Servicios Personalizados
Revista
Articulo
Links relacionados
Compartir
Ciencias Psicológicas
versión impresa ISSN 1688-4094versión On-line ISSN 1688-4221
Cienc. Psicol. vol.17 no.2 Montevideo dic. 2023 Epub 01-Dic-2023
https://doi.org/10.22235/cp.v17i2.2699
Original Articles
Resilience and adherence to antiretroviral therapy in people living with HIV: An integrative review
1Universidade Federal do Triângulo Mineiro. Universidade de São Paulo, Brasil
2 Universidade Federal do Triângulo Mineiro. Universidade de São Paulo, Brasil, rossatousp@usp.br
3 Universidade de São Paulo, Brasil
The objective of this integrative literature review was to synthesize the available evidence on the role of resilience in adherence to antiretroviral therapy (ART) among people living with HIV. A committee of independent judges performed systematic searches in the CINAHL, LILACS, PePSIC, PsycINFO, PubMed, SciELO, Scopus and Web of Science databases/libraries. The data were organized in the Rayyan software. A total of 14 articles published between 2010 and 2021 were retrieved. The results were presented regarding the approach and level of adherence, resilience approach and association between resilience and adherence. In all the studies it was observed that resilience was involved in the ART adherence process, in addition to evidencing the use of different conceptual approaches to resilience, with predominance of a procedural understanding of the construct and scarcity of measuring instruments. The literature review showed that few studies have assessed resilience in people living with HIV and, especially, the relationship between resilience and adherence, despite acknowledging that resilience can modulate a person's ability to deal with the stressors of living with HIV and its health care measures.
Keywords: resilience; HIV/AIDS; treatment adherence and compliance; antiretroviral therapy
O objetivo desta revisão integrativa de literatura foi sintetizar as evidências disponíveis sobre o papel da resiliência na adesão à terapia antirretroviral em pessoas vivendo com HIV. Um comitê de juízes independentes realizou buscas sistematizadas nas bases/bibliotecas CINAHL, LILACS, PePSIC, PsycINFO, PubMed, SciELO, Scopus e Web of Science. Os dados foram organizados no software Rayyan. Foram recuperados 14 artigos publicados entre 2010 e 2021. Os resultados foram apresentados quanto à abordagem e nível da adesão, abordagem da resiliência e associação entre resiliência e adesão. Observou-se, em todos os estudos, que a resiliência esteve envolvida no processo de adesão à TARV, além do uso de diferentes abordagens conceituais acerca da resiliência, com predomínio de uma compreensão processual do construto e escassez de instrumentos de mensuração. A revisão de literatura evidenciou que poucos estudos avaliaram a resiliência em PVHIV e principalmente a relação entre resiliência e adesão, apesar do reconhecimento de que a resiliência pode modular a capacidade da pessoa de lidar com os estressores do viver com HIV e seus cuidados em saúde.
Palavras-chave: resiliência; HIV/AIDS; cooperação e adesão ao tratamento; terapia antirretroviral
El objetivo de esta revisión integradora de la literatura fue sintetizar la diversa evidencia disponible sobre el rol de la resiliencia en la adherencia a la terapia antirretroviral en personas que viven con VIH. Un comité de jueces independientes realizó búsquedas sistemáticas en las bases de datos CINAHL, LILACS, PePSIC, PsycINFO, PubMed, SciELO, Scopus y Web of Science. Los datos se organizaron en el programa Rayyan. Se recuperaron 14 artículos publicados entre 2010 y 2021. Se presentaron los resultados en cuanto al enfoque y el nivel de adherencia, enfoque de resiliencia y asociación entre resiliencia y adherencia. En todos los estudios se observó que la resiliencia estuvo implicada en el proceso de adherencia a la ART, además de evidenciarse diferentes acercamientos conceptuales de la resiliencia, con predominio de una comprensión procedimental del constructo y escasez de instrumentos de medición. La revisión de la literatura demostró que pocos estudios han evaluado la resiliencia en PVVIH y, especialmente, la relación entre resiliencia y adherencia, a pesar de reconocerse que la resiliencia puede modular la capacidad de una persona para lidiar con los factores estresantes de vivir con el VIH y su atención médica.
Palabras clave: resiliencia; VIH/SIDA; cumplimiento y adherencia al tratamiento; terapia antirretroviral
HIV/AIDS is still a global public health problem. In the world, approximately 37.7 million people were living with the disease in 2020 and, in the same period, approximately 680,000 deaths related to the infection were recorded (United Nations Programme on HIV/AIDS, Unaids, 2021). In recent decades there has been a significant reduction in morbidity and mortality related to HIV/AIDS with the introduction and availability of antiretroviral therapy (ART), turning the infection into a chronic condition with control possibilities (Drain et al., 2020; Seidl & Remor, 2020).
ART aims at modulating HIV progression by suppressing its plasma viral load, improving the immune reconstitution of people living with HIV (PLHIV) and preventing transmission of the virus (Rodger et al., 2019). However, efficacy of the treatment necessarily depends on adherence to ART throughout life (Carvalho et al., 2019). Adherence to a medication involves taking it at the prescribed dose and frequency, which represents a complex, dynamic and multidetermined process that is directly related to the economic and sociocultural context in which PLHIV are inserted (Mendelsohn et al., 2014).
