adolescents, there are few published works and a striking dispersion criteria in terminology, classification and treatment guidelines (9, 20).
The purpose of this literature review is to establish clear and updated guidelines for clinical management, prevention and treatment of oral infections in this age group.
Overview
Antibiotics era begins with the discovery of penicillin by Fleming in 1928. This is a substantial change for successful infection treatment. From then on, new types of antimicrobial agents have constantly arisen to control infections and overcome resistance caused by bacteria, viruses, fungi and protozoa, and their destructive action (21). Presently, the speed at which new multi-resistant microorganisms grow, far exceeds the rate at which new antimicrobial substances arise. This serious problem concerns the medical and scientific community who fear the threat of mankind going back to pre-antibiotic era, making many infections untreatable. The rapid spread of these organisms together with the efficiency and speed of the current means of transport harm the effectiveness of health care and security. Fast mobility for humans and goods also enables microorganism transportation between continents (14). Therefore, a serious updated study of antimicrobials is imposed for their proper use, without excesses generating new resistance.
Rational use of medicines (RUM)
Among strategies to prevent microbial resistance, one of the most important is the rational use of antimicrobials. It is important for patients to receive the
appropriate medications for their clinical needs: dosing to meet individual requirements for an adequate period of time at the lowest cost for them and their community (14, 22).
These are other mechanisms currently used to prevent antimicrobial resistance:
• Graduate and postgraduate medical education on infectious diseases and evidence-based antimicrobial prescription.
• Monitoring programs for resistant strainsemergence (23).
• Rational use of antimicrobials for animal food production in veterinary medicine
• Cyclic rotation of antibiotics in health institutions (a novel concept with questionable results) (21-24).
• Hospital infections control and prevention
• Increasing vaccines use (21).
Choosing an antimicrobial.
It is vital to choose the correct antimicrobial and dosage considering odontopediatric patients’ characteristics. That includes their different life stages as well as anatomical, physiological and metabolic characteristics, namely, size and body composition, immature gastrointestinal, hepatic, renal and
immunological systems. Anatomical features of children’s jaws are unique because they present dental follicles, larger amount of less trabeculated cancellous
bone but with larger trabeculae, highly vascularized with extensive marrow spaces and presence of bone growth centers (7-8).
These conditions vary as the child grows. In this patient, health status should also be assessed (well-constitution, any previous disease or if he is immunologically depressed) and the type and severity of infection (mild, moderate or severe) (1,25-27). In order to arrive at the correct diagnosis and prognosis to indicate a proper treatment plan for the patient, a complete medical history should be performed. It details certain information about the patient, such as living
environment, customs, health coverage, age, family and personal background, body, fitness, nutrition, general and oral health.
Additionally to patient’s characteristics, which are very important when choosing treatment, other factors should also be considered when
prescribing medications. The drug, an antimicrobial agent in this case, should be indicated in clinically justified situations and usually as a relevant adjuvant
treatment (6, 12, 25). Quality tested drugs should be used in order to ensure that, with the correct dosage according to the severity of infection, the patient’s age, weight, liver and kidney function, the result will be as expected. For selecting the administration via, nature and severity of the infection and absorptive
capacity of the drug need to be considered (28).
When infections threaten the patient’s life, intravenous via (IV) is usually indicated. Those drugs with good oral absorption (VO) can be used in children even in severe cases because they are very well tolerated. The quite painful intramuscular route must be avoided in children and adolescents whenever possible.
Considering all these elements and the infected area (oral cavity) and flora associated with it, drug choice is made empirically (6-25).
In children and adolescents, it is necessary to inquire about the type of presentation, whether pediatric tablets or solution, they commonly use. Regardless of age, it can happen some children take pills and teenagers prefer a pediatric solution. It is essential to give correct, detailed and accurate information to the person responsible for the drug administration.
The indicated time and frequency between takes must be respected for successful treatment (26, 29, 30).
When the presentation is in oral solution, it is necessary to explain how to prepare, dispense and preserve it. Emphasis should be made not to change the dosage form by dissolving solution in juices or opening capsules, to improve drug acceptance by the child in all cases.
The practitioner must observe short-term response to treatment, especially in children, since infectious processes spread very fast because of their anatomical, physiological, immunological and pathological characteristics (25). The first control must be within 24 hours after the emergency consultation even by telephone if necessary.
Recommended length of time must not be excessively long because it favors the emergence of resistance and possible side effects. Neither should it be less than 7 days for bacteriostatics or 5 days for bactericidals to avoid recurrence of the infection, forcing to repeat the treatment and favoring the appearance of resistance by using frequent subtherapeutic doses (1, 6, 12, 26).
