Serviços Personalizados
Journal
Artigo
Links relacionados
Compartilhar
Odontoestomatología
versão On-line ISSN 1688-9339
Odontoestomatología vol.16 no.24 Montevideo nov. 2014
Retention probability of permanent mandibular second molars (Pilot study)
Sandoval Vidal Paulo*,
Bizcar Mercado Betty **
* Dental Surgeon. Master’s Degree in Education. Orthodontics and Dentomaxillofacial Orthopedics Specialist. Director of the Program of Specialization in Orthodontics and Dentomaxillofacial Orthopedics. Universidad de la Frontera, Temuco, Chile. paulosandoval@ufrontera.cl
** Dental Surgeon. Degree in Pediatric Preventive and Interceptive Orthodontics. Currently doing a Master’s Degree in Dentistry. Universidad de la Frontera, Temuco, Chile.
Sandoval Vidal Paulo*,
Bizcar Mercado Betty **
* Dental Surgeon. Master’s Degree in Education. Orthodontics and Dentomaxillofacial Orthopedics Specialist. Director of the Program of Specialization in Orthodontics and Dentomaxillofacial Orthopedics. Universidad de la Frontera, Temuco, Chile. paulosandoval@ufrontera.cl
** Dental Surgeon. Degree in Pediatric Preventive and Interceptive Orthodontics. Currently doing a Master’s Degree in Dentistry. Universidad de la Frontera, Temuco, Chile.
Abstract
Objectives. To estimate the prevalence of Bruxism and Temporomandibular Disorders (TMD) in two populations: a nationwide sample (Uruguay) and another sample formed by patients in treatment for problematic drug use in Portal Amarillo. Method. Two cross-sectional, descriptive and analytical studies: one nationwide and the other one in Portal Amarillo. Results. Portal Amarillo: TMD symptoms 67.6%, bruxism symptoms 33.8%, current TMD clinical signs 42.3%, current or past bruxism signs 47.9%. Nationwide sample: TMD symptoms 61.3%, bruxism symptoms 27.7%, current TMD signs 37.3%, current or past bruxism signs 67.5%. Conclusions. Trend that signals a higher prevalence of current TMD and bruxism in Portal Amarillo than in the nationwide sample. Current or past bruxism signs are more prevalent in the nationwide sample. New research should review the effects of the medication administered to treat the addiction before and during the treatment. Meanwhile we recommend the use of occlusal devices to minimize the side-effects on the structures of the masticatory system.
Keywords: Prevalence, Bruxism, Temporomandibular Disorders (TMD), Drug Dependence.
Received on: 04 Mar 2014 – Accepted on: 18 Aug 2014
Introduction
Failure of eruption of lower second molars (MM2) is a relatively rare eruption complication. However, its prevalence has increased in the last few years; Bondemark & Tsiopa in 2007 (1) observed a prevalence of 0.8% (retention and impaction), Cho et al. in 2008 (2) found a frequency of 1% (impaction), Shapira et al. in 2011 (3) reported a prevalence of 1.4% in Israeli children and of 2.3% in Chinese-American children (impaction) and in 2013 Cassetta et al. (4) reported a prevalence of 1.36% (impaction). Dental crowding and insufficient space between the distal face of the first molar and the front edge of the ramus are cited as causes for eruption failure of MM2 (5). Retention of MM2 appears most frequently on one side, with mesial molar inclination (4), but clearly the most prevalent characteristic is increased angulation of the second molar, described for the first time by Evans in 1988 (6) and then by Ferro and Sonis (7, 8). This angle is measured at early ages to be able to standardize its value so that the clinician can predict the risk of impaction and thus make an early diagnosis.
This enables us to provide interceptive therapy, which in turn can help avoid the serious consequences of the impaction of the permanent second molar. Besides, there is agreement regarding the fact that treatment is more successful and presents fewer complications when dental organs have immature apices and a more resilient and vascularized bone structure (9, 10).
Materials and methods
A cross-sectional study was conducted using non-probability, consecutive sampling from a universe of 4,500 records of initial consultations in two private clinics in the city of Temuco, Chile. The records of 2095 individuals of both sexes were analyzed. Criteria for inclusion: clinical records with printed panoramic radiographies taken between 2008 and 2013 to children aged between 7 and 13, with at least one second permanent molar with mesial contact point located under the amelocemental junction of the first permanent molar. Criteria for exclusion: presence of syndromic pathology and second permanent molar absent or divergent (distal coronal inclination). The sample was formed by 370 clinical records that fulfilled the criteria for inclusion. Finally, 740 permanent lower second molars were analyzed. The variables measured were angle of second molar (Fig.1), angle of first and second permanent lower molars in relation to occlusal plane (Fig. 2), invasion of distal space of first molar by second molar (Fig. 3), distance between distal edge of first molar and front edge of ramus (Fig. 4).
