Locus of control has been associated with mental health and well-being variables (April et al., 2012; Shojaee & French, 2014). It is understood as the individual’s perception of the control they exercise in their daily life, which can be internal, when they attribute the results of their actions to yourself, or external, when the subject perceives that the result of some event is the result of the action of agents external to them (Nowicki, 2016; Rotter, 1966). Health-specific locus of control scales are commonly used to gauge the relationship of loci linked to psychological disorders (e.g., Ko & Hsu, 2005; Moshki et al., 2015; Skidmore et al., 2014). However, scales that aim to assess the locus of control without a dependent context (e.g., school, physical health) can be useful for providing comparison and generalization of results. Therefore, seeking to indicate the psychometric qualities of a new locus of control scale for adults (Escala de Locus de Controle, ELOCUS; Couto et al., 2021; 2022), this study aimed to verify the associations between locus of control and mental health variables such as depression, anxiety and emotional dysregulation, and their predictive and mediative relationships, as no studies were found in the literature that contemplated models which measured all these variables together.
The importance of verifying the relationships between locus of control, emotional dysregulation, and psychopathologies such as depression and anxiety is centered on the possibility of interventions in several areas of Psychology, since the locus of control has been used in international research as a predictor of these psychopathologies in diverse contexts (e.g., Clarke, 2004; Hope et al., 2018; Hovenkamp-Hermelink et al., 2019; Moshki et al., 2015). It is therefore necessary to understand how these relationships can be used to structure effective actions to promote mental health.
The relationship between depression and locus of control has been extensively highlighted in the literature (Bliznashki, 2020). Benassi et al. (1988), after a systematic review study with meta-analysis that evaluated the relationship between locus of control and depression, concluded that these constructs were significantly related and the association was moderate. In addition, the study indicated that the higher the externality scores, the greater the depression. Other studies have continued to support the relationship that people with greater external locus of control have more manifestations of depressive symptomatology (Abdolmanafi et al., 2011; Bjørkløf et al., 2018; Khumalo & Plattner, 2019; Millman et al., 2017).
Regarding anxiety, studies have indicated its relationship with the external locus of control, especially in the context of health. For example, women hospitalized with gynecological diseases had greater anxiety manifested by uncertainty about their health status and less need to seek information when their control beliefs in relation to health were more associated with chance (i.e., belief that life events are due to random events, without the individual exerting any influence) (Ko & Hsu, 2005). The influence of the powerful others in external locus of control (i.e., the belief that other people have control over the outcomes of events) was also presented in a study that measured anxiety in a non-clinical group of US college students and health behaviors, mediated by health locus of control. The results suggested that there was a belief that health professionals (powerful others), in general, are responsible for the health states of individuals and that people who had higher scores in anxiety about health also endorsed external control by powerful others more (Skidmore et al., 2014).
About emotional dysregulation, individuals with greater manifestation of external locus of control tend to have more negative emotions (i.e., sadness), affecting their overall state of mental health (Yu & Fan, 2016), and demonstrate difficulties in terms of seeking coping strategies and using maladaptive strategies (i.e., rumination), aggravating their mental health problems (Groth et al., 2019). Therefore, when the individual realizes that they have control over their attitudes, they tend to orient towards action to solve problems and when they do not have this perception, they tend toward paralysis, pessimism, sadness, and fear, becoming passive and even giving up on the action (Skinner, 2016).
For these reasons, this study aims to present the associations between the locus of control and mental health variables. Accordingly, the research hypotheses are that both the external and internal loci of control present correlations of moderate magnitude with the psychopathological variables, alternating the direction of the correlation, as it is understood that the external locus of control is positively associated with the psychopathological variables and the internal locus of control, in opposition, acts as a protective element against psychopathologies.
In terms of prediction and mediation models for the locus of control, no study was found in the literature that has measured the predictive and/or mediating power of the locus of control with the variables depression, anxiety, and emotional dysregulation together. Studies linking the locus of control to one of these variables are commonly found, however, studies with depression and anxiety together are much rarer (e.g., Ceyhan & Ceyhan, 2009; Hovenkamp-Hermelink et al., 2019; Pahlevan Sharif, 2017). Studies that address emotional dysregulation or emotional self-regulation are also scarce (e.g., Farradinna et al., 2019; Hope et al., 2018).