Finally, the least costly alternative compared to the same benefit and safety should be considered (22).
Antimicrobials commonly used in Dentistry
The first choice is penicillins. Among them, Amoxicillin has bactericidal activity, good oral absorption (75-90%) (1), can be administered with food intake and its half-life is longer than the rest (31). Dosing every 8 hours allows schedule flexibility to let the patient sleep at night, especially when he is a child. Moreover, the difference between therapeutic and toxic doses is very broad, allowing a safe dosage range (32, 33).
Aantimicrobial resistance (AMR) is a growing global problem. Indiscriminate and excessive use of penicillins generated resistant organisms producing beta-lactamases through mutations.
Amoxicillin, associated with irreversible betalactamase inhibitors such as clavulanic acid or sulbactam pivoxil, offers the chance to treat infections caused by producing betalactamases bacteria.
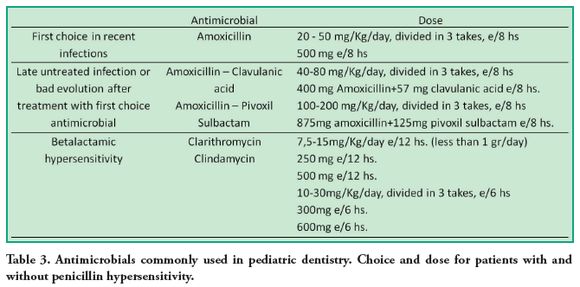
This type of associated antibiotic is the choice for patients who have been systemically treated, but have not received adequate local treatment (access opening and drainage), making the infectious process to persist. It is also indicated for subjects who do not do or do not receive an adequate antibiotic therapy (Table 3).
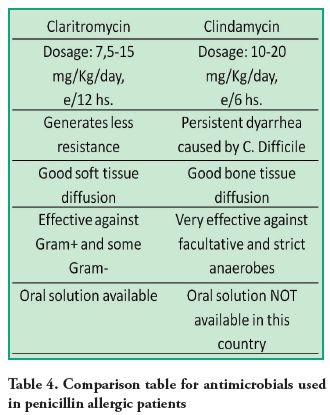
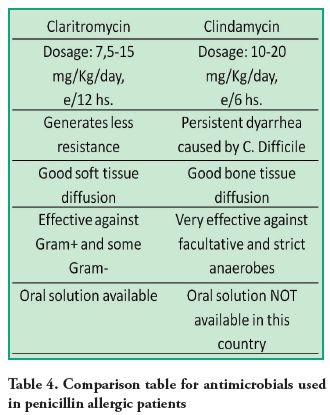
Ampicillin, due to its poor oral absorption, food intake incompatibility and dosing frequency (50 to 100 mg/kg/day every 6 hours), is preferred to be administered parenterally. Clindamycin (lincosamide) or clarithromycin (macrolide) are indicated for patients with penicillin hypersensitivity in the reviewed literature (1, 12, 25, 27) (Table 4). Clarithromycin has the advantage of a more convenient dosing every 12 hours, generates less resistance, has good distribution in soft tissues, and is available in pediatric tablets and oral solution. Its disadvantage is the therapeutic and toxic doses are very close so
it should not exceed a gram daily.
Clindamycin is taken every 6 hours and may cause diarrhea due to Clostridium Difficile infection (1). This makes it difficult for the patient to comply with all the indicated doses but it has good distribution in bone tissue. Besides, it is very effective against facultative and obligate anaerobes, thus, it is reserved for those cases.
In some countries there is no oral solution for clindamycin presentation which is considered a drawback in Dentistry34-36 (Table 4).
The most important penicillin adverse effect is hypersensitivity, which can go from a simple rash to an anaphylactic reaction. Allergic reactions to penicillin are described in 0.7-10 % of exposed individuals, and anaphylactic reactions in less than 0.004 to 0.2 % (32-36). It is contraindicated for individuals with anaphylaxis history, urticaria or rash immediately after penicillin administration because of the immediate hypersensitivity risk. In such cases, neither cephalosporins or other beta -lactam antibiotics are used as they share the basic structure (30, 34). Subjects with a minor eruption history (not confluent and restricted to a small area of the body) or one occuring more than 72 hours after penicillin administration, are possibly not allergic to it. For these subjects, penicillin can be used for a severe infection if necessary.
Discussion
Odontogenic infection is common and often leads to widespread and severe processes. In spite of this, the recommended treatments are not based on scientific evidence because the available clinical trials are difficult to implement and very diverse. Instead, they are based on professional agreements and consensus documents (6).
Due to the special characteristics explained above, the severity of these infections may be higher in children. Conducting clinical trials is more difficult in this group; that is the reason for such few publications on this particular population, especially in the oromaxillo-facial field.