Recent progress has been observed in the fight against the epidemic, such as the recommendation of regular tests for HIV and the protocol called Treatment as Prevention (TasP), becoming one of the most relevant measures in control of virus transmission (Sabapathy et al., 2022). Another important response to HIV/AIDS is the conceptual model of the PLHIV care continuum, used to monitor and follow-up the challenging Unaids 95/95/95 target, in which the countries should aim at achieving the following by 2030: 95 % of diagnosed PLHIV; 95% of the diagnosed PLHIV using ART; and 95 % of the PLHIV on ART with viral suppression. These indicators were 84/87/90 in 2020. The care cascade also allows identifying gaps and opportunities for specific interventions to improve retention in health services and health outcomes in this field, pointing to the need to face the vulnerabilities that permeate prevention and living with HIV/AIDS (Sabapathy et al., 2022; Unaids, 2015; Unaids, 2021).
It is observed that the epidemic is disproportionately concentrated in some population segments, the so-called key populations: sex workers, men who have sex with men, transgender people, people who use drugs, people deprived of their freedom and their sex partners, who are in situations of greater vulnerability to HIV/AIDS, present before and remaining after the diagnosis, hindering access, prevention and treatment, as well as their maintenance, in addition to harms to health and well-being (Unaids, 2019).
To understand adherence to antiretrovirals, a systemic view is necessary: the HIV/AIDS experience is permeated by structural, cultural, political, social and psychological vulnerabilities, by stigmatizing and discriminatory processes and by social and gender inequalities, among others, which exert a significant impact on the quality of life of this population, which constantly needs to adapt and deal with the challenges of their condition. In this context, the resilience resources gain prominence (Carvalho et al., 2019; Carvalho et al., 2022; Dulin et al., 2018; Seidl & Remor, 2020).
Resilience is among the factors that can interfere with adherence to ART (Dulin et al., 2018), as it represents a significant aspect that may (or may not) be developed by people in the therapeutic path. In this sense, some studies have suggested that resilience can be associated with better adherence to antiretrovirals and viral suppression (Dale et al., 2014).
Resilience is understood as the ability of a person or a group to recover or successfully face a situation despite adversity (Harrison & Li, 2018). This construct has been investigated as a characteristic, a personality trait, or as a process (Pruchno et al., 2015). Ungar et al. (2013) conceptualize resilience in a socioecological framework, as a person's ability to adaptively deal with adversities and/or to recover after traumatic experiences through physical, psychological, social and cultural resources.
In the studies about HIV/AIDS, introducing the concept of resilience shifted the emphasis from vulnerability to protection factors (Jimenez-Torres et al., 2017). Resilience resources can protect PLHIV by promoting positive health behaviors (adherence to ART and regular attendance at health services), in addition to helping people cope with vulnerabilities and stressful events related to living with HIV, thus improving their overall health and health behaviors (Dulin et al., 2018; Harper et al., 2014; Jimenez-Torres et al., 2017).
When reviewing the definition and study of resilience resources in PLHIV, Dulin et al. (2018) point out significant gaps in this research field, with the need to encourage research studies on this topic so that their results are incorporated into clinical contexts. Due to the importance it assumes in the health care process, it is important to study the impact of resilience on PLHIV and its relationship with adherence to the treatment (Araújo et al., 2019; Dulin et al., 2018; Jimenez-Torres et al., 2017). Thus, the objective of this integrative literature review was to synthesize the available evidence on the role of resilience in adherence to antiretroviral therapy among PLHIV, so that health practices that consider such relationships can be outlined.
Method
Type of study
This is an integrative literature review. Integrative reviews are characterized as a research method that allows incorporating diverse evidence into the professional practice, as they gather and summarize the results of papers on a given topic or issue in a systematic and orderly manner and using different levels of evidence (Beyea & Nicoll, 1998). The guiding question was as follows: Which is the evidence available in the literature about the relationship between resilience and adherence to ART in PLHIV?
Path followed to select the articles
Search and selection of the articles was carried out by two independent judges in July 2021, using a date filter from January 2010 to July 2021 in the databases. The objective of this time frame was to describe the studies from the last decade, allowing access to a recent repertoire of publications. A librarian from the university to which the authors are linked assisted in elaborating the search strategy, performing previous tests together with the authors to define the strategy that best suited the study purpose, in addition to monitoring the entire process. Searches were conducted in the following indexing sources: Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), Periódicos Eletrônicos de Psicologia (PePSIC), Cumulative Index to Nursing and Allied Health Literature (CINAHL), National Library of Medicine (USA) (PubMed), Psychology Information (PsycINFO), Scientific Electronic Library Online (SciELO), Scopus and Web of Science. The following crossings between descriptors were used in the CINAHL, PsycINFO, PubMed, Scopus and Web of Science databases: (resilience) AND (adherence) AND (antiretroviral) AND (HIV OR AIDS OR acquired immunodeficiency syndrome), whereas the following was used in LILACS, SciELO and PePSIC: (resiliência OR resiliencia OR resilience) AND (adesão OR adhesión OR adherence) AND (antirretroviral OR antiretroviral) AND (HIV OR VIH OR SIDA OR AIDS OR síndrome de imunodeficiência adquirida OR síndrome de inmunodeficiencia adquirida OR acquired immunodeficiency syndrome).
The inclusion criteria established to select the articles were as follows: a) empirical articles that identified the relationship between resilience and adherence to ART; b) articles published in English, Spanish or Portuguese; and c) articles depicting studies conducted with PLHIV. Literature review articles, theoretical studies, case reports, dissertations, theses, book chapters, books, consensus, supplements or comments to the editor or by the editor and obituaries were excluded, as well as papers on elaboration and validation of instruments.
To verify that the articles met the inclusion and exclusion criteria, two independent judges with experience in the theme and in literature review designs carried out the following evidence assessment sequence by consensus: 1. Reading, analysis and selection of the titles from all the studies identified; 2. Reading, analysis and selection of the abstracts from the studies selected in the previous phase; and 3. Full-reading, analysis and selection of the final articles. In case of disagreements between the reviewers as to adequacy of a study, a third judge made a final assessment. The entire process to select the articles was performed in the Rayyan platform (Ouzzani et al., 2016).