In this study, two models were proposed to measure the predictive and mediating capacity of the construct. The first model evaluated the direct predictive power of the locus of control with all variables (depression, anxiety factors and emotional dysregulation) and the second model, the locus of control acted as a mediator of the relationship between the factors of emotional dysregulation (seeking strategies and pessimism) and depression and anxiety. The choice to keep emotional dysregulation as a predictor was due to the fact that the measure used to assess this construct was developed considering emotional self-regulation in relation to sadness. In other words, starting from the difficulty of managing sadness, could the locus of control contribute in a protective or deleterious way to the levels of anxiety and depression? The hypotheses were that the external locus of control would be found to be a predictor of psychopathologies, as well as emotional dysregulation as it is commonly associated with negative emotions and the internal locus of control would be negatively associated with these, with internality expected to be a protective aspect.
Method
Participants
The convenience sample was composed of 327 participants, with ages between 18 to 79 years old (M = 38.3, SD = 12.8), of both genders (Fem. = 75.2%), with mainly incomplete high school education and marital status composed of married (48.3%) and single (40.7%) people. Regarding the mental health diagnosis, 46.5% of the sample had had a diagnosis of depression, anxiety, or both at some point in life.
Instruments
First, the participants completed a Sociodemographic Questionnaire to characterize the sample in terms of gender, age, marital status and psychodiagnosis. Subsequently, the instruments were answered.
Locus of Control Scale (Escala de Locus de Controle, ELOCUS; Couto et al., 2021; 2022). This is a self-report instrument with two factors, consisting of 29 items (16 for internal locus of control and 13 for external locus of control), with a Likert-type response format ranging from 1 (has nothing to do with me) to 5 (has everything to do with me). In a study of the internal structure, the scale showed good evidence of validity and reliability, with RMSEA (Root Mean Square Error of Approximation) = .066, CFI (Comparative Fit Index) = .977, TLI (Tucker-Lewis Index) = .973, Composite Reliability (CR) and McDonald’s Omega of .96 and .94 for the internal locus and .89 and .84 for the external locus, respectively.
Baptista Depression Scale-adult version (Escala Baptista de Depressão-versão adulto, EBADEP-A; Baptista, 2012). This is a scale to measure depressive symptoms in adults, consisting of 90 paired sentences, forming 45 items, with a four-point Likert-type response format. For interpretation, it is considered that lower scores equate to lower presentations of depressive symptoms. Sensitivity and specificity values for the scale were 77.5% and 87.5%, respectively, and in relation to reliability, the scale had an alpha coefficient of .95.
Emotional Dysregulation Scale - Adults (Escala de Desregulação Emocional Adultos, EDEA; Baptista et al., 2021). The instrument assesses emotional self-regulation when faced with an event in which the individual feels sad. Consisting of 15 items in four factors (coping strategy, externalization of aggressiveness, pessimism, and paralysis), it has a four-point Likert-type response scale, with zero being “none of the time/nothing” and three “always”, with higher scores equating to higher levels of emotional self-regulation. Through CFA, Cremasco et al. (2020) found a model with the following fit indices: RMSEA = .06, CFI = .98, TLI = .98 and internal consistency, through an alpha coefficient of .94 and omega of .96, both for the general scale.
Cognitive Anxiety Scale (Escala Cognitiva de Ansiedade, ECOGA; Falcone et al., 2016). This is a self-report scale for adults to measure distorted anxiety beliefs. The instrument has 31 items with a Likert-type response format, ranging from “strongly disagree” to “strongly agree”. In a study on the internal structure of the scale, Baptista et al. (2020) obtained results that indicated three factors (Negativity and Intolerance of vulnerability, with 12 items each, and Intolerance of uncertainty, with 7 items). The reliability indices ranged from .89 to .94 for the factors and was .94 for the general scale.