This motivated a literature review to generate a clear guideline for clinical resolution of these processes in pediatric dentistry.
To prescribe an antimicrobial, literature shows it is essential to respect the characteristics of the drug used (time or concentration dependent), dosage form,
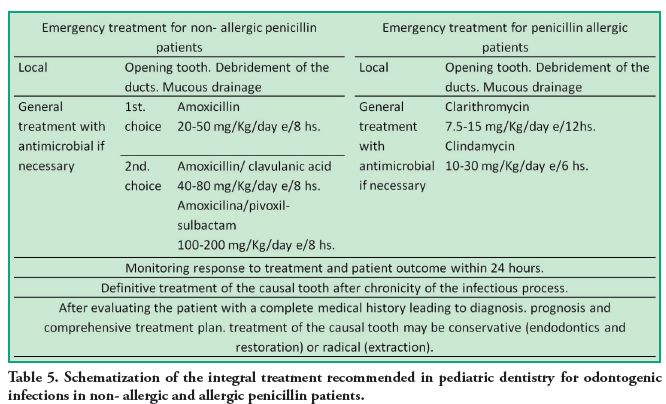
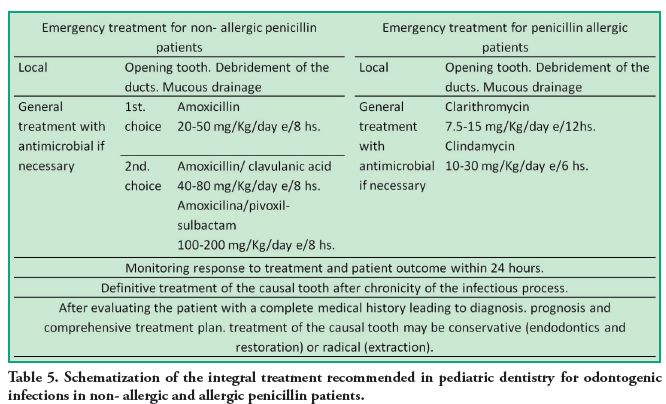
patient characteristics, type and severity of infection dental care so it must be a positive experience. It is important to avoid additional pain and effectively solve the patient’s problem. For this reason, it is recommended to use procedures to calm the infectious process during emergency treatment and, later, the definitive treatment can be done. (Table 5)
These guidelines aim to rationalize the use of antibiotics in pediatric dentistry, providing clear criteria for treatment that minimizes antimicrobial resistance according to the RUM current criteria. Clinical experience shows that urgency is often the entrance for the child or adolescent’s.
Conclusions
Dental Infections, should first receive the appropriate local therapy which can sometimes be complemented with a systemic treatment. Therefore, treatment of an odontogenic infection is based on local or combined (local and general) methods (25). It is vital to obtain a correct diagnosis through a complete medical history to offer an appropriate treatment. If antimicrobial therapy is decided, the professional must make the correct drug choice according to the patient and case. Submedication should be avoided (at a dose and/or time) as well as changes in the dosage form to improve acceptance by the child. There are few references in the literature to provide information on antimicrobial use in dental origin infections in pediatric dentistry.
Literature and clinical experience show amoxicillin is the first choice for children. Amoxicillin associated with sulbactam pivoxil or clavulanic acid is indicated in patients who previously received inadequate systemic treatment.
For patients with penicillin hypersensitivity, clindamycin or clarithromycin are the correct choice. Literature and clinical experience indicate it is convenient to avoid radical procedures such as extractions at the acute stage of infection, taking into account the patient’s anatomophysiological and psychological aspects The best thing to do is to limit and cool the process and decide the definitive treatment then. Correct emergency
handling can change an unpleasant situation into a valuable opportunity for the patient and his family to be incorporated in oral health care. This emphasizes health education, prevention, rehabilitation and periodical checks according to individual risk.
Considering the current concerns of the scientific community, it is necessary to go further with studies promoting rational antimicrobials prescription for children and adolescents. It is also important to support investigation on limiting the production of multiresistant microorganisms which compromise effective infection control in the near future.
Acknowledgements.
Special thanks to Prof. Dr. R. Romero, Professor of Pharmacology from UDELAR, and Prof. Dr. Graciela Gonzalez, Professor of Dentistry from UDELAR for their important contribution. Also, thanks go to Claudia Silvera and Carina Patrón, graduates in Librarianship, for their assistance in revising and organizing bibliographic references.
References
Caviglia Inés *, Techera Adriana *, García Graciela *.
