Services on Demand
Journal
Article
Related links
Share
Odontoestomatología
Print version ISSN 0797-0374On-line version ISSN 1688-9339
Odontoestomatología vol.17 no.25 Montevideo May 2015
Cast posts: a 44-year retrospective clinical study in a specialized private clinic
Borgia Botto Ernesto*, Barón Rosario**, Borgia José L.***
* Professor, Postgraduate Degree in Comprehensive Restorative Dentistry, Postgraduate School, School of Dentistry, Universidad de la República. Uruguay
eborgiabotto@gmail.com
** Professor, Operative Dentistry Clinical Department, School of Dentistry, Universidad de la República. Uruguay
*** Associate Professor, Prosthodontics Clinic, School of Dentistry, Universidad de la República. Uruguay
Abstract
Aim. The aim of this study was to examine the longitudinal clinical result of the use of cast posts and cores and crown restorations in endodontically treated teeth over a 44-year period. Materials and methods. Out of 130 randomly selected patients, 95 had had 297 teeth rehabilitated with cast posts and cores and crown restorations. The endodontic rehabilitation was considered successful when the tooth remained functional with no clinical or radiographic pathology. Results. The success rate was 90% (268) and the failure rate 10% (29). Cohen’s Kappa index ranged between 0.78 and 1. Conclusions. In this 44-year retrospective study, the clinical success rate was 90%. The mean survival time of the studied teeth was 19 years. The failure rate was 10%; tooth fractures were the most prevalent failures (5% of all restored teeth).
Keywords: Endodontically treated teeth, Root anchorage, Tooth fracture, Bruxism, Clinical success.
Received on: 25.02.15 - Accepted on: 26.03.15
Introduction
Endodontically treated teeth (ETT) are often structurally compromised due to several factors (1-4). ETTs may be restored with cast posts, which provide adequate retention for crowns restorations or fixed dental prostheses (FDPs) (5, 6).
Cast posts rate of success varies according to the literature, biomechanical failures being the most common ones. Post loosening and tooth fractures are the most frequent failures (7-11). Recurrent caries and apical periodontitis are less prevalent (9, 12).
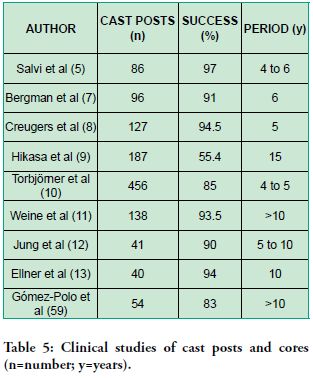
Long-term (over 10 years) longitudinal clinical studies are rare. Five such studies showed varying degrees of success ranging from 55% to 94% (9.11-13.59). This lack of long-term studies and the varying results reported make the analysis of a 44-year study documented clinical results particularly interesting.
The aim of this retrospective investigation was to evaluate the longitudinal clinical outcomes of cast posts and cores used in the rehabilitation of ETTs as carried out by the first author in his private practice for 44 years.
Materials and methods
The Inclusion Criteria for the sample was that the patients to be evaluated must have attended the first author’s clinic for at least 3 years and they had to be current patients.
Out of 2552 registered patients, excluding those who had moved or passed away, 210 met this requirement. Of these, 140 patients were selected at random by a dental assistant, who did not know the aim of the selection. This sample was considered appropriate by the authors. These 140 patients were invited to a clinical examination between November 2013 and April 2014: 130 agreed to participate while 10 declined for personal reasons. Among the examined patients, 95 had ETTs, in total 297 cast posts and cores in noble alloy.
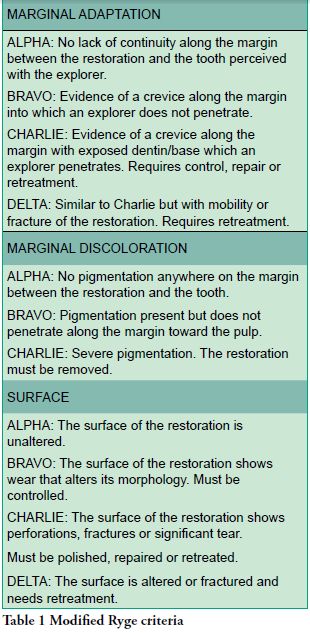
All the clinical restorations were carried out by one operator (the first author). The co-authors participated as independent evaluators. The calibration between the evaluators and the first author was carried out previously on 120 restorative procedures outside the sample. The quality analysis of the restorations was based on modified Ryge (14) criteria (Table 1). Cohen’s Kappa Coefficient ranged between 0.78 and 1 (15), which is rated as excellent in the Fleiss Guide (16).