Procedures and Data Analysis
The research project was approved by the Research Ethics Committee (Universidade São Francisco, Brazil; CAAE: 36482420.1.0000.5514). The collection procedure took place through the Google Forms platform and participants were invited to participate through social networks. First, the participants accessed the research objectives and the consent form. After acceptance, the instruments were made available.
To assess the correlations, Spearman’s correlation coefficient (r s ) between the locus of control and other constructs was used. The evaluation of the correlation coefficients was made considering the indications of Cohen (1988): weak correlations with r s between .10 and .30; medium or moderate from .30 to .50; and strong above .50. Fisher’s z-transformation test was used to measure the strength of associations between the variables (Eid et al., 2011), which can be used in the case of Spearman’s correlation (Myers & Sirois, 2006).
Path analyses were performed, with the Maximum Likelihood (ML) estimation method, in the two proposed theoretical models, to evaluate the predictive and mediating capacity for the locus of control. The first was a direct prediction model between the loci and all study variables. The second model sought to present the mediating capacity of the locus of control with emotional dysregulation and depression and anxiety. Finally, all descriptive and inferential analyses were performed using SPSS version 23 for Windows, PROCESS for SPSS version 4 (Hayes, 2018) and SPSS AMOS (Arbuckle, 2011). Fisher’s test was performed using the Psychometrica Online-calculator for testing correlations (Lenhard & Lenhard, 2014).
Results
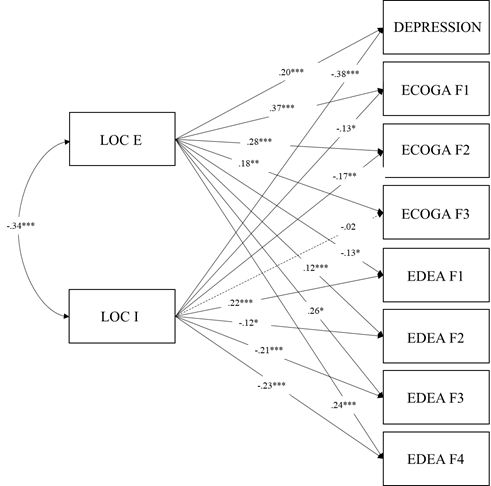
First, Spearman correlations (r s ) were verified between the variables internal and external locus of control, depression, anxiety variables (negativity, intolerance of vulnerability and uncertainty) and emotional dysregulation variables (seeking coping strategies, externalization of aggressiveness, pessimism, and paralysis) (Table 1).
Table 1: Means, standard deviations and correlations between locus of control, depression, anxiety, and emotional dysregulation variables
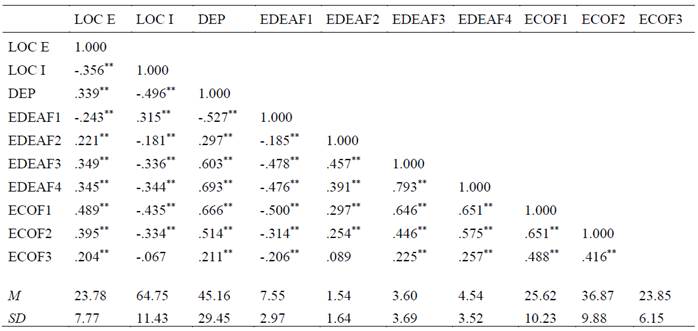
Note: LOC E: External locus of control; LOC I: Internal locus of control; DEP: Depression; EDEAF1: Strategy; EDEAF2: Aggressiveness; EDEAF3: Pessimism; EDEAF4: Paralysis; ECOF1: Negativity; ECOF2: Intolerance of vulnerability; ECOF3: Intolerance of uncertainty; M: Mean; SD: Standard deviation. ** The correlation is significant at level .01 (bilateral).
According to Table 1, all variables showed correlations with statistical significance (p <.01), except for the intolerance of uncertainty variable with the internal locus of control and with externalization of aggressiveness. The external locus of control had a moderate negative correlation with the internal locus of control (r s = -.356).