* Facultad de Odontología, Universidad de la República, Uruguay.
dragracielagarcía@gmail.com
Abstract
Oral infections are caused by an imbalance in the patient’s indigenous flora which changes from commensal to opportunistic. Odontogenic infections are the most common reason for consultation in children and adolescents. Rational use of antibiotics is the best strategy to avoid microbial resistance. Dental infections should first receive proper local treatment, which can also be complemented with a systemic method. Appropriate drug selection and dosing should be made. Amoxicilin is the first choice for antimicrobial agents in pediatric dentistry. Clindamycin and clarithromycin are the best alternative for patients with penicillin hypersensibility. In this literature review, the authors intended to establish clear clinical management guidelines for emergency treatment and subsequent final resolution.
Keywords: Antibiotics, microbial drug resistance, dental focal infection, children and adolescents.
The original version of Antimicrobial therapies for odontogenic infections in children and adolescents. Literature review and clinical recomendations was published in J Oral Res 2014; 3(1): 50-56 (DOI: 10.17126/joralres.2014.013). Permission to reproduce the paper in Odontoestomatología was granted on 31 March,2016.
Receipt: 10/19/2013 Revised: 11/11/2013 Acceptance: 12/10/2013 Online: 12/10/2013
Introduction
Oral infections are polymicrobial and mixed. They arise when normal flora changes from commensal to opportunistic due to a broken balance with the host in certain circumstances (1). The oral microbial flora starts to grow in the newborn’s mouth about 8 hours after birth.
This is followed by a continuous change in its composition from the time the child is edentulous until teeth appearance (2-5). (Table 1)
These oral infections can show themselves in an acute form (acute onset, quick evolution and evident signs and symptoms), or in
a chronic form (slow onset and evolution showing less obvious signs and symptoms). They are classified as odontogenic and nonodontogenic.
Odontogenic infections are the most frequent and begin affecting peridental and dental structures. Non-odontogenic infections start in extra dental structures,
such as mucous, glands, tongue, etc (6).
These infections are usually localized and respond well to treatment. However, favored by children’s special features, they can spread to remote regions and cause serious processes compromising even the patient’s life. General anatomical and physiological characteristics of children are varied because the age range covered by Pediatric Dentistry is wide. For instance, the percent of body water and fat, as well as liver enzymes and plasma proteins levels, are different in neonates and infants from those of children and adolescents. Therefore, body size and composition, immature gastrointestinal, renal and immune system and nutritional status should be considered when assessing odontopediatric patients (7-8).
In the same way, jaw anatomical features also differ. They present dental follicles, more cancellous bone with bigger medular holes and growth sites which make the infectious process spread quicker than in adults. For this reason, control in children should be in a short time. The pediatric dentist must take patient evolution into account and pay attention to alarm signs which may lead to hospitalization. The Consensus Document on Antimicrobial Treatment of Odontogenic Bacterial Infections (9), written by specialists in microbiology and odontology in Spain and modified for Pediatric Dentistry (Table 2), considers these causes for hospitalization of a child or adolescent with odontogenic cellulitis:
• General affectation and/or immunocompromisedpatient (diabetes, malnutrition, HIV, etc).
• Rapidly progressive cellulitis.
• Cellulitis extending to deep facial spaces.
• Fever higher than 38°C, dyspnea and/or dysphagia and/or severe trismus limiting mouth opening less than 10 mm.
• Patient or family unable to comply with the prescribed treatment.
• Failure of initial treatment.
About 10% of prescribed antibiotics are used for treating oral infections (6, 10-13). Antimicrobials are indicated for therapeutic purposes: to eliminate infection, make it less severe, make evolution shorter and prevent general complications. Besides, they are used for preventive purposes in subjects with underlying diseases such as cardiac illnesses or immunocompromised patients.
Inappropriate and irrational use of antimicrobials creates favorable conditions for resistant organisms to appear, spread and persist, causing infections which do not respond to standard treatment (14).
For odontogenic infections in temporary or young permanent dentition, local treatment is imposed. It always includes access opening to the infected tooth debridement with or without ducts in order to decompress the affected area. Sometimes, it must be supplemented with mucosal drainage if there is a real collection of suppurative process. This is performed by an incision or mucosal necrosis with trichloroacetic acid in the largest decline. For limited to ground tooth abscesses, for example, local procedure is usually enough. However, if the abscess is more diffuse (covering neighboring areas, bottom of vestibule or other facial regions or affecting the patient’s general appearance), local treatment should be supplemented with an antibiotic therapy to limit the infectious process expansion. If local handling is not properly done and only antibiotics are prescribed, the virulence process decreases. Consequently, it will become acute again when medication is discontinued.