After excluding the articles that failed to meet the criteria adopted, both judges filed the material that comprised the analysis corpus, with the following data: authors, title of the study, year of publication, study locus, number of participants, study design, type of conceptual approach to resilience, instruments used to address resilience, adherence measures used, levels of adherence and association between resilience and adherence. From the meticulous reading of the corpus, the data were organized and discussed in thematic axes, previously established, aiming to answer the review guiding question: (a) Approach and adherence level; (b) Approach to resilience; and (c) Associations between resilience and adherence.
Results
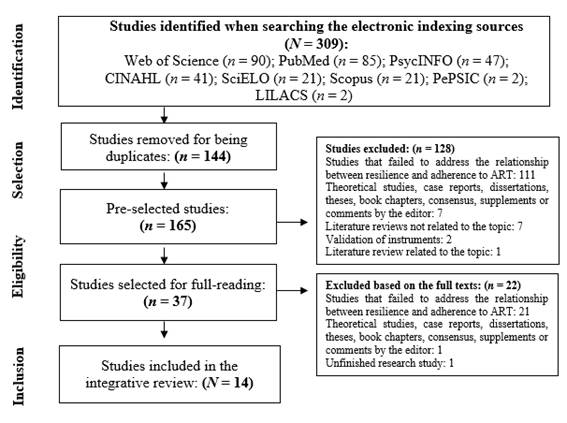
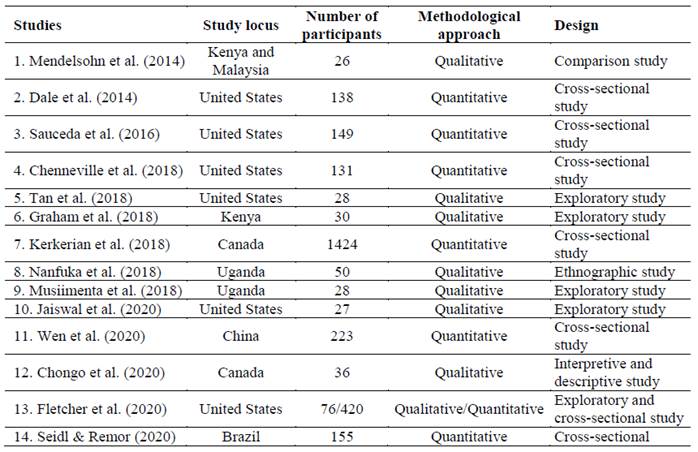
Figure 1 shows the study selection strategy flowchart according to the PRISMA protocol (Galvão et al., 2015) and Table 1 explains the main characteristics of the studies included in the final sample. As presented in Table 1, 14 articles were retrieved.
In relation to the participants, three papers were carried out with men who have sex with men (MSM); of these, two studies were conducted with the black-skinned population (Tan et al., 2018; Graham et al., 2018) and one with MSM at an American health center for Latinos near the border with Mexico (Sauceda et al., 2016). Three articles were conducted with women (Dale et al., 2014; Fletcher et al., 2020; Kerkerian et al., 2018). Two studies researched users of public health centers with limited resources in the African continent (Musiimenta et al., 2018; Nanfuka et al., 2018). One paper dealt with low-income black-skinned and Latino populations (Jaiswal et al., 2020). One study was conducted with refugees (Mendelsohn et al., 2014). One survey interviewed adolescents and young adults with HIV (Chenneville et al., 2018), whereas Chongo et al. (2020) researched native Canadian men. Wen et al. (2020) interviewed users of health services in a Chinese city and Seidl and Remor (2020) approached people undergoing medical and psychosocial follow-up in a Brazilian hospital.
Also, according to Table 1, it is verified that six quantitative studies, seven qualitative ones and one mixed-methods paper were retrieved. The corpus categorization is presented below, in three main topics:
1) Approach and adherence level
In relation to the approach to adherence to ART, eight studies used self-report on medication use as an adherence measure, employed through questionnaires (Dale et al., 2014; Fletcher et al., 2020; Mendelsohn et al., 2014) and validated instruments (Chenneville et al., 2018; Kerkerian et al., 2018; Sauceda et al., 2016; Seidl & Remor, 2020; Wen et al., 2020). Among the instruments, Wen et al. (2020) made use of the Morisky Medication Adherence Scale, Seidl and Remor (2020) resorted to the Questionnaire for the Assessment of the Adherence to the Antiretroviral Treatment (Cuestionario para Evaluar la Adhesión al Tratamiento Antirretroviral, CEAT-VIH), Chenneville et al. (2018) resorted to BEHKA-HIV and Sauceda et al. (2016) and Kerkerian et al. (2018) employed the Visual Analog Scale (VAS) for Adherence. Five studies addressed this topic by means of interviews, exploring the participants' narratives about adherence (Chongo et al., 2020; Graham et al., 2018; Musiimenta et al., 2018; Nanfuka et al., 2018; Tan et al., 2018), whereas Jaiswal et al. (2020) did not use instruments to assess adherence, as they interviewed participants who previously had low engagement in adherence and retention in health services.
