Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.17 no.25 Montevideo May 2015
Partial parallelized obturator prosthesis in oncological patient
de Lima, Javier*, Cabrera, Carlos*, Estrada Esquivel, Blanca**, Sánchez Rubio, Raúl***, Soler, Roberto****
* Assistants at the Bucco-maxillo-facial Prostheses Service. School of Dentistry, Universidad de la República. Uruguay. jjdelima76@gmail.com
** Professor in the Department of Oral Rehabilitation at the School of Stomatology, Benemérita Universidad Autónoma de Puebla, Mexico
*** Responsible for Removable Oral Prostheses at the Prosthodontics Postgraduate Course. School of Dentistry of Mexicali, Universidad Autónoma de Baja California, Mexico
**** Professor of Clinical Rehabilitation and Removable Prosthodontics II. Director of the Bucco-maxillo-facial Prostheses Service. School of Dentistry, Universidad de la República. Uruguay
Abstract
When dealing with neck and head cancer patients, we must consider the many different types of such tumors that appear when conducting histopathologic and anatomic topography assessment. To this we must add etiological or risk factors that will result in various epidemiological and symptomatological characteristics, both regarding the progression of the disease and the prognosis and treatment plan. In this work a clinical case is presented: a 25-year-old female patient who underwent right maxillectomy for an odontogenic myxoma (fibromyxoma) located in her right maxillary sinus. Prosthetic rehabilitation is done with framework obturator prosthesis. The remaining teeth are prepared by creating parallel pillars to obtain a single and accurate axis for insertion and removal.
Keywords: maxillary sinus, tumors, obturator, parallelized pillars.
Received on: 08.10.14 - Accepted on: 26.03.15
Introduction
Patients with extensive substance loss in the maxilla, the maxillary sinus and the nostrils on account of tumor resection show an abnormal communication between the oral cavity and the adjoining cavities: nasal, nasopharyngeal and even the orbital cavity. Though patients are clinically cured, they suffer a mutilation, which in turn affects their functions, aesthetics and relational life. In this article a clinical case is presented: a 25-year-old female diagnosed with odontogenic myxoma.
A myxoma is a tumor that can be found in the heart, the skin, the subcutaneous cell tissue and in bones. However, head and neck myxomas are rare. Two types have been identified: one from bone tissue from the facial skeleton, formerly subdivided into true osteogenic myxoma and odontogenic myxoma, and the other derived from the perioral soft-tissue, parotid gland, ear and larynx (1).
It is a rare aggressive intra-osseous lesion derived from embryonic mesenchymal tissue associated with odontogenesis and primarily consisting of a myxomatous ground substance with widely scattered undifferentiated spindled mesenchymal cells (2).
It represents 0.1% of general bone tumor pathology and 0.6% of oral pathology. It shows no sex predilection, but some authors think that it is more frequent in women, it being most common between the ages of 10 and 40, and in the mandibular body and branch. The teeth can be displaced, and the cortical bones are expanded, even perforated at times (3-5).
They are painless swellings that grow slowly and tend to displace teeth. In advanced stages they can cause pain and paresthesia. Radiographically, the myxoma appears as a unilocular or multilocular radiolucency with a soap bubble, honeycomb or tennis racket pattern (6).
Its histologic variant is the Odontogenic Fibromyxoma, but there is no information regarding its prevalence (5). It is a benign intra-osseous lesion of controversial origin that appears in the facial skeleton, occurring more frequently in the mandible (7).
Differential diagnosis is necessary for: ameloblastoma, usual in young people, frequently located in the mandible, and of slow growth. Radiographically, it appears as a unilocular or multilocular process, generally with well-defined radiographic borders, mobility of roots, radicular resorption, and histological variability. It is also necessary to differentiate from central giant-cell granuloma and keratocyst (4-7).
Treatment: Curettage can be performed for small unilocular lesions, followed by chemical cauterization of the bone walls. Block resection is performed in larger lesions due to the gelatinous or mucous characteristics that make it difficult to perform curettage properly. The treatment is surgical excision, which must be wide and complete if the tumor has invaded deeper tissues. Given the high recurrence rate, block resection with tumor-free bone margins at least 2 mm wide is recommended (8).
It is sensitive neither to chemotherapy, nor to radiation therapy. It has a recurrence rate of 25%, which is why X-rays must be taken annually as follow-up for the following 10 years. There is controversy regarding the convenience of reconstructing the damaged tissue immediately or doing it at a later stage (2-9).