Once the process is reverted, it is time to decide whether the best treatment is conservation of the causal tooth with proper endodontic treatment and restoration or extraction. Just then, the urgency is considered resolved. Extracting the causal tooth during the emergency while the infection is acute is absolutely contraindicated in children and adolescents. Local treatments are always performed with and without adjuvant antimicrobial medication, as described, until the infection is controlled and becomes chronic or the process cools; the reason is to avoid producing bacteremia through the spreading routes. When anesthesia does not go deep in infected areas with acid pH, it produces pain which can affect children and adolescents’ subsequent care.
There is enough scientific evidence linking oral infections to systemic diseases (15-19). However, although odontogenic infections are common in children and adolescents, there are few published works and a striking dispersion criteria in terminology, classification and treatment guidelines (9, 20).
The purpose of this literature review is to establish clear and updated guidelines for clinical management, prevention and treatment of oral infections in this age group.
Overview
Antibiotics era begins with the discovery of penicillin by Fleming in 1928. This is a substantial change for successful infection treatment. From then on, new types of antimicrobial agents have constantly arisen to control infections and overcome resistance caused by bacteria, viruses, fungi and protozoa, and their destructive action (21). Presently, the speed at which new multi-resistant microorganisms grow, far exceeds the rate at which new antimicrobial substances arise. This serious problem concerns the medical and scientific community who fear the threat of mankind going back to pre-antibiotic era, making many infections untreatable. The rapid spread of these organisms together with the efficiency and speed of the current means of transport harm the effectiveness of health care and security. Fast mobility for humans and goods also enables microorganism transportation between continents (14). Therefore, a serious updated study of antimicrobials is imposed for their proper use, without excesses generating new resistance.
Rational use of medicines (RUM)
Among strategies to prevent microbial resistance, one of the most important is the rational use of antimicrobials. It is important for patients to receive the
appropriate medications for their clinical needs: dosing to meet individual requirements for an adequate period of time at the lowest cost for them and their community (14, 22).
These are other mechanisms currently used to prevent antimicrobial resistance:
• Graduate and postgraduate medical education on infectious diseases and evidence-based antimicrobial prescription.
• Monitoring programs for resistant strainsemergence (23).
• Rational use of antimicrobials for animal food production in veterinary medicine
• Cyclic rotation of antibiotics in health institutions (a novel concept with questionable results) (21-24).
• Hospital infections control and prevention
• Increasing vaccines use (21).
Choosing an antimicrobial.
It is vital to choose the correct antimicrobial and dosage considering odontopediatric patients’ characteristics. That includes their different life stages as well as anatomical, physiological and metabolic characteristics, namely, size and body composition, immature gastrointestinal, hepatic, renal and
immunological systems. Anatomical features of children’s jaws are unique because they present dental follicles, larger amount of less trabeculated cancellous
bone but with larger trabeculae, highly vascularized with extensive marrow spaces and presence of bone growth centers (7-8).
These conditions vary as the child grows. In this patient, health status should also be assessed (well-constitution, any previous disease or if he is immunologically depressed) and the type and severity of infection (mild, moderate or severe) (1,25-27). In order to arrive at the correct diagnosis and prognosis to indicate a proper treatment plan for the patient, a complete medical history should be performed. It details certain information about the patient, such as living
environment, customs, health coverage, age, family and personal background, body, fitness, nutrition, general and oral health.
Additionally to patient’s characteristics, which are very important when choosing treatment, other factors should also be considered when
prescribing medications. The drug, an antimicrobial agent in this case, should be indicated in clinically justified situations and usually as a relevant adjuvant
treatment (6, 12, 25). Quality tested drugs should be used in order to ensure that, with the correct dosage according to the severity of infection, the patient’s age, weight, liver and kidney function, the result will be as expected. For selecting the administration via, nature and severity of the infection and absorptive
capacity of the drug need to be considered (28).
When infections threaten the patient’s life, intravenous via (IV) is usually indicated. Those drugs with good oral absorption (VO) can be used in children even in severe cases because they are very well tolerated. The quite painful intramuscular route must be avoided in children and adolescents whenever possible.
Considering all these elements and the infected area (oral cavity) and flora associated with it, drug choice is made empirically (6-25).
In children and adolescents, it is necessary to inquire about the type of presentation, whether pediatric tablets or solution, they commonly use. Regardless of age, it can happen some children take pills and teenagers prefer a pediatric solution. It is essential to give correct, detailed and accurate information to the person responsible for the drug administration.
The indicated time and frequency between takes must be respected for successful treatment (26, 29, 30).
When the presentation is in oral solution, it is necessary to explain how to prepare, dispense and preserve it. Emphasis should be made not to change the dosage form by dissolving solution in juices or opening capsules, to improve drug acceptance by the child in all cases.