Of the 14 studies that comprise this review, six presented a defined cutoff point for adherence, which varied between 80 % (Chongo et al., 2020), 90 % (Kerkerian et al., 2018), 95 % (Dale et al., 2014; Fletcher et al., 2020; Mendelsohn et al., 2014) and 100 % (Wen et al., 2020). In turn, the adherence degree found was informed by six studies (Dale et al., 2014; Fletcher et al., 2020; Kerkerian et al., 2018 ; Mendelsohn et al., 2014; Sauceda et al., 2016; Seidl & Remor, 2020), with the lowest adherence measured being 76.5 % in a survey conducted in the United States (Dale et al., 2014), whereas the highest adherence degree was 91.6 % in a study also carried out in the same country (Sauceda et al., 2016) and 90 and 91 % in a paper carried out in Kenya and Malaysia, respectively (Mendelsohn et al., 2014).
2) Approach to resilience
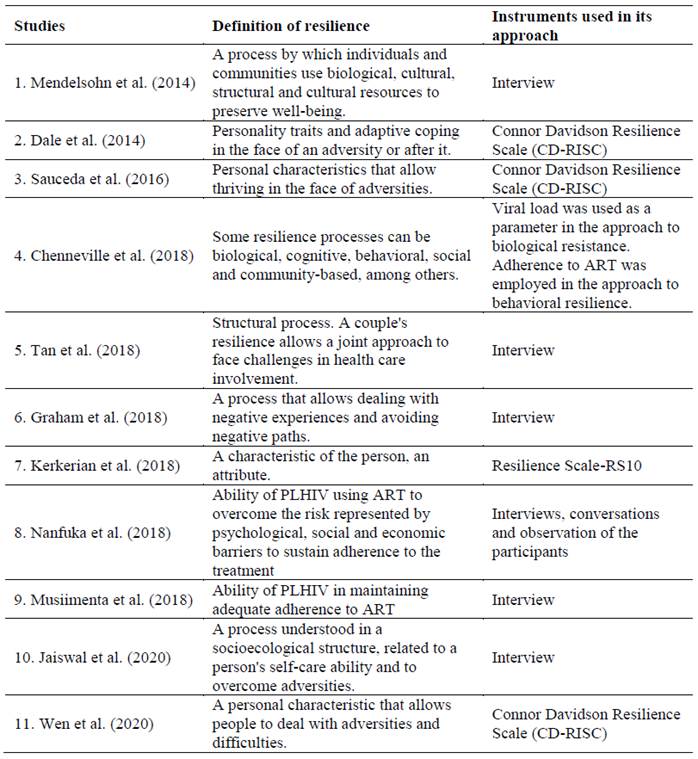
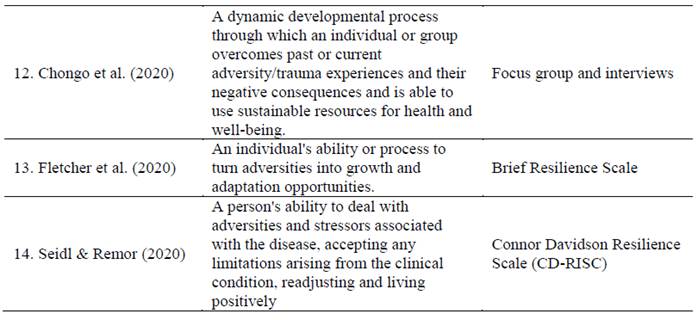
The articles analyzed dealt with resilience using different conceptual approaches. These approaches, as well as the instruments employed to assess resilience, are summarized in Table 2 T3.
Mendelsohn et al. (2014), Chenneville et al. (2018), Tan et al. (2018), Graham et al. (2018), Jaiswal et al. (2020), Chongo et al. (2020) and Fletcher et al. (2020) approached resilience as a process. It is noted that, in their paper, Chenneville et al. (2018) include resilience processes, in which it can be approached as biological, behavioral, social and community-based. Five research studies defined resilience as a characteristic of the person that allows them to deal with adversities (Dale et al., 2014; Kerkerian et al., 2018; Sauceda et al., 2016; Seidl & Remor, 2020; Wen et al., 2020). In turn, Nanfuka et al. (2018) and Musiimenta et al. (2018) approached resilience as the ability of PLHIV to overcome adversities and sustain adherence to the treatment; in these two studies and in the one by Chenneville et al. (2018), adherence to antiretrovirals was and indicator of resilience.
In relation to the instruments employed in the approach to resilience (Table 2), seven studies resorted to interviews (Chongo et al., 2020; Graham et al., 2018; Jaiswal et al., 2020; Mendelsohn et al., 2014; Musiimenta et al., 2018; Nanfuka et al., 2018; Tan et al., 2018). In addition to the interviews, Chongo et al. (2020) used focus groups, and Nanfuka et al. (2018) employed conversations and observation of the participants. Among the studies that employed validated instruments, Dale et al. (2014), Sauceda et al. (2016), Seidl and Remor (2020) and Wen et al. (2020) used the Connor Davidson Resilience Scale (CD-RISC), Kerkerian et al. (2018), the Resilience Scale (RS10) and Fletcher et al. (2020) resorted to the Brief Resilience Scale. In turn, Chenneville et al. (2018) used viral load as a parameter for biological resilience and adherence to ART for behavioral resilience.
3) Associations between resilience and adherence
It is observed that, in all 14 studies analyzed, resilience was involved in the adherence process, with 11 of them showing that resilience was associated with better adherence to ART or influenced involvement with the treatment and adherence (Chongo et al., 2020; Dale et al., 2014; Fletcher et al., 2020; Graham et al., 2018; Jaiswal et al., 2020; Kerkerian et al., 2018; Mendelsohn et al., 2014; Sauceda et al., 2016; Seidl & Remor 2020; Tan et al., 2018; Wen et al., 2020). In turn, adherence to antiretrovirals was an indicator of resilience in three research studies (Chenneville et al., 2018; Musiimenta et al., 2018; Nanfuka et al., 2018). These findings are better discussed below.
