Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Odontoestomatología
versión impresa ISSN 0797-0374versión On-line ISSN 1688-9339
Odontoestomatología vol.17 no.25 Montevideo mayo 2015
Presurgical orthopedics in children with cleft palate. Case Report
Bravo Rivera, Lorena*, Muñoz Tobar, Daniela**, Torres Chianale, Francisca***, Fierro Monti, Claudia****, Pérez Flores, Antonieta*****
* Assistant Professor, Department of Oral Pediatrics, School of Dentistry, Universidad de Concepción, MSc in Medical Education UdeC, Chile. Pediatric Dentist, Dentistry and Maxillofacial Service, Hospital Clínico Guillermo Grant Benavente, Concepción, Chile. luciabravo@udec.cl
** Dental Surgeon, School of Dentistry, UdeC, Chile
*** Assistant Professor, Department of Oral Pediatrics, School of Dentistry, UdeC, MSc in Medical Education UdeC, Chile
**** Associate Professor, Department of Oral Pediatrics, School of Dentistry, Universidad de Concepción. Chile. PhD Candidate, Universidad Nacional de Córdoba, Argentina
**** Associate Professor, Department of Oral Pediatrics, School of Dentistry, Universidad de Concepción, Chile. ASC in Oral Pediatrics, PhD Candidate, Universidad Nacional de Córdoba, Argentina
Abstract
Cleft lip and palate require presurgical orthopedics to achieve the normal alignment of the cleft maxillary segments prior to Primary Cheiloplasty. Clinical case. A male newborn treated at the Hospital Regional de Concepción diagnosed with complete bilateral cleft lip and palate treated with presurgical orthopedics. Evolution was observed after the first year, as well as the advantages of the Grayson technique and the interaction of the participating multidisciplinary team. Conclusion. Presurgical orthopedic treatment is effective in the rehabilitation of cleft children, and contributes breastfeeding and child feeding. It also makes possible to move the affected bony and soft tissue elements to a better anatomical position in an early stage resulting a better surgery aesthetic and functional. Primary cheiloplasty is thus facilitated by a tension reduction of soft tissues and of the width of the alveolar cleft palate.
Received on: 30.09.14 - Accepted on: 27.01.15
Cleft
lip and palate is one of the most frequent congenital malformations
that affect the maxillofacial complex. It ranks third among all
malformations and has multifactorial etiology. During gestation there
is an alteration in the fusion of tissues that form the upper lip and
palate (1, 2).
Around the world, 1 in 1,200 children born alive present this
malformation according to data of the Latin American Collaborative
Study of Congenital Malformations. In Chile, the rate almost doubles
the world rate: approximately 1.8 in 1,000 children born alive (1, 3).
This malformation, a cleft lip or a cleft palate or both, affects
different functions of children, such as feeding, hearing, breathing
and phonation (1, 4), and it entails aesthetic, psychological and social adaptation problems (3, 4).
The rehabilitation of affected patients is a complex process that
begins early and includes a multidisciplinary focus that aims to
achieve complete rehabilitation, to improve the aesthetic appearance of
the soft and hard tissues compromised and to facilitate the
individual’s social integration (5).
Current protocols support the use of presurgical orthopedics from birth
to align the segments of the cleft maxilla and the nasal molding in the
first months, prior to the surgical reconstruction of the lip and
palate. This procedure is based on Matsuo and Hirose’s research.
They report that in newborns, the nasal cartilage is still in
development and subject to relocation due to the plasticity of the
cartilage that has high levels of hyaluronic acid that circulates in
the body several weeks after birth (4, 6-10).
It is also possible to modify these anomalies in newborns because of
the maternal estrogens present that make the cartilaginous and bony
structures of the fetus elastic and plastic (3).
Presurgical infant orthopedics has been used since 1950, with McNiel
and Burston in England, as adjuvant neonatal therapy to correct cleft
lip and cleft palate. However, it is only many years later that it
becomes an accepted technique (7, 11).
Grayson et al. designed an orthodontic plate where they added a nasal
extension for simultaneous nasal and alveolar molding. The combination
of these two elements creates the nasoalveolar molding device. The
nasal extension is placed when the distance between the cleft alveolar
segments is lower than 5 mm (4).
