Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão impressa ISSN 0797-0374versão On-line ISSN 1688-9339
Odontoestomatología vol.17 no.26 Montevideo nov. 2015
Dental care for a baby with holoprosencephaly: case report
Figueiredo, Márcia Cançado *, Cassuriaga, Karoline Farinha **, Alves, Mariana ***
* Associate Professor. School of Dentistry, Federal University of Rio Grande do Sul\UFRGS, Brazil. MA and PhD awarded by the School of Dentistry of Bauru, Universidade de São Paulo/ Bauru/USP. Brazil. mcf1958@gmail.com
** Dentist. School of Dentistry. Universidade Federal do Rio Grande do Sul\UFRGS, Brazil.
*** Psychologist. Student at the University Outreach Course: Interdisciplinary Work in Health Education. School of Dentistry, Universidade Federal do Rio Grande do Sul. Brazil
Abstract
Being the caregiver of a child with birth defects is a difficult task which entails a significant role in the family, to the extent that this person becomes responsible for the care of this special being. This is why the conduct of health professionals in this context must be specialized and of high quality to provide the necessary support to the family/caregiver. To promote effective care, professionals must research the patient’s syndrome, as well as his or her behavioral response and most prevalent characteristics. The aim of this study is to present a case report on a female baby who requires undivided care by her parents, who sought professional help at the Federal University of Rio Grande do Sul, Brazil, in the field of Dental Care for Patients with Special Needs. Additionally, this paper aims to stress the importance of the work of dentists regarding the necessary management and care for patients born with disabilities so as to provide them with the necessary resources through guidelines on oral hygiene. This is done so that the patient can have and maintain good oral health conditions, which in turn helps improve the quality of life of patients with disabilities.
Keywords: holoprosencephaly, congenital abnormalities, dentistry, dental care for disabled people.
Received on: 15 Jan 2015 Accepted on: 26 Mar 2015
Introduction
Among the causes of disabilities in human beings we find congenital anomalies that cause functional or structural abnormalities during embryonic or fetal development. These anomalies are detected at birth and can have genetic, environmental or unknown causes (1, 2). Brain malformations, such as the clinical case this work focuses on, appear because of anomalies in brain development. These anomalies can be genetic or acquired, and it is difficult to determine their etiology. It is known that between 3 to 5% of newborns have some sort of congenital malformation (1), which illustrates the relevance of these deficiencies.
The team of professionals that provide care for patients born with disabilities, both in the public and private sectors, must have a strong humanistic element, from the moment the family/caregiver is informed about the diagnosis, and throughout the process. Family members turn to the health professional for solace, to appease their fear and suffering, hoping to be sheltered and protected and not be made responsible for the situation they are in (3).
Health care for special-needs patients must be provided through a multi-professional team by promoting and coordinating the articulation of different areas through the exchange of knowledge and information. This will enable professionals to provide comprehensive treatment. This professional behavior, which must be committed and humanistic, values individuals in their life situation, considering their special characteristics to have a complete understanding of the person. These are essential features the health team must address when treating patients with disabilities.
In this context, the aim of this study was to communicate the clinical case of a patient receiving care at the Federal University of Rio Grande do Sul, Brazil, in the field of Dental Care for Patients with Special Needs. We must highlight the importance of educational and preventive dental health care for patients with disabilities from their first months of life.
Case Report
Patient's initials: G. B. M. Female. Ten months old. Born with leucodermia on 05 June 2012 in Municipio de Novo Hamburgo, Rio Grande Do Sul, Brazil. She was taken to the School of Dentistry of the Federal University of Rio Grande do Sul (FO/UFRGS) in May 2013 for a control check-up. The child's health records showed the presence of multiple malformations, including neurological deficiencies, major cephalic problems with a diagnosis of holoprosencephaly (HPE), microcephaly, hypotelorism and displaced nose. These anomalies hindered her development and require her parents to provide undivided and permanent care. As she suffered from seizures, she needed anti-seizure drugs, anti gastroesophageal reflux drugs and vitamins. Given her serious deficiencies, the patient needed a tracheotomy at 1 month of age, of which decannulation has not been possible yet according to the medical report dated May 2013. She also had a nasogastric tube. From her birth, the patient has received the care of a multidisciplinary team: a pediatrician, a neurologist, an oral & maxillofacial surgeon, a gastroenterologist and an ophthalmologist from the Hospital de Clínicas de Porto Alegre (HCPA). The CT taken by the team showed agenesis of the corpus callosum in the bone structure image. The hospital team, through the oral & maxillofacial surgeon, referred the patient to FO/UFRGS in April 2013 to receive dental care. In the first appointment at FO/UFRGS an oral interview was conducted with her parents. They explained that the health team had told them that the child's life expectancy was a maximum of one year (the child was 10 months old at the time).