Patient-based data collected from the clinical history and the examination were registered on specially designed forms. The patients were examined clinically and radiographically. In case of disagreement regarding the assessment of the quality of restorations, the lowest rating was assigned.
The inclusion criteria applied for the cast posts were as follow:
- The post under study had to have been functional for at least two years, in individual teeth or abutments of fixed dental prosthesis (FDPs).
- Having X-ray tests of the teeth under study taken in the last 12 months.
- One-piece gold onlay and metal ceramic crown with posts were taken as cast posts.
- Existing cast posts not made by the operator but which he deemed acceptable for crown retreatment were included from the moment the new rehabilitation was placed.
The success criteria for the cast posts and cores were as follows:
- ETT rehabilitated with a cast post and a crown restoration was still clinically in function and pathology-free.
- Radiographic examination of the rehabilitated ETT did not show apical pathology.
When preparing the tooth, the author: tried to preserve the maximum amount of coronal dentin; avoided drilling the root canal more than one third of the mesial-distal width of the root; tried to preserve at least 4 mm of remaining apical endodontic sealing and to reach a post crown-root ratio of 1-1 to 1-1.5 when possible.
Variables analyzed: age, sex, X-ray tests, distribution in the dental arches, type of cement, decay, parafunctional habits, maintenance therapy, success, failures and survival of cast posts.
Data processing was done using Epidat 3.1 software developed by the Consellería de Sanidade de la Xunta de Galicia with the support of PAHO-WHO and SPPS 13.0. In all cases, the variables considered were taken as corresponding to an identically distributed independent random variable, generated from a probability sample. A result is considered statistically relevant when, upon the rejection of a null hypothesis, the probability of error is below 5%. Statistical significance was set at P< 0.05. When analyzing the complete and censored values, the mean and the median were used to describe the central tendency.
Results
The sample consisted of 70 women and 25 men, with a ratio of 2.8 women/men. The median age was 67 in women (range: 40 to 80) and 69 in men (range: 42 to 71), there being no statistically significant differences between the sexes. The treatment period for these patients varied between 3 and 44 years. The average period was 27 years.
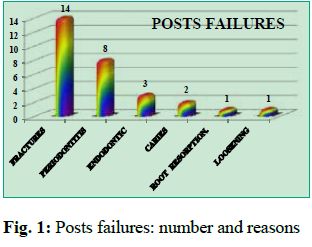
Out of 297 cast posts, 268 (90%) were still functional. Twenty-nine (10%) failed: 19 in single teeth and 10 in abutments of FDPs. The number of and reasons for failure are shown in Fig 1. Twenty-six teeth (9%) were lost.
The radiographic examination showed apical radiolucencies in three patients, which were considered non-pathological since they showed no macroscopic variations in 9, 21, and 23-year periods respectively (17). It was also noted that three chronic periapical processes which had been treated by means of apicoectomies had healed.
During the follow-up period, caries was found in only one crown restoration (0.4%) of the functioning teeth: the lesion was treated conserving the original treatment.
All of the 22 existing posts used were still in function but it was not possible to know the alloy type. The other 246 functioning casts made by the first author were cast in gold alloy type III or noble alloy (Ag, Pd, Au). All cast posts and cores were luted with zinc phosphate cement and one loosened (0.4%): a new cast post and core was placed.
At the time of the evaluation, two aluminous porcelain crowns on the same patient, with a survival time of 38 years and 7 months, fractured and had to be replaced with metal-free ceramic crowns, while maintaining the existing cast posts.
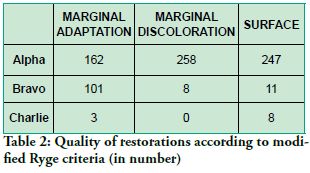
The 266 functional crown restorations were distributed as follows: 189 single full crown restorations, 65 abutments of FDPs and 12 crown-root restorations in one piece (8 onlays in gold alloy type III and 4 metal-ceramic crowns in gold (Au, Pd) or noble alloy (Ag, Pd)). According to modified Ryge criteria (14), the quality of these restorations is presented in Table 2. The combined quality analysis of each restoration showed that 255 (95%) restorations reached levels of clinical acceptance (rate: Alpha or Bravo in marginal adaptation, marginal discoloration and surface).