Presurgical orthopedics is indicated for infants with a large cleft lip
and palate defect and a severe skeletal malformation of the maxilla.
Its main aim is to achieve a normal anatomy at an early stage by
decreasing the size of the opening and re-establishing the correct
anatomic ratio of the cleft maxillary segments (2, 12). It also helps guide the growth of the segments where the maxilla is divided (13), improve lingual function, facilitate newborn feeding, mold the nasal cartilages and reshape the columella (14).
Ideally the infant should be younger than 72 hours for this procedure.
The presurgical treatment is completed at the age of 5 months
approximately, before the closing of the primary palate (1, 15), after which, the device is removed and the first surgery is performed (16).
Clinical case
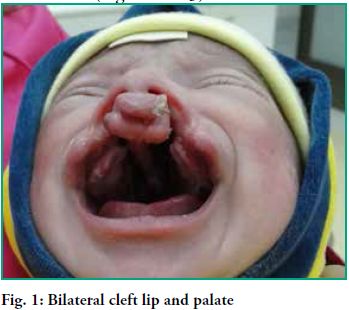
Male newborn diagnosed with complete bilateral cleft lip and palate
(Fig. 1). He received care at the Hospital Guillermo Grant Benavente by
a multidisciplinary team of health specialists that included, in the
first phase: a pediatric surgeon, an obstetrician, a kinesiologist, a
speech therapist, a pediatric dentist and a psychologist.
In the general physical exam, low weight and normal skin coloration is
observed. In the extraoral and intraoral exam, a bilateral cleft lip is
observed, as well as a good jaw ratio, premaxilla displacement greater
than 4 mm from the lateral segments, with greater displacement to the
left, and bilateral complete cleft palate.
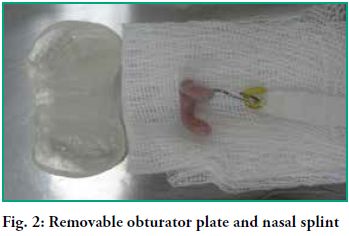
Presurgical orthopedics rehabilitation was started at an early stage
with the insertion of a removable obturator plate and a nasal splint
which were in place until the infant was 4 months old (Figs. 2 and 3).
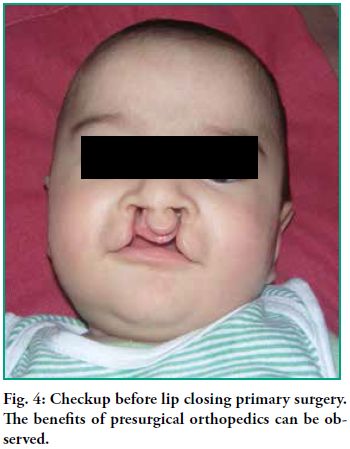
The treatment of
the newborn was coordinated by a multidisciplinary team to achieve
complete rehabilitation and to improve the infant’s living
conditions: feeding, phonation and aesthetics. Presurgical orthopedics
began at birth and was in place until the infant was 4 months old, when
Mülliken’s bilateral cheiloplasty was performed (Fig. 4).
Good results were obtained and there was no lip retraction. According
to the care protocol, a kinesiology treatment was applied to heal the
wound using mesotherapy and ultrasound, among other techniques. Both
the appearance and the texture of the skin improved, with greater
mobility and more action capacity and functionality of perioral muscles
(Figs. 5 and 6). In the dental checkup after the cheiloplasty, the
infant’s mother was given information about the need for good
oral hygiene habits with dressings, as well as a healthy diet. The
following stage would be when primary teeth erupted and preventive
clinical measures would need to be taken. A speech therapist was part
of the process as there was a delay in the use of expressive language.
A palatoplasty was performed when the infant turned one year old. The
patient evolved well and there was good movement of the soft palate.
Nowadays the patient attends periodical checkups with the medical team.
Different
techniques and management guides have been described for the early
rehabilitation of the cleft alveolar ridge. They include presurgical
orthopedics, which is important for creating and preserving normal
functions (17).