During the interview, the child's mother explained how she had suffered from high blood pressure and a urinary infection at 12 weeks pregnant. She was treated with antibiotics as her doctors believed that the risk of infection might affect the baby.
When asked about the child's oral habits, her parents explained that she used a pacifier when going to bed, and that no oral hygiene procedures had been followed yet. The patient showed a heavy flow of salivary secretion. Therefore, in the dental appointment it was necessary to use a saliva ejector to suction excess secretion through a catheter attached to a suction device brought in by her parents (Figures 1 and 2).

Fig. 1. Suction device

Fig. 2. Saliva ejector
The extraoral clinical exam showed microcephaly and nasal deformity (Figure 3). In the initial intraoral exam, Epstein pearls were detected on the lower-edge mucosa and no teeth were detected.

Fig. 3. Facial features
As the infant had no teeth, parents were instructed to clean the oral cavity using moistened gauze twice a day, cleaning also the tongue. A new appointment was set for fifteen days later, where the initial eruption stage of central incisors was observed. Therefore the infant's caregivers were instructed to use a soft toothbrush for children to perform oral hygiene, and to complement it with fluoride toothpaste once a week. After 11 months, in March 2014, the infant's parents returned to FO-UFRGS for a control check-up. The infant was 1 year 9 months old at the time. Another oral interview was conducted to obtain updated information and to discuss the results of the tests ordered by the HCPA. These tests could not determine the cause that led to the child’s deficiencies. In the intraoral clinical exam, deciduous upper and lower central incisors were detected, as well the eruption of deciduous upper first molars and upper lateral incisors. Visible dental plaque was detected on all teeth, and there were no carious lesions or spontaneous bleeding.
After this evaluation, the infant's parents were again given guidelines regarding oral hygiene of the teeth using a toothbrush for children and moistened gauze to clean the tongue (Figure 4). Parents’ authorization was requested to transcribe the clinical case, and to use the patient’s photographs. They agreed and signed a free and informed consent.

Fig. 4. Intraoral clinical exam and hygiene guidelines (March 2014)
On 29th August 2014, at 26 months of age, the child was admitted to the Hospital de Clínicas de Porto Alegre (HCPA), where she died from unspecified heart failure.
Discussion
Holoprosencephaly (HPE) is a major malformation of the central nervous system (CNS) in which the prosencephalon fully or partially fails to develop into two hemispheres: the telencephalon (brain hemispheres) and the diencephalon (thalamus and hypothalamus). Prosencephalic cleavage does not occur and brain hemispheres fail to develop. These disorders generally develop in weeks 5 and 6 of gestation (4). This can be diagnosed in the intrauterine stage through an ultrasound after the third month of pregnancy (5). Our patient's mother did not know that her daughter suffered from HPE during her pregnancy.
HPE is associated with aneuploidy (trisomy of chromosome 13). This abnormality manifests in different ways (Figure 5) that include serious anomalies in the brain and facies, mainly associated to the midline, such as cyclopia, ethmocephaly, cebocephaly, cleft lip and/or cleft palate, ocular hypotelorism and hypertelorism (4, 8, 9, 10). There can also be chromosome 18-related disorders: triploidy, monosomy, mosaicism, Meckel syndrome, type 1 diabetes, teratogenic and tobacco-related effects, and congenital infections. In this clinical case, although several studies were conducted, including a genetic study, it was not possible to determine the etiology of the malformations given its heterogeneous nature. The incidence of HPE in Brazil is 1 per 16,000 live births (4, 6). In a study conducted in a reference public institution for high-risk pregnancies, holoprosencephaly appeared in 7.5% of cases of CNS anomalies (7).