The practitioner must observe short-term response to treatment, especially in children, since infectious processes spread very fast because of their anatomical, physiological, immunological and pathological characteristics (25). The first control must be within 24 hours after the emergency consultation even by telephone if necessary.
Recommended length of time must not be excessively long because it favors the emergence of resistance and possible side effects. Neither should it be less than 7 days for bacteriostatics or 5 days for bactericidals to avoid recurrence of the infection, forcing to repeat the treatment and favoring the appearance of resistance by using frequent subtherapeutic doses (1, 6, 12, 26).
Finally, the least costly alternative compared to the same benefit and safety should be considered (22).
Antimicrobials commonly used in Dentistry
The first choice is penicillins. Among them, Amoxicillin has bactericidal activity, good oral absorption (75-90%) (1), can be administered with food intake and its half-life is longer than the rest (31). Dosing every 8 hours allows schedule flexibility to let the patient sleep at night, especially when he is a child. Moreover, the difference between therapeutic and toxic doses is very broad, allowing a safe dosage range (32, 33).
Aantimicrobial resistance (AMR) is a growing global problem. Indiscriminate and excessive use of penicillins generated resistant organisms producing beta-lactamases through mutations.
Amoxicillin, associated with irreversible betalactamase inhibitors such as clavulanic acid or sulbactam pivoxil, offers the chance to treat infections caused by producing betalactamases bacteria.
This type of associated antibiotic is the choice for patients who have been systemically treated, but have not received adequate local treatment (access opening and drainage), making the infectious process to persist. It is also indicated for subjects who do not do or do not receive an adequate antibiotic therapy (Table 3).
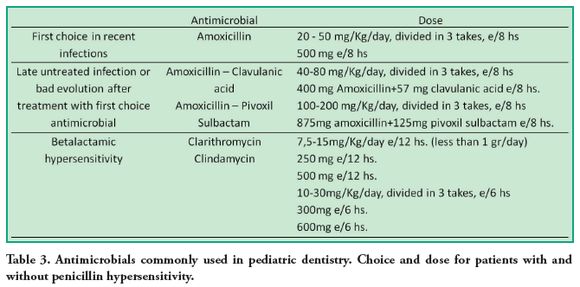
Ampicillin, due to its poor oral absorption, food intake incompatibility and dosing frequency (50 to 100 mg/kg/day every 6 hours), is preferred to be administered parenterally. Clindamycin (lincosamide) or clarithromycin (macrolide) are indicated for patients with penicillin hypersensitivity in the reviewed literature (1, 12, 25, 27) (Table 4). Clarithromycin has the advantage of a more convenient dosing every 12 hours, generates less resistance, has good distribution in soft tissues, and is available in pediatric tablets and oral solution. Its disadvantage is the therapeutic and toxic doses are very close so
it should not exceed a gram daily.
Clindamycin is taken every 6 hours and may cause diarrhea due to Clostridium Difficile infection (1). This makes it difficult for the patient to comply with all the indicated doses but it has good distribution in bone tissue. Besides, it is very effective against facultative and obligate anaerobes, thus, it is reserved for those cases.
In some countries there is no oral solution for clindamycin presentation which is considered a drawback in Dentistry34-36 (Table 4).
The most important penicillin adverse effect is hypersensitivity, which can go from a simple rash to an anaphylactic reaction. Allergic reactions to penicillin are described in 0.7-10 % of exposed individuals, and anaphylactic reactions in less than 0.004 to 0.2 % (32-36). It is contraindicated for individuals with anaphylaxis history, urticaria or rash immediately after penicillin administration because of the immediate hypersensitivity risk. In such cases, neither cephalosporins or other beta -lactam antibiotics are used as they share the basic structure (30, 34). Subjects with a minor eruption history (not confluent and restricted to a small area of the body) or one occuring more than 72 hours after penicillin administration, are possibly not allergic to it. For these subjects, penicillin can be used for a severe infection if necessary.
Discussion
Odontogenic infection is common and often leads to widespread and severe processes. In spite of this, the recommended treatments are not based on scientific evidence because the available clinical trials are difficult to implement and very diverse. Instead, they are based on professional agreements and consensus documents (6).
Due to the special characteristics explained above, the severity of these infections may be higher in children. Conducting clinical trials is more difficult in this group; that is the reason for such few publications on this particular population, especially in the oromaxillo-facial field.
This motivated a literature review to generate a clear guideline for clinical resolution of these processes in pediatric dentistry.