Autoplastic closure (Slotovof) is contraindicated when there is extensive oncologic substance loss: it causes accumulation of nasal secretions and the subsequent ballooning of the palate. Additionally, it hinders the clinical monitoring of the defect when checking for possible tumor recurrence. This is why alloplastic restitution (obturator) is the first choice (9).
The main role of an obturator, from the Latin “obturare”, is to occlude an opening between the oral cavity and the upper air passages, which is the consequence of a surgical exeresis. It also protects the residual surgical field (surgical defect), preventing its subsequent collapse. It contributes to restoring the functions of mastication, deglutition and resonance, also improving hearing (functioning of the Eustachian tubes).
It restores the support of facial soft tissues that have lost their bone substrate, restoring the altered aesthetics, which is also important as emotional and psychological support (10).
We must remember that the best maxillofacial prosthesis is the one created by a multidisciplinary team where surgeons, prosthetists, lab technicians, psychologists, speech therapists and social workers coordinate the patient’s rehabilitation process (11).
If there is extensive substance loss, the obturator can be quite large, therefore, if rigid, it must be hollow, with minimal thickness, to be as light as possible (12). The size of the defect conditions the design and shape of the obturator. We must also stress that the larger the defect, the more difficult it is to occlude the opening and less support and anchorage capacity will be achieved.
Depending on each case, this will require special considerations regarding the study of the appliance mechanics.
Nowadays, rigid obturators are favored over flexible obturators, made with medical grade silicone, as the latter are affected by nasal microbial flora (13).
Rigid obturators enter the defect, sealing its peripheral throat area to prevent food reflux or air leaks. Open in the upper part, they collect nasal discharge and therefore facilitate prosthesis hygiene and are comfortable for the patient (14).
Materials and methods
In this article we present a clinical case of a maxillectomy on account of an odontogenic myxoma, in its histologic variant, the Odontogenic Fibromyxoma, located in the right maxillary sinus.
We will highlight the prosthetic rehabilitation treatment done with framework obturator prosthesis by preparing the parallel pillars to obtain a single and accurate axis for insertion and removal.
Therefore, given this clinical case, the study of obturators and the design of partial removable prostheses are especially relevant.
Classification of obturators
There are multiple classifications of the patients that use obturators, such as:
- • According to when it is made: immediate, transitional and definitive or delayed.
- • According to the material used: rigid or flexible.
- • According to the dental state of the contralateral maxilla: complete or partial edentulism.
Brown’s is the most widely accepted and most modern classification.
According to the location of the defect (Brown et al. 2010):
Vertically:
I- Maxillectomy not causing an oronasal fistula
II- Maxillectomy not involving the orbit
III- Maxillectomy involving the orbital adnexa with orbital retention
IV- Maxillectomy with orbital enucleation or exenteration
V- Orbitomaxillary Defect
VI- Nasomaxillary Defect
Horizontally:
I- Palate defect only, not involving the dental alveolus
II- Less than or equal to half unilateral maxillectomy
III- Less than or equal to half bilateral or transverse anterior maxillectomy
IV- Greater than half maxillectomy (10, 11)
Classification of partially edentulous patient with maxillary defects
According to the remaining teeth (Aramany):
Class I: Tripodal design for curved arches (total maxillectomy)
Class I: Linear design for straight arches (total maxillectomy)
Class II: Tripodal design (posterior maxillectomy)
Class III: Quadrangle design (central maxillectomy, both maxilla and mandible)
Class IV: Linear design (posterior maxillectomy)
Class V: Tripodal design (posterior maxillectomy, both maxilla and mandible)
Class VI: Quadrangle design (anterior maxillectomy, both maxilla and mandible) (15)
Design
When designing a partial obturator, we must consider the remaining teeth, their distribution in the arcade and the location and size of the defect. Aramany’s classification is used in the design of this type of obturator to summarize the variables resulting from the combination of the aspects above (16).
The planning stage must include certain principles of partial removable prostheses that are applicable to a partial framework obturator or plate (17). In all cases the mucous membrane is weaker both in quality and quantity. This total or partial lack of maxilla subjects the remaining teeth which support the appliance to excessive force in most cases, in a linear or polygonal rotational axis with the occlusal prosthetic surface, outside the anchorage surface.
To minimize the negative effects on the support area and to improve the anchorage of the appliance, certain design requirements are considered, especially regarding cavity preparation.