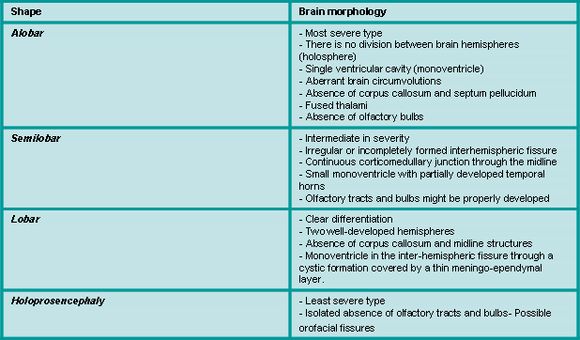
Fig. 5. Holoprosencephaly classification. Source: Noronha et al, 2001
HPE prognosis varies according to the type of malformation, as in some rare cases where the malformation is milder, life expectancy is close to normal figures (4, 9). Alobar and semilobar holoprosencephaly are the most aggressive types and have an unfavorable prognosis as they are usually fatal and associated with serious cognitive deficits (9). According to a study conducted by Cericato (2007), the life expectancy of children with serious facial malformations, as in the case of alobar HPE, is lower than that of children with less serious facial deficiencies. Child mortality is affected by the severity of the anomaly as well as other factors: mother's health, quality of and access to health services, socieconomic factors and public health practices (1).
Given the above definitions and considerations, we believe that this patient had semilobar holoprosencephaly, as the facial malformations were less serious. However, the infant had other malformations which hindered her development and made her dependent on an oropharyngeal airway with a tracheotomy. This made it difficult for the medical team to agree on the HPE type this patient had.
One of the main malformations in HPE is that of the corpus callosum: an encephalic structure that develops between weeks 12 and 18 of gestation. Its agenesis is a congenital anomaly caused by a telencephalic migratory defect that can be complete or partial. When there is isolated agenesis of the corpus callosum, the brain might develop normally, as it is not essential for vital functions (6). It is more usual for the malformation to also cause neurological deficiencies that range from mild to serious. They typically include anomalies in psychomotor development, intellectual disabilities, epilepsy and behavioral changes.
The MRI is considered the gold standard among paraclinical studies in the diagnosis of agenesis of the corpus callosum (5, 7). However, this exam was no ordered for this patient: a CT was performed instead. Additionally, it is essential to inform the general population, and caregivers in particular, about the complexity of the health-disease process, highlighting the importance of prevention, control and early detection regarding health problems. We must also remember that oral diseases caused by the increased risk posed by these deficiencies may affect not just the nutrition of people with disabilities, but also increase the risk of infection, which in turn increases morbidity (10).
In this case, the patient's caregivers were informed of the importance of maintaining oral health and soft tissue hygiene in their child, and also when the first teeth erupted. The child's parents were very receptive, which made it possible to forge a strong professional family-patient bond. This bond was considered essential for the dental treatment of the child as an outpatient, which focused on maintaining her oral health. The relevant literature includes studies that mention how difficult it is to achieve good and effective oral hygiene for the removal of biofilm in patients with this type of deficiency. This happens on account of motor and cognitive limitations, as they lack the necessary skills to brush their teeth and use floss (10). When patients are not able to maintain their oral health, it is the family/caregivers who should take on this responsibility. However, they might do this with uncertainty, given the lack of information about the most effective resources and procedures.
It should be noted that in this case, the drugs taken by the mother may have affected the fetus. In the account provided by the family, the antibiotic described is not mentioned by name, but we must remember that scientific literature reports that drugs must be prescribed when their benefits significantly outweigh their potential risks: the use of medication during pregnancy is a very unusual situation (11). It is important to know that drugs administered to the mother reach the fetus through the placenta. The health team must know the right dosage for each drug, which can be administered, and when to do so (12).
Urinary tract infection (UTI) is a major complication during pregnancy, which can lead to an unclear prognosis. Possible complications are: premature deliveries, low-birth-weight babies, restricted intrauterine growth, cerebral palsy or intellectual disability and perinatal death (13). There are several clinical expressions of the effects of medication on the fetus. This may have anatomical, physiological or behavioral effects, with an early or late onset. Many of these complications during pregnancy can be prevented if there is prenatal monitoring, which allows for the early detection of possible disorders. It is necessary for the doctor to order a urine sample and culture in the first pregnancy check-up.