Discussion
This integrative literature review explored the role of resilience in adherence to ART among PLHIV. The analysis of a decade of production in this field showed an increase in studies from 2018 onwards, and this trend may be related to the recent theoretical accumulation on the infection and the new prevention technologies that have emerged in recent years, especially those structured from ART use (Rodger et al., 2019; Sabapathy et al., 2022).
TasP, the HIV care cascade and the Unaids targets led to an increase in the number of people undergoing treatment (Brito & Seidl, 2019; Seidl & Remor, 2020), in addition to fostering monitoring and research of the HIV indicators from the global response to the pandemic and the vulnerability and protection factors for preventing and coping with HIV/AIDS. However, research studies on the topic are still incipient in the national and international literature (Araújo et al., 2019; Brito & Seidl, 2019; Dulin et al., 2018; Jimenez-Torres et al., 2017). These authors point to the lack of literature on resilience in contexts of chronic diseases, mainly in relation to HIV/AIDS and associated with the impact of this construct on health care, physical health and progression of the disease.
There were variations in the groups of participants from the studies reviewed. Most of the studies were carried out with populations exposed to multiple vulnerabilities, such as social, ethnic, racial, gender inequalities and stigmatizing processes, in addition to the HIV experience itself. The literature highlights that there are differences in the way adherence to ART and resilience are presented cross PLHIV populations and contexts, remaining a challenge to sustain adherence in scenarios with different social and structural realities (Lacombe-Duncan et al., 2020; Mendelsohn et al., 2014; Nanfuka et al., 2018). In general, the HIV infection disproportionately affects minority and economically disadvantaged groups, rendering it important to study resilience with these population segments, which need specific strategies for HIV prevention and interventions to cope with the disease (Chenneville et al., 2018; Kerkerian et al., 2018).
According to Unaids (2021), in 2020 there were 1.5 million new HIV infections predominantly among key populations, their companions and their sex partners, corresponding to 65 % of the infections. However, these population groups remain invisible and distant from health services for HIV, as can be corroborated in the current review.
The existing inequalities in access and adherence to the treatment are the result of excluding or nonexistent public policies and actions. Vulnerabilities support the social invisibility experience, which in turn is related to stigma, prejudice and discrimination, leading to intense psychosocial distress (Unaids, 2019). Investigating the role of individual and community resilience in overcoming adverse health outcomes and social barriers, especially in people who face adversity and significant stressors, is a priority for global public health (Fletcher et al., 2020; Graham et al., 2018; Kerkerian et al., 2018; Nanfuka et al., 2018; Tan et al., 2018).
In this review, it was possible to perceive variations in the adherence rates between population groups, even within the same country, such as the United States, where studies with PLHIV with low adherence were carried out (Jaiswal et al., 2020) as well as surveys that found average and high adherence rates. Dale et al. (2014) assessed 76.5 % adherence in women living with HIV, whereas Sauceda et al. (2016) obtained 91.6 % adherence in their research conducted with Latino MSM. High adherence rates were also found in developing countries. Mendelsohn et al. (2014) verified between 90 % and 91 % adherence in refugees from Kenya and Malaysia. In addition to showing the heterogeneous character of the HIV/AIDS pandemic and, consequently, of adherence to antiretrovirals, which represents a major challenge for public health, this variability in the adherence rates points to the complexity of assessing adherence to ART, given that there is no gold standard measure for adherence, which can hinder comparing outcomes across studies (Carvalho et al., 2019).
All the studies analyzed included a conceptualization of resilience, although from different approaches. In general, they highlighted that resilience allows people to overcome potentially traumatic circumstances and adapt positively to adverse conditions. Some studies approached resilience as a process whereas others did so as a characteristic of each person. For Pruchno et al. (2015) there is a continuous debate involving the nature of resilience, sometimes as a personality trait and other as a dynamic process. There are growing criticisms about defining resilience exclusively as an individual phenomenon, as this ignores the social context and systems in which resilience can occur. In the HIV/AIDS context, permeated by significant vulnerabilities, such approach might contribute to blaming PLHIV and increasing the stigma related to the illness, with the risk of losing sight of the multiple health determinants that permeate the existence of this population segment (Dulin et al., 2018; Harrison & Li, 2018; Unaids, 2019).
In this scenario, Dulin et al. (2018) explore resilience as a resource that promotes positive psychological, behavioral and/or social adaptation in the face of stressors and adversity. Therefore, such resources would protect the health of PLHIV by promoting positive health behaviors and allowing them to deal positively with the adversities of living with HIV. Among the resilience resources, the literature herein retrieved refers to self-efficacy, the capacity for positive coping with adversity, positive religious coping, optimism, hope, self-compassion, resistance, compassionate love, self-esteem, control and problem-solving beliefs, good relationships with health professionals and services, and social support.
Some of the studies reviewed conceptualized resilience as the ability of PLHIV to sustain adherence to the treatment (Chenneville et al., 2018; Musiimenta et al., 2018; Nanfuka et al., 2018). Among these papers, Chenneville et al. (2018) encompass resilience processes as biological, cognitive, behavioral, social and community-based. Harper et al. (2014) also used this definition and evidenced in their intervention with adolescent trans women and young adults living with HIV that resilience processes included cognitive processes that promote health, adoption of healthy behavioral practices and mobilization of social support. For Hussen et al. (2017), cognitive and behavioral resilience is associated with health-promoting psychosocial factors. Also in conceptual terms, the definition of the construct as involvement in health care also emerged (Jaiswal et al., 2020; Tan et al., 2018), in a sense that would allow for the adaptation and management of elements associated with the therapeutic path.