Basic objectives:
- • Guide planes and surfaces to provide stability and fixation. This results in a single axis for insertion and removal that optimizes the anchorage of the parallelized obturator prosthesis.
- • Occlusal rests that provide support and axial transmission of forces.
- • Sufficient retention to prevent the vertical movement of the appliance.
- • Maximum coverage designs, seeking to transfer forces to the mucous and dental support area in the maximum possible extension.
- • Major connector of great coverage to provide better secondary support.
- • Stiff or labile anchorage connection, depending on the case.
- • Occlusal design, to reduce the occlusal surface in the vestibule-lingual direction, to improve mastication efficiency; and the anteroposterior surface to decrease the lever arm. Set punctiform, axial, and low-intensity occlusal contacts in the artificial teeth (15, 18, 19).
Preparation of the periodontium:
As in any partial removable prosthesis, the remaining teeth must be adapted to align mastication forces, to protect the marginal periodontium and to optimize anchorage.
1.- Contour modification: this makes it possible to have a single insertion and removal axis for the appliance, as if there were a rail structure, thus facilitating reciprocation and retention. Drilling should be done following the prosthetic equator set in the parallelometer, or perpendicular to the occlusion plane. Necessary preparation:
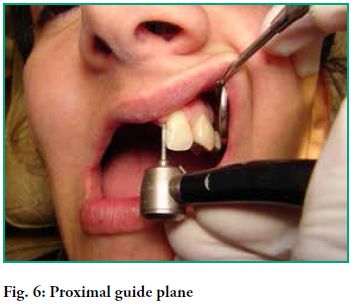
- Guide planes: they should be drilled with a size 8 cylindrical diamond stone in all the proximal surfaces opposite an edentulous gap. The main aim is to contribute to the axis for insertion and removal and to the horizontal stability of the appliance, as well as to reduce the embrasure and to improve the black scape toward the gum in the adjacent prosthetic piece.
- Guide surfaces are drilled: all free surfaces, generally lingual surfaces, of primary and secondary pillar teeth, with a size 8 cylindrical diamond stone, preserving the planimetry of the drilled tooth. Its main aim is to reciprocate the horizontal force of the active arm, enabling the passive arm of the retainer to come into primary contact with the pillar tooth. In the secondary pillar teeth it comes into contact with the stabilizing device or the major connector. It contributes to achieving an axis for insertion and removal and the horizontal stability of the appliance.
- Retention: drilling is performed if necessary, with a round diamond stone if the pillar tooth does not have a 0.25 or 0.5 mm pinhole retention. Through this retention, with guide surfaces and planes, a calibrated removal load of approximately 750 gr. is obtained. This is sufficient, and not excessive, for a pillar tooth, thus ensuring the efficient operation of the appliance.
2.- Rest seats: the preparation that enables the appliance to axially transfer the forces it withstands, and which protects the marginal periodontium of the pillar teeth by preventing its intrusion.
- Occlusal: on the occlusal surfaces of molars and premolars with size 4 and size 8 cylindrical diamond stones respectively.
- Incisal: on anterior teeth; they can be strictly incisal or cingular, mesial or distal, depending on the case (20, 21).
Clinical case
The patient sought professional advice in 1999 on account of a lump in the right maxilla, with a primary diagnosis of myxoma.
Imagenology:
A Magnetic Resonance Imaging (MRI) of the head was performed, which showed signs compatible with an abnormal tissue process that expands, destroys and substitutes part of the right maxilla in the alveolar area. It is a solid lesion, clearly delimited, without signs of invasiveness and probably with moderately high cellularity. It grows only toward the lumen of the maxillary sinus and there is probably a central sector that is damaged or undergoing a necrotic process.
Anatomic pathology:
Material formed by bone trabeculae and skeletal muscle tissue, with multiple recent focal bleeding. Turbinate sections formed by mucosal lining. The chorion is not very dense and there are mucous glands and plenty of dilated vessels. The anatomic pathology analysis showed a myxoma, more specifically an odontogenic myxofibroma.
Treatment plan: The multidisciplinary team prepares the treatment: first a surgical-prosthetic phase, and a second phase of prosthetic rehabilitation.
Surgical approach
Intraoral and intranasal approach, separation of tissues, osteotomy with chisel to dry the affected area of the maxilla, with the corresponding margins; resection of anatomic piece. Extemporaneous biopsy. Toilet of wound. Iodine gauze dressing and fixation of immediate obturator. Joint work with the surgeon allows for better planning of the future rehabilitation. It is requested that the pillar tooth (2.1) next to the defect be removed during the exeresis, which was performed with the corresponding safety margins. In this way there remains a bone fragment of the removed tooth which provides support to the remaining pillar at the end of the gap.