Fisher’s z-transformation test allowed the strength of associations between the variables to be verified. From this, the external locus of control was found to be more strongly associated with negativity (r s = .489, p < .01) than with pessimism (r s = .349, p< .01) (z = 3.375; p < .001) or with depression (r s = .339, p < .01) (z = 3.709; p < .001). The internal locus of control was more strongly associated with depression (r s = -.496, p < .01) than with pessimism (r s = -.336, p < .01) (z = 3.648; p < .001). Finally, regarding the anxiety variables, both the external and internal loci of control were more strongly associated with negativity than with intolerance of vulnerability (z external = 2.311; p = .010) (z internal = 2.398; p = .008). Next, two theoretical models are presented (Figure 1 and Figure 2) for the assessment of the predictive and mediating capacity of the locus of control based on path analysis.
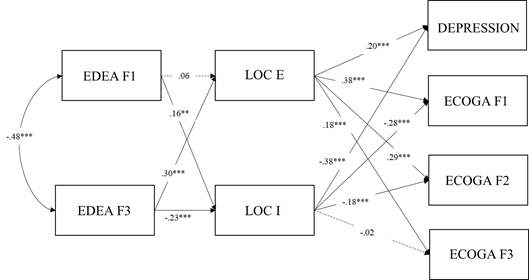
In model 1, the internal and external loci of control were predictors of all aspects of emotional dysregulation, of depression and of the anxiety factors, except for the internal locus of control which was not a predictor for intolerance of uncertainty. In the second model (Figure 2), the locus of control was placed as a mediator between the variables of emotional dysregulation (strategy and pessimism) and the anxiety factors and depression. The paths between the externalization of aggressiveness (F2) and paralysis (F4) variables did not present paths with statistical significance when mediated by the locus of control and, therefore, in a second stage of analysis, they were excluded.
Figure 2 shows the results of the path analysis, which indicated direct associations between strategy and the internal locus (β = .16; p = .009) and between pessimism and the internal locus (β = -.23; p < .001) and external locus (β = .30; p < .001). The external and internal loci of control had direct associations with all anxiety factors and depression, except the internal locus of control and intolerance of uncertainty.
For the mediation between the loci, from the paths which obtained statistical significance in model 2, each path was tested in relation to the mediating effect of each locus. Accordingly, 10 paths from model 2 had statistical significance and were tested individually in mediation models (Table 2).
Table 2: Mediation models between the variables from model 2
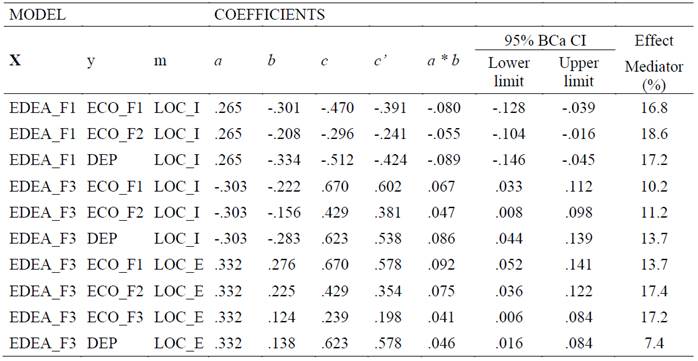
Note: LOC_E: External locus of control; LOC_I: Internal locus of control; EDEA_F1: Strategy; EDEA_F3: Pessimism; ECO_F1: Negativity; ECO_F2: Intolerance of vulnerability; ECO_F3: Intolerance of uncertainty; DEP: Depression; x: predictor variable; y: outcome variable; m: mediating variable; a: direct effect of the predictor variable (x) on the mediating variable (m); b: direct effect between the mediating variable (m) and the outcome variable (y); c: total effect between the predictor variable (x) and the outcome (y); c’: direct effect between the predictor variable and the outcome variable; a*b: indirect effect; 95% BCa CI = 95% confidence interval with bootstrapping technique.
According to Table 2, the internal and external loci of control were mediators in all proposed models. The mediation effect (indirect effect) was significant in all cases and the mediator effect ranged from 7.4% (pessimism → depression) to 17.4% (pessimism → intolerance of vulnerability) for the external locus and from 10.2% (pessimism → negativity) to 18.6% (strategy → intolerance of vulnerability) for the internal locus of control.