Regarding the testing instruments, it is observed that general resilience scales were used that were not developed or adapted for the PLHIV condition. Dulin et al. (2018) point out the importance of resilience measures aimed at PLHIV that capture this construct not only at an individual level, but in its complexity and multiple levels. Brito and Seidl (2019) reported on the difficulty finding validated resilience instruments for PLHIV in Brazil, which evidences a significant gap in the field of research on resilience and HIV infection. The use of qualitative instruments, such as interviews, was referred to as appropriate in a complex context, allowing greater flexibility and depth (Jimenez-Torres et al., 2017; Pruchno et al., 2015).
All papers analyzed recognize that resilience can modulate a person's ability to deal with the stressors of living with HIV and its health care, with 11 studies showing that resilience was associated with better adherence to ART or influenced engagement with treatment and adherence. When thinking about seropositivity, resilience allows PLHIV to overcome psychological, social and economic barriers to accepting their condition, preventing the impacts of the disease and developing their well-being and quality of life; however, it is reiterated that resilience should be understood as a complex and dynamic phenomenon built from the relationship between a person and their social context (Brito & Seidl, 2019; Jimenez-Torres et al., 2017). The study by Nanfuka et al. (2018) showed that, even with several barriers, the participants maintained adherence to ART, making use of the resources from their social networks to continue the treatment, which reiterates the importance of social support networks in promoting resilience among PLHIV in environments with limited resources (Dulin et al., 2018; Nanfuka et al., 2018; Ungar et al., 2013).
The research by Sauceda et al. (2016), conducted with Latin American MSM living with HIV, evidenced that people with a history of sexual abuse in childhood reported greater depressive symptoms and worse adherence, mainly when they were not able to deal with the stressful event but, as their resilience was strengthened, they managed to cope better with the traumatic situation and their adherence to antiretrovirals was increased. Resilience can be developed or reinforced and depends on social factors and environmental influences and on the resilience processes to occur when individuals encounter a stressful situation and have access to or have protective conditions that isolate them against the negative effects of that stress (Harper et al., 2014). Chongo et al. (2020) warn that, although some studies postulate that resilience increases with exponential exposure to a traumatic experience, this assumption needs to be understood sparingly so as not to trivialize and romanticize the resilience process, considering that although trauma is always harmful and imposes distress, not everyone who experiences it develops a psychopathology and/or becomes more resilient.
Introducing the concept of resilience has contributed a new panorama to studies on HIV/AIDS: the analysis of protective factors, known to be associated with positive health outcomes (Brito & Seidl, 2019; Jimenez-Torres et al., 2017). When thinking about strategies to strengthen resilience resources, it is important to consider the complexity of this phenomenon, the multiplicity of elements to which it is related and the different cultural contexts involved. Based on the synthesis of the diverse evidence available in the literature, it is recommended that the topic should be included more systematically in research and health care protocols, expanding the list of knowledge for future designs.
Final considerations
The literature review indicated that few studies evaluated the relationship between resilience and adherence, in addition to diversity of approaches to resilience and scarcity of validated instruments for this construct aimed at PLHIV, which presents itself as a significant gap in this theme. It is observed that the papers analyzed recognize that resilience can modulate a person's ability to deal with the stressors of living with HIV and its health care, highlighting the importance of resilience in this context and the need for evidence-based actions in health services to improve adherence to antiretrovirals, with a focus on building resilience. Thus, the role of resilience in this context is reinforced, as well as of strengthening adherence, which can lead to better health outcomes. It is noted that this synthesis was produced from a few studies retrieved from the current review, emphasizing the need for this topic to continue to be investigated, as well as the importance of future surveys that retrieve increasingly recent evidence and that add up to already consolidated knowledge in the area.
This review also signaled the importance of studying resilience and its social and population-based determinants. It is noted that research studies investigating the relationship between resilience, adherence to ART and clinical, emotional and social conditions, as well as interventions that address these dimensions, would contribute to the academic and technical areas, as well as to the general population. Among the limitations of the current study, it is noteworthy that the review did not consider retention in health services and clinical outcomes, such as the relationship between resilience with CD4 lymphocyte counts and HIV viral loads. Such delimitation is recommended for future studies. Although this study favored the integrative review strategy based on the concept of evidence-based practice, which only considered empirical articles, knowledge from other designs can be added, such as scoping reviews. Due to the fact that few studies have been retrieved, exploration of the phenomenon based on a scoping review, more exploratory, may allow access to diverse evidence built in different scenarios and that have not yet been published, for example, in sources captured by the databases/libraries employed in this review. Follow-up of this literature, perennially updating the available evidence, can contribute to the role of resilience in adherence to be increasingly matured. It is essential that there is an increase in the number of measuring instruments, which should be increasingly refined in order to compare a complex concept that has also been problematized in the health field.