In this case, the treatment began by following the clinical guide on
cleft lip and palate of the Chilean Ministry of Health: an impression
of the cleft maxilla was taken with quick-set silicone. Then, the
working model was used to build an acrylic obturator plate which was
used during the first week of life. The plate should remain in contact
with the palate and the alveolar processes, and it must be fixed using
elastic tapes externally attached to the cheeks and to an extension of
the plate through the cleft lip. The plate was modified weekly to bring
alveolar segments closer gradually. This is achieved by adding soft
acrylic in the areas where bone displacement is desired and by
selectively removing acrylic in the areas where bone is expected. This
is done to reshape alveolar segments to achieve alignment and the
occlusion of the alveolar gap (9).
A study conducted by Spengler et al. (10) showed that
presurgical therapy has major advantages for the treatment of bilateral
cleft lip and palate. Some of them were observed when treating our
patient. A few examples: improvement of nasal asymmetry and projection
of the deficient nasal tip associated bilateral cleft lip and palate.
It allows for an appropriate alignment of alveoli, lip and nose, which
results in better surgical outcomes (18). The size of the cleft palate is significantly reduced before the surgery (18, 19),
which allows the surgeon to successfully perform a
gingivoperiostoplasty, and facilitates the closure of the nasolabial
gap by reducing the tension in soft tissues (2, 12, 18).
Once the alveolar segments are better positioned and bone bridges
through the defect become more solid, permanent teeth have a greater
probability of erupting in a good position with the necessary
periodontal support. It also results in fewer and less complicated
surgeries to restore and maintain acceptable nasolabial aesthetics such
as the growth of the nose (16-19), resulting in substantial savings for the family. Another advantage was shown by Lee et al. (7),
who reported that midfacial growth on the sagittal and vertical planes
is unaffected. Besides, it results in good long-term nasal aesthetics,
it corrects the wrong position of the nasal cartilages and the alar
base on the affected side, it extends the columella, and it restores
the normal contour of the maxillary arch (5). It also
makes it possible to separate the oral and nasal cavities thus
minimizing the entry of food into the nasal cavity, reducing adverse
effects on the nasal mucosa and facilitating feeding (2, 9, 11, 14). It minimizes or reduces the future need for a nasoalveolar bone graft (15, 17, 18).
It improves breathing and the development of orofacial functions:
deglutition, phonation and feeding (16). It corrects the disposition of
long-term facial structures (9, 18) and it also has psychological and social benefits for parents and patients (20).
In a prospective study conducted by Spengler (9) in
Houston with patients with bilateral cleft lip and palate, measurements
were taken in cast models to compare before and after treatment
results. They showed significant reductions in protrusion and deviation
of the premaxilla, and in the width of the defect, which was observed
in subsequent checkups.
During the treatment, patients must attend periodical checkups with the
pediatric dentist, as was the case of this patient, to prevent and
monitor decay, as well as otolaryngologic evaluations at least once a
year (21).
Presurgical orthopedics treatment is efficient in the rehabilitation of cleft children as it allows for early redirection of the affected bony elements and soft tissues to a favorable anatomic position. This yields better surgical results, both aesthetic and functional, as primary surgery of the lip is facilitated by the reduction of the tension in soft tissues and the reduction of the cleft palate and alveoli.
Nasoalveolar molding has proven efficient to achieve greater symmetry of the lip and of the nasal cartilages, as well as to improve the projection of the tip of the nose.
Presurgical orthopedics plates are part of the care protocol of the cleft child, as it is not only an important element when closing the defect and relocating soft tissues, but also a contributing factor to facilitate feeding.
Besides, it reduces the need for surgical reconstruction of the columella. The use of the nasoalveolar molding brings the maxillary segments closer so that, if the gingivoperiostoplasty is performed when the lip is closed, there is a significant reduction in the need for a subsequent alveolar bone graft.
Treating a cleft patient is a complex procedure which requires a multidisciplinary approach and parents’ full cooperation to achieve a successful result.
1. Almeida E, Castillo G, Castillo P, Iturriaga P. Ortopedia prequirúrgica: aparato de Grayson para fisuras labiopalatinas. Int J Odontostomat. 2011; 5(1):87-110.
2. Carrasco L, Faraggi M, Merino A. Rinoseptoplastía en pacientes fisurados. Rev Otorrinolaringol Cir Cabeza Cuello. 2011; 71(2):171-178.