Two hundred and ninety-seven posts under study were between 31 months (2 years, 7 months) and 532 months (44 years, 4 months) old.
The observed survival time of the posts may be broken down as follows:
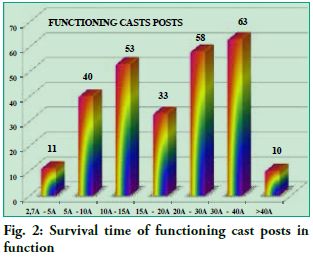
- The 268 posts which were still functional had an average survival time of 231 months (19 years, 3 months), and the upper quartile of 388 months (32 years, 4 months). Of the cast posts still in function, the survival time was >20 years for 49%, between 10 and 20 years for 32%, and <10 years for 19% (Fig. 2).
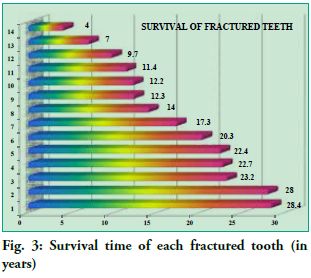
- The observed survival time of the 29 cast posts that failed was 208 months (17 years, 4 months), and the upper quartile of 282 months (23 years, 6 months). Of the 14 fractures, 43% had a survival time of between 20 and 28 years, 36% between 10 and 20 years, and 21% less than 10 years (Fig. 3).
There was no difference in survival rate of cast posts between men and women (Mantel-Cox Log-Rank test “P” = 0.54).
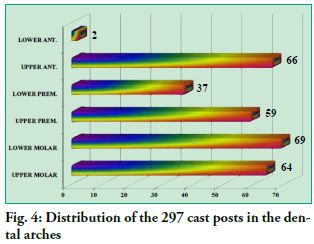
The distribution of the 297 cast posts in the dental arches is shown in Fig. 4. The mandibular incisors and premolars were the most seldom treated teeth, whereas the distribution of the cast posts was similar in the other groups of teeth.
Of the 14 tooth fractures, 5 occurred in the maxillary anterior and 5 in the maxillary premolar teeth, whereas 4 occurred in the molars, two in each jaw.
At the clinical evaluation, 20 asymptomatic patients had parafunctional wear facets (the activity was not assessed); 26 reported nocturnal bruxism and were using occlusal stabilization splints; 6 were being treated for signs and symptoms of Temporo- Mandibular-Disorders (TMD) with occlusal devices and other therapies; and 17 had been in treatment for bruxism.
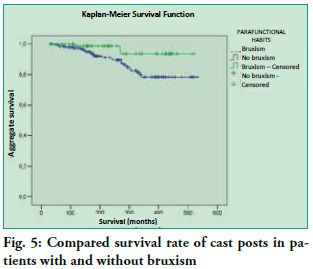
If these 4 groups of patients are considered jointly, 69 of the 95 patients (73%) have or had a history of parafunction in the observed period. Patients with reported parafunction had statistically significantly lower survival rate of cast posts than those without parafunctional habits. (Mantel-Cox Log-Rank test “P” = 0.020) (Fig. 5).
The survival rate of the cast posts fit a multivariate Cox regression model (Table 3), including sex, age, bruxism and maintenance as explanatory variables (Chi-square omnibus test “P” = 0.01). The older the patient, the lower the survival rate of the ETT. Women showed a higher survival rate than men.
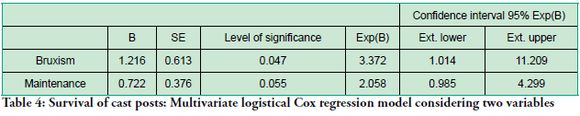
Survival rates of cast posts are aligned with a simpler logistical Cox regression model (Table 4), with bruxism and maintenance as explanatory variables (Chi-square omnibus test “P” =0.009).
There was a statistically significant relationship between bruxism and ETT survival time, both at univariate (Mantel-Cox test “P” = 0.02) and multivariate levels (Cox regression model “P”=0.047). The probability of a lower survival rate for ETTs among patients with bruxism was 3.37 times higher than for patients without a diagnosis of bruxism.