REFERENCES
Araújo, L. F. D., Leal, B. D. S., Santos, J. V. D. O., & Sampaio, A. V. C. (2019). Análise da resiliência entre pessoas que vivem com HIV/AIDS: Um estudo psicossocial. Psicologia: Teoria e Pesquisa, 35. https://doi.org/10.1590/0102.3772e35416 [ Links ]
Beyea, S. & Nicoll, L. H. (1998). Writing an integrative review. AORN Journal, 67(4), 877-881. https://doi.org/10.1016/S0001-2092(06)62653-7 [ Links ]
Brito, H. L. D. & Seidl, E. M. F. (2019). Resiliência de pessoas com HIV/AIDS: Influência do coping religioso. Trends in Psychology, 27(3), 647-660. https://doi.org/10.9788/tp2019.3-04 [ Links ]
Carvalho, P. P., Barroso, S. M., Coelho, H. C., & Penaforte, F. R. O. (2019). Fatores associados à adesão à terapia antirretroviral em adultos: Revisão integrativa de literatura. Ciência & Saúde Coletiva, 24, 2543-2555. https://doi.org/10.1590/1413-81232018247.22312017 [ Links ]
Carvalho, P. P., Cunha, V. F., & Scorsolini-Comin, F. (2022). Religiosidade/espiritualidade e adesão à Terapia Antirretrovial em pessoas vivendo com HIV. Psico-USF, 27(1), 45-60. https://doi.org/10.1590/1413-82712022270104 [ Links ]
Chenneville, T., Gabbidon, K., Lynn, C., & Rodriguez, C. (2018). Psychological factors related to resilience and vulnerability among youth with HIV in an integrated care setting. AIDS Care, 30(sup4), 5-11. https://doi.org/10.1080/09540121.2018.1488032 [ Links ]
Chongo, M., Lavoie, J. G., Mignone, J., Caron, N. R., Harder, H. G., & Chase, R. (2020). Indigenous men adhering to highly active antiretroviral therapy: Navigating through culturally unsafe spaces while caring for their health. Frontiers in Public Health, 8, 519. https://doi.org/10.3389/fpubh.2020.569733 [ Links ]
Dale, S., Cohen, M., Weber, K., Cruise, R., Kelso, G., & Brody, L. (2014). Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care and STDs, 28(3), 136-143. https://doi.org/10.1089/apc.2013.0329 [ Links ]
Drain, P. K., Bardon, A. R., Simoni, J. M., Cressey, T. R., Anderson, P., Sevenler, D., Olanrewaju, A. O., Gandhi, M., & Celum, C. (2020). Point-of-care and near real-time testing for antiretroviral adherence monitoring to HIV treatment and prevention. Current HIV/AIDS Reports, 17(5), 487-498. https://doi.org/10.1007/s11904-020-00512-3 [ Links ]
Dulin, A. J., Dale, S. K., Earnshaw, V. A., Fava, J. L., Mugavero, M. J., Napravnik, S., Hogan, J. W., Carey, M. P., & Howe, C. J. (2018). Resilience and HIV: A review of the definition and study of resilience. AIDS Care, 30(sup. 5), S6-S17. https://doi.org/10.1080/09540121.2018.1515470 [ Links ]
Fletcher, F. E., Sherwood, N. R., Rice, W. S., Yigit, I., Ross, S. N., Wilson, T. E., Weiser, S. D., Johnson, M. O., Kempf, M. C., Konkle-Parker, D., Wingood, G., Turan, J. M., & Turan, B. (2020). Resilience and HIV treatment outcomes among women living with HIV in the United States: A mixed-methods analysis. AIDS Patient Care and STDs, 34(8), 356-366. https://doi.org/10.1089/apc.2019.0309 [ Links ]
Galvão, T. F., Pansani, T. D. S. A., & Harrad, D. (2015). Principais itens para relatar revisões sistemáticas e meta-análises: A recomendação PRISMA. Epidemiologia e Serviços de Saúde, 24, 335-342. https://doi.org/10.5123/S1679-49742015000200017 [ Links ]
Graham, S. M., Micheni, M., Secor, A., van der Elst, E. M., Kombo, B., Operario, D., Amico, K. R., Sanders, E. J., & Simoni, J. M. (2018). HIV care engagement and ART adherence among Kenyan gay, bisexual, and other men who have sex with men: A multi-level model informed by qualitative research. AIDS Care, 30(sup5), S97-S105. https://doi.org/10.1080/09540121.2018.1515471 [ Links ]
Harper , G. W., Bruce, D., Hosek, S. G., Fernandez, M. I., & Rood, B. A. (2014). Resilience processes demonstrated by young gay and bisexual men living with HIV: Implications for intervention. AIDS Patient Care and STDs, 28(12), 666-676. https://doi.org/10.1089/apc.2013.0330 [ Links ]
Harrison, S. & Li, X. (2018). Toward an enhanced understanding of psychological resilience for HIV youth populations. AIDS Care, 30(sup4), 1-4. https://doi.org/10.1080/09540121.2018.1556384 [ Links ]
Hussen, S. A., Harper, G. W., Rodgers, C. R. R., van den Berg, J. J., Dowshen, N., & Hightow-Weidman, L. B. (2017). Cognitive and behavioral resilience among young gay and bisexual men living with HIV. LGBT Health, 4(4), 275-282. https://doi.org/10.1089/lgbt.2016.0135 [ Links ]
Jaiswal, J., Singer, S. N., & Lekas, H. M. (2020). Resilience and beliefs in the effectiveness of current antiretroviral therapies among recently disengaged low-income people of color living with HIV. Behavioral Medicine, 46(1), 75-85. https://doi.org/10.1080/08964289.2019.1570070 [ Links ]
Jimenez-Torres, G. J., Wojna, V., Rosario, E., Hechevarría, R., Alemán-Batista, A. M., Matos, M. R., Madan, A., Skolasky, R. L., & Acevedo, S. F. (2017). Assessing health-related resiliency in HIV+ Latin women: Preliminary psychometric findings. PloSOne, 12(7). https://doi.org/10.1371/journal.pone.0181253 [ Links ]
Kerkerian, G., Kestler, M., Carter, A., Wang, L., Kronfli, N., Sereda, P., Roth, E., Milloy, M. J., Pick, N., Money, D., Webster, K., Hogg, R. S., de Pokomandy, A., Loutfy, M., & Kaida, A. (2018). Attrition across the HIV cascade of care among a diverse cohort of women living with HIV in Canada. JAIDS Journal of Acquired Immune Deficiency Syndromes, 79(2), 226-236. https://doi.org/10.1097/QAI.0000000000001775 [ Links ]