Immediate and transitional prosthesis
An immediate surgical obturator was placed. It was made before the surgery and placed during the procedure, immediately after the resection of the tumoral lesion. The surgeon then sutured the area. When the patient wakes up from the anesthesia, changes to resonance, mastication and deglutition are minimal. Recovery is shorter and better, as the prosthesis acts as support for tissues and as surgical dressing, which guides the healing of the bleeding surface and decreases the risk of immediate infection. The prosthesis was fixed using 0.9 mm circular section steel wire retainers. Loops were used in the vestibular area of the defect to use penetrating wire and to fix the prosthesis to the zygoma. This immediate obturator is essential as it provides post-surgical protection with a low risk of infection in the area, as well as immediate oral feeding. Thus we can prevent decompensation, which is frequent in these patients, and reduce costly hospitalization times, all of which results in a better quality of life.
After 15 days, the fixation of the surgical obturator and the Iodine gauze dressings were removed. The immediate obturator was relined with soft silicone-based conditioner and transformed into a transitional or temporary obturator. Forty days after the surgery, the conditioner was removed and the obturator relined with acrylic to better adjust the base of the defect, thus covering again the basal surface completely with conditioner. The presence of a psychologist is essential throughout this process, as it is the first time that the patient realizes how serious the defect is. It is also essential to work with a speech therapist, since every transformation implies changes to resonance. Thus it is necessary to ask the patient to articulate a few phonemes when taking the impression to achieve better adjustment to the defect and to ensure paraprosthetic tissues contribute to the treatment.
Definitive obturator
It is made once the tissues have healed, which is usually 6 months after the surgery, although it can be less or more time if the patient has received additional treatment such as radiotherapy or chemotherapy. We must consider that the concept of “definitive” is relative, as no removable prosthesis is definitive because oral tissues and the surgical site change, especially in unconventional cases such as this one.
We start off from primary anatomic impressions obtained using the alginate technique and primary models mounted on the articulator. The clinical study and the study of mounted models allow for better planning when preparing the pillar teeth for the parallelized obturator.
Cavity preparation
The patient has an interdental edentulous space and few remaining teeth in the unaffected maxilla. Reduced bone insertion in the main pillars, not very good root shape and decay (2.4 and 2.8). The obvious pillar tooth 2.2, adjacent to the main gap, could not be used as main anchorage despite having bone support on distal surface, since it would give way in a short period of time. It is a class I case, and after analyzing pillar 2.2, linear anchorage is performed.
As there were cavities in pillars 2.4 and 2.8, cast restorations were planned. Cavity preparation was done considering prosthetic restoration. This implied slightly more grinding of dental tissue to have the necessary widths in the wax-up phase.
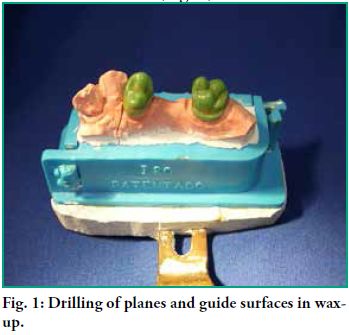
- • Proximal plane guides were drilled in the wax-up considering the axis of the mesial surface of 2.2 that will be drilled subsequently.
Guide surfaces were drilled on the lingual surfaces of both pillars with a cervical ridge. This allows for an accurate axis of insertion, effectively reciprocating the active arm for insertion and removal (Fig. 1).
When coming into contact with the cervical ridge, the passive arm provides support and axial transmission of forces.
Under-drilling these surfaces makes it possible to place a reciprocating ribbon arm that completes the dental anatomy without over-contouring the pillar.
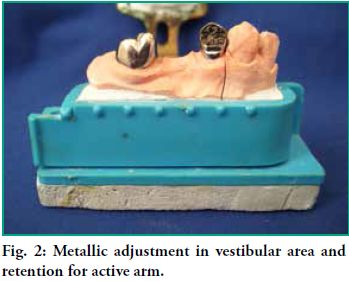
- • The restoration of 2.4 requires a veneer crown, therefore a vestibular gingival adjustment was made in metal, with a gingival occlusal height. This was done to place the active arm of the retainer and a 0.25 mm cavity of pinhole retention to provide the necessary, and not excessive, retention to that pillar (Fig. 2).