Discussion
The study aimed to present the associations, predictions, and mediations between the locus of control and mental health variables. From the results presented, the ELOCUS showed the expected associations, as indicated in the literature, regarding external variables related to mental health, such as depression, anxiety, and emotional dysregulation.
Between the mental health variables and the locus of control, the results supported the study hypotheses. Depression presented a positive correlation of moderate magnitude with the external locus of control and a moderate negative correlation with the internal locus of control. As indicated in other studies (Abdolmanafi et al., 2011; Benassi et al., 1988; Bjørkløf et al., 2018; Khumalo & Plattner, 2019; Millman et al., 2017; Yu & Fan, 2016; Zampieri & Souza, 2011), the locus of control is associated with depression, suggesting that externality corroborates increased levels of depressive symptomatology and that internality can function as a protective agent to depression, as “internal” individuals tend to experience the effects of depressive symptoms less, probably because they perceive greater control over the environment and end up being more active, obtaining more positive outcomes for their behavior.
The internal locus of control was more strongly associated with depression than with pessimism and the external locus of control was more strongly associated with negativity than with depression. The most strongly significant correlation was the internal dimension with depression, contrary to most studies that tend to show this as the external locus correlation with depression. In a recent study on Major Depressive Disorder (MDD) and perceived control, Myles et al. (2020) indicated that people with a lower perception of environmental control tend to have greater depressive symptoms and that the perception of environmental control is causally linked to the initial conditions of MDD. Furthermore, Strong and Gore (2020) stated that a socially predictable environment favors the perception of control and, consequently, an increase in mental health. Given the above, it is suggested that it is possibly more relevant to know the level of internal locus of those with depressive symptoms so that, based on this information, it is possible to plan interventions for this group, with the development and use of strategies to provide the expansion of environmental control in a way that is protective against depression.
Regarding anxiety, the associations agreed with those already found in previous studies (e.g., Ko & Hsu, 2005; Skidmore et al., 2014), which indicated a prejudice due to anxiety when linked to high levels of externality. Gallagher et al. (2014) indicated in a meta-analytic review study that the lack of perception of control was associated with both trait anxiety and anxiety disorders, especially Generalized Anxiety Disorder (GAD). Furthermore, with people who have suffered some type of trauma, high levels of internal locus of control played a protective role in triggering anxiety after the trauma, with the external locus of control being indicated as a risk factor (Atilola et al., 2021).
Also concerning the anxiety factors, both the external and internal locus of control were more strongly associated with negativity than with intolerance of vulnerability. Therefore, in this study, among the components of anxiety, negativity was the most strongly associated with the loci, which leads us to suppose that the most effective interventions for the public diagnosed with anxiety is the increase of internality, however, without losing focus of the need to assist the cognitive restructuring of negative anxiogenic beliefs.
For emotional dysregulation, it is possible to understand this relationship with the locus of control in a similar way to what happens with depression, since, in both cases, sadness is a common variable and, therefore, similar correlations are expected, mainly in the negative dimensions such as pessimism and paralysis. In the case of paralysis, its relationship with externality is understood, as external individuals tend to lack action due to the low perception of environmental control (Skinner, 2016). In the same way, a correlation between seeking coping strategies and internality was expected, as, unlike “external” individuals, “internal” individuals are more action-oriented, proactive, interested, and persistent because they have the belief that they are responsible for the results and consequences of actions (Nowicki, 2016; Skinner, 2016; Zampieri & Souza, 2011). Groth et al. (2019) indicated that the use of maladaptive strategies was related to externality and the use of adaptive strategies related to internality.