3. Cáceres A, Ford A, Tastets M. Tratamiento de la fisura labio palatina. Rev Med Clin Condes. 2010; 21(1):16-25.
4. España-López AJ, et al. Tratamiento ortopédico con moldeador nasoalveolar prequirúrgico en la fisura labiopalatina unilateral. Rev Esp Cir Oral Maxilofac. 2012. Disponible en: doi:10.1016/j.maxilo.2012.03.001
5. Cerón AM, Grajales CA, López AM, Suárez AF. Rehabilitación temprana de los maxilares en pacientes con labio y paladar hendido bilateral utilizando un dispositivo ortopédico dinámico intraoral, cinta adhesiva labial y gingivoperiosteoplastia: Estudio piloto experimental. Rev Fac Odontol Univ Antioq. 2009; 20(2):138- 148.
6. Fundación Gantz. Hospital del Niño con Fisura: Plan de Tratamiento. Disponible en: http://gantz.cl/fisura-del-paladar/ [Consultado Junio 2014] Grayson BH, Shetye PR. Presurgical nasoalveolar moulding treatment in cleft lip and palate patients. Indian J Plast Surg. 2009 Oct; 42:56-61
8. Rivera R. Moldeo nasal postqueiloplastia primaria. Presentación de un caso. Acta Médica del Centro. 2012; 6(2).
9. Ministerio de Salud. Guía Clínica Fisura Labio Palatina. Anexo 8: ortopedia prequirúrgica. Santiago: Minsal: 2009.
10. Chavarria C, Gateno J, Spengler A, Teichgraeber J, Xia J. Presurgical nasoalveolar molding therapy for the treatment of bilateral cleft lip and palate: A preliminary study. Cleft Palate Craniofac J. 2006 May; 43(3):321-8.
11.
Rossell P. Tratamiento de la Fisura Labio Palatina: VI Manejo prequirúrgico. 2010 Jun. 12. Alfaro
C, Gutiérrez C, Giugliano C, Morales H, Muñoz A. Ortopedia pre
quirúrgica de Latham en el tratamiento quirúrgico de lactantes con
fisuras labio alveolo palatinas. Rev Dental de Chile. 2001; 92(3):23-27. 13. Gedrange
T, Gesch D, Heinrich A, Kirbschus A. Presurgical nasoalveolar molding
in patients with unilateral clefts of lip, alveolus and palate. Case
study and review of the literature. J Craniomaxillofac Surg. 2006;
34(2):45-48. 14. Delgado-Muñoz
M, Herrero E, Romance-García A, Romero-Maroto M. Tratamiento ortopédico
prequirúrgico de la fisura palatina con la filosofía de Latham. RCOE.
2005; 10(2):199-204. 15. Broder
H, Chan J, Sischo L, Smith C, Stein M, Van Aalst J. Nasoalveolar
Molding: Prevalence of Cleft Centers Offering NAM and Who Seeks It.
Cleft Palate Craniofac J. 2012 May;49(3):270-275. 16. Cimadevilla
M, González B, Mejía M, Salamanca J. Tratamiento temprano de la fisura
Labiopalatina unilateral con ortopedia dentofacial prequirurgica. Rev
Esp Ortod. 2008; 38:(1)67-72. 17. Grabowski
R, Gundlach K, Kopp H, Stahl F. Presurgical orthopaedic treatment of
newborns with clefts – functional treatment with long-term effects. J
Craniomaxillofac Surg. 2006; 34(2):34-44. 18. Delgado
M, Lagarón E, Marti E, Romance A, Romero M et al. Uso de la ortopedia
prequirúrgica en pacientes con fisura palatina: nuestra experiencia.
Cir Pediatr. 2004; 17:(1)17-20. 19. Cutting
C, Grayson B. Presurgical Nasoalveolar Orthopedic Molding in Primary
Correction of the Nose, Lip, and Alveolus of Infants Born With
Unilateral and Bilateral Clefts. Cleft Palate Craniofacial J. 2001 May;
38(3):193-8. 20. Adali
N, Mars M, Noar J, Petrie A, Sommerlad B. Presurgical Orthopedics Has
No Effect on Archform in Unilateral Cleft Lip and Palate. Cleft Palate
Craniofac J. 2012 Jan; 49(1):5-13. 21. Ford A. Tratamiento actual de las fisuras labio palatinas. Rev Med Clin Condes. 2004 Enero; 15(1): 3-11.











 texto en
texto en