Only 37 patients (39%) attended at least once a year to receive maintenance therapy. ETTs with no maintenance showed a higher survival rate (“P”= 0.055) than those who had maintenance. However, out of a total of 14 fractures, nine were recorded for ETTs without maintenance (OR=1.17). The ETTs of patients with bruxism who had not had any maintenance had 1.59 more chances of presenting fractures (Relative risk 1.59 IC 95% 1.05 – 2.41).
Discussion
This retrospective study covering 44 years shows a 90% success rate of ETTs after a mean survival of 19 years. Regarding the long observation period, the results can be considered excellent when compared to other clinical international studies (Table 5). Only one study presented results after 15 years with a success rate of 55% (9) and three studies over about ten years reported success rates of 83% (59) to 94% (11,13).
When considering occlusal forces, sex could be a variable related to the integrity of the rehabilitated ETT. Indeed, the maximum occlusal force developed by women has been reported to be 597 N, significantly lower than that of men, which reached 847 N. Fifty-five percent of this force is exerted at second molar level, with a 20% reduction in the incisors. However, in men with parafunctional habits, the force may go from 911 N at the molars to 597 N in the incisors (18).
Only a few studies have examined age, sex, bruxism and frequency of the maintenance therapy (9, 12, 19, 20). Statistical analysis in this study showed that age, sex, bruxism and maintenance, with different association values, were related to the survival of ETTs rehabilitated with a cast post and a crown restoration.
In a cross-sectional study to determine the prevalence of TMD and bruxism in Uruguay, the prevalence of active bruxism was reported to be 31%. Female prevalence was strongly predominant (21). Comparable results in epidemiological studies of TMD have been presented elsewhere (22).
In this study the prevalence of active bruxism was 27%, thus in relative accordance with the papers mentioned above. According to the data previously presented, 69 of the 95 patients (73%) in the observed period have or had a history of parafunction.
Heavy forces caused by parafunction may be a risk factor for the integrity of the ETTs rehabilitated with a cast post and a crown restoration. In fact, 12 of the 14 fractures occurred in patients diagnosed with bruxism. Five teeth fractures occurred in maxillary premolars and 5 in maxillary anterior teeth, which can suggest that the type of tooth, the location in the dental arch and parafunctional non-axial strong forces might be risk factors for tooth fracture.
The use of posts has decreased in recent years. In many ETTs with large coronal remnants, it is possible to make restorations using adhesive procedures, without the need for root anchorage (23). There are laboratory (24-30) and clinical studies (31, 32) supporting this. Some clinical studies into ETTs with large coronal remnant, restored with or without post and a single crown, showed similar clinical results (5, 8, 40, 41). Therefore, coronal remnants and type of restoration could be more important than the post. However, further longer-running clinical studies are needed.
Furthermore, laboratory studies have shown that the best protection against fractures is the presence of 2 mm or more of coronal dentin, which allows for the ferrule or clamp effect (33). A uniform coronal remnant of 2 mm in height is more important than the length of the post (34, 35) and more important than the length of the post and the type of cement used (36). When the coronal remnant is not uniform, the location and the volume of the remnant affect the resistance to fracture (37, 38). The possibility of covering the coronal remnant with the cast post increases its resistance to fracture by 30% (39).
Five clinical prospective studies (8, 13, 40-42), three retrospectives studies (9, 12, 43) and a review (44) concluded that the coronal remnant was the most highly predictable factor in the longitudinal success of ETTs. This very important variable cannot be assessed scientifically in this work because the presence and location of the coronal remnant for each case was not recorded. However, the good clinical outcome may be attributed to the existence of a single operator (45) who followed the above recommendations, aiming at preserving the dental structure as much as possible.
In laboratory studies, the adhesive resistance of fiber posts was equivalent to gold posts, whether adhesively or conventionally cemented (36, 46). Cast posts had higher retention values when cemented with zinc phosphate cement than with resin cements (47, 48).
Donovan and Cho (49) consider zinc phosphate cement the cement of choice for cast posts, gold and metal ceramic restorations. In the present study, zinc phosphate cement was used, and only one post loosened, which would support these authors’ view.