To prescribe an antimicrobial, literature shows it is essential to respect the characteristics of the drug used (time or concentration dependent), dosage form,
patient characteristics, type and severity of infection dental care so it must be a positive experience. It is important to avoid additional pain and effectively solve the patient’s problem. For this reason, it is recommended to use procedures to calm the infectious process during emergency treatment and, later, the definitive treatment can be done. (Table 5)
These guidelines aim to rationalize the use of antibiotics in pediatric dentistry, providing clear criteria for treatment that minimizes antimicrobial resistance according to the RUM current criteria. Clinical experience shows that urgency is often the entrance for the child or adolescent’s.
Conclusions
Dental Infections, should first receive the appropriate local therapy which can sometimes be complemented with a systemic treatment. Therefore, treatment of an odontogenic infection is based on local or combined (local and general) methods (25). It is vital to obtain a correct diagnosis through a complete medical history to offer an appropriate treatment. If antimicrobial therapy is decided, the professional must make the correct drug choice according to the patient and case. Submedication should be avoided (at a dose and/or time) as well as changes in the dosage form to improve acceptance by the child. There are few references in the literature to provide information on antimicrobial use in dental origin infections in pediatric dentistry.
Literature and clinical experience show amoxicillin is the first choice for children. Amoxicillin associated with sulbactam pivoxil or clavulanic acid is indicated in patients who previously received inadequate systemic treatment.
For patients with penicillin hypersensitivity, clindamycin or clarithromycin are the correct choice. Literature and clinical experience indicate it is convenient to avoid radical procedures such as extractions at the acute stage of infection, taking into account the patient’s anatomophysiological and psychological aspects The best thing to do is to limit and cool the process and decide the definitive treatment then. Correct emergency
handling can change an unpleasant situation into a valuable opportunity for the patient and his family to be incorporated in oral health care. This emphasizes health education, prevention, rehabilitation and periodical checks according to individual risk.
Considering the current concerns of the scientific community, it is necessary to go further with studies promoting rational antimicrobials prescription for children and adolescents. It is also important to support investigation on limiting the production of multiresistant microorganisms which compromise effective infection control in the near future.
Acknowledgements.
Special thanks to Prof. Dr. R. Romero, Professor of Pharmacology from UDELAR, and Prof. Dr. Graciela Gonzalez, Professor of Dentistry from UDELAR for their important contribution. Also, thanks go to Claudia Silvera and Carina Patrón, graduates in Librarianship, for their assistance in revising and organizing bibliographic references.
References
1. Bascones A. Bases farmacológicas de laterapéutica odontológica. Madrid: Avances Médico-Dentales; 2000.
2. Smith DJ, Anderson JM, King WF, VanHoute J, Taubman MA. Oral streptococcal colonization of infant. Oral Microbiol Immunol 1993;8:1-4.
3. Bezerra da Silva, LA . Tratado deodontopediatría. Caracas: Amolca; 2008.
4. Liébana Ureña J. Microbiología Oral. 2ª ed. Madrid: Mc Graw-Hill Interamericana; 2002.
5. Van Houte J, Green DB. Relationshipbetween the concentration of bacteria in saliva an the colonization of teeth in humans. Inf Immun. 1974 Apr;9(4):62430.
6. Rodriguez-Alonso E, Rodrigez-Monje MT. Tratamiento antibiótico de la infección odontogénica. Inf Ter Sist Nac Salud 2009;33:67-79.
7. Biondi AM, Cortese SG. Odontopediatría. Fundamentos y prácticas para la atención integral personalizada. 1ª ed. Buenos Aires: Alfaomega; 2010.
8. Pinkham JR. Odontología pediátrica. 3ª ed. México: Mc Graw-Hill Interamericana; 1999
9. Bascones A, Aguirre JM, Bermejo A, et al. Documento de consenso sobre el tratamiento antimicrobiano de las infecciones bacterianas odontogénicas. Med Oral Patol Oral Cir Bucal 2004;9:363-76.
10. Matesanz P, Figuero E, Giménez MJ, Aguilar L, Llor C, Prieto J, Bascones A. Del conocimiento de la ecología bacteriana al tratamiento y la prevención de las infecciones más prevalentes en la comunidad: las infecciones odontogénicas. Rev Esp Quimioterap 2005;18(2):136-20.
11. Granizo JJ, Giménez MJ, Bascones A, Aguilar L. Impacto ecológico del tratamiento antibiótico de las infecciones odontológicas. Rev Esp Quimioterap 2006;19(1):14-145.
12. Najla Saeed Dar-Odeh, Osama AbdallaAbu-Hammad, Mahmoud Khaled AlOmiri, Ameen Sameh Khraisat, Asem Ata Shehabi. Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag. 2010;6:301-306.