- • As 2.8 was not aesthetically compromised, a metallic crown was made with a retention of 0.50 mm for its active arm (Fig. 2).
- • Distal support in 2.4 which will hold an Akers clasp (Fig. 4).
- • Mesial and distal support in 2.8, to hold a ring clasp. As it is the last isolated pillar, it must not migrate distally (Fig. 4).
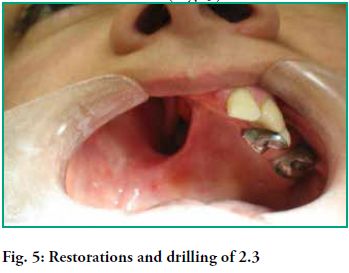
- Cingular support in 2.3 to provide support and a vestibule-lingual path to allow the passage of a minor connector towards the vestibular area, with an active circumferential arm (Fig. 5).
- Cingular support and a proximal guide plane in 2.2 enable us to place a proximal wedge which provides horizontal stability to the appliance and contributes to a single and accurate axis for insertion and removal.
Cobalt Chromium framework obturator:
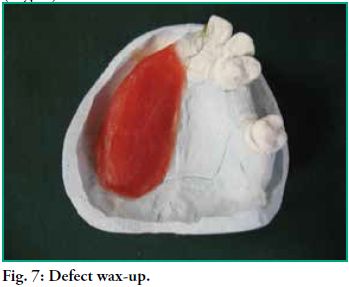
After having the final impression and emptying the model, the area of the defect is waxed, shaping and resizing the residual alveolar ridge that should be present in the area (Fig. 7).
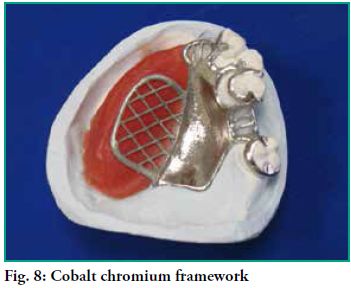
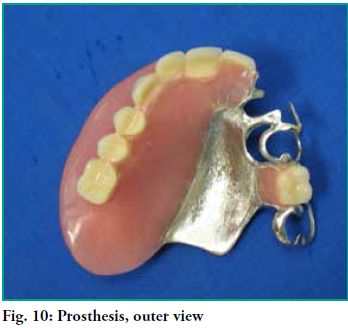
A maximum coverage framework is designed, where primary and secondary retainers come into contact with all the remaining pieces (Fig. 8).
Hence, when sending the impression to the chromium lab, it is requested that the saddle be placed where a normal maxilla would be. Further specifications:
-The location of the rests and the type of anchorage element in each pillar.
-Ribbon passive arms that provide support in the ridges drilled in 2.4 and 2.8.
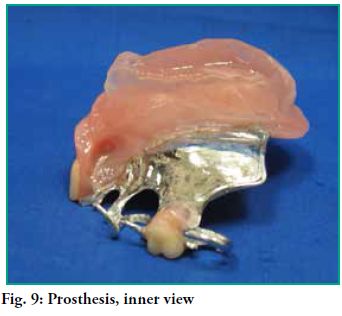
-The retentions drilled in the pillars are marked in the model so that the end of the active arm is placed there. The following stages are the same as in a conventional prosthesis (Figs. 9 and 10).
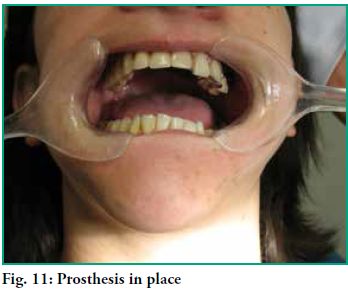
The obturator prosthesis is placed. The defect is properly closed (Fig. 11) and there is stable occlusion in maximum and eccentric occlusion ratios, hence with punctiform and low-intensity contacts in the area of the defect (Fig. 12).
There is a good final aesthetic effect as the active arm in 2.2 was eliminated and there is a single axis of insertion and removal that allows for excellent retention of the obturator prosthesis. There is controlled retention without overloading the pillar teeth (Fig. 12).
Good hygiene is essential to preserve tissues and the prosthesis. The patient is told about the need for regular check-ups, at least every 6 months. She is also told that after losing the initial adjustment, the prosthesis will need to be regularly relined given the normal modifications in the area.