Finally, this case confirmed the importance of the care for patients with disabilities from the first months of life, as it was possible to forge a bond with the girl and her caregivers, hence facilitating prevention and health education actions. This involved not only parents and family members but also other professionals committed to health services. Additionally, this case proved that dental care has to be personalized and provided with love to the patient and the family. This is why we feel that G.B.M. was more than just a case: she was a life model.
Conclusion
Patients with a deficiency require special care regarding their history, clinical condition, prognosis and treatment. Professionals must be able to provide comprehensive care, including the family/caregiver as part of the health team responsible for taking the necessary therapeutic measures. They must also guide the family/caregiver regarding the special care the patient needs.
References
Figueiredo, Márcia Cançado *, Cassuriaga, Karoline Farinha **, Alves, Mariana ***
* Associate Professor. School of Dentistry, Federal University of Rio Grande do Sul\UFRGS, Brazil. MA and PhD awarded by the School of Dentistry of Bauru, Universidade de São Paulo/ Bauru/USP. Brazil. mcf1958@gmail.com
** Dentist. School of Dentistry. Universidade Federal do Rio Grande do Sul\UFRGS, Brazil.
*** Psychologist. Student at the University Outreach Course: Interdisciplinary Work in Health Education. School of Dentistry, Universidade Federal do Rio Grande do Sul. Brazil
Abstract
Being the caregiver of a child with birth defects is a difficult task which entails a significant role in the family, to the extent that this person becomes responsible for the care of this special being. This is why the conduct of health professionals in this context must be specialized and of high quality to provide the necessary support to the family/caregiver. To promote effective care, professionals must research the patient’s syndrome, as well as his or her behavioral response and most prevalent characteristics. The aim of this study is to present a case report on a female baby who requires undivided care by her parents, who sought professional help at the Federal University of Rio Grande do Sul, Brazil, in the field of Dental Care for Patients with Special Needs. Additionally, this paper aims to stress the importance of the work of dentists regarding the necessary management and care for patients born with disabilities so as to provide them with the necessary resources through guidelines on oral hygiene. This is done so that the patient can have and maintain good oral health conditions, which in turn helps improve the quality of life of patients with disabilities.
Keywords: holoprosencephaly, congenital abnormalities, dentistry, dental care for disabled people.
Received on: 15 Jan 2015 Accepted on: 26 Mar 2015
Introduction
Among the causes of disabilities in human beings we find congenital anomalies that cause functional or structural abnormalities during embryonic or fetal development. These anomalies are detected at birth and can have genetic, environmental or unknown causes (1, 2). Brain malformations, such as the clinical case this work focuses on, appear because of anomalies in brain development. These anomalies can be genetic or acquired, and it is difficult to determine their etiology. It is known that between 3 to 5% of newborns have some sort of congenital malformation (1), which illustrates the relevance of these deficiencies.
The team of professionals that provide care for patients born with disabilities, both in the public and private sectors, must have a strong humanistic element, from the moment the family/caregiver is informed about the diagnosis, and throughout the process. Family members turn to the health professional for solace, to appease their fear and suffering, hoping to be sheltered and protected and not be made responsible for the situation they are in (3).
Health care for special-needs patients must be provided through a multi-professional team by promoting and coordinating the articulation of different areas through the exchange of knowledge and information. This will enable professionals to provide comprehensive treatment. This professional behavior, which must be committed and humanistic, values individuals in their life situation, considering their special characteristics to have a complete understanding of the person. These are essential features the health team must address when treating patients with disabilities.
In this context, the aim of this study was to communicate the clinical case of a patient receiving care at the Federal University of Rio Grande do Sul, Brazil, in the field of Dental Care for Patients with Special Needs. We must highlight the importance of educational and preventive dental health care for patients with disabilities from their first months of life.