Lacombe-Duncan, A., Logie, C. H., Newman, P. A., Bauer, G. R., & Kazemi, M. (2020). A qualitative study of resilience among transgender women living with HIV in response to stigma in healthcare. AIDS Care, 32(8), 1008-1013. https://doi.org/10.1080/09540121.2020.1728212 [ Links ]
Mendelsohn, J. B., Rhodes, T., Spiegel, P., Schilperoord, M., Burton, J. W., Balasundaram, S., Wong, C., & Ross, D. A. (2014). Bounded agency in humanitarian settings: A qualitative study of adherence to antiretroviral therapy among refugees situated in Kenya and Malaysia. Social Science & Medicine, 120, 387-395. https://doi.org/10.1016/j.socscimed.2014.06.010 [ Links ]
Musiimenta, A., Atukunda, E. C., Tumuhimbise, W., & Haberer, J. E. (2018). Resilience after withdrawing a technology-based medication adherence support intervention from people living with HIV in rural Uganda. AIDS Care, 30(sup5), S89-S96. https://doi.org/10.1080/09540121.2018.1510107 [ Links ]
Nanfuka, E. K., Kyaddondo, D., Ssali, S. N., & Asingwire, N. (2018). Social capital and resilience among people living on antiretroviral therapy in resource-poor Uganda. PloSOne, 13(6). https://doi.org/10.1371/journal.pone.0197979 [ Links ]
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan: A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4 [ Links ]
Pruchno, R., Heid, A. R., & Genderson, M. W. (2015). Resilience and successful aging: Aligning complementary constructs using a life course approach. Psychological Inquiry, 26(2), 200-207. https://doi.org/10.1080/1047840X.2015.1010422 [ Links ]
Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., Degen, O., & Pechenot, V. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): Final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428-2438. https://doi.org/10.1016/S0140-6736(19)30418-0 [ Links ]
Sabapathy, K., Balzer, L., Larmarange, J., Block, L., Floyd, S., Iwuji, C., Wirth, K., Ayles, H., Fidler, S., Kamya, M., Petersen, M., Havlir, D., Dabis, F., Moore, J., & Hayes, R. (2022). Achieving the UNAIDS 90-90-90 targets: A comparative analysis of four large community randomised trials delivering universal testing and treatment to reduce HIV transmission in sub-Saharan Africa. BMC Public Health, 22(1), 2333. https://doi.org/10.1186/s12889-022-14713-5 [ Links ]
Sauceda, J. A., Wiebe, J. S., & Simoni, J. M. (2016). Childhood sexual abuse and depression in Latino men who have sex with men: Does resilience protect against nonadherence to antiretroviral therapy? Journal of Health Psychology, 21(6), 1096-1106. https://doi.org/10.1177%2F1359105314546341 [ Links ]
Seidl, E. M. F. & Remor, E. (2020). |ao tratamento, resiliência e percepção de doença em pessoas com HIV. Psicologia: Teoria e Pesquisa, 36(spe.). https://doi.org/10.1590/0102.3772e36nspe6 [ Links ]
Tan, J. Y., Campbell, C. K., Conroy, A. A., Tabrisky, A. P., Kegeles, S., & Dworkin, S. L. (2018). Couple-level dynamics and multilevel challenges among black men who have sex with men: A framework of dyadic HIV care. AIDS Patient Care and STDs, 32(11), 459-467. https://doi.org/10.1089/apc.2018.0131 [ Links ]
Ungar, M., Ghazinour, M., & Richter, J. (2013) Annual research review: What is resilience within the social ecology of human development? Journal of Child Psychology and Psychiatry, 54, 348-366. https://doi.org/10.1111/jcpp.12025 [ Links ]
United Nations Programme on HIV/AIDS. (2015). Understanding fast‐track: Accelerating action to end the AIDS epidemic by 2030. United Nations. https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf [ Links ]
United Nations Programme on HIV/AIDS. (2019). Global AIDS update 2019: Communities at the centre. https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf [ Links ]
United Nations Programme on HIV/AIDS. (2021). Global HIV & AIDS statistics: Fact sheet. United Nations. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf [ Links ]
Wen, J., Yeh, T. P., Xie, H., Yu, X., Tang, J., & Chen, Y. (2020). Resilience, self-esteem, self-efficacy, social support, depression and ART adherence among people living with HIV in Sichuan, China. AIDS Care, 33(11), 1414-1421. https://doi.org/10.1080/09540121.2020.1828800 [ Links ]
Funding: This research was possible thanks to the Coordination for the Improvement of Higher Education Personnel (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, CAPES) and the National Council for Scientific and Technological Development (CNPq).
How to cite: Carvalho, P. P., Rossato, L., & Scorsolini-Comin, F. (2023). Resilience and adherence to antiretroviral therapy in people living with HIV: An integrative review. Ciencias Psicológicas, 17(2), e-2699. https://doi.org/10.22235/cp.v17i2.2699
Authors’ participation: a) Conception and design of the work; b) Data acquisition; c) Analysis and interpretation of data; d) Writing of the manuscript; e) Critical review of the manuscript. P. P. C. has contributed in a, b, c, d, e; L. R. in a, b, c, d, e; F. S.-C. in a, c, d, e.
Received: October 11, 2021; Accepted: August 09, 2023











 texto en
texto en