13. Lewis MA. Why we must reduce dentalprescription of antibiotics: European Union Antibiotic Awareness Day. Br Dent J. 2008; 205 (10):537-538.
14. Organización Mundial de la Salud( OMS). Resistencia a los antimicrobianos (RAM) Nota descriptiva N°194. Marzo de 2012. [Internet]. 2013 [citado 2013 Oct 7]; [aprox. 5 p]. Disponible en: http://www.who.int/mediacentre/factsheets/fs194/es/
15. Beck JD, Pankow J, Tyroler HA,Offenbacher S. Dental infections and aterosclerosis. Am Heart J 1999; 138: 52833.
16. Offenbacher S, Beck J. Periodontitis: apotential risk factor for spontaneous preterm birth. Compend Contin Educ Dent 1988; 19: 32-9.
17. Loesche WJ. Association of the oralflora with important medical diseases. Curr Opin Periodontol 1997; 4: 21-8.
18. Walter W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Associations: a guideline from the American Heart Associations rheumatic fever, endocarditis, and Kawasaki disease committee, council on cardiovascular disease in the young, and tie council on clinical cardiology, council on cardiovascular surgery and anesthesia, and the quality of care and outcomes research interdisciplinary working group. Circulation 2007;116:17361754.
19. Nishimura RA, Carabello BA, FaxonDP, et al. ACC/AHA 2008 guideline update on valvular hear t disease: Cardiology/American Heart Association Task Force on Practice Guidelines Endorsed by the Society of Cardiovascular Anesthesiologists, Society of Thoracic Surgeons J Am Coll Cardiol 2008;52:676685.
20. Cherry WR, Lee JY, Shugars DA, WhiteRP Jr, Vann WF Jr. Antibiotic use for treating dental infections in children: a survey of dentists’ prescribing practices. J Am Dent Assoc 2012; 143(1): 31-8. 21 .
21. Fernández F, López J, Ponce LM, Machado C. Trabajos de revisión. Resistencia bacteriana. Rev Cubana Med Milit. 2003; 32(1): 44-8.
22. Bordoni N, Esobar A, Castillo R. Odontología Pediátrica. La salud bucal del niño y el adolescente en el mundo actual. 1ª ed. Buenos Aires: Panamericana; 2010.
23. Viera J, Verolo C. Prevalencia de la resistencia bacteriana en la flora bucal en niños de 4-8 años. Odontoestomatología 2010;12(16):51-59.
24. Quintero GA. Reciclaje de antibióticos.Rev Colomb Cir. 2000 Jul-Sept;15(3):167170.
25. Peedikayil FC. Antibiotics: use andmisuse in pediatric dentistry. Review article. J Indian Soc Pedod Prev Dent. 201; 29(4): 282-7.
26. Agency for Helthcare Research andQuality. AAPD Guideline on use of antibiotic therapy for pediatric dental Rockville: AHRQ; 2013.
27. Planells del Pozo P, Barra Soto MA,Troisfontaines ESE. Antibiotic prophylaxis in pediatric odontology. An update. Med Oral Patol Oral Cir Bucal Julio 2006;11(4): E352-7.
28. Malgor LA, Valsecia ME. Farmacologíamédica. Buenos Aires: Mc Graw Hill; 2006.
29. Ramalle Gómara E. Cumplimiento del tratamiento antibiótico en niños no hospitalizados. Aten Prim. 1999;24(6):36467.
30. Asociación Dental Americana. Guía deterapéutica dental. 4ª ed. Madrid: Ripano; 2009.
31. Barcelona L, Marín M, Stamboulian D.Betalactámicos con inhibidores de betalactamasas. Amoxicilina-Sulbactam. Medicina 2008;68:65-74.
32. Marín M. Artículo. Penicilina. [Internet] 2012 ; [citado 7 Oct 2013] 12 (1): [aprox.5 p ] . Disponible en: http://www.ub.edu.ar/revistas_digitales/Ciencias/Vol12Numero1/Articulo_penicilina.pdf
33. Agencia Española de medicamentos y productos sanitarios. Guías de Prescripción Terapéutica (GPT). Madrid: AEMPS; 2012.
34. Goodman y Gilman. Bases farmacológicas de la terapéutica. 10ª ed. México: Mc Graw Hill Interamericana; 2001.
35. Lampiris HW, Maddix DS. Uso clínico de antimicrobianos. En: Katzung BG, Contreras E, Villalpando J, et al. Farmacología básica y clínica. 8. ed. México: Manual Moderno; 2001. pp. 959-975.
36. Florez J. Farmacología humana. 5ª ed. Barcelona: Elsevier Masson; 2008.











 texto em
texto em 