Case Report
Patient's initials: G. B. M. Female. Ten months old. Born with leucodermia on 05 June 2012 in Municipio de Novo Hamburgo, Rio Grande Do Sul, Brazil. She was taken to the School of Dentistry of the Federal University of Rio Grande do Sul (FO/UFRGS) in May 2013 for a control check-up. The child's health records showed the presence of multiple malformations, including neurological deficiencies, major cephalic problems with a diagnosis of holoprosencephaly (HPE), microcephaly, hypotelorism and displaced nose. These anomalies hindered her development and require her parents to provide undivided and permanent care. As she suffered from seizures, she needed anti-seizure drugs, anti gastroesophageal reflux drugs and vitamins. Given her serious deficiencies, the patient needed a tracheotomy at 1 month of age, of which decannulation has not been possible yet according to the medical report dated May 2013. She also had a nasogastric tube. From her birth, the patient has received the care of a multidisciplinary team: a pediatrician, a neurologist, an oral & maxillofacial surgeon, a gastroenterologist and an ophthalmologist from the Hospital de Clínicas de Porto Alegre (HCPA). The CT taken by the team showed agenesis of the corpus callosum in the bone structure image. The hospital team, through the oral & maxillofacial surgeon, referred the patient to FO/UFRGS in April 2013 to receive dental care. In the first appointment at FO/UFRGS an oral interview was conducted with her parents. They explained that the health team had told them that the child's life expectancy was a maximum of one year (the child was 10 months old at the time).
During the interview, the child's mother explained how she had suffered from high blood pressure and a urinary infection at 12 weeks pregnant. She was treated with antibiotics as her doctors believed that the risk of infection might affect the baby.
When asked about the child's oral habits, her parents explained that she used a pacifier when going to bed, and that no oral hygiene procedures had been followed yet. The patient showed a heavy flow of salivary secretion. Therefore, in the dental appointment it was necessary to use a saliva ejector to suction excess secretion through a catheter attached to a suction device brought in by her parents (Figures 1 and 2).

Fig. 1. Suction device

Fig. 2. Saliva ejector
The extraoral clinical exam showed microcephaly and nasal deformity (Figure 3). In the initial intraoral exam, Epstein pearls were detected on the lower-edge mucosa and no teeth were detected.

Fig. 3. Facial features
As the infant had no teeth, parents were instructed to clean the oral cavity using moistened gauze twice a day, cleaning also the tongue. A new appointment was set for fifteen days later, where the initial eruption stage of central incisors was observed. Therefore the infant's caregivers were instructed to use a soft toothbrush for children to perform oral hygiene, and to complement it with fluoride toothpaste once a week. After 11 months, in March 2014, the infant's parents returned to FO-UFRGS for a control check-up. The infant was 1 year 9 months old at the time. Another oral interview was conducted to obtain updated information and to discuss the results of the tests ordered by the HCPA. These tests could not determine the cause that led to the child’s deficiencies. In the intraoral clinical exam, deciduous upper and lower central incisors were detected, as well the eruption of deciduous upper first molars and upper lateral incisors. Visible dental plaque was detected on all teeth, and there were no carious lesions or spontaneous bleeding.
After this evaluation, the infant's parents were again given guidelines regarding oral hygiene of the teeth using a toothbrush for children and moistened gauze to clean the tongue (Figure 4). Parents’ authorization was requested to transcribe the clinical case, and to use the patient’s photographs. They agreed and signed a free and informed consent.

Fig. 4. Intraoral clinical exam and hygiene guidelines (March 2014)
On 29th August 2014, at 26 months of age, the child was admitted to the Hospital de Clínicas de Porto Alegre (HCPA), where she died from unspecified heart failure.
Discussion
Holoprosencephaly (HPE) is a major malformation of the central nervous system (CNS) in which the prosencephalon fully or partially fails to develop into two hemispheres: the telencephalon (brain hemispheres) and the diencephalon (thalamus and hypothalamus). Prosencephalic cleavage does not occur and brain hemispheres fail to develop. These disorders generally develop in weeks 5 and 6 of gestation (4). This can be diagnosed in the intrauterine stage through an ultrasound after the third month of pregnancy (5). Our patient's mother did not know that her daughter suffered from HPE during her pregnancy.