Conclusions
The treatment of any tumor must include a biopsy and a histopathologic study. There must also be close multidisciplinary teamwork including the pathologist, the radiologist, the maxillofacial surgeon and the prosthetist.
Block resection is still the most accepted surgical procedure to treat odontogenic myxomas in larger lesions. For smaller lesions, enucleation and curettage are preferred.
In the case of partial obturators, it is essential to apply the concepts of cavity preparation that govern conventional partial removable prostheses. In this case, pillar teeth had to be restored. Otherwise, healthy teeth would have been prepared.
The prosthesis has been in use since October 2009. It was relined in 2012. It is close to reaching its service life, but it operates as it should, and support structures are in perfect health.
1. Alfaro L, Martínez B. Atlas de patología de los maxilares. Madrid: Ripano S.A.; 2011. 216-315.
2. Sapp JP, Eversole LR, Wysocki GP. Patologia oral maxilofacial contemporánea. 2da ed. Madrid: Mosby; 2005. 185-190.
3. Uruguay. Instituto Nacional de Estadística - Defunciones según causa de muerte en 1992. Estadística del movimiento natural de la población. Tomo I, Resultados básicos. Madrid: INE: ed. Artes gráficas, 1995, p.11-12.
4. Phillips RL, Garfinkel L, Kuzma JW, Beeson WL, Lotz T, Brin B. Mortality among California Seventh-Day Adventists for selected cancer sites. J. Natl Cancer Inst. 1980 Nov; 65(5):1097-107.
5. Boring CC, Squires TS, Tong T, Montgomery S. Cancer statistics. CA Cancer J Clin. 1994 Ene; 44(1):7-26.
6. Chen AY, Myers JN. Cancer of the oral cavity. Curr Probl Surg. 2000 Oct; 37(10):633-731.
7. Escamilla LE, Ruiz R, Mosqueda A. Mixoma odontogénico - presentación de caso clínico. Rev Odont Mex. 2012; 15(4):244-50.
8. Gómez M, Luengas JP. Fibromixoma odontogénico. An Pediatr [Internet]. 2005 Abr [citado 30 Set 2014]; 62(4):370-2. Disponible en: http://www.analesdepediatria.org/es/fibromixomaodontogenico/articulo/13073251/
9. LI, F. Inherited susceptibility to cancer. 86th Annual Meeting of the American Association for Cancer Research, March, 18-22, 1995, Toronto, Ontario, Canada. Proc Am Assoc Cancer res, 36, p. 638-9.
10. Jankielewicz I, Russo C. Técnica para confeccionar un obturador palatal flexible. Revista de Tecnología Dental. 1984 Ene; 6-11.
11. Cabrera, C. Rehabilitación bio psico social en Prótesis buco maxilo facial. marzo 15 de 2015. Disponible en http://www.odon.edu.uy/catedrasyserv/bmf/rehabilitacion_pbmf.htm
12. Vidulich de Rezende, JR. Fundamentos da Prótese Buco-Maxilo-Facial. San Pablo: Sarvier; 1997. (5) 61-68
13. Shifman A. Clinical applications of visible light-cured resin in maxillofacial prosthetics – Part 1:Denture base and reline material. J Prosthet Dent 1990 Nov; 64(5): 578-82
14. Wu YL, Schaaf NG. Comparison of wheight reduction in different designs of solid and hollow obturator prostheses. J Prosthet Dent. 1989 Ago; 62(2): 214-17.
15. Bocage M. Prótesis parcial removible - clínica y laboratorio. Montevideo: Bocage / Feuer; 2009, p. 278-286.
16. Crespo Y, Capín E, Alvarez A. Procederes básicos de Laboratorio en Prótesis Bucomaxilofacial. La Habana: CIMEQ; 2008: 134-163.
17. Cacciacane OT. Prótesis - bases y fundamentos. Madrid: Ripano S.A.; 2012, p. 488-514.
18. McGivney GP, Carr AB. McCracken prótesis parcial removible. Buenos Aires: Editorial Médica Panamericana; 2004.
19. Loza D, Valverde HR. Prótesis Parcial Removible - procedimientos clínicos y de laboratorio. Lima: Savia; 2012, p. 208-226.
20. Davenport JC, Basker RM, Heath JR, Ralph JP, Glantz PO. A clinical guide to Removable Partial Dentures. London: BDJ Books; 2000, cap 5.











 text in
text in