We also measured the distance between the mesial contact point of the second molar and the amelocemental junction of the first permanent molar. To measure the angle of the second molar two lines were drawn: one in the center of the axis of the first molar and the other in the second molar. To preserve objectivity in the lines, three midpoints were determined in both molars: coronal, cervical and apical (Fig.1).
To determine the angles with regard to the occlusal plane, the central lines of the axis of the molars and a line drawn on the occlusal plane on the right side and another on the left side were used (Fig. 2). To determine distal invasion of the first molar, a line parallel to the axis of the first molar was drawn. The line went through the most distal point of the crown. Then, the area of the second molar within this space was measured in millimeters (Fig. 3). To determine distal space of the first molar, the most distal point of the crown of the first molar was determined and a line parallel to the axis of the first molar was drawn. Then a line on the front edge of the ramus was drawn, and the line of the occlusal plane was extended distally. Finally, measurements were taken in mm following the occlusal line (Fig. 4). An Excel spreadsheet was used to record the data, and a manual direct method was used to measure the elements on the panoramic radiographies. The instruments used to take the measurements were acetate sheets (cephalometric analysis) and lead pencil, and to measure the angles a goniometer (BaselineTM CE Diagnostic and Measuring Instruments) was used. Descriptive statistics were applied using SPSS 15.0.1 for Windows (LEAD Technologies, Inc. 2006).

Fig. 1. Angle of inclination between 1st and 2nd lower permanent molar

Fig. 2. Inclination of 1st and 2nd molars in relation to occlusal plane and front edge of ramus

Fig. 3. Invasion of 2nd molar in distal face of 1st permanent molar
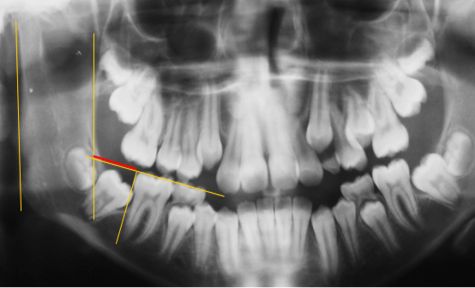
Fig. 4. Distance between distal edge of 1st permanent molar
Results
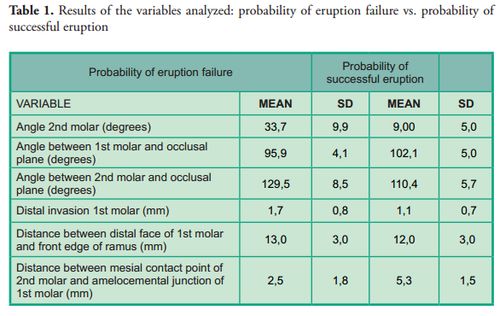
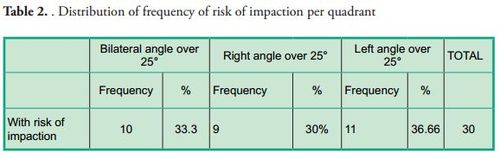
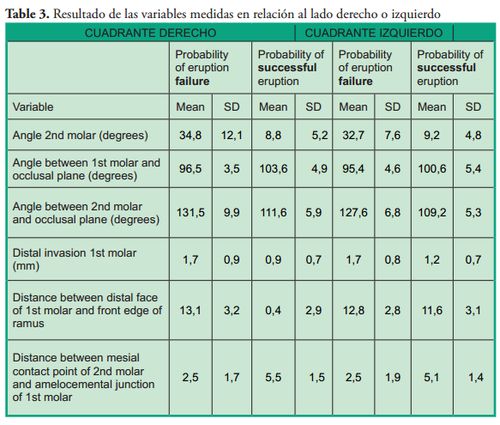
Patients with probability of eruption failure amounted to 1.43% of the sample, their mean age was 10 ± 1.7 years, and 73.3% of them were female. The variable used to determine the probability of success or failure of eruption was the angle of the second molar: an angle equal to or smaller than 24° showed probability of successful eruption, whereas an angle equal to or greater than 25° was considered with probability of eruption failure according to the average established by Evans in 1988 (average of 25° with a range from 15° to 65°). Tables 1, 2 and 3 show the results of the variables studied and their relation with the probability of teeth eruption or noneruption, unilateral or bilateral presence and distribution per quadrant.