HPE is associated with aneuploidy (trisomy of chromosome 13). This abnormality manifests in different ways (Figure 5) that include serious anomalies in the brain and facies, mainly associated to the midline, such as cyclopia, ethmocephaly, cebocephaly, cleft lip and/or cleft palate, ocular hypotelorism and hypertelorism (4, 8, 9, 10). There can also be chromosome 18-related disorders: triploidy, monosomy, mosaicism, Meckel syndrome, type 1 diabetes, teratogenic and tobacco-related effects, and congenital infections. In this clinical case, although several studies were conducted, including a genetic study, it was not possible to determine the etiology of the malformations given its heterogeneous nature. The incidence of HPE in Brazil is 1 per 16,000 live births (4, 6). In a study conducted in a reference public institution for high-risk pregnancies, holoprosencephaly appeared in 7.5% of cases of CNS anomalies (7).
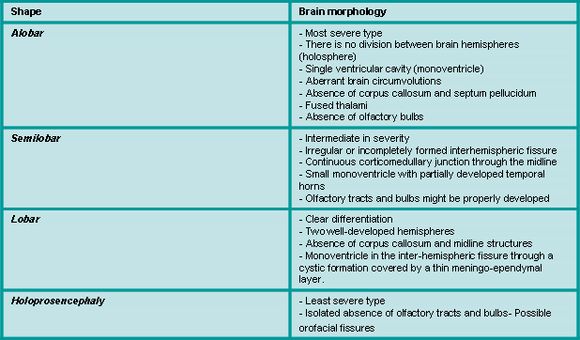
Fig. 5. Holoprosencephaly classification. Source: Noronha et al, 2001
HPE prognosis varies according to the type of malformation, as in some rare cases where the malformation is milder, life expectancy is close to normal figures (4, 9). Alobar and semilobar holoprosencephaly are the most aggressive types and have an unfavorable prognosis as they are usually fatal and associated with serious cognitive deficits (9). According to a study conducted by Cericato (2007), the life expectancy of children with serious facial malformations, as in the case of alobar HPE, is lower than that of children with less serious facial deficiencies. Child mortality is affected by the severity of the anomaly as well as other factors: mother's health, quality of and access to health services, socieconomic factors and public health practices (1).
Given the above definitions and considerations, we believe that this patient had semilobar holoprosencephaly, as the facial malformations were less serious. However, the infant had other malformations which hindered her development and made her dependent on an oropharyngeal airway with a tracheotomy. This made it difficult for the medical team to agree on the HPE type this patient had.
One of the main malformations in HPE is that of the corpus callosum: an encephalic structure that develops between weeks 12 and 18 of gestation. Its agenesis is a congenital anomaly caused by a telencephalic migratory defect that can be complete or partial. When there is isolated agenesis of the corpus callosum, the brain might develop normally, as it is not essential for vital functions (6). It is more usual for the malformation to also cause neurological deficiencies that range from mild to serious. They typically include anomalies in psychomotor development, intellectual disabilities, epilepsy and behavioral changes.
The MRI is considered the gold standard among paraclinical studies in the diagnosis of agenesis of the corpus callosum (5, 7). However, this exam was no ordered for this patient: a CT was performed instead. Additionally, it is essential to inform the general population, and caregivers in particular, about the complexity of the health-disease process, highlighting the importance of prevention, control and early detection regarding health problems. We must also remember that oral diseases caused by the increased risk posed by these deficiencies may affect not just the nutrition of people with disabilities, but also increase the risk of infection, which in turn increases morbidity (10).
In this case, the patient's caregivers were informed of the importance of maintaining oral health and soft tissue hygiene in their child, and also when the first teeth erupted. The child's parents were very receptive, which made it possible to forge a strong professional family-patient bond. This bond was considered essential for the dental treatment of the child as an outpatient, which focused on maintaining her oral health. The relevant literature includes studies that mention how difficult it is to achieve good and effective oral hygiene for the removal of biofilm in patients with this type of deficiency. This happens on account of motor and cognitive limitations, as they lack the necessary skills to brush their teeth and use floss (10). When patients are not able to maintain their oral health, it is the family/caregivers who should take on this responsibility. However, they might do this with uncertainty, given the lack of information about the most effective resources and procedures.
It should be noted that in this case, the drugs taken by the mother may have affected the fetus. In the account provided by the family, the antibiotic described is not mentioned by name, but we must remember that scientific literature reports that drugs must be prescribed when their benefits significantly outweigh their potential risks: the use of medication during pregnancy is a very unusual situation (11). It is important to know that drugs administered to the mother reach the fetus through the placenta. The health team must know the right dosage for each drug, which can be administered, and when to do so (12).