Several clinical studies have shown that loosening of cast posts and tooth fractures were the most frequent reasons for failures (7-11), while caries and periodontitis were less prevalent (9, 12). About half the failures (48%) in this study were root fractures, whereas loosening and caries were rare causes of failure.
The fractures could be related to the position in the dental arches, presence and location of the coronal remnant, thickness of the root walls, parafunctional forces, the high elasticity module of the post and the absence of a periodical functional occlusal control. Furthermore, the loss of pulp tissue reduces proprioception, increasing the risk of overloads and fractures (50-52).
On the other hand, some researchers consider occlusal design to be more important than the kind of post (19, 20).
Laboratory studies showed that in endodontically treated premolars with MOD cavities, bonded ceramic inlays did not reinforce the remnant dental structures (28, 53) while endodontically treated premolars with MOD cavities increased their resistance to fracture with bonded cast onlays (25, 29).
The design of tooth preparation and the type of restoration could influence clinical success. Of the successful ETTs, 181 had a full crown restoration which fully embraced the dental structure. Eighty-two posterior partial restorations were gold onlays and 5 bonded ceramic onlays, which mainly transmit compressive forces to the teeth (27). Furthermore, according to some studies (54-57), the good quality evaluation of these restorations could have influenced the good result of endodontic treatment and therefore the success of the restored ETTs.
Considering the kind of restoration, the survival rate was 91% for single teeth and 84% for abutments of FDPs, indicating a higher risk of failure for ETTs as abutments in FDPs. This agrees with the meta-analysis in a systematic review by Ploumaki et al (58) showing 92% success rate for single crowns and 79% for FDPs.
Therefore, according to the results of this research, a long survival of ETT restored with cast post and core in gold or noble alloy and a crown restoration can be expected, but several factors must be considered to reach a good level of clinical success.
Conclusions
In this retrospective study covering 44 years, the clinical success of ETTs rehabilitated with cast posts and cores in gold or noble alloy and a crown restoration was high: 90% for a mean survival time of 19 years. The failure rate was 10%. Tooth fracture was the most prevalent reason for failure (5% of all restored teeth and half of the failures), whereas cases of caries and loosening were rare.
This research also showed that the clinical success of cast posts and cores, in gold or noble alloy, was related to different factors, and that the clinician must bear in mind the several variables that could statistically influence these results.
Acknowledgements
Thanks to Professor Emeritus Dr. Gunnar E. Carlsson for his comments and suggestions on the manuscript.
Conflict of interest
The authors reported no conflicts of interest related to this study.
2. Jameson MW, Hood JA, Tidmarsh BG. The effects of dehydratation and rehydratation on some mechanical properties of human dentin. J Biomech 1993;26:1055-1065.
3. Goldsmith M, Gulabivala K, Knowles JC. The effect of sodium hypochlorite irrigant concentration on tooth surface strain. J Endod 2002;28:575-579.
4. Souza Bier CA, Shemesh H, Tanomaru-Filho H, Wesselink PR, Wu M. The ability of different nickel-titanium rotary instruments to induce dentinal damage during canal preparation. J Endod 2009;35:236-238.
5. Salvi GE, Siegrist BE, Amsta T, Joss A, Lang NP. Clinical evaluation of root filled teeth restored with or without post and core systems in an specialist practice setting. Int Endod J 2007;40:209-215.
6. Ferrari M, Vichi A, García-Godoy F. Clinical evaluation of fiber-reinforced epoxy resin posts and cast post and cores. Am J Dent 2000;13:15B-18B.
7. Bergman B, Lundquist P, Sjögren U, Sundquist G. Restorative and endodontic results after treatment with cast posts and cores. J Prosthet Dent 1989;61:10-15.
8. Creugers NH, Mentink AG, Fokkinga WA, Kreulen CM. 5-year follow-up of a prospective clinical study on various types of core restorations. Int J Prosthodont 2005;18:34-39.
9. Hikasa T, Matsuka Y, Mine A, Minakuchi H, Hara ES, Van Meerbeek B, Yatani H, Kuboki T. A 15-year clinical comparative study of the cumulative survival rate of cast metal core and resin core restorations luted with adhesive resin cement. Int J Prosthodont 2010;23:397-405.
10. Torbjörner A, Karlsson S, Odman PA. Survival rate and failure characteristics for two post designs. J Prosthet Dent 1995;73:439-444.