Finally, the path analyses in relation to the two models presented corroborate the hypothesis that the locus of control tends to be a predictor for psychopathologies such as depression and anxiety, with externality as a deleterious agent, aggravating symptoms, and internality working in the opposite direction, suggesting a beneficial effect, in addition to acting as a mediator for the seeking coping strategies and pessimism variables with depression and anxiety. However, no similar model was found in other works. In the literature, in the case of depression, the “chance” locus of control was a predictor of neuroticism-mediated depression (Clarke, 2004) and for health the “chance” locus of control was a predictor of postpartum depression (Moshki et al., 2015). As a mediator, Bliznashki (2020) highlighted the effect of the locus of control on the relationship between the strength of an environmental stimulus and depression, indicating that the strength of the stimulus reduced the locus of control and, consequently, increased depressive symptomatology. Myles et al. (2020) studied the effect of personality factors on depression mediated by the perception of control and the desire to control, and their results showed that both mediated the effects of personality factors with depressive symptomatology, in addition to indicating that the desire to control had the effect of increasing perceived control and this, in turn, influenced decreasing depression symptoms.
Ceyhan and Ceyhan (2009) and Skidmore et al. (2014) presented studies in which the locus of control was a mediator in the relationship between separation anxiety and depressive symptoms and between anxiety in relation to health and behaviors related to illness, respectively. In both cases, the external locus of control was present in the mediation, increasing the effect for the outcome variable. It should be noted that these studies used anxiety as an independent variable, unlike the current study in which anxiety factors were placed in the model as dependent variables.
In terms of emotional dysregulation, as with the other psychopathological constructs, the external locus of control had a predictive effect for pessimism, paralysis and aggressiveness, and the internal locus of control for seeking coping strategies. Emotional self-regulation is expressed by the subject’s ability to adjust their emotional reactions through seeking strategies that lead to a state of emotional rebalancing in order to facilitate the achievement of personal goals (Cremasco et al., 2020). Therefore, it is suggested that individuals with a greater perception of control are more focused on seeking strategies because they perceive themselves capable of implementing them.
Conclusions
This study presented the associations, predictions, and mediations between the locus of control and prevalent psychopathologies in the population, such as depression and anxiety, in addition to emotional dysregulation. The results indicated that the research hypotheses were endorsed. In summary, the external locus of control was more associated with the worsening of depression and anxiety symptoms, as well as with the increase in emotional dysregulation for sadness, while the internal locus of control was associated with the mitigation of these symptoms.
Among the limitations of the study is the unbalanced sample, with the majority being women. On the other hand, 46.5% of the people of the sample had been diagnosed with one or more of the disorders presented, which may indicate some quality of the data. Another possible limitation is the age diversity of the sample, ranging from 18 to 79 years. Future studies may verify the differences in means in the locus of control of young adults, middle-aged and older adults, in addition to gender differences.
In this sense, due to the unbalanced sample, another potential limitation is due to the differences between genders for the study variables. Systematic reviews point to a higher prevalence of depression and some anxiety disorders, such as phobia, agoraphobia, and generalized anxiety disorder in women (Gutiérrez-Rojas et al., 2020; Martin, 2003; Stein et al., 2017), which may have caused some bias in the results. Furthermore, it is possible that females are more susceptible to sadness thus impacting on the emotional self-regulation. Finally, regarding the locus of control, there is still no consensus on the differences between genders. Churchill et al. (2020) indicated several studies that suggested that women tend to present with higher external locus of control scores, which made the authors set the hypothesis that it is a factor for worsening of women's mental health levels. On the other hand, in the study by Suárez-Álvarez et al. (2016) the authors found, in a Spanish sample, that women had higher scores of internal locus of control and men of external locus of control. Thus, it is concluded that when assessing the differences between genders in relation to the locus of control, it is necessary to consider the cultural, social, and economic differences and, therefore, it is suggested that in future studies these elements be considered in the analyses.
Another limitation is the research design, which, due to being cross-sectional and correlational, does not cover the influence of the locus of control on the study variables over time. Finally, it is worth noting that the results of these analyses should not be generalized as this is a convenience sample. However, these results may indicate ways that consider the positive effects of the internal locus of control for interventions in mental health.
Future studies need to invest in longitudinal projects and interventional studies, in the most diverse contexts, so that the capacity of the locus of control, on one hand being deleterious and on the other protective for psychopathologies, can be determined, confirming its predictive and mediating power. The locus of control is indicated as an important ally in intervention processes, favoring the improvement of the population’s mental health levels.