Urinary tract infection (UTI) is a major complication during pregnancy, which can lead to an unclear prognosis. Possible complications are: premature deliveries, low-birth-weight babies, restricted intrauterine growth, cerebral palsy or intellectual disability and perinatal death (13). There are several clinical expressions of the effects of medication on the fetus. This may have anatomical, physiological or behavioral effects, with an early or late onset. Many of these complications during pregnancy can be prevented if there is prenatal monitoring, which allows for the early detection of possible disorders. It is necessary for the doctor to order a urine sample and culture in the first pregnancy check-up.
Finally, this case confirmed the importance of the care for patients with disabilities from the first months of life, as it was possible to forge a bond with the girl and her caregivers, hence facilitating prevention and health education actions. This involved not only parents and family members but also other professionals committed to health services. Additionally, this case proved that dental care has to be personalized and provided with love to the patient and the family. This is why we feel that G.B.M. was more than just a case: she was a life model.
Conclusion
Patients with a deficiency require special care regarding their history, clinical condition, prognosis and treatment. Professionals must be able to provide comprehensive care, including the family/caregiver as part of the health team responsible for taking the necessary therapeutic measures. They must also guide the family/caregiver regarding the special care the patient needs.
References
1.Oliveira CIF. Estudo genético prospectivo de recém-nascidos e natimortos com defeitos congênitos [dissertação]. São José do Rio Preto (SP): Universidade Estadual Paulista, Instituto de Biociências, Letras e Ciências Exatas; 2010.
2.Santos RS. Refletindo sobre a malformação congênita. Rev. Bras. Enferm. 2005 set/out; 58(5): 592-6.
3.Bazon F VM, Campanelli EA, Assis SMB. A importância da humanização profissional no diagnóstico das deficiências. Psicologia: teoria e prática. 2004 ago/set;6(2): 89-99.
4.Noronha L, Ghanem RC, Medeiros F, Knopfholz J, Magalhaes TA, Sampaio GA et al. Holoprosencefalia: análise do seu espectro morfológico em doze casos de autópsia. Arq. Neuropsiquiatr. 2001 mar/abr; 59(4): 913-9.
5.Garcias GL, Martino-Roth MG, Fontana T. Holoprosencefalia. Incidência na cidade de Pelotas. Arq. Bras. Neurocir. 2005 jun; 24(2): 52-7.
6.Ribeiro CL. Sistema Nervoso Central Anomalias estruturais de linha média – Agnesia de corpo caloso- Holoprosencefalia [Monografia]. São Paulo: Fetus – Centro de estudos; 2011.
7.Barros ML, Fernandes DA, Melo EV, Porto RLS, Maia MCA, Godinho AS et al.Malformações do sistema nervoso central e malformações associadas diagnosticadas pela ultrassonografia obstétrica Radiol. Bras.2012 nov/dez;45(6):309-14.
8.Cassab TV, Lamônica DAC, Zorzetto NL, Giacheti CM. Perfil de habilidades do desenvolvimento em crianças com holoprosencefalia e holoprosencefalia like. Rev. CEFAC. 2012 mai/Jun; 14(3): 423-9.
9.Lamego IS, Coutinho LMB. Holoprosencefalia:estudo de seis casos. Arq. Neuropsiquiatr. 1994 abr; 52(4): 523-9.
10.Cericato GO. Educaçao em saúde bucal em portadores de necessidades especiais: um estudo de caso em deficientes visuais [dissertação]. Florianópolis (SC) Universidade Federal de Santa Catarina, Faculdade de Odontologia; 2007
11.Filho EAF, Bispo AMB, Vansconcelos de MM, Maia MZ, Celestino FG. Infecção do trato urinário na gravidez: aspectos atuais. FEMINA. 2009 mar; 37(3): 165-171.
12.Wannamacher L, Ferreira MBC. Farmacologia clínica para dentistas. 3a. Ed. Rio de Janeiro: Guanabara Koogan; 2007.
13.Duarte G, Marcolin AC, Quintana SM, Cavali RC. Infecção urinária na gravidez. Rev Bras Ginecol Obstet 2008 fev/mar; 30 (2):93-10.











 texto em
texto em 