11. Weine FS, Wax AH, Wenckus CS. Retrospective study of tapered, smooth post system in place for 10 years or more. J Endod 1991;17:293-297.
12. Jung RE, Kalkstein O, Sailer I, Roos M, Hämmerle ChHF. A comparison of composite post buildups and cast gold post-and-core buildups for the restoration of non vital teeth after 5 to 10 years. Int J Prosthodont 2007;20:63-69.
13. Ellner S, Bergendal T, Bergman B. Four post-and-core combinations as abutments for fixed single crowns: a prospective up to 10-year study. Int J Prosthodont 2003;16:249-254.
14. Ryge G. Clinical criteria. Int Dent J 1980;30:347-358.
15. Cohen J, Weighed Kappa: Nominal scale agreement with prevision for scaled disagreement or partial credit. Psychological Bulletin, 1968;70:213-220.
16. Fleiss J L. Statistical methods for rates and proportions (2nd. Ed), New York: John Wiley, 1981:38-46.
17. Friedman S, Abitbol S, Lawrence HP. Treatment outcomes in endodontics: the Toronto Study. Phase 1: initial treatment. J Endod 2003;29:787-793.
18. Arlan CV, Dimitriu B, Arlan VV, Bodnar D, Suciu I. Current opinions concerning the restoration of endodontically treated teeth: basic principles. J Med Life 2009;15:165-172.
19. Fokkinga WA, Kreulen CM, Vallittu PK, Creugers NHJ. A structural analysis of in vitro failure loads and failure modes of fiber, metal and ceramic post and core systems. Int J Prosthodont 2004;17:476-482.
20. Torbjörner A, Fransson B. A literature review on the prosthetic treatment of structurally compromise teeth. Int J Prosthodont 2004;17:369-376.
21. Riva R, Sanguinetti M, Rodríguez A, Guzzetti L, Lorenzo S, Alvarez R, Massa F. Prevalencia de trastornos témporo mandibulares y bruxismo en Uruguay. Odontoestomatología 2011;17:54-71.
22. Carlsson GE, MagnussonT. Epidemiologic studies of TMD. En: Carlsson GE, Magnusson T. Management of Temporomandibular Disorders in the general dental practice. Quintessence,1999:13-17.
23. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature-Part 1. Composition and micro and macrostructure alterations. Quintessence Int 2007;38:737-743.
24. Reeh ES, Douglass WH, Messer HH. Stiffness of endodontically treated teeth related to restoration technique. J Dent Res 1989; 88:1540-1544.
25. Costa LC, Pegoraro LF, Bonfante G. Influence of different metal restorations bonded with resin on fracture resistance of endodontically treated maxillary premolars. J Prosthet Dent 1997;77:365-369.
26. Salis SG, Hood JA, Stokes AN, Kirk E. Patterns of indirect fracture in intact and restored human premolar teeth. Endodon Dent Traumatol 1987;3:10-14.
27. Magne P, Belser UC. Porcelain versus composite inlays/onlays : effects of mechanical loads on stress distribution, adhesion and crown flexure. Int J Periodontics Restorative Dent 2003; 23:543-555.
28. St-Georges AJ, Sturdevant JR, Swift EJ Jr, Thompson JY. Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent 2003;89: 551-557.
29. Yamada Y, Tsubota Y, Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont 2004;17: 94-98.
30. Krejci I, Duc O, Dietschi D, De Campos E. Marginal adaptation, retention and fracture resistance of adhesive composite restorations on devital teeth with and without posts. Oper Dent 2003;28:127-135.
31. Rocca GT, Rizcalla N, Krejci I. Fiber-reinforced resin coating for endocrown preparations: a technical report. Oper Dent 2013;38:242-248.
32. Rocca GT, Krejci I. Crown and post-free adhesive restorations for endodontically treated posterior teeth: from direct composite to endocrowns. Eur J Esthet Dent 2013;8:156-179.
33. Sorensen J, Engelman M. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent 1990;63:529- 539.
34. Akkayan B. An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowell systems. J Prosthet Dent 2004;92:155-162.
35. Isidor F, Brondum K, Ravnholt G. The influence of post length and crown ferrule length on the resistance to cycling loading of bovine teeth with prefabricated titanium posts. Int J Prosthodont 1999;12:78-82
36. Messomo E, Massa F, Dalla Libera S. Fracture resistance of teeth restored with two different post and core designs cemented with two different cements: an in vitro study. Part 1. Quintessence Int 2003;34:301-306.