Discussion
This study of mixed dentition was conducted in the field of dental development with the aim to help prevent dento-maxillary anomalies in permanent dentition. We evaluated variables already studied by other authors to determine if this sample behaves in a similar way as previous samples or if it differs in some aspects. We found a 1.43% frequency of eruption failure of the second permanent molar. This percentage is similar to the results of Bondemark & Tsiopa in 2007 (1), who observed a prevalence of 0.8%, and of Cho et al. in 2008, which was of 1% (2). It differs from the findings of Sonis & Ackerman in 2011: 8.5% (8). Regarding the age of patients, we found a mean age of 10, as opposed to Sonis & Ackerman who reported a mean age of 11.2 years (8); 12.8 years for Evans (6) and 15 years for Magnusson & Kjellberg in 2009 (11). Regarding the angle of the second permanent molar, this study found a range from 25 to 80 degrees, which is similar to the findings of Cho et al. (13 to 75 degrees); Evans (15 to 65 degrees) and Sonis & Ackerman (19 to 33 degrees). The ranges described in the measurements of this angle are quite similar, which allows us to infer that patients with an angle included in the above ranges should be periodically checked. The invasion of the distal space of the first molar by the permanent second molar was of 1.7 mm in this study, which is greater than the invasion described by Sonis & Ackerman (0.57 mm). The angle of the second molar with regard to the line of the occlusal plane of this study was of 129.5 ± 8.5, which is smaller than the angle found by Shapira et al. in 2011 (134.66 ± 12.07).
Conclusions
The prevalence of risk of impaction of the lower second molar is low. The invasion of the distal face of the first molar in this study was greater than what was found in other studies. Risk of unilateral impaction is more frequent. Greater frequency of risk of impaction was found on the left side. No correlation was found between the size of the distal space of the first molar and the front edge of the ramus, and the risk of impaction of the second molar.
Referencias
1. Bondemark L, Tsiopa J. Prevalence of ectopic eruption, impaction, retention and agenesis of the permanent second molar. Angle Orthod. 2007; 77(5):773-8.
2. Cho SY, Ki Y, Chu V, Chan J. Impaction of permanent mandibular second molars in ethnic Chinese schoolchildren. J Can Dent Assoc. 2008; 74(6):521.
3. Shapira Y, Finkelstein T, Shpack N, Lai YH, Kuftinec MM, Vardimon A. Mandibular second molar impaction. Part I: Genetic traits and characteristics. Am J Orthod Dentofacial Orthop. 2011; 140(1):32-7.
4. Cassetta M, Altieri F, Di Mambro A, Galluccio G, Barbato E. Impaction of permanent mandibular second molar: A retrospective study. Med Oral Patol Oral Cir Bucal [en línea]. 2013; 18(4):e564-8. Fecha de acceso: marzo 2014. Disponible en:
http://www.medicinaoral.com/pubmed/medoralv18_i4_p564.pdf
5. Grover PS, Lorton L. The incidence of unerupted permanent teeth and related clinical cases. Oral Surg Oral Med Oral Pathol. 1985; 59(4):420-5. 6.
6. Evans R. Incidence of lower second permanent molar impaction. Br J Orthod. 1988; 15(3):199-203.
7. Ferro F, Funiciello G, Perillo L, Chiodini P. Mandibular lip bumper treatment and second molar eruption disturbances. Am J Orthod Dentofacial Orthop. 2011; 139(5):622-7.
8. Sonis A, Ackerman M. E-space preservation. Angle Orthod 2011; 81(6):1045-9. Fecha de acceso: marzo 2014. Disponible en: http://www.angle.org/doi/abs/10.2319/030711-165.1
9. Johnson JV, Quirk GP Surgical repositioning of impacted mandibular second molar teeth. Am J Orthod Dentofacial Orthop. 1987; 91(3):242-51
10. García-Calderón M, Torres-Lagares D, González-Martín M, Gutiérrez-Pérez JL. Rescue surgery (surgical repositioning) of impacted lower second molars. Med Oral Patol Oral Cir Bucal 2005; 10:448-53.
11. Magnusson C, Kjellberg H. Impaction and retention of second molars: diagnosis, treatment and outcome. A retrospective follow-up study. Angle Orthod. 2009; 79(3):422-7.











 texto em
texto em 