37. Tan PLB, Aquilino SA, Gratton DG, Stanford CM, Tan SCh, Johnson WT, Dawson D. In vitro fracture resistance of endodontic treated central incisors with varying ferrule heights and configurations. J Prosthet Dent 2005;93:331-335.
38. NG CC, Dumbrigue HB, Al-Bayat MI, Griggs JA, Wakefield CW. Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J Prosthet Dent 2006;95:290-296.
39. Barkhordar RA, Radke R, Abbasi J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent 1989;61:676-678.
40. Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: a prospective observational clinical study. J Endod 2012;38:432-435.
41. Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH. Up to 17-year controlled clinical study on post-and-cores and covering crowns. J Dent 2007;35:778-786.
42. Sterzenbach G, Franke A, Naumann M. Rigid versus flexible dentine-like endodontic posts clinical testing of a biomechanical concept: seven-year results of a randomized controlled clinical pilot trial on endodontically treated abutment teeth with severe hard tissue loss. J Endod 2012;38:1557-1563.
43. Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent 1984;52:28-35.
44. Soares CJ, Correia Miranda Valdivia AD, Rodrigues da Silva G, Ribeiro Santana F, Meneses M de S. Longitudinal clinical evaluation of post systems: a literature review. Braz Dent J 2012;23:135-140.
45. Frankenberger R, Reinelt C, Petschelt A, Krämer N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent Mater 2009;25:960-968.
46. Kremeier K, Fasen L, Klaiber B, Hofmann N. Influence of endodontic post type (glass fiber, quartz fiber or gold) and luting material on push-out bond strength to dentin in vitro. Dent Mater 2008;24:660-666.
47. Habib B, Von Fraunhofer JA, Driscoll CF. Comparison of two luting agents used for the retention of cast dowel and cores. J Prosthodont 2005;14:164-169.
48. Schwartz RS, Murchison DF, Walker IIIWA. Effects of eugenol and non eugenol endodontic sealer cements on post retention. J Endod 1998;24:564-567.
49. Donovan TE, Cho GC. Contemporary evaluation of dental cements. Compend Contin Educ Dent 1999;20:197-199,
50. Randow K, Glanz PO. On cantilever loading of vital and no vital teeth. An experimental clinical study. Acta Odontol Scand 1986;44:271-277.
51. Jacobs R, Van Steenberghe D. Role of periodontal ligament receptors in the tactile function of teeth: a review. J Periodont Res 1994;29:153-67.
52. Jacobs R, Van Steenberghe D. From osseoperception to implant-mediated sensory- motor interactions and related clinical implications. J Oral Rehabil 2006;33:282-92.
53. Hanning C, Westphal C, Becker K, Attin T. Fracture resistance of endodontically treated maxillary premolars restored with CAD-CAM ceramic inlays. J Prosthet Dent 2005;94:342-349.
54. Iqbal MK, Johansson AA, Akeel RF, Bergenholtz A, Omar R. A retrospective analysis of factors associated with the periapical status of restored endodontically treated teeth. Int J Prosthodont 2003;16:31-38.
55. Valderhaug J, Jokstad A, Ambjornsen E, Norheim P W. Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent 1997;25:97-105.
56. Tronstad L, Asbjornsen K, Doving L, Pedresen I, Eriksen HM. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol 2000;16:218-221.
57. Gillen BM, Looney SW, Gu LS, Loushine BA, Weller RN, Pashley DH, Tay FR. Impact of the quality of coronal restorations versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod 2011;37:895-902.
58. Ploumaki A, Bilkhair A, Tuna T, Stampf S, Strub JR. Success rates of prosthetic restorations on endodontically treated teeth: a systematic review after 6 years. J Oral Rehabil 2013;40:618-630.
59. Gómez-Polo M, Llidó B, Rivero A, Del Río J, Celemín A. A 10-year retrospective study of the survival rate of teeth restored with metal prefabricated posts versus cast metal posts and cores. J Dent 2010;38:916-920.
 All the contents of this journal, except where otherwise noted, is licensed under a Creative Commons Attribution License
All the contents of this journal, except where otherwise noted, is licensed under a Creative Commons Attribution License











 text in
text in